Abstract
Retinal ganglion cell (RGC) degeneration occurs within 2 weeks following optic nerve crush (ONC) as a consequence of reduced retro-transport of growth factors including nerve growth factor (NGF). The hypothesis that intravitreal (ivt) and eye drop (ed) administration of recombinant human NGF (rhNGF) might counteract ONC in adult rats is explored in this study. We found that both ivt- and ed-rhNGF reduced RGC loss and stimulated axonal regrowth. Chiefly, survival and regenerative effects of rhNGF were associated with a reduction of cells co-expressing Nogo-A/p75NTR at crush site borders, which contribute to glia scar formation following nerve injury, and induce further degeneration. We also found that ocular application of rhNGF reduced p75NTR and proNGF and enhanced phosphorylation of TrkA and its intracellular signals at retina level. Nogo-R and Rock2 expression was also normalized by ed-rhNGF treatment in both ONC and contralateral retina. Our findings that ocular applied NGF reaches and exerts biological actions on posterior segment of the eye give a further insight into the neurotrophin diffusion/transport through eye structures and/or their trafficking in optic nerve. In addition, the use of a highly purified NGF form in injury condition in which proNGF/p75NTR binding is favored indicates that increased availability of mature NGF restores the balance between TrkA and p75NGF, thus resulting in RGC survival and axonal growth. In conclusion, ocular applied NGF is confirmed as a good experimental paradigm to study mechanisms of neurodegeneration and regeneration, disclose biomarkers, and time windows for efficacy treatment following cell or nerve injury.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Extensive literature describes and demonstrates the role of the neurotrophin nerve growth factor (NGF) in the development and maintenance of the nervous system [1,2,3,4,5]. The ability of exogenous NGF to stimulate neuronal survival and the structural and functional recovery after brain injury in vivo was also extensively reported [6,7,8,9,10,11]. Central neurons [12,13,14] and retinal ganglion cells (RGCs) depend on NGF that is produced in the retinal recipient areas and retrograde transport via the optic nerve to the eyes [15,16,17]. The reduced availability of NGF as a consequence of optic nerve crush (ONC) or complete axotomy is responsible for RGC loss and axon degeneration, and it resembles ocular degenerative diseases, like glaucoma [18, 19].
Studies of the retinal response to ONC demonstrated that axonal signal impairment induced rapid cellular and molecular modifications that are associated with the local induction of NGF [20, 21]. The transient post-injury increase in NGF is necessary to inhibit glial proliferation and promote repair mechanisms. However, the limited availability of growth factor over time results in RGC loss, glial scar formation, and further axonal degeneration [22]. We recently demonstrated that p75NTR upregulation in Müller cells and the parallel activation of apoptotic signals that occur immediately after nerve crush resulted in approximately 50% of RGC death in the first 7 days after crush (dac). The subsequent increase in proNGF and p75NTR contributed to the exacerbation of retinal degeneration via further stimulation of apoptosis [20]. Less than 20% of RGCs survived and/or retained the ability to regenerate their axons within 2 weeks after ONC [20, 23]. The increased expression of inhibitory factors, such as Nogo-A, and the activation of Rho-A/Rock signaling via the p75NTR/Nogo receptor (Nogo-R) also occur in the first week after ONC, and it is responsible for cone growth collapse and blockade of axonal growth [24]. Axonal growth inhibition in the retina, PC12 cell line [25], and hippocampus [26] is also under the control of the proNGF/p75NTR signaling complex, which further confirms the role of NGF ligands in the regulation of RGC function. Pharmacodynamic studies demonstrated that administration of murine NGF to the ocular surface reached the retina and optic nerve [27] and exerted neuroprotective effects in animal models of retinitis pigmentosa, diabetic retinopathy, and glaucoma [8, 28,29,30,31,32,33,34]. Murine NGF improved visual loss in childhood optic pathway gliomas [35]. A recent, novel human recombinant form of mature NGF (rhNGF) was demonstrated safe in healthy subjects [36], and it exhibited high efficacy to promote corneal healing in patients. The potential use of rhNGF treatment in patients with retinitis pigmentosa is currently under investigation in a phase Ib/II, multicenter, randomized, double-masked, placebo-controlled study [37].
There are no current data of direct rhNGF efficacy on RGCs and/or its ability to stimulate intracellular survival pathways following retinal injury.
The present study addressed these questions via evaluations of the morphological and biochemical effects of intravitreal and topical (eye drop form) application of rhNGF in an acute unilateral ONC model in adult rats. The anti-apoptotic and regenerative actions of topically applied rhNGF on mature RGC are discussed.
Materials and Methods
Animals and Study Design
Ninety adult Long–Evans rats (male, 300–350 g) were purchased from Charles River (Charles River Laboratories Italia s.r.l.). Rats were maintained on a 12-h light–dark cycle and provided food and water ad libitum. The study was performed in accordance with the ARVO Statement for the Use of Animals in Ophthalmic and Vision Research, and the Animal Care and Use Committee of the San Raffaele Scientific Institute approved all protocols. All surgical and treatment procedures were performed under ketamine and xylazine anesthesia, and every effort was made to minimize animal suffering. Rats that did not recover weight or exhibited signs of suffering after delivery were not included in the experiments.
Rats were submitted to unilateral ONC, which was performed as previously described [38,39,40] and as described in S1 (supplementary files). ONC rats were used to investigate the effects of ocular rhNGF administration (Dompé S.p.A. L’Aquila, Italy). The study included two sets of experiments to analyze and compare the intravitreal (ivt) or eye drop administration (ed) of rhNGF.
The first experiment set investigated retinas 7 days after crush (dac), when approximately 50% of the RGC population was present [41,42,43]. The effects of ivt-rhNGF (n = 6) and ed-rhNGF daily administration (n = 12) on the eyes with ONC were compared to treatment with vehicle (n = 6 ivt; n = 6 ed) to evaluate the efficacy of different routes and doses of rhNGF ocular administration. Untouched and untreated contralateral right eyes were used as controls for ONC-induced loss of RGCs.
A second set of experiments further investigated the survival effects of ed-rhNGF at 14 dac, when a large portion of RGCs and their axons degenerate [38, 42, 44]. Six ONC rats per groups were used to analyze the RGC distribution and axonal growth at 14 dac.
Rats for biochemical investigation underwent ONC and received daily ed treatment with vehicle or ed NGF. These rats were euthanized at 7 and 14 dac to evaluate the expression levels of proNGF, NGF receptors, and intracellular downstream signaling molecules in the retina and optic nerve (n = 6 per time points/group of treatment). A group of naïve rats (n = 3) was used as controls in these experiments.
