Abstract
Lipoprotein receptor transport across the blood-brain barrier (BBB) mediates beta-amyloid (Aβ) accumulation in the brain and may be a contributing factor in Alzheimer’s disease (AD) pathogenesis. Lipoprotein receptors are susceptible to proteolytic shedding at the cell surface, which precludes the endocytic transport of ligands. A ligand that closely interacts with the lipoprotein receptors is apolipoprotein E (apoE), which exists as three isoforms (apoE2, apoE3, apoE4). Our prior work showed an inverse relationship between lipoprotein receptor shedding and Aβ transport across the BBB, which was apoE-isoform dependent. To interrogate this further, the current studies investigated an enzyme implicated in lipoprotein receptor shedding, matrix metalloproteinase 9 (MMP9). Treatment with MMP9 dose-dependently elevated lipoprotein receptor shedding in brain endothelial cells and freshly isolated mouse cerebrovessels. Furthermore, treatment with a MMP9 inhibitor (SB-3CT) mitigated Aβ-induced lipoprotein receptor shedding in brain endothelial cells and the brains of apoE4 animals. In terms of BBB transit, SB-3CT treatment increased the transport of Aβ across an in vitro model of the BBB. In vivo, administration of SB-3CT to apoE4 animals significantly enhanced Aβ clearance from the brain to the periphery following intracranial administration of Aβ. The current studies show that MMP9 impacts lipoprotein receptor shedding and Aβ transit across the BBB, in an apoE isoform-specific manner. In total, MMP9 inhibition can facilitate Aβ clearance across the BBB, which could be an effective approach to lowering Aβ levels in the brain and mitigating the AD phenotype, particularly in subjects carrying the apoE4 allele.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alzheimer’s disease (AD) is a neurodegenerative process characterized by a progressive deterioration in memory, executive function, and behavior [1]. One of the key pathological hallmarks of AD is the deposition of beta-amyloid proteins (Aβ) in the brain and cerebrovasculature [2]. Prior evidence suggests the excessive accumulation of Aβ in AD is the result of impaired Aβ clearance from the brain [3,4,5], including diminished Aβ transport at the blood-brain barrier (BBB). It has been reported that Aβ clearance across the BBB is reduced by approximately 30% in AD patients [6]. Two BBB receptors that contribute to the brain-to-blood elimination of Aβ are the low-density lipoprotein receptor (LDLR) and the LDLR-related protein 1 (LRP1) [7, 8]. Proteolytic cleavage of these receptors at the cell surface (i.e., ectodomain shedding) generates a soluble receptor, which retains the capacity to bind ligands, but loses the ability to internalize or transport ligands intracellularly [9, 10]. One of the more closely associated ligands of these lipoprotein receptors is apolipoprotein E (apoE), which exists as three isoforms in humans (apoE2, apoE3, and apoE4). Numerous studies have acknowledged that possession of the apoE4 allele represents the strongest genetic risk factor for late-onset AD [11]. Our prior studies [12] and the work of others indicate Aβ clearance from the brain is differentially regulated by the type of apoE isoform expressed [3]. More recently, we reported an isoform-specific effect of apoE on lipoprotein receptor shedding (LRP1 and LDLR) with a rank order of apoE4 > apoE3 > apoE2 [13]. Collectively, these findings showed an inverse relationship between lipoprotein receptor shedding in the brain and Aβ elimination across the BBB, one that is apoE-genotype specific [13].
While our prior studies observed a correlation between lipoprotein receptor shedding and Aβ removal from the brain, the factors driving lipoprotein receptor proteolysis have yet to be fully explored. One group of protease enzymes implicated in receptor shedding is the matrix metalloproteinases (MMPs) [14]. MMP9, in particular, has been identified as a ligand for LRP1 [15, 16], and prior studies have suggested a role for MMP9 in the shedding of LRP1 [17, 18]. In terms of apoE, there has been a little investigation into the relationship between MMP9 and apoE. Recent work observed that apoE2 and apoE3, but not apoE4, control the levels of certain inflammatory molecules that activate MMP9 [19, 20], and these effects were mediated through LRP1 signaling [19, 21, 22]. Given the interactions between MMP9 and the lipoprotein receptors, the present studies investigated the role of MMP9 in lipoprotein receptor shedding and the resulting impact on Aβ elimination across the BBB. Moreover, as our prior work has shown apoE to be a strong mediator of these processes [12, 13], we also examined MMP9 function in the context of apoE genotype to further understand the influence of apoE on the elimination of Aβ from the brain.
Materials and Methods
Materials
Primary human brain microvascular endothelial cells (HBMEC) and associated culture reagents were purchased from Sciencell Research Laboratories (Carlsbad, CA, USA). Fibronectin solution, marimastat, and SB-3CT were purchased from MilliporeSigma (St. Louis, MO, USA). Fluorescein-labeled Aβ(1–42) was purchased from rPeptide (Bogart, GA, USA). Recombinant human MMP9 was purchased from ProSpec Bio (East Brunswick, NJ, USA). Lucifer yellow dextran, unlabeled human Aβ(1–42), and the human Aβ(1–42) and human MMP9 enzyme-linked immunosorbent assays (ELISAs) were purchased from Invitrogen Corp. (Carlsbad, CA, USA). The ELISA kits for LRP1 and LDLR were purchased from Cedarlane Labs (Burlington, NC, USA). The halt enzyme inhibitor cocktails, the bicinchoninic acid (BCA) protein assay, and the lactate dehydrogenase (LDH) cytotoxicity assay kit were purchased from Thermo Scientific (Waltham, MA, USA). The 24-well membrane inserts (translucent, 0.4 μm pore) and 24-well companion plates were purchased from Fisher Scientific (St. Louis, MO, USA). The stereotaxic apparatus and large probe holder were purchased from Stoelting Co. (Wood Dale, IL, USA).
