Abstract
There is now evidence that, based on cytokine profiles, bipolar disorder (BD) is accompanied by simultaneous activation of the immune-inflammatory response system (IRS) and the compensatory immune-regulatory system (CIRS), and that both components may be associated with the staging of illness. Nevertheless, no BD studies have evaluated the IRS/CIRS ratio using CD (cluster of differentiation) molecules expressed by peripheral blood activated T effector (Teff) and T regulatory (Treg) subpopulations. This study examined Teff/Treg subsets both before and after ex vivo anti-CD3/CD28 stimulation using flow cytometric immunophenotyping in 25 symptomatic remitted BD patients and 21 healthy controls and assessed human cytomegalovirus (HCMV)–specific IgG antibodies. BD is associated with a significantly lowered frequency of unstimulated CD3 + CD8 + CD71+ and CD4 + CD25 + FOXP3 and increased CD4 + CD25 + FOXP3 + CD152+ frequencies and with lowered stimulated frequencies of CD3 + CD8 + CD71+, CD4 + CD25 + FOXP3 + CD152+, and CD4 + CD25 + FOXP3 + GARP cells and, consequently, by an increased stimulated Teff/Treg ratio. Moreover, the number of manic, but not hypomanic or depressive episodes, is significantly and negatively associated with the stimulated proportions of CD3 + CD4 + CD154+, and CD69+ and CD71+ expression on CD4+ and CD8+ cells, while duration of illness (≥ 10 years) is accompanied by a depleted frequency of stimulated CD152+ Treg, and CD154+ and CD71+ CD4+ T cells. BD and anti-human cytomegalovirus (HCMV) IgG levels significantly interact to decrease the expression of CD4 + CD25 + FOXP+GARP T phenotypes. In conclusion, in BD patients, immune injuries, staging, and HCMV seropositivity interact and cause CIRS dysfunctions and exaggerated IRS responses, which play a key role in parainflammation and neuroaffective toxicity. HCMV seropositivity contributes to an immune-risk phenotype in BD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bipolar disorder (BD) is a progressive disorder with recurrent manic, hypomanic, and depressive episodes which alternate with remitted phases, whereby the number of mood episodes is associated with increasing severity of symptoms, increased risk of future episodes, functional decline in the performance of daily tasks, and deficits in memory and executive functions [1,2,3,4,5,6,7]. Based on staging characteristics including recurrence of episodes and past suicidal behaviors, BD patients may be classified into three stages: (a) an early stage when patients show only a few recurrent episodes and increased suicidal ideation; (b) the relapse-regression stage with increased recurrent episodes, more disabilities, lower health-related quality of life and socioeconomic status, and cognitive deficits in memory and executive functions; and (c) the suicidal-regression stage with all hallmarks of stage 2 combined with highly increased suicidal behaviors [7].
There is now also evidence that BD is accompanied by activation of the immune-inflammatory response system (IRS) as well as the compensatory immune-regulatory system (CIRS) [8]. Activated IRS cytokine profiles in BD are indicated by activated M1 macrophage cells with elevated levels of interleukin (IL)-1β, IL-6, and tumor necrosis factor-α (TNFα); T helper-1 (Th-1) cells with increased interferon-γ (IFN-γ) and IL-2 levels; and activated Th-17 cells with increased IL-17 [7]. Activated CIRS profiles are indicated by activated Th-2 cells, including increased IL-4 and IL-5, and T regulatory cells including increased IL-10 and transforming growth factor-β (TGF-β) production [7]. A recent meta-analysis shows that increased levels of immune-regulatory Th-2 (IL-4) and Treg (IL-10) cytokines play a role in BD and, additionally, that cytokine receptors with immune-regulatory functions are involved including increased levels of the soluble IL-1 receptor (sIL-1R) antagonist (indicating increased IL-1 signaling), sTNFR (indicating M1 activation), and sIL-2R (indicating Th-1 cell activation) [9]. The IRS-CIRS theory of BD considers that (a) activated M1, Th-1, Th-2, and Th-17 pathways may mediate the affective and neurocognitive symptoms of the illness through neurotoxic effects, and that (b) increased CIRS functions through IL-4 and IL-10, but also sIL-1RA, sIL-2R, and sTNFR, may attenuate M1 and Th-1 effector functions thereby attenuating the primary IRS [8]. The IRS/CIRS ratio is somewhat higher in BD depression versus unipolar depression while there is no evidence whether IRS or CIRS functions prevail in the different phases of BD [10].
Immune-inflammatory and related oxidative and nitrosative stress (IO&NS) pathways become more sensitized with increasing numbers of episodes and suicidal behaviors which accompany staging of illness. For example, Sowa-Kucma et al. [11] reported that in BD patients, previous episodes, suicide attempts, and hospitalizations are associated with cell-mediated immune and CIRS activation and increased oxidative stress pathways. Furthermore, a machine learning-generated staging index was significantly associated with nitro-oxidative stress and lowered activity of paraoxonase 1 (PON1), a key lipid-associated antioxidant enzyme [7]. There are also some preliminary results showing that inflammatory responses may be more pronounced in the later stages of the illness [12,13,14]. Nevertheless, these conclusions were mainly derived from results on cytokine/cytokine receptor profiles.
Another approach is to define IRS and CIRS immune cell phenotypes using surface markers or cluster of differentiation (CD) molecules expressed by activated T cells or soluble CD markers released in the plasma [15]. Already in the 1990s, it was established that patients with BD depression and mania show signs of T-cell activation as measured with increased sCD25 or sIL-2R plasma levels while patients with unipolar and bipolar depression show increased soluble transferrin receptor (sTfR) concentrations [16, 17]. Measuring CD markers with flow cytometric immunophenotyping methods allows to delineate the frequencies of activated T cells including (a) activated T effector (CD69+ and CD154+) subpopulations; (b) replication CD markers on T cells (e.g., CD71+ or TfR); and (c) activated Treg cells as defined by CD4 + CD25 + FOXP3+ expressing CD152+ or GARP [15, 17,18,19,20,21]. Table 1 summarizes the functional characterization of those immune subsets and CD markers. Nevertheless, only a few papers examined T-cell activation markers in BD. For example, proportions of activated CD4 + CD25+ T cells, as well as increased p-ERK signaling, were observed in peripheral T-cell subsets of patients with BD, while CD4 + CD25 + FOXP3+ cells are lowered or increased [22,23,24,25]. Treg cells not only regulate and suppress inappropriate peripheral immune responses, thereby participating in CIRS functions, but also participate in immune surveillance in the brain, thereby mediating neuro-immune cross-talks [26]. T cells regulate hippocampal neurogenesis including neurocognitive functions and as such aberrations in the ratio between Teff and Treg cells may play an important role in affective disorders through direct effects and the production of IRS/CIRS cytokines [26]. Nevertheless, no studies have examined the ratio between the proportions of activated Teff and activated Treg cells in BD.