A scheme of the experimental design and details of the surgical procedure and sample collection and processing are provided as supplementary information.
NGF Treatment
Rats were submitted to ivt or ed administration with rhNGF or vehicle in the left eyes after ONC. The first group of animals received a first ivt injection or 1–1.5 μg/eye of rhNGF (ivt-rhNGF) or vehicle immediately after crush and a second injection of the same dose 72 h post-crush.
Two concentrations of rhNGF were used for ed administration based on previous observations on the efficacy of NGF eye drops [8]: 180 μg/ml (ed-rhNGF 180) and 540 μg/ml (ed-rhNGF 540). Ed-treated rats received a 10-μL droplet of rhNGF or vehicle (ed-vehicle) on the ocular surface immediately after crush and twice daily from day 1 after crush for 7 or 14 days. A group of naïve rats was used as controls (CTR) to evaluate the basal condition and disclose possible effects of ONC or ocular treatment on the contralateral eye (CoEye).
Histological Preparation
Rats received an overdose of anesthetics 7 or 14 days after ONC and were perfused through the heart with ice-cold saline, followed by 4% paraformaldehyde in PBS. The eyes and optic nerves were removed, post-fixed for 24 h, and dehydrated in 10–30% sucrose solutions. Retinas were dissected and used for flat-mount preparation and analyses of RGC survival. The optic nerves were sectioned at a 14 μm thickness using a cryostat (Leica Microsystems GmbH, Wetzlar, Germany), mounted on superglass slides and processed for immunofluorescence.
RGC Immunofluorescence and Neuronal Count
Retinas were incubated overnight at 4 °C with a primary antibody against Tuj1 (1:250, mouse IgG; Covance, Berkeley, USA) in PBS with 2% Triton X-100 plus 5% normal donkey serum (Sigma-Aldrich Co, St. Louis, USA). Retinas were washed, incubated for 2 h at room temperature with donkey anti-goat Cy3-conjugated secondary antibody (1:1000; Jackson Immunoresearch Laboratories, West Grove, USA), washed, flat-mounted, and covered with Vectashield (Vector Laboratories). All steps were performed under gentle shaking. A blinded observer imaged all retinas under a fluorescence microscope (Leica CTR5500; Leica Microsystems). The focus was positioned in the ganglion cell layer, as described previously [20].
Images for quantification of Tuj1 staining were randomly acquired at approximately a 1.0- (central retina) and 3.5-mm (peripheral retina) distance from the optic disc in all quadrants of the retina, and 20 fields (0.064 mm2/field, × 40 objective) were taken. Cell counting was performed as previously described [38] (see also supplementary data for details). Data are expressed as the mean cell number/mm2 ± s.d. or as a percentage cell number of the CoEye group.
Optic Nerve Immunofluorescence and Axon Outgrowth Quantification
The effects of ONC and rhNGF administration on the distribution of Nogo-A and p75NTR at the crush site were investigated using double immunofluorescence. Table S1 lists the primary and secondary antibodies used. Gap-43 immunofluorescence was performed on nerve sections to evaluate axon regrowth following ONC plus rhNGF treatment. Briefly, sections from each experimental group were rinsed with PBS with 0.1% Triton X-100 and incubated in blocking solution for 1 h at room temperature, followed by incubation for 2 or 12 h depending on the primary antibody used (Table S1). Alexa-conjugated secondary antibodies (1:1000) were applied for 2 h at room temperature. Slides were rinsed in PBS, mounted with VectaShield (Vector Laboratories), and observed under an epifluorescent (Leica CTR5500; Leica Microsystems) and/or confocal microscope (Leica TCS SP5). Nerve sections for axonal growth quantification were observed under an epifluorescent microscope using a × 40 magnification objective lens, and the number of GAP-43-labeled axons extending for 0.25–2.0 mm from the crush site was counted and distributed per distance from the crush site (Fig. S2). Values were normalized using the formula described by Leon and colleagues (2000), and the results are expressed as the total number of axons per nerve at a given distance from the lesion site.
Western Blot Analysis
Western blot analysis was performed on protein extracts from retinas at 7 and/or 14 dac. Tissue samples were homogenated via ultrasonication in lysis buffer and centrifuged at 10,000 rpm for 30 min at 4 °C. The supernatants were used for total protein concentration measurements using a Biorad assay.
The Supplementary Methods and Table S1 describe the details of the primary antibodies and procedures. Briefly, samples (20–50 μg total protein) were dissolved in a loading buffer, separated using SDS-PAGE, and electrophoretically transferred to polyvinylidene fluoride (PVDF) or nitrocellulose membranes. Membranes were blocked and incubated overnight at 4 °C with primary antibody, followed by a horseradish peroxidase-conjugated the secondary antibody (Table S1). The blots were developed using ECL Chemiluminescent HRP Substrate (Millipore) as a chromophore. The public domain Image J software (http://rsb.info.nih.gov/ij/) was used for gel densitometry and protein quantification following the method described at http://lukemiller.org/index. php/2010/11/analyzing-gels-and-western-blots-with-image-j/. The integrated density of glyceraldehyde 3-phosphate dehydrogenase (GAPDH) served as the normalizing factor.
Statistical Analysis
Statistical analysis was performed using GraphPad Prism software (Graph Pad Software Inc.) and Statplus Software (AnalystSoft. Inc.). Cell counts were compared using one-way analysis of variance (ANOVA) with ONC and rhNGF treatment as variables. Axon growth measures were compared using two-way ANOVA with the distance from the crush site and treatment as variables. Biochemical data were compared using two-way ANOVA with time, ONC, and rhNGF treatment as variables. Significance between groups was evaluated using Tukey–Kramer’s post hoc test, and p < 0.05 was considered statistically significant.
Results
Effects of Ocular rhNGF Treatment on RGC Survival and Axonal Growth at 7 dac
The Tuj1 antibody was used to stain flat-mounted retinas and identify RGCs in central and peripheral retinas of intact and nerve-crushed eyes. ONC induced a loss of Tuj1 immunoreactivity in central and peripheral retinas compared to CTR (naïve) and CoEyes after 7 days, as previously observed [20]. Therefore, the CoEyes were used as internal controls, and the number of Tuj1 cells in ONC/CoEye retinas was calculated to evaluate the effects of ONC and ivt- and ed-rhNGF treatments.