Animals
All animals (male and female mice, 6 months of age) were purchased from Taconic Farms (Germantown, NY, USA) and allowed to adapt to the vivarium for 2 weeks prior to any experimental procedures. The apoE-targeted replacement (apoE-TR) mice were created by gene targeting and carried one of the three human alleles (APOE2, APOE3, or APOE4) in place of the endogenous murine apoE gene [23], and all mice were on a C57BL/6 background. These mice retain the endogenous regulatory sequences required for apoE production and express the human apoE protein at physiological levels. Mice were housed under standard laboratory conditions (23 ± 1 °C, 50 ± 5% humidity, and a 12-h light/dark cycle) with free access to food and water throughout the study. All experiments using animals were performed under protocols approved by the Institutional Animal Care and Use Committee of the Roskamp Institute.
Peptide Preparation
Using a standard process to limit aggregation, as we previously described [24], lyophilized Aβ peptides were solubilized in 1,1,1,3,3,3-hexafluoro-2-propanol (HFIP) to acquire a monomeric/dimeric sample and minimize the formation of β-sheet structures. Briefly, 1 mg of each lyophilized peptide was dissolved in 1 ml of ice-cold HFIP. The peptides were allowed to air dry in a chemical fume hood for 1 hour followed by further drying in a speed-vac centrifuge for 30 min. The resulting clear film was resuspended in 100% dimethylsulfoxide to a concentration of 1 mM and stored at − 80 °C. Of note, all studies involving Aβ administration used the monomeric form of Aβ.
Effect of Aβ on MMP9 Levels In Vitro
HBMEC were seeded at 50,000 cells per cm2 onto fibronectin-coated 6-well plates. When approximately 90% confluent, cells were treated with human Aβ(1–42) (0-20 μM) for 48 h at 37 °C. After the incubation period, the extracellular media was collected and assessed for MMP9 levels using an MMP9 ELISA. In addition, to assess potential cellular toxicity, the extracellular media was probed for LDH using an LDH cytotoxicity assay.
Effect of MMP9 on Lipoprotein Receptor Shedding In Vitro
HBMEC were seeded at 50,000 cells per cm2 onto fibronectin-coated 6-well plates. When approximately 90% confluent, cells were treated with recombinant human MMP9 (0, 50, 100, and 250 ng/ml) for 48 h at 37 °C. In a similar manner, HBMEC were treated with human Aβ(1–42) (2 μM) alone or in the presence of a broad spectrum MMP inhibitor, marimastat (1 μM), or a MMP9 inhibitor, SB-3CT (1 μM), for 48 h at 37 °C. For both studies, following the incubation period, the extracellular media was collected and assessed for soluble LRP1 and soluble LDLR levels using an LRP1 or LDLR ELISA.
Aβ Transcytosis across an In Vitro BBB Model
The in vitro model of the BBB used for these studies was characterized by our group previously [25]. Briefly, HBMEC were seeded at 100,000 cells/cm2 onto fibronectin-coated (4 μg/cm2), 24-well, 0.4 μm-pore, translucent membrane inserts (0.3 cm2/insert) to establish a polarized monolayer. The layer of cells separates this system into an apical (“blood” side) and basolateral (“brain” side) compartment. Fresh media containing (2 μM) fluorescein-labeled Aβ(1–42) was introduced to the basolateral side of the cellular model, while various concentrations of SB-3CT (0.1, 0.5, 1, 5, and 10 μM) was placed in the apical compartment. The inserts containing SB-3CT were exposed to the wells containing fluorescein-labeled Aβ(1–42) and incubated at 37 °C. The basolateral compartment was sampled at time 0 to establish the initial concentration of fluorescein-labeled Aβ(1–42). Samples were collected from the apical compartment at 0, 30, and 60 min to assess the rate of fluorescein-Aβ(1–42) transcytosis across the cell monolayer (basolateral-to-apical). The apparent permeability of fluorescein-Aβ(1–42) was determined using the equation, apparent permeability = 1/AC0 × (dQ/dt), where A represents the surface area of the membrane, C0 is the initial concentration of fluorescein-Aβ(1–42) in the basolateral compartment, and dQ/dt is the amount of fluorescein-Aβ(1–42) appearing in the apical compartment in the given time period. The apparent permeability of fluorescein-Aβ(1–42) in the presence of each SB-3CT concentration was compared with control and expressed as a percentage. Furthermore, in the same manner as the peptide studies, we utilized a known paracellular marker, 10 kD lucifer yellow dextran (LYD10), to monitor cellular integrity in the presence of each SB-3CT concentration, as we previously described [25].