Human cytomegalovirus (HCMV) infection may be associated with the pathophysiology of BD and with changes in the expression of CD markers and immune cell functions. A recent study showed that IgG antibodies to HCMV are associated with BD and with elevated manic, but not depressed, mood [27]. One hypothesis is that herpes viruses and especially HCMV may facilitate exacerbations of mental disorders via interactions with susceptibility genes and through alterations in the production of neurotoxic cytokines [27]. Upon primary infection, HCMV remains persistent and may be accompanied by increased expression of late-differentiated memory T cells in the CD4+ and CD8+ lineages, by a shift towards CD8+ T-cell production with increased levels of M1 and Th-1 cytokines, and large populations of HCMV-specific CD4+ and CD8+ T cells [28, 29]. As such, HCMV latency may be accompanied by dysfunctional T-cell populations that could contribute to loss of T-cell functions and, thus, an immune-risk phenotype that could contribute to the pathophysiology of illness including BD. Nevertheless, there are no studies that examined the impact of HCMV seropositivity on immune subsets in patients with BD.
Hence, this study was performed to examine whether (a) the ratio between activated Teff and Treg cells as assayed with flow cytometric immunophenotyping is increased in patients with BD and whether this balance is affected by staging of illness and (b) whether HCMV IgG seropositivity is associated with aberrations in immune subsets thereby aggravating T-cell impairments in BD.
Subjects and Methods
Participants
This study recruited 25 symptomatic remitted BD patients with type I BD and 21 healthy volunteers of both sexes and aged 18 to 65 years. The BD patients attended the Department of Psychiatry, Federal University of Sao Paulo (UNIFESP/EPM), Sao Paulo, Brazil. Controls were recruited by word of mouth from the same catchment area. The diagnosis of BD was made according to DSM-IV-TR diagnostic criteria and using the Structured Clinical Interview for DSM-IV-Axis-I (SCID-I). The severity of depression and mania was assessed using the Hamilton Depression Rating Scale-17 (HAM-D) items and the Young Mania Rating Scale (YMRS), respectively [30, 31]. BD patients were divided into two groups according to the duration of illness using a visual binning method, namely those in an early phase of illness (≤ 4 years, n = 9) and those with a longer duration of illness (≥ 10 years, n = 15). An increased number of episodes (≥ 10) is accompanied by greater functional impairments [32]. The Global Assessment of Functioning (GAF) symptom scale was measured in all subjects [33]. Inclusion criteria for patients were (a) being in a symptomatic remitted state for at least 2 months, (b) not fulfilling any DSM-IV-TR criteria for current mood episodes, (c) a HAM-D rating scale score < 8, (d) a YMRS score < 7, and (e) being under a stable medication treatment regimen for at least 2 months. By inference, all patients had HAM-D and YMRS scores < 7 in the previous weeks, indicating a symptomatic remission [34].
Exclusion criteria for normal controls were any lifetime or current axis-I diagnosis and positive family history for affective disorders and suicide. Exclusion criteria for patients and controls were (a) a current and lifetime treatment with immunomodulatory drugs including glucocorticoids; (b) use of any anti-inflammatory drugs 2 weeks before inclusion in this study; (c) pregnant and lactating women; and (d) medical illness including (auto)immune disorders such as psoriasis, inflammatory bowel disease, chronic kidney disease, rheumatoid arthritis, HIV infection, asthma, and neuroinflammatory disorders including Parkinson’s disease and multiple sclerosis. Some of the BD patients used mood stabilizers (n = 13), lithium (n = 9), antipsychotics (n = 15), antidepressants (n = 5), and benzodiazepines (n = 9), and 17 BP patients used combinations of these drugs. Body mass index (BMI) was computed as body weight (in kg) divided by height (in m2). This study was approved by the local Institutional Research Board, Universidade Federal de São Paulo (no: 57938516.4.0000.5505). All participants provided written informed consent prior to their inclusion. It is known that most symptomatic remitted patients in the inter-episodic period have the capacity to consent [35]. Moreover, all patients included in this study were medically and psychiatrically stable and had adequate levels of understanding with adequate decisional capacity. Therefore, no informed consent is required from the next of kin, guardians, or legally authorized representatives as is required for patients with schizophrenia or dementia.
Assays
Blood Collection and Cell Isolation
After an overnight fast (12 h), 15 mL of blood was sampled between 08:00 and 10:00 a.m. and collected in BD Vacutainer® EDTA tube (10 mL) and BD Vacutainer® SST™ tube (5 mL) (BD Biosciences, Franklin Lakes, NJ, USA). The blood was kept at room temperature (30 min) to allow clotting and to isolate serum. Both tubes were centrifuged at 1100×g (4 °C, 10 min) and the supernatant was aliquoted and kept at − 80 °C. Consequently, we isolated PBMCs by density gradient centrifugation (30 min at 900×g; Ficoll® Paque Plus, GE Healthcare Life Sciences, Pittsburgh, PA, USA). Cells were counted by means of microscopy and viability was confirmed to exceed 95% as assessed from their ability to exclude Trypan Blue (Sigma-Aldrich Corporation, St. Louis, MO, USA).
Immunophenotyping Without Stimulation
To examine specific lymphocyte subsets, 2 × 10 PBMCs were stained directly for 30 min with combinations of anti-CD3 FITC, anti-CD4 APCCy7, anti-CD8 BV510, anti-CD71 PE, anti-CD69 PeCy7, anti-CD25 BV510, and anti-CD152 PECy5 monoclonal antibodies (BD Biosciences). For intracellular FoxP3 staining, we used the Human FoxP3 Buffer Set (BD Biosciences), which includes cell fixation, permeabilization, and staining with the monoclonal antibody anti-FoxP3 Alexa647. Cells were analyzed by flow cytometry immediately after staining. A minimum of 50,000 lymphocytes was identified by size (forward scatter, FSC) and granularity (side scatter, SSC) and they were acquired with a FACSCantoII flow cytometer (BD Biosciences). Isotype controls for all fluorophores were used as negative controls. Data were analyzed using the FlowJo 7.2.5 software (Tree Star Inc., Ashland, OR, USA).
PBMC Stimulation and Activation CD Marker Immunophenotyping
Ninety-six well plates were coated with 5 μg/mL anti-human CD3 antibody (OKT3, eBioscience). PBMCs (1 × 105 cells) were added to each well with anti-human CD28 antibody (CD28.2, eBioscience) in a final concentration of 5 μg/ml. Subsequently, PBMCs were cultivated in RPMI 1640 culture medium supplemented with L-glutamine, 10% fetal bovine serum (Life technologies, California, USA), antimycotics, and antibiotics (Thermo Fischer Scientific, Waltham, MA, USA). The cells could grow for 3 days at 37 °C in a 5% CO2 atmosphere. The experiments comprised a negative control (PBMC without anti-CD3 and anti-CD28 cultivated for 3 days). After 3 days, the same CD markers as described above were counted and stained and analyzed by flow cytometry as described above.