Figure 1a–e shows representative confocal images of RGC cell distribution in the central retina of CoEye (a), ivt-vehicle (b), ivt-rhNGF (c), and ed-rhNGF 180 and ed-rhNGF 540 (d and e, respectively).Quantitative analyses revealed that the percentage of Tuj1+ cells in the crush eyes treated with vehicle (respective to the CoEyes) was reduced by approximately 50% in the central retina and 30% in the peripheral retina at 7 dac (Fig. 1f–h). No significant changes were found in comparisons of ivt-vehicle and ed-vehicle treatments, which indicates that the delivery route per se did not contribute to retinal cell death (see the Table in Fig. 1).The percentage of Tuj1 cell loss in rats receiving ivt-rhNGF was less than 20% in the central retina, which is an ~ 1.5-fold increase over vehicle-treated rats (p < 0.05; Fig. 1f, h). No significant differences were found in the peripheral retina (Fig. 1g, h). Only a slight increase in RGC number was found in the central retinas of ONC rats that received ed-rhNGF 180 treatment (p = 0.06; Fig. 1f). RGC number was similar to the CoEye following ed-rhNGF 540 (Fig. 1f, h). A significant increase in RCG number was found in the peripheral retinas of rats that received ed-rhNGF 540 (Fig. 1g).
RGC survival 7 days after optic nerve crush. a–e Representative of Tuj1 immunostaining on flat-mounted retinas of the CoEye (a), ivt + vehicle (b), and NGF-treated groups: ivt-rhNGF (c): ed-rhNGF 180 (d); and ed-rhNGF 540 (e). The results of RGC quantification are shown in the graph (f and g; percentage of RGC cells respect to CoEye) and table (h; cells number). Ivt-rhNGF and ed-rhNGF 540 promoted a significant increase in RGC survival in the central retina (f), and only ed-rhNGF 540 affected peripheral RGC number (g). Significantly different versus CoEye: *p < 0.05, **p < 0.001, ***p < 0.0001. Scale bar 20 μm
RGC degeneration was associated with a lack of axon regeneration at 7 dac following ONC. GAP-43-positive fibers were detectable beyond the crush site in vehicle and rhNGF groups, but axon quantification revealed no significant differences between groups at this experimental time point (data not shown).
Effects of ed-rhNGF Treatment on RGC Survival and Axon Growth at 14 dac
A further decrease in RGCs was observed at 14 dac in ONC compared to healthy CoEye retinas. Greater than 80% of RGCs were lost in the central and peripheral retinas following ONC, which is consistent with our previous study [20], and no differences were observed between CTR (naïve) and CoEye (data not showed). The effects of vehicle and ed-rhNGF treatment on the distribution of Tuj1+ cells in the central retinas are presented in representative confocal images in Fig. 2b–d. A twofold increase in the number of Tuj1+ cell was found in the central retinas of ed-rhNGF 180- (p < 0.0001) and ed-rhNGF 540-treated (p < 0.001) groups compared to vehicle-treated rats (Fig. 2a, e). Both ed-rhNGF doses produced a 1.5-fold increase in the number of Tuj1+ cells in the peripheral retinas (Fig. 2a, f).
Ed-rhNGF effects on RGC survival 14 days after optic nerve crush. RCG numbers in central and peripheral retinas are shown in a table (a). The pictures are representative images of Tuj1-stained cells in central retinas of ONC rats that received vehicle (b) or ed-rhNGF at 180 (c) and 540 μg/ml (d) for 14 dac. The percentage increase in RGCs in central and peripheral retinas after rhNGF administration are shown in a graphs (e and f). Significantly different versus CoEye: *p < 0.05, **p < 0.001, ***p < 0.0001. Scale bar 20 μm
Quantification of axon regeneration at 14 dac demonstrated that few axons expressed GAP-43 and crossed the injury site in ONC rats that received vehicle (Fig. 3a), but numerous GAP-43-positive fibers were detected in the nerves of ed-rhNGF-treated rats (Fig. 3b, c). Two-way ANOVA demonstrated a significant interaction between the treatments and axon growth distance from the crush site (table in Fig. 3d). Post hoc analyses revealed that ed-rhNGF 180 and ed-rhNGF 540 significantly increased axon numbers 0.25 mm from the crush site, but only ed-rhNGF 540 increased axons at 0.50 mm (Fig. 3d). No GAP-43-positive fibers were found 1.5 mm from the crush site in any of the experimental groups.
Axon regeneration at 14 dac. Representative images of GAP-43 immunostaining in optic nerves of ONC rats that received vehicle (a) or ed-rhNGF (b, c) for 2 weeks. The graph shows the numbers of GAP-43 fibers at increasing distances from the crush site across treatments (d). Significantly different versus CoEye: *p < 0.05, **p < 0.001, ***p < 0.0001. Scale bar 100 μm
Nogo-A and p75NTR Immunofluorescence in Optic Nerves
The decreased ability of mature RGCs to regrow axons following ONC was previously demonstrated to be dependent on the upregulation and interaction between p75NTR and Nogo-A at the optic nerve level [45]. Therefore, we investigated the expression of these two markers at the crush site at 7 and 14 dac in rats that received vehicle or rhNGF treatment.
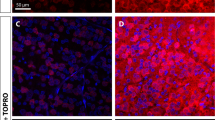
A dense accumulation of p75NTR and Nogo-A immunoreactive cells was observed at the crush site border in the ONC group at 7 dac (Fig. 4a, b, respectively). Cells with or without processes co-expressing p75NTR and Nogo-A were also found in this area (Fig. 4c). Reduced expression and different distributions of p75NTR (Fig. 4d, g) and Nogo-A (Fig. 4e, h) were found in the nerves of ONC rats that received ivt- and ed-rhNGF treatments. Many Nogo-A-expressing cells were detected, but few of these co-expressed p75NTR (Fig. 4f, i). p75NTR-positive cells accumulated at the crush site border in the ONC + vehicle rats, but p75NTR immunoreactivity was found in cells and fibers localized in the central area of the crush site in ivt- and ed-rhNGF-treated rats.