Isolation of Brain Fractions
Various brain fractions, including the cerebrovasculature, were isolated from the mouse brain tissue as characterized and described by our group previously [13]. Briefly, fresh mouse brains were ground in ice-cold HBSS with 6–8 passes of a Teflon pestle in a glass Dounce homogenizer. An equal volume of 40% dextran solution was added to the brain homogenate for a final concentration of 20% dextran and immediately centrifuged at 6000 g for 15 min at 4 °C. This procedure results in a pellet at the bottom of the container (cerebrovasculature) and a compact mass at the top of the solution (parenchyma) separated by a clear dextran interface (soluble fraction, i.e., non-cell associated). The dextran supernatant was collected and stored at − 80 °C until analysis. The freshly isolated cerebrovessels were immediately collected and used for the ex vivo studies described below.
Effect of MMP9 on Lipoprotein Receptor Shedding Ex Vivo
Akin to the in vitro studies earlier, freshly isolated cerebrovessels from apoE-TR mice (E2, E3, and E4) were treated with recombinant MMP9 (0, 50, 100, and 250 ng/ml) for 3 h at 37 °C. After the incubation period, the extracellular media was collected and assessed for soluble LRP1 and soluble LDLR levels using an LRP1 or LDLR ELISA.
Effect of MMP9 Inhibition on Lipoprotein Receptor Shedding and Aβ(1–42) BBB Clearance In Vivo
These studies were performed using a mouse Aβ BBB clearance model described by our group previously [26]. ApoE-TR mice were administered vehicle (25% DMSO/65% PEG400/10% water) or the MMP9 inhibitor, SB-3CT (25 mg/kg), via intraperitoneal (i.p.) injection, consistent with prior reported use of this drug [19, 27, 28]. Forty-five minutes after the i.p. injection, the mice were stereotaxically injected with 3 μl of 1 mM human Aβ(1–42) bilaterally into the caudate putamen of the brain (0.5 mm anterior to the bregma, 2 mm lateral to the midline, and 3 mm below the surface of the skull). Ten minutes after intracerebral administration of human Aβ(1–42), the mice were euthanatized, and plasma samples were collected via cardiac puncture. Additionally, the brain (minus the cerebellum) was extracted, and all tissue samples were immediately snap frozen in liquid nitrogen. The appearance of human Aβ in the plasma following drug treatment was analyzed by an ELISA for human Aβ(1–42). Moreover, to assess the potential impact of SB-3CT or the intracranial injection itself on BBB integrity, we also examined the appearance of glial fibrillary acidic protein (GFAP) in the plasma, which has been used previously as a peripheral marker of BBB disruption [29, 30]. To assess lipoprotein receptor shedding, mouse brains were processed to isolate various brain fractions, as described above. The soluble (i.e., non-cell associated) brain fraction was examined for mouse LRP1 and mouse LDLR using an ELISA.
Statistics
Statistical analyses were performed using an ANOVA and Bonferonni post hoc test.
Results
Effect of Aβ on MMP9 Levels In Vitro
Monomeric Aβ(1–42) treatment in HBMEC resulted in a dose-dependent increase in MMP9 levels in the extracellular media (Fig. 1) compared with control conditions (vehicle alone). The MMP9 levels observed with 2 μM Aβ(1–42) were 2 times that observed for the control group, while the highest concentration tested, 20 μM Aβ(1–42), resulted in a 7-fold increase in MMP9 levels over control. For these studies, no cellular toxicity was observed with Aβ concentrations 0 to 2 μM, as determined using a LDH cytotoxicity assay (data not shown). A significant increase in LDH release was observed at 20 μM Aβ, indicating potential toxicity at this concentration.
Appearance of extracellular MMP9 levels in the human brain endothelial cells (HBMEC) upon treatment with Aβ(1–42). HBMEC were exposed to various concentrations (0.2, 1, 2, 10, and 20 μM) of human Aβ(1–42) for 48 h at 37 °C. Following the treatment period, the extracellular media was collected and analyzed for MMP9 content by ELISA. Values represent mean ± SEM (n = 3) and are expressed as pg of MMP9 per ml of extracellular media. *P < 0.05 compared with control as determined by ANOVA and Bonferroni post hoc test
Effect of MMP9 on Lipoprotein Receptor Shedding In Vitro
Treatment with rhMMP9 in HBMEC increased soluble lipoprotein receptor levels in the extracellular media compared to control. LRP1 levels were significantly greater than control (2-fold) upon treatment with 250 ng/mL rhMMP9 (Fig. 2a). LDLR levels were also increased in a dose-dependent manner in response to rhMMP9 treatment, but these values did not reach statistical significance (Fig. 2b).
Appearance of extracellular soluble a LRP1 or b LDLR in the human brain endothelial cells (HBMEC) upon treatment with recombinant human MMP9 (rhMMP9). HBMEC were treated with rhMMP9 (50, 100, and 250 ng/ml) for 48 h at 37 °C. Following the treatment period, the extracellular media was collected and analyzed for LRP1 or LDLR content by ELISA. Values represent mean ± SEM (n = 3) and are expressed as ng of LRP1 or LDLR per ml of extracellular media. *P < 0.05 compared with control as determined by ANOVA and Bonferroni post hoc test
Effect of MMP9 Inhibition on Lipoprotein Receptor Shedding In Vitro
In HBMEC, treatment with the MMP9 inhibitor, SB-3CT, significantly lowered Aβ-induced lipoprotein receptor levels in the extracellular media. Soluble LRP1 levels were decreased by approximately 40% upon treatment with SB-3CT (1 μM) compared with Aβ alone (Fig. 3a). With respect to LDLR, treatment with the broad spectrum MMP inhibitor, marimastat (1 μM), or SB-3CT (1 μM) in HBMEC significantly reduced soluble LDLR levels (both ~ 40%) compared with Aβ alone (Fig. 3b).