Human Cytomegalovirus Serology
HCMV titers were measured in serum using commercial ELISA kits (EUROIMMUN AG, Luebeck, Germany) according to the manufacturer’s instructions. Anti-HCMV IgG was used at a cutoff value of 20 IU/mL. All subjects included in this study showed negative IgM antibody titers against HCMV. All assays in all subjects were measured in the same run and on the same day to reduce analytical variation.
Statistics
Analysis of contingency tables (χ2 test) was used to check associations between nominal variables and analysis of variance (ANOVA) or the Mann-Whitney U test to check differences in scale variables between diagnostic groups. Binary logistic regression analysis was used to examine the best predictors of BD as dependent variable and controls as the reference group. The odds ratio and 95% confidence intervals (CI) were computed. We used generalized estimating equation (GEE) analysis, repeated measures, to assess the effects of time (unstimulated versus stimulated), diagnosis (e.g., BD versus controls and/or IgG HCMV positive versus negative subjects), and two or three-way interactions between diagnostic groups × positive IgG HCMV antibodies while adjusting for possible effects of age and sex. Protected pairwise post hoc analyses were employed to examine the significant two- or three-way interaction patterns only when the omnibus test was significant. The effects of BMI, smoking, and the drug state of the patients on the frequency of the immune cell populations were examined by entering these data in the same GEE analyses. The false-discovery rate (FDR) procedure was used to control for type-I errors [36]. Tests were two-tailed and a p value of 0.05 was considered for statistical significance. All statistical analyses were performed using IBM SPSS for Windows, version 25 (IBM Corporation, Armonk, NY, USA). A priori computation (G*Power 3.1.9.2) showed that the required sample size given an effect size of 0.22, alpha = 0.05, power = 0.8, and two groups should be n = 44 for a repeated measurement ANOVA with two time points.
The immune subset data were processed in z transformations and we also computed z unit-weighted composite scores reflecting (activation of) T effector (Teff) and Treg (Treg) functions: Teff was computed as z % CD3 + CD4 + CD154+ + z % CD3 + CD4 + CD69+ (%); Treg was computed as z % CD4 + CD25 + FOXP3 + CD152+ + z % CD4 + CD25 + FOXP3 + GARP; and the Teff/Treg ratio computed as zTeff – zTreg.
Results
Sociodemographic Data
Table 2 shows the sociodemographic data of the patients and healthy controls. There were no significant differences in age, sex ratio, years of education, BMI, ethnicity, and marital status between the study groups. There were somewhat more smokers and unemployed individuals in the BD study group. The latter showed marginally increased HAM-D and YMRS scores as compared with controls, while both GAF symptom and function scores were significantly lower in patients than in controls.
Association Between BD and T-Cell Subpopulations
In order to examine the differences in T-cell subsets between BD and controls, both in baseline conditions and after ex vivo polyclonal stimulation, we have performed GEE analysis, which included effects of groups (diagnosis), time (basal versus stimulation), and the (time × group) interaction. The same analyses also included effects of age, sex, IgG HCMV positive versus negative samples (HCMV), and (time × HCMV) and (group × time × HMCV) interactions. We also examined the effects of BMI, smoking, the drug state (mood stabilizers, lithium, antipsychotics, antidepressants, benzodiazepines), and when significant, we adjusted the results for these variables. Table 3 shows the results of those GEE analyses and the effects of time, BD (versus controls), and the (time × diagnosis) interaction. There were significant effects of time on all immune subpopulations. Significant (time × diagnosis) interactions were observed for CD3 + CD4 + CD69+, CD3 + CD8 + CD69+, CD3 + CD4 + CD71+, CD3 + CD8 + CD71+, CD4 + CD25 + FOXP3 + CD152+, and Treg and Teff/Treg ratio. The time X group (at p = 0.0017) and groups (at p = 0.0059) effects remained significant after p-correction for FDR. Consequently, we examined post hoc pairwise comparisons between the groups to explain the interactions. Thus, the basal CD3 + CD4 + CD69+ and CD3 + CD8 + CD69+ proportions were significantly lower in BD while the stimulated proportions did not differ between the groups. There were no inter-group differences in basal CD3 + CD4 + CD71+ and CD3 + CD8 + CD71+ proportions, and the Treg score, but their stimulated values were significantly lower in BD than in controls. The proportion of baseline CD4 + CD25 + FOXP3 + CD152+ was significantly higher in BD than in controls, but their stimulated frequencies were significantly lower in BD than in controls. The stimulated Teff/Treg ratio was significantly higher in BD than in controls while its unstimulated values showed a trend towards lower values in BD.
Table 4, first regression analysis, shows that lowered basal CD3 + CD8 + CD71+ and CD + CD25 + FOXP3+ significantly predicted BD (χ2 = 26.77, df = 2, p < 0.001, Nagelkerke = 0.590) with an accuracy of 84.8%, a sensitivity of 84.0%, and a specificity of 85.7%. The second logistic regression shows that lowered proportions of the stimulated CD3 + CD8 + CD71+ and CD + CD25 + FOXP3 + GARP proportions significantly predicted BD (χ2 = 40.68, df = 2, p < 0.001, Nagelkerke = 0.785) with an accuracy of 89.1%, a sensitivity of 88.0%, and a specificity of 90.5%.
Effects of Background Variables
In the GEE analysis reported in Table 2, we always entered age and sex and did not detect significant effects of these two variables. Also, BMI and smoking did not show any significant effects. Entering the drug state of the patients in GEE analyses showed that the drug state of the patients has a significant effect on CD3 + CD4 + CD69+, CD3 + CD8 + CD69+, and CD3 + CD25 + FOXP3 + CD152+ T cells. The Electronic Supplementary File (ESF) Table 1 shows that, after p-correction for false discovery rate, antidepressants, lithium, mood stabilizers, and benzodiazepines increased the proportions of the CD3 + CD4 + CD69+ T-cell subset. After p-correction for FDR, antidepressants increased the frequency of CD3 + CD8 + CD69+ and CD3 + CD25 + FOXP3 + CD152+ cells, while mood stabilizers, lithium, and benzodiazepines significantly lowered the proportion of the same subset. All data in Table 3 concerning those three subsets were adjusted for those drug effects.
We also examined (using ANOVAs) possible effects of the use of antidepressants, antipsychotics, mood stabilizers, lithium, and benzodiazepines on the HAM-D, YMRS, GAF-S, and GAF-F scores, but could not find effects of any drug on these scale scores, even without p-correction for false discovery rate.