Distribution of p75NTR and Nogo-A in optic nerves 7 days after crush. Increases in immunoreactive cells expressing p75NTR (a) and Nogo-A (b) and co-expressing the two markers (c) were detected at the proximal border of a cells/staining free zone at crush sites in ONC + vehicle rats. Staining of p75NTR (d, g) and Nogo-A (e, h) were differently distributed in ONC + rhNGF groups and show reduced p75NTR immunoreactivity and a marked decrease in p75NTR/Nogo-A cells at crush sites in ivt and ed-rhNGF nerves (f, i). Scale bars are shown in the pictures
A more visible central unstained area delimited by intense p75NTR and Nogo-A immunoreactivity was recognizable in the ONC + vehicle group at 14 dac (Fig. 5a–c). Z-stack analysis confirmed the co-expression of p75NTR and Nogo-A at both margins of crush sites and major accumulation of double-stained cells in the area proximal to the nerve head (see arrow in Fig. 5c). Cells and fibers expressing p75NTR surrounded by Nogo-A immunoreactive spots were also located in the central zones of crush sites (Fig. 5g). Cells co-expressing p75NTR and Nogo-A were found at the proximal and distal borders of crush sites (Fig. 5h). The major difference in the distribution of the two markers at crush sites in ONC + vehicle and ONC + ed-rhNGF groups was the marked reduction in p75NTR immunoreactivity (Fig. 5d). No appreciable changes were found in Nogo-A expression (Fig. 5e), but few cells were positive for p75NTR, and no co-expression of these two markers was observed in ONC rats that received ed-rhNGF (Fig. 5f). Z-stack analysis confirmed that only occasional cells/fibers expressing p75NTR and Nogo-A were found in vehicle-treated rats.
Effects of ed-rhNGF on p75NTR and Nogo-A expression in optic nerves at 14 dac. Intense p75NTR (a) and Nogo-A (b) remained at crush site borders in the ONC + vehicle group after 14 days of treatment, and a major accumulation of double-stained cells in the area proximal to the nerve head was observed (see arrow in c). p75NTR/NogaA-positive cells and fibers were also detected in the central zones (see c, g). Magnifications show that Nogo-A immunoreactivity around fibers and cellular bodies of p75NTR+ cells in the central zone, which was free of recognizable cells (g). Cells co-expressing the two markers or showing an intense distribution of Nogo-A around their cellular bodies are also visible at both sides of the central crush area in ONC + vehicle rats (h). Reduction in p75NTR staining was observed at crush sites in ONC rats that received ed-rhNGF for 2 weeks (d). Nogo-A distribution was similar to ONC + vehicle rats (e). No co-expression of the two markers at the crush site was observed in ONC + ed-rhNGF rats on z-stack analysis (see a representative picture in f). Scale bars are shown in the pictures
Effects of ed-rhNGF on Nogo-A, Nogo-R, and Rock2 Expression in ONC Retinas
Changes in Nogo-A, Nogo-R, and the intracellular signal Rock2 were previously reported in injured retinas [46]. Therefore, the expression levels of these molecules were also examined in our experimental conditions. No changes were found in Nogo-A expression in CTR, ONC, and CoEye retinas with or without rhNGF treatment at 7 and 14 dac (Fig. 6A). However, a time-dependent variation in Nogo-R and Rock2 expression was found (Fig. 6B, C, respectively). Nogo-R and Rock2 levels in the crushed retinas of ONC + vehicle rats increased dramatically compared to CTR and following rhNGF treatment at both doses at 7 dac. However, no significant differences between groups were detected at 14 dac. An increase in Rock2 expression was also found in the contralateral eyes of the ONC and ONC + NGF groups compared to healthy controls at 7 dac (Fig. 6C).
Nogo-A, Nogo-R, and Rock2 expression in CoEye and ONC retinas. The graphs report the semiquantitative evaluation of ONC and ed-rhNGF effects on retinal levels of Nogo-A (A), Nogo-R (B), and Rock2 (C) at 7 and 14 dac. Representative cropped gels showing bands corresponding to the three proteins and loading control (GAPDH) are presented at the bottom of each graph. Samples from the different treatment groups were processed in parallel, as described in the “Materials and Methods” section and Supplementary information S1. No changes in Nogo-A were found in comparisons to ONC with or without rhNGF to the related CoEyes and CTR (A). Nogo-R (B) and Rock2 (C) were significantly increased at 7 dac in ONC + vehicle rats compared to the related CoEye and CTR, and no significant changes were observed at 14 dac. Treatment with ed-rhNGF counteracted the ONC-induced increases in Nogo-R (B) and Rock2 (C) but not the significant effects in related CoEyes. Data are expressed as the mean optical density (arbitrary units) and presented as the mean ± s.d. Significantly different: a vs. untouched and untreated rats (CTR); b vs. CoEye; c vs. ONC. *p < 0.05, **p < 0.001, ***p < 0.0001
ProNGF and NGF Receptor Expression and Activation in the Retina
The expression levels of proNGF, p75NTR, and TrkA were analyzed in the retinas of the CTR, CoEye, and ONC groups, with or without rhNGF treatment at 7 and 14 dac. No significant differences were found in the expression levels of proNGF and NGF receptors in the CTR group and CoEye of the ONC group at the two time points considered or following ed-rhNGF administration to the left eyes (ANOVA Table S2 in supplementary data). Therefore, the CoEyes were used as internal controls, and the related levels of proNGF and NGF receptors in ONC/CoEye retinas were calculated to evaluate the effects of ONC and rhNGF. Two-way ANOVA revealed an effect of treatment and time, but no interaction of a time* treatment effect (Table S2 in supplementary data).
Post hoc analyses revealed significant increases in the expression levels of proNGF and p75NTR in ONC retinas at 7 and 14 dac and no reduction in TrkA at 14 dac (Fig. 7A–D). A reduction in proNGF and p75NTR levels at 7 and 14 dac was found in the 180 and 540 μg/ml ed-rhNGF groups compared to ONCs that received vehicle (Fig. 7A, B, respectively). A significant increase in TrkA levels was observed at 14 dac in the 540 μg/ml ed-rhNGF group (Fig. 7C).
NGF receptor and proNGF expression levels in retinas at 7 and 14 dac. The graphs show proNGF (A), p75NTR (B), and TrkA (C) expression in the retinas of CTR (untouched and untreated rats), ONC + vehicle, and ONC + rhNGF rats at 7 and 14 dac. Representative western blots reporting the band sizes of each protein and the expression trends in the different groups at the two time points are shown in D. Values are expressed as the mean of ONC/CoEye ± s.d. Significantly different: a vs. CTR; b vs. ONC. *p < 0.05, **p < 0.001, ***p < 0.0001
The effects of treatment on TrkA phosphorylation levels were also evaluated at 14 dac. No differences in TrkA phosphorylation were found in any CoEye group or the crushed retinas of the ONC + vehicle group (Fig. 8A, D). An increase in pTrkA/TrkA was detected in ONC + rhNGF retinas compared to CTR and ONC + vehicle retinas, independent of the dose used. Analyses of ERK1/2 expression and phosphorylation levels revealed that rhNGF treatment significantly increased ERK phosphorylation at 540 μg/ml compared to ONC + vehicle (Fig. 8B, E). No significant changes in the levels of total or phosphorylated AKT were found in any rat group (Fig. 8C, F).