Appearance of extracellular soluble a LRP1 or b LDLR in the human brain endothelial cells (HBMEC) upon MMP9 inhibition. HBMEC were treated with human Aβ(1–42) (2 μM) alone or in the presence of a MMP inhibitor, marimastat (1 μM), or a MMP9 inhibitor, SB-3CT (1 μM), for 48 h at 37 °C. Following the treatment period, the extracellular media was collected and analyzed for LRP1 or LDLR content by ELISA. Values represent mean ± SEM (n = 3) and are expressed as ng of LRP1 or LDLR per ml of extracellular media. *P < 0.05 compared with Aβ42 alone as determined by ANOVA and Bonferroni post hoc test
Effect of MMP9 Inhibition on Aβ BBB Clearance In Vitro
MMP9 inhibition with SB-3CT dose-dependently enhanced the (basolateral-to-apical) transit of monomeric Aβ(1–42) across an in vitro model of the BBB (Fig. 4). Aβ BBB clearance was increased by > 50% at 100 nM SB-3CT compared with control, and statistically significant increases were observed at SB-3CT concentrations 5 μM and higher (2.5-fold). Moreover, to assess the potential impact of SB-3CT on BBB monolayer integrity, we evaluated the movement of a paracellular marker (10 kDa lucifer yellow dextran) across the in vitro BBB model and observed no difference between each SB-3CT group and control conditions, indicating the barrier properties of the BBB model are maintained in the presence of SB-3CT exposure (data not shown).
Basolateral-to-apical transcytosis of fluorescein-Aβ(1–42) across an in vitro model of the BBB upon MMP9 inhibition. Fluorescein-Aβ(1–42) (2 μM) was exposed to the basolateral (“brain”) compartment while a MMP9 inhibitor, SB-3CT (0.1, 0.5, 1, 5, and 10 μM), was exposed to the apical (“blood”) compartment of the BBB model. Samples were collected from the apical compartment at 0, 30, and 60 min to determine fluorescein-Aβ(1–42) transcytosis across the BBB model. Values represent mean ± SEM (n = 3) and are expressed as a percentage of control. *P < 0.05 compared with control as determined by ANOVA and Bonferroni post hoc test
Influence of apoE on MMP9-Induced Lipoprotein Receptor Shedding Ex Vivo
Similar to our findings in vitro, lipoprotein receptor levels in the extracellular media were significantly elevated following rhMMP9 exposure to freshly isolated cerebrovessels from apoE-TR mice. In terms of apoE genotype, soluble LRP1 levels were significantly increased in apoE4 cerebrovessels (50%) compared with apoE3 or apoE2 cerebrovessels (Fig. 5a). Soluble LDLR levels also increased in a dose-dependent manner with rhMMP9 treatment. An apoE-genotype dependent effect on soluble LDLR levels was also apparent (apoE4 > apoE3 > apoE2), but these values did not reach statistical significance for any of the rhMMP9 concentrations tested (Fig. 5b).
Appearance of extracellular soluble a LRP1 or b LDLR upon treatment with recombinant human MMP9 (rhMMP9) in freshly isolated mouse cerebrovessels. Cerebrovessels from apoE-TR mice (E2, E3, and E4) were treated with rhMMP9 (50, 100, and 250 ng/ml) for 3 h at 37 °C. Following the treatment period, the extracellular media was collected and analyzed for LRP1 or LDLR content by ELISA. Values represent mean ± SEM (n = 4) and are expressed as ng of LRP1 or LDLR per ml of extracellular media. *P < 0.05 compared with each respective apoE2 as determined by ANOVA and Bonferroni post hoc test
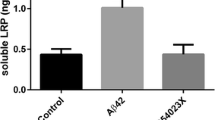
Effect of MMP9 Inhibition on Lipoprotein Receptor Shedding and Aβ Clearance In Vivo
In line with our findings in vitro and ex vivo, treatment with the MMP9 inhibitor, SB-3CT, significantly reduced (> 2-fold) soluble LRP1 and LDLR levels in the brains of apoE4-TR animals compared with vehicle-treated apoE4-TR mice (Fig. 6). With respect to brain Aβ elimination, apoE4-TR mice treated with the SB-3CT showed a significant increase in the appearance of Aβ in the plasma following intracranial monomeric Aβ administration (2-fold) compared with apoE4-TR mice treated with vehicle (Fig. 7), indicating enhanced Aβ elimination across the BBB upon MMP9 inhibition. Interestingly, the extent of Aβ BBB elimination in the apoE4-TR mice treated with SB-3CT was the same as that observed in the apoE3-TR animals (Fig. 7). Lastly, we also probed the plasma for the appearance of GFAP in each of the mice from SB-3CT study in addition to age-matched naïve mice (i.e., no intracranial Aβ injection). Moreover, as a positive comparison, we examined GFAP in the plasma of E4FAD mice, which express five familial AD mutations (5xFAD) alongside the targeted replacement of human apoE [31]. The E4FAD mice have been shown to exhibit BBB dysfunction and cerebrovascular leakiness [32]. In our studies, we did not observe differences between any of the groups of mice in the appearance of GFAP in the plasma, when compared with the respective apoE3 naïve group (Fig. 8). Of note, no statistically significant difference in lipoprotein receptor shedding or Aβ elimination across the BBB was observed between the male and female cohorts in these studies.