Association Between the Staging of BD and Immune Subsets
ESF Table 2 shows the features of BD patients divided into those with an early versus a later stage of illness. Table 5 shows the results of GEE analyses, which considered the same variables as described in Table 2 except that we now used three subgroups, namely normal controls and the two BD subgroups. We found significant time X group (at p = 0.0039) and group (at p = 0.003) effects in four immune cell subsets (after FDR p-correction). Both the unstimulated and stimulated CD3 + CD4 + CD154+ T-cell proportions were significantly lower in late-stage BP, as compared with controls and early-stage BD. The unstimulated CD3 + CD4 + CD71+ proportions were significantly lower in late-stage BD than in controls. The stimulated frequencies of CD3 + CD8 + CD71+ and CD4 + CD25 + FOXP3 + CD152+ subpopulations were significantly different between the three study groups with the lowest values in late-stage BD.
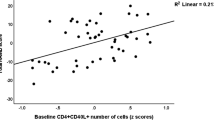
Consequently, we have computed Spearman’s rank-order correlation coefficients between the stimulated T-cell proportions and the number of episodes. Table 6 shows that the proportions of CD3 + CD4 + CD154+, CD3 + CD4 + CD69+, CD3 + CD8 + CD69+, CD3 + CD4 + CD71+, and CD3 + CD8 + CD71+ were significantly and negatively associated with the total number of episodes and number of mania episodes, but not with the number of hypomanic or depressive episodes.
Effects of HCMV IgG Seropositivity
ESF Table 3 shows the differences in the T-cell subsets between subjects with and without positive IgG antibodies to HCMV. These results were derived from the GEE analyses, repeated measures, shown in Table 2 which also considered the effects of HCMV groups and (time × HCMV) groups. ESF Table 3 shows that the stimulated proportions of CD3 + CD4 + CD69+, CD3 + CD8 + CD69+, CD3 + CD4 + FOXP3 + GARP, and Teff/Treg ratio, and the basal proportion of CD3 + CD4 + FOXP3 + GARP were significantly lower in patients with increased IgG to HCMV as compared with those with negative antibody levels. In contrast, the proportions of stimulated CD3 + CD4 + FOFP3 + CD152+ and basal Teff/Treg ratio were higher in subjects who showed increased IgG HCMV antibodies as compared with those without.
ESF Table 4 shows that two (time × diagnostic group × HCMV group) interactions were significant, namely CD4 + CD25 + FOXP3+ and CD4 + CD25 + FOXP3 + GARP. In IgG HCMV-positive subjects, the stimulated CD4 + CD25 + FOXP3+ proportion was significantly higher in BD patients than in controls, whereas in HCMV-negative subjects, there was a trend towards a lowered proportion in BD than in controls. In HCMV-positive subjects, the stimulated CD4 + CD25 + FOXP3 + GARP proportion was significantly lower in BD patients than in controls, whereas in HCMV-negative subjects, there was a trend towards a higher proportion in BD patients than in controls.
Discussion
Aberrations in Baseline Teff/Treg Cell Subsets in BD
The first major finding of this study is that BD is characterized by a lowered baseline frequency of CD3 + CD4 + CD69+, CD3 + CD8 + CD69+, CD3 + CD8 + CD71+, and CD4 + CD25 + FOXP3 T lymphocytes and that the unstimulated frequency of CD4 + CD25 + FOXP3 + CD152+ is increased in BD. These findings indicate that in baseline conditions, there is a disbalance in T lymphocyte functions with a lowered expression of early (CD69+) and later (CD71+ and CD25+) [15] activation markers, while the proportion of activated CD152+ Treg cells is increased. The comparison of these data with previous results is limited because only a few papers examined CD markers in mood disorders [22,23,24,25]. Early findings in the acute phase of a major depressive episode and melancholia showed increased expression of T lymphocyte activation markers including CD4 + CD45RA (T memory), CD25+, and HLA-DR+ (very late activation marker) cells [37, 38]. Moreover, both unipolar depression and melancholia are qualitatively distinct classes (using machine learning techniques) with respect to those T-cell activation markers as compared with minor depression and healthy controls [38, 39].
The acute phases of BD, both depression and mania, are also accompanied by signs of T-cell activation as indicated by increased levels of sIL-2R [17] and by indicants of M1, Th-1, Th-2, and Treg activation [8]. Nevertheless, in the present study, we included BD type 1 patients who were in the symptomatic remitted phase of the illness. As such, it appears that the acute phase of BD is accompanied by T-cell activation, whereas symptomatic remission is characterized by inhibition of proliferation (CD71+) and immune induction (CD69+) coupled with activation of some Treg phenotypes.
Aberrations in Stimulated Teff/Treg Cell Subsets in BD
The second major finding of this study is that there are highly significant deficits in the expression of polyclonal-stimulated CD152+ and GARP+ Treg cells in BD patients coupled with a depletion of CD71+ bearing CD4+ and CD8+ cells. In the present study, T lymphocytes were activated with CD3/CD28 antibodies and, therefore, the results reflect the in vivo immune response following immune injury. As such, our results suggest that following infections or other injuries, BD patients will show marked impairments in both T-cell proliferation and Treg functions as compared with controls.
In the 1980s, there were some studies showing that major depression is accompanied by lowered mitogen-induced T lymphocyte proliferative responses [40], although, to the best of our knowledge, no such results were reported in symptomatic remitted BD patients. Our results may suggest that deficits in polyclonal-stimulated lymphoproliferative responses could be explained by deficits in the uptake of the iron-transferrin complex and transport of iron into proliferating cells [15]. It is noteworthy that plasma levels of sTfR are significantly increased during the acute phase of BD, either in depression or mania [16, 17]. Increased plasma levels of sTfR not only reflect alterations in iron status, but also immune activation including IL-2-related mechanisms [41]. Thus, it appears that the increased shedding of TfR during the acute phase of BD [16] is accompanied by longer-lasting deficits in the expression of surface CD71+ and, therefore, by deficits in T-cell proliferation. Since CD71-related mechanisms positively mediate T and B cell functions, deficits in CD71 surface expression may at least in part underpin the impairments in T lymphocyte proliferation.
Consequences of Aberrations in Treg Cell Subsets in BD
Treg cells play a key role in the resolution of inflammation and immune homeostasis, thereby preventing excessive inflammation and autoimmune responses, while deficits in Treg functions may impair healing and tissue remodeling [18, 19, 21]. Treg cells mediate and regulate regeneration via different mechanisms including inhibition of M1 macrophages and increased Teff activities [42]. Moreover, Treg cells play a key role in tissue repair by interacting with neutrophils and macrophages and they are additionally involved in repair mechanisms in the central nervous system by promoting remyelination and differentiation of oligodendrocyte progenitor cells [43]. Treg cells have also neuroprotective effects and depletion of Treg cells may induce neurocognitive deficits [44] and may be accompanied by increased infiltration of T cells into the brain as well as reactive astrogliosis [44].
Consequences of Abnormal CIRS Signaling in BD
Our unstimulated flow cytometric results may indicate that the symptomatic remission of BD is characterized by increased CIRS signaling and that, consequently, IRS signaling pathways are more adequately suppressed. Moreover, it should be underscored that the symptomatic remitted phases of BD type 1 and a major depressive episode are characterized by increased neurotoxicity due to oxidative and nitrosative stress with hypernitrosylation and increased levels of malondialdehyde and advanced oxidation protein products, and increased bacterial translocation [45, 46]. Therefore, it is safe to posit that the symptomatic remitted phase of BD is accompanied by enhanced CIRS signaling, which attempts to repair the damage by nitro-oxidative and immune-inflammatory stressors.