TrkA and intracellular signal phosphorylation. The phosphorylation levels of TrkA, ERK 1/2, and AKT were analyzed and compared to the expression of the total unphosphorylated forms in CoEye and crushed retinas of ONC and ONC + ed-rhNGF rats at 14 dac. The results are shown in the graphs (A–C), and a representative western blot showing the band size and expression in each experimental group is shown in D–F. Lanes: CTR; 1 = CoEyes + vehicles; 2 = CoEyes + rhNGF180; 3 = CoEyes + rhNGF540; 4 = ONC + vehicles; 5 = ONC + rhNGF180; 6 = ONC + rhNGF540 CoEyes. Values are expressed as the mean of ONC/CoEye ± s.d. Significantly different: a vs. untouched and untreated rats (CTR); b vs. ONC + vehicle; *p < 0.05, **p < 0.001, ***p < 0.0001
Discussion
The present study verified the efficacy of an ocularly applied rhNGF formulation on injured retinas. The working hypothesis was that administration of exogenous NGF in the first days after ONC would counteract and/or revert the intracellular events resulting in RGC death. Our morphological and molecular results support this hypothesis and demonstrated that rhNGF reduced RGC loss and stimulated axon regrowth via interfering with apoptotic and growth inhibitory pathways in retinas and nerve crush sites.
Ivt and ed were equally efficient routes of rhNGF administration to counteract the initial ONC-induced loss of RGCs, which confirmed that rhNGF in the form of eye drops to the ocular surface reached the retina in sufficient amounts to promote survival and activate protective pathways [27, 47]. Ed-rhNGF 180 and ed-rhNGF 540 recovered ONC-induced RGC degeneration, and ed-rhNGF 540 approximately doubled the number of surviving RGCs and regenerating axons at 14 dac. This last finding suggests that a higher rhNGF dose increased the rate of neurotrophin delivery or accumulation in the posterior eye segment, which could explain the increased effects.
The development of a delivery device implant to allow the use of decreasing rhNGF concentrations should be considered to overcome the possible side-effects related to prolonged use of high NGF doses and/or its accumulation and for further evaluation and characterization of the neuroprotective ability of ed-rhNGF.
Notably, 540 μg/ml rhNGF did not produce cytotoxic effects regardless of intraocular accumulation. Both doses of rhNGF revered the ONC-induced increase in proNGF/p75NTR and stimulated TrkA receptors. The early and concomitant upregulation of p75NTR and proNGF in ONC retinas is consistent with the activation of apoptotic signals that lead to RGC degeneration [20]. ProNGF binding to p75NTR in Müller cells likely induces RGC death via stimulation of the secretion of the proapototic factor TNF-α [48]. Our previous study observed that p75NTR was upregulated in glial cells in ONC retinas, including astrocytes and Müller cells, which may preferentially respond to the proNGF increase [20]. RGCs may also express p75NTR [33, 49], and proNGF directly interacts with receptors on RGC membranes to activate apoptosis [50]. Therefore, the possibility that RGCs expressed p75NTR cannot be excluded.
Our study suggests that rhNGF administration, likely via increasing the availability of mature NGF, favored TrkA activation and/or competed with the ONC-induced proNGF binding to p75NTR, independently of the cell types expressing p75NTR. The rhNGF-induced increase in TrkA phosphorylation and the downstream intracellular signals, like ERK 1/2, is consistent with this hypothesis.
Another aspect of rhNGF neuroprotection is the modulation of Nogo-R and Rock2 expression in the retina. Formation of the Nogo-R/p75NTR complex and activation of the Rho/Rock pathway following ONC hinder the survival of RGCs and axonal regeneration [51]. The upregulation of Rock2 is a specific RGC response to axon lesion, and it begins during the first week after nerve crush to inhibit RGC survival [52, 53]. Rock2 inhibitors enhance survival and induce axonal growth after ONC via stimulation of AKT and ERK phosphorylation [52, 54]. We demonstrated that rhNGF treatment reduced Rock2 and Nogo-R expression in ONC retinas and activated survival pathways, which suggests that the increased availability of mature NGF in ONC eyes counteracts the loss of RGCs.
Reductions in Rock2 expression and the counteraction of increased NogoR/p75NTR were only observed in the eyes that received NGF treatment and not in the contralateral eyes, in which changes in Rock2 and Nogo-R were detected. Our previous study [20] found that unilateral ONC affected contralateral retinas and increased GFAP and intracellular signals associated with cell stress and inflammation. These observations are consistent with previous studies that demonstrated cellular and molecular changes, including the activation of glial cells, in the contralateral eye in the first days after unilateral optic nerve crush [20, 55]. A similar effect was also found in experimental glaucoma models, and the activation of micro- and macroglia in CoEyes may be attributed to damaging signals from degenerating axons that reach the unaffected eyes via the chiasma or post-chiasma areas, including the LGN and visual cortex [56]. A propagation of astrocyte reaction from the damaged eyes to the contralateral retina via the chiasma and optic nerve was also hypothesized. The meaning of glial responses in contralateral retinas following unilateral injury is not fully understood, but it was not associated with RCG loss. Therefore, this response may represent an initial phase of neurodegeneration that is balanced by the presence of endogenous protective mechanisms. The increase in Rock2 in CoEyes in the first week after ONC may be associated with the early activation of signaling pathways that regulate apoptosis, cell stress, and inflammation. Notably, no RGC loss or significant alterations in proNGF or NGF receptors were found in contralateral eyes, which indirectly demonstrates that neuronal survival is regulated via a balance between NGF receptors and their ligands.
Whether the decrease in Nogo-R/Rock2 following ed-rhNGF treatment depends on reduced expression of p75NTR or TrkA-mediated Rho-A inhibition, as previously proposed [25], was not investigated in our experimental conditions. Therefore, the possible mechanisms of action can only be speculated.
Amhed and colleagues [57] demonstrated the survival and regenerative effects of intravitreal administration of sciatic nerve-derived Schwann cells, which secrete growth factors, including NGF, in ONC rats. These authors suggest that the increase in neurotrophin at the retina level promoted p75NTR cleavage at the growth cone level, which resulted in reduced Nogo-R binding and blockade of inhibitory intracellular signals activated by Nogo-A, including Rho/Rock enhancement.
The p75NTR antibody recognizes the full-length 75-kDa protein. Therefore, we cannot conclude that the ed-rhNGF-induced reduction in p75NTR in the retina depended on receptor proteolysis. However, the finding that rhNGF stimulated axon growth supports the idea that rhNGF contributed to the mechanism of disinhibition of RGC axon growth at the nerve level.