Levels of LRP1 and LDLR in the soluble brain fraction of apoE transgenic mice following treatment with a MMP9 inhibitor, SB-3CT. Vehicle or SB-3CT (25 mg/kg) was administered i.p. to apoE4-TR mice and, after 45 min, human Aβ(1–42) was injected intracranially. Ten minutes after the intracerebral injection, the brains were collected and various brain fractions were isolated. LRP1 or LDLR levels in the soluble brain fraction were determined using an ELISA. Values represent mean ± SEM (n = 4) and are expressed as ng of LRP1 or LDLR per ml of soluble brain material. *P < 0.05 compared with respective vehicle as determined by ANOVA and Bonferroni post hoc test
Appearance of human Aβ(1–42) in the plasma following intracerebral Aβ(1–42) administration and treatment with a MMP9 inhibitor, SB-3CT. Vehicle or SB-3CT (25 mg/kg) was administered i.p. to apoE4-TR and apoE3-TR mice and, after 45 min, human Aβ(1–42) was injected intracranially. Ten minutes after the intracerebral injection, the plasma was collected and evaluated for human Aβ(1–42) by ELISA. Values represent mean ± SEM (n = 4) and are expressed as pg of Aβ(1–42) per ml of plasma. *P < 0.05 compared with vehicle-treated apoE4-TR mice as determined by ANOVA and Bonferroni post hoc test
Appearance of GFAP in the plasma following intracerebral Aβ(1–42) administration and treatment with a MMP9 inhibitor, SB-3CT. Vehicle or SB-3CT (25 mg/kg) was administered i.p. to apoE4 and apoE3 mice, and, after 45 min, human Aβ(1–42) was injected intracranially. Ten minutes after the intracerebral injection, the plasma was collected and evaluated for GFAP by ELISA. Plasma was also collected from naïve age-matched apoE3, apoE4, and E4FAD mice for GFAP analysis. Values represent mean ± SEM (n = 4) and are expressed as ng of GFAP per ml of plasma. *P < 0.05 compared with naïve apoE3 mice as determined by ANOVA and Bonferroni post hoc test
Discussion
Our previous work [12] and the reporting of others demonstrate Aβ clearance from the brain is differentially regulated by the type of apoE isoform expressed [3, 33]. Our findings also suggest the effect of apoE on brain Aβ clearance may be driven by alterations in lipoprotein receptor shedding [13]. In these studies, we observed an isoform-specific effect of apoE on lipoprotein receptor shedding (LRP1 and LDLR) with apoE4 showing the highest levels of lipoprotein receptor shedding compared with other apoE isoforms [13]. As mentioned earlier, shedding of the soluble receptor into the extracellular environment prevents the transport of ligands within the cell. Collectively, our prior studies suggest apoE4 is less efficient than other apoE isoforms in preventing lipoprotein receptor shedding, which leads to reduced Aβ clearance across the BBB. The purpose of the present studies was to identify the factors driving lipoprotein receptor shedding in the brain and to further understand the influence of apoE on these processes.
As mentioned earlier, MMP9 has a binding site on LRP1 [15, 16] and has been implicated in the proteolytic shedding of LRP1 [17, 18]. In the present studies, treatment with recombinant MMP9 showed a dose-dependent increase in lipoprotein receptor shedding in brain endothelial cells. As our previous work suggests Aβ can also induce lipoprotein receptor shedding [13], we investigated the potential relationship between Aβ and MMP9. Exposure of monomeric Aβ to brain endothelial cells in vitro increased MMP9 levels in the extracellular media, which is consistent with prior reports in which Aβ treatment induced MMP9 expression and activity in mouse cerebral endothelial cells [34] and rat brain microvessels [35]. As a complementary approach, we also found that treatment with the MMP9 inhibitors marimastat and SB-3CT, mitigated the effect of monomeric Aβ on lipoprotein receptor shedding in brain endothelial cells, suggesting the effect of Aβ on lipoprotein receptor shedding may be mediated through MMP9. As lipoprotein receptor shedding in the brain (and the BBB in particular) can be a major determinant in Aβ elimination, we also investigated the effect of MMP9 on Aβ clearance across the BBB. Modulation with the MMP9 inhibitor, SB-3CT, facilitated the basolateral-to-apical transit of monomeric Aβ across an in vitro BBB model which, based on our current observations, is likely the result of reduced lipoprotein receptor shedding, and provides further evidence for the influence of MMP9 on Aβ removal from the brain.