Our stimulated flow cytometric results reveal that, following immune injuries, patients with BD will exhibit a strong suppression of regulatory CIRS signaling leading to greater activation of IRS signaling through M1, Th-1, Th-2, and Th-17-like cytokine production and Teff cell differentiation. Such mechanisms could have dire effects during the acute phase of BD, because lowered Treg activities may lead to less resilience against host-commensal interactions, enhanced IRS and autoimmune responses, metabolic inflammation, and increased damage by oxidative and nitrosative stress pathways [8, 18, 19, 21, 42, 47, 48]. As such, the deficits in Treg functions in BD may play a key role in the IO&NS pathophysiology of BD.
Associations with Staging of Illness
The third major finding of this study is that staging of illness, either duration of illness or number of episodes, has a highly significant suppressant effect on the expression of activated Teff (CD154+ and CD69+) and Treg (CD152+) surface molecules, as well as the proportion of CD71+ cells, indicating that staging of illness is accompanied by deficits in Treg and Teff functions and lymphoproliferative mechanisms. As described in the introduction, increased staging in BD is associated with increased sTNFR80, sIL-1RA, and TBARS levels, and an index which comprises superoxide dismutase, lipid peroxidation, nitric oxide metabolites, and advanced oxidation protein products (AOPP) and lowered levels of paraoxonase 1 (PON1) enzymatic activity [7, 11]. Other results show that immune-inflammatory responses are more pronounced in the later stages of the illness [12, 14]. Furthermore, in major depression, the number of prior depressive episodes is accompanied by increased levels of plasma IL-1, sIL-1RA, IL-6, TNF-α, and neopterin [49,50,51], suggesting that staging of illness is characterized by M1 and Th-1 activation.
Previously, the relationship between staging and immune pathways was explained [49, 50] by the knowledge that pro-inflammatory signals including IFN-γ and LPS may modulate or even induce sensitization in the immune system [52,53,54]. While this is a plausible mechanism, the results of the present study indicate that also staging-associated deficits in Treg functions underpin the exaggerated IO&NS responses during the acute phase of the illness. Nevertheless, in late-stage BD, there are profound deficits in the stimulated CD71+ expression indicating that the CIRS, as well as lymphoproliferative responses, are grossly compromised in BD possibly leading to dire consequences when facing immune injuries.
Effects of Manic Versus Depressive Episodes on Teff/Treg Cell Subsets
It is also important to note that manic, but not hypomanic or depressive, episodes affect Teff and Treg surface markers. This is interesting because there are highly significant differences between BD type 1 versus type 2 in IO&NS pathways [45, 46]. Furthermore, patients with type 1 BD show higher IgA mediated responses to Gram-negative bacteria as compared with major depressed subjects [55]. Therefore, one hypothesis is that these pathways may play a role in the downregulation of Teff and Treg surface markers. Another possibility is that increased T-cell exhaustion coupled with increased induction of cell death pathways including TIM-3 and PD-1 expression [56] is involved, for example, following repeated activation with increased levels of pro-inflammatory cytokines or chronic antigen exposure (e.g., LPS from Gram-negative bacteria).
Effects of HCMV Seropositivity on Teff/Treg Cell Subsets
The fourth major finding of this study is that Teff and Treg surface markers were modified by HCMV seropositivity. We found that IgG antibodies to HCMV were somewhat albeit significantly higher in BD patients than in controls, findings that agree with those of Prossin et al. [27]. Infected persons will continuously harbor HCMV, which will coexist lifelong with the host through latency or chronic virus infection [28, 29]. Nevertheless, all patients included in this study showed negative IgM responses to HCMV suggesting that patients with increased IgG to HCMV underwent past exposure and show HCMV latency rather than active or reactivated infections. Those subjects maintain large proportions of HCMV T cells while T cell–related surveillance plays a key role in latency [28, 29]. Likewise, persistent HCVM infection may alter the expression of different T-cell surface molecules as reviewed in the “Introduction” [28, 29]. However, in the current study, we detected that HCMV seropositivity is accompanied by a lowered stimulated expression of the CD69+ marker on CD4+ and CD8+ cells and an increased frequency of CD4 + CD25 + FOXP3 + CD152+ cells, suggesting that HCMV latency may interfere with the balance between the Treg and Teff activation ratio. We also detected that HCMV seropositivity may aggravate the depleted proportion of CD4 + CD25 + FOXP3 + GARP Treg cells in BD. GARP or LRRC32, a leucine-rich repeat molecule that is co-expressed with latent TGF-β in platelets and activated Treg membrane surfaces, is critical for tethering TGF-β to the cell surface [57]. Thus, HCMV seropositivity and BD interact to induce a lowered expression of the GARP surface marker on activated Treg cells, suggesting that the combination of both conditions is accompanied by a more profound loss of inhibitory signals mediated by TGF-β [18, 57]. As such, HCMV latency could contribute to an immune-risk phenotype associated with BD.
Effects of Psychotropic Drugs on Teff/Treg Cell Subsets
The current study also showed that psychotropic drugs impact selected T-cell phenotypes, namely CD69+ bearing CD4+ and CD8+ T cells and CD152+ activated Treg cells. Thus, all psychotropic drugs significantly enhanced expression of CD69+ surface molecule, while antidepressants increase the frequency of CD3 + CD25 + FOXP3 + CD152+ cells. Lithium, antipsychotics, and benzodiazepines, on the other hand, attenuated the frequency of the CD152+ Treg cells and, therefore, these psychotropic drugs may further inhibit Treg functions in BD patients. Previously, it was found that lithium may enhance the stimulated production of TNF-α and IFN-γ, and sIL-1RA and IL-10 mediated Treg activities [58]. On the other hand, antidepressants could have more beneficial effects because they appear to enhance the proportion of CD152+ bearing Treg cells, which are known to downregulate immune responses [19, 59]. Previously, it was shown that antidepressants of different classes have immune-regulatory effects by increasing the production of IL-10 [8]. In this respect, it is interesting to note that the continued use of benzodiazepines, lithium, and mood stabilizers (but not antidepressants) in the inter-episodic period may aggravate some aspects of immune-inflammatory responses (activated Teff and lowered Treg functions) following immune injury. As such, these drugs including benzodiazepines could maybe contribute to immune-inflammatory responses upon immune injury. Nevertheless, the results of the current study are based on associations between the drug state and baseline CD markers or ex vivo stimulated CD markers and, therefore, do not necessarily reflect the in vivo situation.