Notably, rhNGF counteracted the ONC enhancement of p75NTR, Nogo-R, and Rock2 in the retina at 7 dac without exerting effects on axon regrowth. These findings suggest that ed-rhNGF administration immediately after crush altered the early molecular events that otherwise lead to progressive RGC loss and axon degeneration. However, prolonged treatment is needed to stimulate axon regrowth.
Morphological observations also demonstrated that ocular rhNGF administration altered Nogo-A and p75NTR distribution at crush sites at 7 and 14 dac. We found increased Nogo-A immunoreactivity at crush sites that delineated the border around a central zone that was free of staining/cells, which is consistent with a previous study [58]. Cell localization of Nogo-A and p75NTR at 7 days was similar to the described accumulation of reactive glial cells that form the scar that inhibits axon growth [59]. Nogo-A and p75NTR-overlapping immunostaining was intense at both crush borders at 14 dac, and cells and fibers expressing p75NTR surrounded by Nogo-A immunoreactive spots were localized in central crush sites.
Treatment with rhNGF resulted in a redistribution of p75NTR at the nerve level. A marked decrease and different distribution of p75NTR was observed at crush sites in ONC rats that received ed-rhNGF. The suppression of cell accumulation at crush sites at 7 dac and reduced p75NTR expression at 14 dac were detected following rhNGF, which suggests that this treatment hindered formation of the glial scar and facilitated axonal regrowth. Z-stack analyses demonstrated that numerous cells co-expressing Nogo-A and p75NTR were localized at crush sites, especially at 7 dac. To the best of our knowledge, this study is the first report demonstrating the presence of Nogo-A/p75NTR-positive cells in mature intact or injured optic nerves.
The site of injury following nerve crush is populated by numerous cellular elements that express p75NTR constitutively or following activation, including damaged oligodendrocytes, astrocytes, and activated macrophage/microglia [51]. Nogo-A in adult optic nerves is primarily exclusively reported in mature oligodendrocytes [51], but oligodendrocyte precursors, including the subpopulation of NG2/glia cells, which play an axon growth inhibitory role, also accumulate at injury sites [60, 61]. Neither Nogo-A nor p75NTR expression were described in these cells. However, these cells act as neuronal precursors and are responsive to NGF [62]. Therefore, it is very likely that these two markers are expressed at different stages of oligodendrocyte/glial cell activation or differentiation. Eye drop NGF administration [63] exerts anti-inflammatory effects on macrophages and microglia. Therefore, these cells may co-express p75NTR and Nogo-A following injury.
In summary, the present study demonstrated that ocular application of rhNGF recovered the loss of RGCs and stimulated a cellular growth state and/or axon regrowth. Intravitreal-modified cell implants, inflammatory agent injection, and NGF or TrkA agonists [48] recover ONC-induced retina degeneration [64,65,66,67,68]. Our results indicated that stimuli that influence gene expression in the retina or optic nerve may activate the growth state of mature RGCs and assist and/or potentiate axonal regeneration [66]. We propose that the ocular administration of rhNGF influences the dynamic equilibrium between p75NTR and TrkA receptors and NGF ligands to activate survival and regeneration programs in the first 2 weeks after injury. Further studies are necessary to verify the optimal rhNGF dose and its efficacy to stimulate stable axon regeneration and/or extend effects over a longer post-injury period. However, our findings contribute to the development of therapeutic strategies for degenerative ocular diseases. A potential translatability of topical rhNGF as a treatment for optic neuropathies is reasonable based on the evidence that neuroprotection and regeneration may be achieved using a non-invasive route of application, such as NGF eye drops, and that ocular application of rhNGF was well-tolerated without evidence of systemic adverse effects in clinical trials [36, 37].
References
Huang EJ, Reichardt LF (2001) Neurotrophins: roles in neuronal development and function. Annu Rev Neurosci 24:677–736. https://doi.org/10.1146/annurev.neuro.24.1.677
Reichardt LF (2006) Neurotrophin-regulated signalling pathways. Philos Trans R Soc Lond Ser B Biol Sci 361(1473):1545–1564. https://doi.org/10.1098/rstb.2006.1894
Buchman VL, Davies AM (1993) Different neurotrophins are expressed and act in a developmental sequence to promote the survival of embryonic sensory neurons. Development 118(3):989–1001
Harada C, Harada T, Nakamura K, Sakai Y, Tanaka K, Parada LF (2006) Effect of p75NTR on the regulation of naturally occurring cell death and retinal ganglion cell number in the mouse eye. Dev Biol 290(1):57–65. https://doi.org/10.1016/j.ydbio.2005.08.051
Sofroniew MV, Howe CL, Mobley WC (2001) Nerve growth factor signaling, neuroprotection, and neural repair. Annu Rev Neurosci 24:1217–1281
Levi-Montalcini R (1987) The nerve growth factor 35 years later. Science 237(4819):1154–1162
Tuszynski MH, Peterson DA, Ray J, Baird A, Nakahara Y, Gage FH (1994) Fibroblasts genetically modified to produce nerve growth factor induce robust neuritic ingrowth after grafting to the spinal cord. Exp Neurol 126(1):1–14
Lambiase A, Aloe L, Centofanti M, Parisi V, Bao SN, Mantelli F, Colafrancesco V, Manni GL et al (2009) Experimental and clinical evidence of neuroprotection by nerve growth factor eye drops: implications for glaucoma. Proc Natl Acad Sci U S A 106(32):13469–13474. https://doi.org/10.1073/pnas.0906678106
Hefti F (1986) Nerve growth factor promotes survival of septal cholinergic neurons after fimbrial transections. J Neurosci 6(8):2155–2162