In addition to identifying an inverse relationship between lipoprotein receptor shedding and Aβ BBB clearance, our prior studies also observed an isoform-dependent effect of apoE on these processes [13]. As such, in the current studies, we examined MMP9 function in the context of apoE genotype. In line with our in vitro studies, rhMMP9 treatment dose-dependently induced lipoprotein shedding in freshly isolated cerebrovessels from apoE-TR animals. Moreover, cerebrovessels from apoE4-TR mice appeared to be more vulnerable to MMP9 exposure as LRP1 shedding, in particular, was significantly elevated compared with apoE2 or apoE3 cerebrovessels. To further understand the interaction between MMP9 and apoE, we evaluated the impact of MMP9 inhibition on lipoprotein receptor shedding in apoE4-TR mice. For these studies, we focused on apoE4-TR mice as these animals demonstrated the greatest level of brain lipoprotein receptor shedding in our prior work [13]. In line with our prior reporting [13], monomeric Aβ was intracranially administered to induce brain lipoprotein receptor shedding in apoE4-TR mice, following treatment with the MMP9 inhibitor, SB-3CT. MMP9 inhibition substantially reduced both LRP1 and LDLR shedding in the brain compared with vehicle-treated apoE4-TR animals. These observations coincide with more broad-based investigations showing that MMP9 inhibition in apoE4 animals preserved BBB integrity and lessened age-related damage to the brain [19].
In conjunction with our lipoprotein receptor shedding studies, we evaluated the effect of MMP9 inhibition on Aβ elimination from the brain in apoE-TR animals. Treatment with the MMP9 inhibitor, SB-3CT, significantly improved monomeric Aβ elimination from the brain in apoE4-TR mice compared with vehicle-treated animals. Intriguingly, the extent of Aβ removal from the brain in the SB-3CT-treated apoE4-TR mice was comparable to that observed in the apoE3-TR animals. In effect, MMP9 modulation allows an apoE4-TR mouse to function like an apoE3-TR mouse, at least in terms of Aβ BBB clearance. Of note, no significant difference in plasma GFAP was observed between the apoE4 control mice and the apoE4 SB-3CT animals, suggesting the effect of SB-3CT on Aβ transit out of the brain in the apoE4 animals was not driven by alterations in BBB integrity. In total, targeting the proteolytic enzymes that impact lipoprotein receptors may provide a novel approach to reducing Aβ burden in the AD brain. In line with this, our prior work showed that inhibition of another lipoprotein receptor sheddase, ADAM10 (A disintegrin and metalloproteinase domain-containing protein 10), significantly reduced brain lipoprotein receptor shedding in a mouse model of AD, which translated to lower Aβ levels in the brain and a statistically significant increase in Aβ in the plasma [36]. With respect to MMP9, it was previously shown more broadly that MMP9 inhibition can alleviate the cognitive impairment induced by intracranial Aβ administration in wild-type mice [37]. Based on our current findings, MMP9 inhibition may attenuate the effects of Aβ through increased Aβ transit across the BBB, which could be an effective approach to lowering Aβ levels in the brain and mitigating the AD phenotype.
Conclusions
The current studies demonstrate that MMP9 contributes to the ectodomain shedding of lipoprotein receptors, and this process is influenced by apoE in an isoform-dependent fashion. As depicted in Fig. 9, we postulate these events occur in the following manner: (1) cerebrovascular insult increases extracellular MMP9 levels, (2) MMP9 proteolyzes the lipoprotein receptors (i.e., shedding), (3) brain Aβ elimination is attenuated, and (4) Aβ accumulates in the brain, contributing to AD pathology. In prior work, we observed that apoE influences lipoprotein receptor shedding and brain Aβ clearance in an isoform-specific manner, and the current studies suggest the effect of apoE on these processes may be mediated through MMP9. We hypothesize that apoE influences lipoprotein receptor shedding by regulating MMP9, doing so in an isoform-specific manner (apoE3 > apoE4) (Fig. 9). At this stage, the nature of the interaction between apoE and MMP9 has yet to be resolved, and more work is necessary to advance our understanding of this relationship. Collectively, these studies may explain the elevated Aβ levels observed in the brains of apoE4 transgenic animals [38] and AD patients carrying the apoE4 allele [39], and potentially offer a novel strategy for the treatment of AD.