Limitations
The results of the present study should be discussed with respect to its limitations. First, it would have been even more interesting if we had included type II BD patients. Nevertheless, we did not combine type I and type II because the IO&NS pathophysiology is quite different between both groups [45, 46, 55]. There were also differences in smoking and employment between patients and controls. Nevertheless, high rates of unemployment and work loss are features of BD [60] and all results were adjusted for possible effects of smoking, which did not affect the immune variables.
Another limitation is that some patients used psychotropic drugs, including benzodiazepines, which may indicate the fragile state of some patients and that these drugs could interfere with immune functions. Nevertheless, all immune data in this study were adjusted for the effects of psychotropic drugs.
Integration of the Current Findings with the IRS-CIRS Theory of BD
Figure 1 displays the results of the current study and their interpretation with respect to the IRS-CIRS, neurotoxicity, and staging theories of BD [1, 7, 8]. First, the baseline condition in our symptomatic remitted BD patients is characterized by increased CIRS and lowered IRS activities, suggesting that Treg cells participate in the repair of the damage induced by I&ONS pathways, which are all activated in the acute phases of illness [8]. Second, following immune injuries (including infections, severe psychosocial stress), BD patients may show suppressed CIRS functions, which may further aggravate the activated IO&NS pathways in the acute phase of BD [7, 8]. Third, in BD, staging of illness is accompanied by attenuated Treg and Teff cell subsets, suggesting that staging is accompanied by a progressive increased vulnerability to develop inflammatory and compromised lymphoproliferative responses. Fourth, HCMV positivity may further deplete CIRS functions indicating that BD patients with longer duration of illness, more episodes and HCMV latency are prone to develop IRS responses [8]. Suppressed CIRS pathways may drive increased production of neurotoxic cytokines/chemokines including those produced by M1 (IL-1, IL-6, TNF), Th-1 (IFN, IL-22), and Th-2 (IL-4, CCL11) cells and, and may induce O&NS damage to proteins and lipids [7, 8, 45, 46, 55]. Consequently, these neurotoxic products may lead to a breakdown of the blood-brain barrier and induce mild encephalitis, parainflammation, or neuroprogression [7, 8, 61] as well as neurotoxic effects to affective and cognitive circuits [62] in the brain [7, 8, 63], a phenomenon we propose to label “neuroaffective toxicity.” Previously, we constructed nomethetic networks based on early lifetime trauma, number of episodes and suicidal attempts, neuro-oxidative pathways, and neurocognitive impairments which together contribute to a novel staging index of BD [7]. Therefore, future research should examine how the IRS/CIRS markers defined in the current study affect this nomothetic staging network. Our studies add to the reification of the staging concept of BD [64].
Summary of the results of the current study and their interpretations with respect to the immune-inflammatory responses system (IRS)–compensatory immune-regulatory system (CIRS) and neurotoxicity theories of bipolar disorder (BD). HCMV: human cytomegalovirus, Treg: T regulatory, M1: M1 macrophage, Th: T helper, O&NS: oxidative and nitrosative stress
Conclusions
In conclusion, the symptomatic remitted phase of BD is characterized by a suppression of early activation markers and proliferative capacity of Teff cells coupled with activation of Treg cells. Polyclonal stimulation shows that Treg functions will be suppressed in BD patients following immune injuries probably leading to lowered resilience against host-commensal interactions, (auto)immune responses, and nitro-oxidative stress. Moreover, the staging of illness, either duration of illness (≥ 10 years) or an increasing number of manic episodes, is accompanied by impairments in Teff and Treg cells. The presence of latent HCMV infections may contribute to the pathophysiology of BD by depleting the frequency of activated GARP bearing Treg cells. These multiple disorders in adaptive immunity in BD may play a role in the pathophysiology of this disorder through changes in the production of IRS and CIRS cytokines or direct cell-cell interactions within the CNS.
Authorships
All the contributing authors have participated in the manuscript. All authors contributed to the interpretation of the data and writing of the manuscript. All authors approved the final version of the manuscript.
References
Berk M, Brnabic A, Dodd S, Kelin K, Tohen M, Malhi GS, Berk L, Conus P et al (2011) Does stage of illness impact treatment response in bipolar disorder? Empirical treatment data and their implication for the staging model and early intervention. Bipolar Disord 13(1):87–98
Scott J, Leboyer M, Hickie I, Berk M, Kapczinski F, Frank E, Kupfer D, McGorry P (2013) Clinical staging in psychiatry: a cross-cutting model of diagnosis with heuristic and practical value. Br J Psychiatry 202(4):243–245
Moylan S, Maes M, Wray NR, Berk M (2013) The neuroprogressive nature of major depressive disorder: pathways to disease evolution and resistance, and therapeutic implications. Mol Psychiatry 18(5):595–606
Muneer A (2016) Staging models in bipolar disorder: a systematic review of the literature. Clin Psychopharmacol Neurosci 31(2):117–130
Mwangi B, Wu MJ, Cao B, Passos IC, Lavagnino L, Keser Z, Zunta-Soares GB, Hasan KM et al (2016) Individualized prediction and clinical staging of bipolar disorders using neuroanatomical biomarkers. Biol Psychiatry Cogn Neurosci Neuroimaging 1(2):186–194
Maes M, Congio A, Moraes JB, Bonifacio KL, Barbosa DS, Vargas HO, Morris G, Puri BK et al (2018) Early life trauma predicts affective phenomenology and the effects are partly mediated by staging coupled with lowered lipid-associated antioxidant defences. Biomol Concepts 9(1):115–130
Maes M, Moraes JB, Congio A, Bonifacio KL, Barbosa DS, Vargas HO, Michelin AP, Carvalho AF et al (2019) Development of a novel staging model for affective disorders using partial least squares bootstrapping: effects of lipid-associated antioxidant defenses and neuro-oxidative stress. Mol Neurobiol 56(9):6626–6644
Maes M, Carvalho AF (2018) The compensatory immune-regulatory reflex system (CIRS) in depression and bipolar disorder. Mol Neurobiol 55(12):8885–8903