Oudega M, Hagg T (1996) Nerve growth factor promotes regeneration of sensory axons into adult rat spinal cord. Exp Neurol 140(2):218–229. https://doi.org/10.1006/exnr.1996.0131
Ribeiro-Resende VT, Pimentel-Coelho PM, Mesentier-Louro LA, Mendez RM, Mello-Silva JP, Cabral-da-Silva MC, de Mello FG, de Melo Reis RA et al (2009) Trophic activity derived from bone marrow mononuclear cells increases peripheral nerve regeneration by acting on both neuronal and glial cell populations. Neuroscience 159(2):540–549. https://doi.org/10.1016/j.neuroscience.2008.12.059
Hendry IA, Stockel K, Thoenen H, Iversen LL (1974) The retrograde axonal transport of nerve growth factor. Brain Res 68(1):103–121
Johnson EM Jr, Taniuchi M, Clark HB, Springer JE, Koh S, Tayrien MW, Loy R (1987) Demonstration of the retrograde transport of nerve growth factor receptor in the peripheral and central nervous system. J Neurosci 7(3):923–929
Campenot RB, Soin J, Blacker M, Lund K, Eng H, MacInnis BL (2003) Block of slow axonal transport and axonal growth by brefeldin A in compartmented cultures of rat sympathetic neurons. Neuropharmacology 44(8):1107–1117
Harrington AW, Ginty DD (2013) Long-distance retrograde neurotrophic factor signalling in neurons. Nat Rev Neurosci 14(3):177–187. https://doi.org/10.1038/nrn3253
Almasieh M, Wilson AM, Morquette B, Cueva Vargas JL, Di Polo A (2012) The molecular basis of retinal ganglion cell death in glaucoma. Prog Retin Eye Res 31(2):152–181. https://doi.org/10.1016/j.preteyeres.2011.11.002
Murphy JA, Clarke DB (2006) Target-derived neurotrophins may influence the survival of adult retinal ganglion cells when local neurotrophic support is disrupted: implications for glaucoma. Med Hypotheses 67(5):1208–1212. https://doi.org/10.1016/j.mehy.2006.04.049
Vrabec JP, Levin LA (2007) The neurobiology of cell death in glaucoma. Eye (Lond) 21(Suppl 1):S11–S14. https://doi.org/10.1038/sj.eye.6702880
Sposato V, Bucci MG, Coassin M, Russo MA, Lambiase A, Aloe L (2008) Reduced NGF level and TrkA protein and TrkA gene expression in the optic nerve of rats with experimentally induced glaucoma. Neurosci Lett 446(1):20–24. https://doi.org/10.1016/j.neulet.2008.09.024
Mesentier-Louro LA, De Nicolo S, Rosso P, De Vitis LA, Castoldi V, Leocani L, Mendez-Otero R, Santiago MF, Tirassa P, Rama P, Lambiase A (2017) Time-dependent nerve growth factor signaling changes in the rat retina during optic nerve crush-induced degeneration of retinal ganglion cells. Int J Mol Sci 18 (1). doi:https://doi.org/10.3390/ijms18010098
Bai Y, Dergham P, Nedev H, Xu J, Galan A, Rivera JC, ZhiHua S, Mehta HM et al (2010) Chronic and acute models of retinal neurodegeneration TrkA activity are neuroprotective whereas p75NTR activity is neurotoxic through a paracrine mechanism. J Biol Chem 285(50):39392–39400. https://doi.org/10.1074/jbc.M110.147801
Jian Q, Tao Z, Li Y, Yin ZQ (2015) Acute retinal injury and the relationship between nerve growth factor, Notch1 transcription and short-lived dedifferentiation transient changes of mammalian Muller cells. Vis Res 110(Pt A):107–117. https://doi.org/10.1016/j.visres.2015.01.030
Vidal-Sanz M, Galindo-Romero C, Valiente-Soriano FJ, Nadal-Nicolas FM, Ortin-Martinez A, Rovere G, Salinas-Navarro M, Lucas-Ruiz F et al (2017) Shared and differential retinal responses against optic nerve injury and ocular hypertension. Front Neurosci 11:235. https://doi.org/10.3389/fnins.2017.00235
Fujita Y, Yamashita T (2014) Axon growth inhibition by RhoA/ROCK in the central nervous system. Front Neurosci 8:338. https://doi.org/10.3389/fnins.2014.00338
Nusser N, Gosmanova E, Zheng Y, Tigyi G (2002) Nerve growth factor signals through TrkA, phosphatidylinositol 3-kinase, and Rac1 to inactivate RhoA during the initiation of neuronal differentiation of PC12 cells. J Biol Chem 277(39):35840–35846. https://doi.org/10.1074/jbc.M203617200
Deinhardt K, Kim T, Spellman DS, Mains RE, Eipper BA, Neubert TA, Chao MV, Hempstead BL (2011) Neuronal growth cone retraction relies on proneurotrophin receptor signaling through Rac. Sci Signal 4(202):ra82. https://doi.org/10.1126/scisignal.2002060
Lambiase A, Tirassa P, Micera A, Aloe L, Bonini S (2005) Pharmacokinetics of conjunctivally applied nerve growth factor in the retina and optic nerve of adult rats. Invest Ophthalmol Vis Sci 46(10):3800–3806
Siliprandi R, Canella R, Carmignoto G (1993) Nerve growth factor promotes functional recovery of retinal ganglion cells after ischemia. Invest Ophthalmol Vis Sci 34(12):3232–3245
Hammes HP, Federoff HJ, Brownlee M (1995) Nerve growth factor prevents both neuroretinal programmed cell death and capillary pathology in experimental diabetes. Mol Med 1(5):527–534
Lenzi L, Coassin M, Lambiase A, Bonini S, Amendola T, Aloe L (2005) Effect of exogenous administration of nerve growth factor in the retina of rats with inherited retinitis pigmentosa. Vis Res 45(12):1491–1500
Sun X, Xu X, Wang F, Zhang X, Yu Z, Lu H, Ho PC (2007) Effects of nerve growth factor for retinal cell survival in experimental retinal detachment. Curr Eye Res 32(9):765–772. https://doi.org/10.1080/02713680701531082
Sivilia S, Giuliani A, Fernandez M, Turba ME, Forni M, Massella A, De Sordi N, Giardino L et al (2009) Intravitreal NGF administration counteracts retina degeneration after permanent carotid artery occlusion in rat. BMC Neurosci 10:52. https://doi.org/10.1186/1471-2202-10-52
Colafrancesco V, Parisi V, Sposato V, Rossi S, Russo MA, Coassin M, Lambiase A, Aloe L (2011) Ocular application of nerve growth factor protects degenerating retinal ganglion cells in a rat model of glaucoma. J Glaucoma 20(2):100–108. https://doi.org/10.1097/IJG.0b013e3181d787e5