Proposed sequence of events contributing to AD pathogenesis. (1) cerebrovascular insult increases extracellular MMP9 levels, (2) MMP9 proteolyzes lipoprotein receptors (i.e., shedding), (3) brain Aβ elimination is attenuated, and (4) Aβ accumulates in the brain, contributing to AD pathology. The current studies indicate that MMP9 impacts lipoprotein receptor shedding in an apoE-isoform-dependent manner, the result of which leads to reduced Aβ elimination from the brain, particularly when the apoE4 isoform is present
References
Reitz C (2012) Alzheimer's disease and the amyloid cascade hypothesis: a critical review. Int J Alzheimers Dis 2012:1–11
Citron M (2010) Alzheimer's disease: Strategies for disease modification. Nat Rev Drug Discov 9(5):387–398
Castellano JM, Kim J, Stewart FR, Jiang H, DeMattos RB, Patterson BW, Fagan AM, Morris JC et al (2011) Human apoE isoforms differentially regulate brain amyloid-beta peptide clearance. Sci Transl Med 3(89):57–67
Mawuenyega KG, Sigurdson W, Ovod V, Munsell L, Kasten T, Morris JC, Yarasheski KE, Bateman RJ (2010) Decreased clearance of CNS beta-amyloid in Alzheimer's disease. Science 330(6012):1774
Selkoe DJ, Hardy J (2016) The amyloid hypothesis of Alzheimer's disease at 25 years. EMBO Mol Med 8(6):595–608
Krohn M, Lange C, Hofrichter J, Scheffler K, Stenzel J, Steffen J, Schumacher T, Bruning T et al (2011) Cerebral amyloid-beta proteostasis is regulated by the membrane transport protein ABCC1 in mice. J Clin Invest 121(10):3924–3931
Castellano JM, Deane R, Gottesdiener AJ, Verghese PB, Stewart FR, West T, Paoletti AC, Kasper TR et al (2012) Low-density lipoprotein receptor overexpression enhances the rate of brain-to-blood Abeta clearance in a mouse model of beta-amyloidosis. Proc Natl Acad Sci U S A 109(38):15502–15507
Storck SE, Pietrzik CU (2017) Endothelial LRP1 - a potential target for the treatment of Alzheimer's disease: theme: drug discovery, development and delivery in Alzheimer's disease guest editor: Davide Brambilla. Pharm Res 34(12):2637–2651
Rebeck GW, LaDu MJ, Estus S, Bu G, Weeber EJ (2006) The generation and function of soluble apoE receptors in the CNS. Mol Neurodegener 1:15–27
Selvais C, Dedieu S, Hornebeck W, Emonard H (2010) Post-translational proteolytic events influence LRP-1 functions. Biomed Mater Eng 20(3):203–207
Kim J, Basak JM, Holtzman DM (2009) The role of apolipoprotein E in Alzheimer's disease. Neuron 63(3):287–303
Bachmeier C, Paris D, Beaulieu-Abdelahad D, Mouzon B, Mullan M, Crawford F (2013) A multifaceted role for apoE in the clearance of beta-amyloid across the blood-brain barrier. Neurodegener Dis 11(1):13–21
Bachmeier C, Shackleton B, Ojo J, Paris D, Mullan M, Crawford F (2014) Apolipoprotein E isoform-specific effects on lipoprotein receptor processing. NeuroMolecular Med 16(4):686–696
Talamagas AA, Efthimiopoulos S, Tsilibary EC, Figueiredo-Pereira ME, Tzinia AK (2007) Abeta(1-40)-induced secretion of matrix metalloproteinase-9 results in sAPPalpha release by association with cell surface APP. Neurobiol Dis 28(3):304–315
Hahn-Dantona E, Ruiz JF, Bornstein P, Strickland DK (2001) The low density lipoprotein receptor-related protein modulates levels of matrix metalloproteinase 9 (MMP-9) by mediating its cellular catabolism. J Biol Chem 276(18):15498–15503
Mantuano E, Inoue G, Li X, Takahashi K, Gaultier A, Gonias SL, Campana WM (2008) The hemopexin domain of matrix metalloproteinase-9 activates cell signaling and promotes migration of schwann cells by binding to low-density lipoprotein receptor-related protein. J Neurosci 28(45):11571–11582
Selvais C, D'Auria L, Tyteca D, Perrot G, Lemoine P, Troeberg L, Dedieu S, Noel A et al (2011) Cell cholesterol modulates metalloproteinase-dependent shedding of low-density lipoprotein receptor-related protein-1 (LRP-1) and clearance function. FASEB J 25(8):2770–2781
Selvais C, Gaide Chevronnay HP, Lemoine P, Dedieu S, Henriet P, Courtoy PJ, Marbaix E, Emonard H (2009) Metalloproteinase-dependent shedding of low-density lipoprotein receptor-related protein-1 ectodomain decreases endocytic clearance of endometrial matrix metalloproteinase-2 and -9 at menstruation. Endocrinology 150(8):3792–3799
Bell RD, Winkler EA, Singh I, Sagare AP, Deane R, Wu Z, Holtzman DM, Betsholtz C et al (2012) Apolipoprotein E controls cerebrovascular integrity via cyclophilin a. Nature 485(7399):512–516
Teng Z, Guo Z, Zhong J, Cheng C, Huang Z, Wu Y, Tang S, Luo C et al (2017) ApoE influences the blood-brain barrier through the NF-kappaB/MMP-9 pathway after traumatic brain injury. Sci Rep 7(1):6649
Halliday MR, Rege SV, Ma Q, Zhao Z, Miller CA, Winkler EA, Zlokovic BV (2016) Accelerated pericyte degeneration and blood-brain barrier breakdown in apolipoprotein E4 carriers with Alzheimer's disease. J Cereb Blood Flow Metab 36(1):216–227
Main BS, Villapol S, Sloley SS, Barton DJ, Parsadanian M, Agbaegbu C, Stefos K, McCann MS et al (2018) Apolipoprotein E4 impairs spontaneous blood brain barrier repair following traumatic brain injury. Mol Neurodegener 13(1):17