Modabbernia A, Taslimi S, Brietzke E, Ashrafi M (2013) Cytokine alterations in bipolar disorder: a meta-analysis of 30 studies. Biol Psychiatry 74(1):15–25
Brunoni AR, Supasitthumrong T, Teixeira AL, Vieira EL, Gattaz WF, Benseñor IM, Lotufo PA, Lafer B et al (2019) Differences in the immune-inflammatory profiles of unipolar and bipolar depression. J Affect Disord 262:8–15
Sowa-Kućma M, Styczeń K, Siwek M, Misztak P, Nowak RJ, Dudek D, Rybakowski JK, Nowak G et al (2018) Are there differences in lipid peroxidation and immune biomarkers between major depression and bipolar disorder: effects of melancholia, atypical depression, severity of illness, episode number, suicidal ideation and prior suicide attempts. Prog Neuro-Psychopharmacol Biol Psychiatry 81:372–383
Brietzke E, Kapczinski F (2008) TNF-alpha as a molecular target in bipolar disorder. Prog Neuro-Psychopharmacol Biol Psychiatry 32:1355–1361
Kauer-Sant'Anna M, Kapczinski F, Andreazza AC, Bond DJ, Lam RW, Young LT, Yatham LN (2009) Brain-derived neurotrophic factor and inflammatory markers in patients with early- vs. late-stage bipolar disorder. Int J Neuropsychopharmacol 12:447–458
Kapczinski F, Dias VV, Kauer-Sant'Anna M, Brietzke E, Vazquez GH, Vieta E, Berk M (2009) The potential use of biomarkers as an adjunctive tool for staging bipolar disorder. Prog Neuro-Psychopharmacol Biol Psychiatry 33:1366–1371
BD (2019) Human and Mouse CD Marker Handbook. http://static.bdbiosciences.com/documents/cd_marker_handbook.pdf?_ga=2.85815504.811977153.1575184397-413126189.1546826603. As accessed 1 December 2019
Maes M, Bosmans E, Calabrese J, Smith R, Meltzer HY (1995) Interleukin-2 and interleukin-6 in schizophrenia and mania: effects of neuroleptics and mood stabilizers. J Psychiatr Res 29(2):141–152
Maes M, Meltzer HY, Bosmans E, Bergmans R, Vandoolaeghe E, Ranjan R, Desnyder R (1995) Increased plasma concentrations of interleukin-6, soluble interleukin-6, soluble interleukin-2 and transferrin receptor in major depression. J Affect Disord 34(4):301–309
Sun L, Jin H, Li H (2016) GARP: a surface molecule of regulatory T cells that is involved in the regulatory function and TGF-β releasing. Oncotarget 7(27):42826–42836
Kolar P, Knieke K, Hegel JK, Quandt D, Burmester GR, Hoff H, Brunner-Weinzierl MC (2009) CTLA-4 (CD152) controls homeostasis and suppressive capacity of regulatory T cells in mice. Arthritis Rheum 60(1):123–132
Jin H, Sun L, Tang L, Yu W, Li H (2017) Expression of GARP is increased in tumor-infiltrating regulatory t cells and is correlated to clinicopathology of lung cancer patients. Front Immunol 14(8):138
Zhao H, Liao X, Kang Y (2017) Tregs: where we are and what comes next? Front Immunol 8:1578
Breunis MN, Kupka RW, Nolen WA, Suppes T, Denicoff KD, Leverich GS, Post RM, Drexhage HA (2003) High numbers of circulating activated T cells and raised levels of serum IL-2 receptor in bipolar disorder. Biol Psychiatry 53:157–165
Barbosa IG, Rocha NP, Assis F, Vieira ÉL, Soares JC, Bauer ME, Teixeira AL (2014) Monocyte and lymphocyte activation in bipolar disorder: a new piece in the puzzle of immune dysfunction in mood disorders. Int J Neuropsychopharmacol 18(1):pyu021
do Prado CH, Rizzo LB, Wieck A, Lopes RP, Teixeira AL, Grassi-Oliveira R, Bauer ME (2013) Reduced regulatory T cells are associated with higher levels of Th1/TH17 cytokines and activated MAPK in type 1 bipolar disorder. Psychoneuroendocrinology 38:667–676
Drexhage RC, Hoogenboezem TH, Versnel MA, Berghout A, Nolen WA, Drexhage HA (2011) The activation of monocyte and T cell networks in patients with bipolar disorder. Brain Behav Immun 25(6):1206–1213
Debnath M, Raison CL, Maes M, Berk M (2019) Role of the T cell network in psychiatric disorders. In: Merk M, Leboyer M, Sommer I (eds) Immuno-Psychiatry. Springer, Berlin In press
Prossin AR, Yolken RH, Kamali M, Heitzeg MM, Kaplow JB, Coryell WH, McInnis MG (2015) Cytomegalovirus antibody elevation in bipolar disorder: relation to elevated mood states. Neural Plast 2015:939780
Goodrum F, Caviness K, Zagallo P (2012) Human cytomegalovirus persistence. Cell Microbiol 14(5):644–655
van der Heiden M, van Zelm MC, Bartol SJW, de Rond LGH, Berbers GAM, Boots AMH, Buisman AM (2016) Differential effects of cytomegalovirus carriage on the immune phenotype of middle-aged males and females. Sci Rep 6:26892
Hamilton M (1960) A rating scale for depression. J Neurol Neurosurg Psychiatry 23:56–62
Young RC, Biggs JT, Ziegler VE, Meyer DA (1978) A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry 133:429–435
Di Marzo S, Giordano A, Pacchiarotti I, Colom F, Sánchez-Moreno J, Vieta E (2006) The impact of the number of episodes on the outcome of bipolar disorder. Eur J Psychiatry 20:21–28
American Psychiatric Association (1994) Diagnostic and statistical manual of mental disorders, Fourth Edition, Washington, DC, pp 25–35.
Tohen M, Frank E, Bowden CL, Colom F, Ghaemi SN, Yatham LN, Malhi GS, Calabrese JR et al (2009) The International Society for Bipolar Disorders (ISBD) Task Force report on the nomenclature of course and outcome in bipolar disorders. Bipolar Disord 11(5):453–473
Misra S, Rosenstein D, Socherman R, Ganzini L (2010) Bipolar mania, and capacity to consent: recommendations for investigators and IRBs. IRB 32(1):7–15
Benjamini Y, Hochberg Y (1995) Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B Methodol 57:289–300
Maes M, Bosmans E, Suy E, Vandervorst C, De Jonckheere C, Raus J (1990) Immune disturbances during major depression: upregulated expression of interleukin-2 receptors. Neuropsychobiology 24(3):115–120
Maes M, Lambrechts J, Bosmans E, Jacobs J, Suy E, Vandervorst C, de Jonckheere C, Minner B et al (1992) Evidence for a systemic immune activation during depression: results of leukocyte enumeration by flow cytometry in conjunction with monoclonal antibody staining. Psychol Med 22(1):45–53
Maes M, Stevens WJ, Declerck LS, Bridts CH, Peeters D, Schotte C, Cosyns P (1993) Significantly increased expression of T-cell activation markers (interleukin -2 and HLA-DR) in depression: further evidence for an inflammatory process during that illness. Prog Neuro-Psychopharmacol Biol Psychiatry 17(2):241–255
Schleifer SJ, Keller SE, Meyerson AT, Raskin MJ, Davis KL, Stein M (1984) Lymphocyte function in major depressive disorder. Arch Gen Psychiatry 41(5):484–486
Maes M, Bosmans E, Scharpé S, Hendriks D, Cooremans W, Neels H, De Meyer F, D'Hondt P et al (1997) Components of biological variation in serum soluble transferrin receptor: relationships to serum iron, transferrin and ferritin concentrations, and immune and haematological variables. Scand J Clin Lab Invest 57(1):31–41
Li J, Tan J, Martino MM, Lui KO (2018) Regulatory T-cells: potential regulator of tissue repair and regeneration. Front Immunol 9:585
Baek H, Ye M, Kang GH, Lee C, Lee G, Choi DB, Jung J, Kim H et al (2016) Neuroprotective effects of CD4 + CD25 + Foxp3+ regulatory T cells in a 3xTg-AD Alzheimer’s disease model. Oncotarget 7(43):69347–69357
Krämer TJ, Hack N, Brühl TJ, Menzel L, Hummel R, Griemert EV, Klein M, Thal SC et al (2019) Depletion of regulatory T cells increases T cell brain infiltration, reactive astrogliosis, and interferon-γ gene expression in acute experimental traumatic brain injury. J Neuroinflammation 16(1):163
Maes M, Landucci Bonifacio K, Morelli NR, Vargas HO, Barbosa DS, Carvalho AF, Nunes SOV (2019) Major differences in neurooxidative and neuronitrosative stress pathways between major depressive disorder and types I and II bipolar disorder. Mol Neurobiol 56(1):141–156
Maes M, Simeonova D, Stoyanov D, Leunis JC (2019) Upregulation of the nitrosylome in bipolar disorder type 1 (BP1) and major depression, but not BP2: increased IgM antibodies to nitrosylated conjugates are associated with indicants of leaky gut. Nitric Oxide 91:67–76
Walker LS, Sansom DM (2015) Confusing signals: recent progress in CTLA-4 biology. Trends Immunol 36(2):63–70
Peixoto TV, Carrasco S, Botte DAC, Catanozi S, Parra ER, Lima TM, Ugriumov N, Soriano FG et al (2019) CD4(+)CD69(+) T cells and CD4(+)CD25(+)FoxP3(+) Treg cells imbalance in peripheral blood, spleen and peritoneal lavage from pristane-induced systemic lupus erythematosus (SLE) mice. Adv Rheumatol 59(1):30
Maes M, Ombelet W, De Jongh R, Kenis G, Bosmans E (2001) The inflammatory response following delivery is amplified in women who previously suffered from major depression, suggesting that major depression is accompanied by a sensitization of the inflammatory response system. J Affect Disord 63(1-3):85–92
Maes M, Mihaylova I, Kubera M, Ringel K (2012) Activation of cell-mediated immunity in depression: association with inflammation, melancholia, clinical staging and the fatigue and somatic symptom cluster of depression. Prog Neuro-Psychopharmacol Biol Psychiatry 36(1):169–175
Celik C, Erdem M, Cayci T, Ozdemir B, Ozgur Akgul E, Kurt YG, Yaman H, Isintas M et al (2010) The association between serum levels of neopterin and number of depressive episodes of major depression. Prog Neuro-Psychopharmacol Biol Psychiatry 34(2):372–375
Longo DL, Duffey PL, Kopp WC, Heyes MP, Alvord WG, Sharfman WH, Schmidt PJ, Rubinow DR et al (1999) Conditioned immune response to interferon-gamma in humans. Clin Immunol 90:173–181
Blanque R, Meakin C, Millet S, Gardner CR (1998) Selective enhancement of LPS-induced serum TNF-alpha production by carrageenan pretreatment in mice. Gen Pharmacol 31:301–306
Kawasaki Y, Zhang L, Cheng JK, Ji RR (2008) Cytokine mechanisms of central sensitization: distinct and overlapping role of interleukin-1beta, interleukin-6, and tumor necrosis factor-alpha in regulating synaptic and neuronal activity in the superficial spinal cord. J Neurosci 28(20):5189–5194
Simeonova D, Stoyanov D, Leunis J-C, Carvalho AF, Kubera M, Murdjeva M, Maes M (2019, 2019) Increased serum immunoglobulin responses to gut commensal Gram-negative bacteria in unipolar major depression and bipolar disorder type 1, especially when melancholia is present. Neurotox Res. https://doi.org/10.1007/s12640-019-00126-7
Xia Q, Wei L, Zhang Y, Sheng J, Wu W, Zhang Y (2018) Immune checkpoint receptors Tim-3 and PD-1 regulate monocyte and T lymphocyte function in septic patients. Mediat Inflamm 2018:1632902
Tran DQ, Andersson J, Wang R, Ramsey H, Unutmaz D, Shevach EM (2009) GARP (LRRC32) is essential for the surface expression of latent TGF-beta on platelets and activated FOXP3+ regulatory T cells. Proc Natl Acad Sci U S A 106(32):13445–13450
Maes M, Song C, Lin AH, Pioli R, Kenis G, Kubera M, Bosmans E (1999) In vitro immunoregulatory effects of lithium in healthy volunteers. Psychopharmacology 143(4):401–407
Hegel JK, Knieke K, Kolar P, Reiner SL, Brunner-Weinzierl MC (2009) CD152 (CTLA-4) regulates effector functions of CD8+ T lymphocytes by repressing Eomesodermin. Eur J Immunol 39(3):883–893
Bowden CL (2005) Bipolar disorder and work loss. Am J Manag Care 11(3 Suppl):S91–S94
Bechter K, Brown D, Najjar S (2019) Editorial: Recent advances in psychiatry from psycho-neuro-immunology research: autoimmune encephalitis, autoimmune encephalopathy, and mild encephalitis. Front Psychiatry 10:169
Duncan S, Barrett LF (2007) Affect is a form of cognition: a neurobiological analysis. Cognit Emot 21(6):1184–1211
Leonard B, Maes M (2012) Mechanistic explanations how cell-mediated immune activation, inflammation and oxidative and nitrosative stress pathways and their sequels and concomitants play a role in the pathophysiology of unipolar depression. Neurosci Biobehav Rev 36(2):764–785
Stoyanov D (2020) The reification of diagnosis in psychiatry. Neurotox Res 37(3):772–774. https://doi.org/10.1007/s12640-019-00139-2
Funding
This study was funded by an L’Oreal For Women in Science Award 2015, CAPES, and CNPq.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
This study was approved by the local Institutional Research Board, Universidade Federal de São Paulo (no: 57938516.4.0000.5505). All participants provided written informed consent prior to their inclusion.
Conflict of Interest
The authors have no conflict of interest with any commercial or other association in connection with the submitted article. Dr. Brietzke has received research funding from FAPESP, CNPq, CAPES, SEAMO, and Queen’s University and honoraria as a speaker/advisory board member from Daiichi-Sankyo and Otsuka, not related to this study. Dr. Noto has received honoraria as a speaker/advisory board member from Ache, Daiichi-Sankyo, and Janssen.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 22 kb).
Rights and permissions
About this article
Cite this article
Maes, M., Nani, J.V., Noto, C. et al. Impairments in Peripheral Blood T Effector and T Regulatory Lymphocytes in Bipolar Disorder Are Associated with Staging of Illness and Anti-cytomegalovirus IgG Levels. Mol Neurobiol 58, 229–242 (2021). https://doi.org/10.1007/s12035-020-02110-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-020-02110-1