Sullivan PM, Mezdour H, Aratani Y, Knouff C, Najib J, Reddick RL, Quarfordt SH, Maeda N (1997) Targeted replacement of the mouse apolipoprotein E gene with the common human APOE3 allele enhances diet-induced hypercholesterolemia and atherosclerosis. J Biol Chem 272(29):17972–17980
Bachmeier C, Beaulieu-Abdelahad D, Crawford F, Mullan M, Paris D (2013) Stimulation of the retinoid X receptor facilitates beta-amyloid clearance across the blood-brain barrier. J Mol Neurosci 49(2):270–276
Bachmeier C, Mullan M, Paris D (2010) Characterization and use of human brain microvascular endothelial cells to examine beta-amyloid exchange in the blood-brain barrier. Cytotechnology 62(6):519–529
Paris D, Bachmeier C, Patel N, Quadros A, Volmar CH, Laporte V, Ganey J, Beaulieu-Abdelahad D et al (2011) Selective antihypertensive dihydropyridines lower abeta accumulation by targeting both the production and the clearance of abeta across the blood-brain barrier. Mol Med 17(3–4):149–162
Cui J, Chen S, Zhang C, Meng F, Wu W, Hu R, Hadass O, Lehmidi T et al (2012) Inhibition of MMP-9 by a selective gelatinase inhibitor protects neurovasculature from embolic focal cerebral ischemia. Mol Neurodegener 7:21
Gu Z, Cui J, Brown S, Fridman R, Mobashery S, Strongin AY, Lipton SA (2005) A highly specific inhibitor of matrix metalloproteinase-9 rescues laminin from proteolysis and neurons from apoptosis in transient focal cerebral ischemia. J Neurosci 25(27):6401–6408
Mayer CA, Brunkhorst R, Niessner M, Pfeilschifter W, Steinmetz H, Foerch C (2013) Blood levels of glial fibrillary acidic protein (GFAP) in patients with neurological diseases. PLoS One 8(4):e62101
Missler U, Wiesmann M, Wittmann G, Magerkurth O, Hagenstrom H (1999) Measurement of glial fibrillary acidic protein in human blood: analytical method and preliminary clinical results. Clin Chem 45(1):138–141
Youmans KL, Tai LM, Nwabuisi-Heath E, Jungbauer L, Kanekiyo T, Gan M, Kim J, Eimer WA et al (2012) APOE4-specific changes in abeta accumulation in a new transgenic mouse model of Alzheimer disease. J Biol Chem 287(50):41774–41786
Tai LM, Balu D, Avila-Munoz E, Abdullah L, Thomas R, Collins N, Valencia-Olvera AC, LaDu MJ (2017) EFAD transgenic mice as a human APOE relevant preclinical model of Alzheimer's disease. J Lipid Res 58(9):1733–1755
Bell RD, Sagare AP, Friedman AE, Bedi GS, Holtzman DM, Deane R, Zlokovic BV (2007) Transport pathways for clearance of human Alzheimer's amyloid beta-peptide and apolipoproteins E and J in the mouse central nervous system. J Cereb Blood Flow Metab 27(5):909–918
Lee JM, Yin K, Hsin I, Chen S, Fryer JD, Holtzman DM, Hsu CY, Xu J (2005) Matrix metalloproteinase-9 in cerebral-amyloid-angiopathy-related hemorrhage. J Neurol Sci 229-230:249–254
Hartz AM, Bauer B, Soldner EL, Wolf A, Boy S, Backhaus R, Mihaljevic I, Bogdahn U et al (2011) Amyloid-beta contributes to blood-brain barrier leakage in transgenic human amyloid precursor protein mice and in humans with cerebral amyloid angiopathy. Stroke 43(2):514–523
Shackleton B, Crawford F, Bachmeier C (2016) Inhibition of ADAM10 promotes the clearance of abeta across the BBB by reducing LRP1 ectodomain shedding. Fluids Barriers CNS 13(1):14
Mizoguchi H, Takuma K, Fukuzaki E, Ibi D, Someya E, Akazawa KH, Alkam T, Tsunekawa H et al (2009) Matrix metalloprotease-9 inhibition improves amyloid beta-mediated cognitive impairment and neurotoxicity in mice. J Pharmacol Exp Ther 331(1):14–22
Bales KR, Liu F, Wu S, Lin S, Koger D, DeLong C, Hansen JC, Sullivan PM et al (2009) Human APOE isoform-dependent effects on brain beta-amyloid levels in PDAPP transgenic mice. J Neurosci 29(21):6771–6779
Schmechel DE, Saunders AM, Strittmatter WJ, Crain BJ, Hulette CM, Joo SH, Pericak-Vance MA, Goldgaber D et al (1993) Increased amyloid beta-peptide deposition in cerebral cortex as a consequence of apolipoprotein E genotype in late-onset Alzheimer disease. Proc Natl Acad Sci U S A 90(20):9649–9653
Acknowledgments
We would like to thank the Roskamp Foundation for their generosity in helping to make this work possible.
Funding
This work was supported by Merit Review award number I01BX002839 from the United States (U.S.) Department of Veterans Affairs (VA) Biomedical Laboratory Research and Development Program. The research in this publication was also supported by the National Institute on Aging of the National Institutes of Health under award number R01AG041971.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Bachmeier is a Research Scientist at the Bay Pines VA Healthcare System, Bay Pines, FL.
Disclaimer
The contents do not represent the views of the U.S. Department of Veterans Affairs or the United States Government. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shackleton, B., Ringland, C., Abdullah, L. et al. Influence of Matrix Metallopeptidase 9 on Beta-Amyloid Elimination Across the Blood-Brain Barrier. Mol Neurobiol 56, 8296–8305 (2019). https://doi.org/10.1007/s12035-019-01672-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-019-01672-z