Lambiase A, Aloe L (1996) Nerve growth factor delays retinal degeneration in C3H mice. Graefes Arch Clin Exp Ophthalmol 234(Suppl 1):S96–S100
Falsini B, Chiaretti A, Rizzo D, Piccardi M, Ruggiero A, Manni L, Soligo M, Dickmann A et al (2016) Nerve growth factor improves visual loss in childhood optic gliomas: a randomized, double-blind, phase II clinical trial. Brain 139(Pt 2):404–414. https://doi.org/10.1093/brain/awv366
Ferrari MP, Mantelli F, Sacchetti M, Antonangeli MI, Cattani F, D'Anniballe G, Sinigaglia F, Ruffini PA et al (2014) Safety and pharmacokinetics of escalating doses of human recombinant nerve growth factor eye drops in a double-masked, randomized clinical trial. BioDrugs 28(3):275–283. https://doi.org/10.1007/s40259-013-0079-5
Falsini B, Iarossi G, Chiaretti A, Ruggiero A, Manni L, Galli-Resta L, Corbo G, Abed E (2016) Erratum to: NGF eye-drops topical administration in patients with retinitis pigmentosa, a pilot study. J Transl Med 14:43. https://doi.org/10.1186/s12967-016-0800-5
Mesentier-Louro LA, Zaverucha-do-Valle C, da Silva-Junior AJ, Nascimento-Dos-Santos G, Gubert F, de Figueiredo AB, Torres AL, Paredes BD et al (2014) Distribution of mesenchymal stem cells and effects on neuronal survival and axon regeneration after optic nerve crush and cell therapy. PLoS One 9(10):e110722. https://doi.org/10.1371/journal.pone.0110722
Zaverucha-do-Valle C, Mesentier-Louro L, Gubert F, Mortari N, Padilha AB, Paredes BD, Mencalha A, Abdelhay E et al (2014) Sustained effect of bone marrow mononuclear cell therapy in axonal regeneration in a model of optic nerve crush. Brain Res 1587:54–68. https://doi.org/10.1016/j.brainres.2014.08.070
Mesentier-Louro LA, Coronel J, Zaverucha-do-Valle C, Mencalha A, Paredes BD, Abdelhay E, Mendez-Otero R, Santiago MF (2012) Cell therapy modulates expression of Tax1-binding protein 1 and synaptotagmin IV in a model of optic nerve lesion. Invest Ophthalmol Vis Sci 53(8):4720–4729. https://doi.org/10.1167/iovs.11-8198
Parrilla-Reverter G, Agudo M, Sobrado-Calvo P, Salinas-Navarro M, Villegas-Perez MP, Vidal-Sanz M (2009) Effects of different neurotrophic factors on the survival of retinal ganglion cells after a complete intraorbital nerve crush injury: a quantitative in vivo study. Exp Eye Res 89(1):32–41. https://doi.org/10.1016/j.exer.2009.02.015
Selles-Navarro I, Ellezam B, Fajardo R, Latour M, McKerracher L (2001) Retinal ganglion cell and nonneuronal cell responses to a microcrush lesion of adult rat optic nerve. Exp Neurol 167(2):282–289. https://doi.org/10.1006/exnr.2000.7573
Sacchetti M, Mantelli F, Rocco ML, Micera A, Brandolini L, Focareta L, Pisano C, Aloe L et al (2017) Recombinant human nerve growth factor treatment promotes photoreceptor survival in the retinas of rats with retinitis pigmentosa. Curr Eye Res 42(7):1064–1068. https://doi.org/10.1080/02713683.2017.1279634
Zaverucha-do-Valle C, Gubert F, Bargas-Rega M, Coronel JL, Mesentier-Louro LA, Mencalha A, Abdelhay E, Santiago MF et al (2011) Bone marrow mononuclear cells increase retinal ganglion cell survival and axon regeneration in the adult rat. Cell Transplant 20(3):391–406. https://doi.org/10.3727/096368910X524764
Wang KC, Kim JA, Sivasankaran R, Segal R, He Z (2002) P75 interacts with the Nogo receptor as a co-receptor for Nogo, MAG and OMgp. Nature 420(6911):74–78. https://doi.org/10.1038/nature01176
Grandpre T, Strittmatter SM (2001) Nogo: a molecular determinant of axonal growth and regeneration. Neuroscientist 7(5):377–386. https://doi.org/10.1177/107385840100700507
Sposato V, Parisi V, Manni L, Antonucci MT, Di Fausto V, Sornelli F, Aloe L (2009) Glaucoma alters the expression of NGF and NGF receptors in visual cortex and geniculate nucleus of rats: effect of eye NGF application. Vis Res 49(1):54–63
Lebrun-Julien F, Morquette B, Douillette A, Saragovi HU, Di Polo A (2009) Inhibition of p75(NTR) in glia potentiates TrkA-mediated survival of injured retinal ganglion cells. Mol Cell Neurosci 40(4):410–420. https://doi.org/10.1016/j.mcn.2008.12.005
Balzamino BO, Biamonte F, Esposito G, Marino R, Fanelli F, Keller F, Micera A (2014) Characterization of NGF, trkA (NGFR), and p75 (NTR) in retina of mice lacking reelin glycoprotein. Int J Cell Biol 2014:725928–725913. https://doi.org/10.1155/2014/725928
Al-Gayyar MM, Mysona BA, Matragoon S, Abdelsaid MA, El-Azab MF, Shanab AY, Ha Y, Smith SB et al (2013) Diabetes and overexpression of proNGF cause retinal neurodegeneration via activation of RhoA pathway. PLoS One 8(1):e54692. https://doi.org/10.1371/journal.pone.0054692
Vajda F, Jordi N, Dalkara D, Joly S, Christ F, Tews B, Schwab ME, Pernet V (2015) Cell type-specific Nogo-A gene ablation promotes axonal regeneration in the injured adult optic nerve. Cell Death Differ 22(2):323–335. https://doi.org/10.1038/cdd.2014.147
Lingor P, Tonges L, Pieper N, Bermel C, Barski E, Planchamp V, Bahr M (2008) ROCK inhibition and CNTF interact on intrinsic signalling pathways and differentially regulate survival and regeneration in retinal ganglion cells. Brain 131(Pt 1):250–263. https://doi.org/10.1093/brain/awm284
Xu F, Huang H, Wu Y, Lu L, Jiang L, Chen L, Zeng S, Li L et al (2014) Upregulation of Gem relates to retinal ganglion cells apoptosis after optic nerve crush in adult rats. J Mol Histol 45(5):565–571. https://doi.org/10.1007/s10735-014-9579-y
Koch JC, Tonges L, Barski E, Michel U, Bahr M, Lingor P (2014) ROCK2 is a major regulator of axonal degeneration, neuronal death and axonal regeneration in the CNS. Cell Death Dis 5:e1225. https://doi.org/10.1038/cddis.2014.191
Bodeutsch N, Siebert H, Dermon C, Thanos S (1999) Unilateral injury to the adult rat optic nerve causes multiple cellular responses in the contralateral site. J Neurobiol 38(1):116–128
Macharadze T, Goldschmidt J, Marunde M, Wanger T, Scheich H, Zuschratter W, Gundelfinger ED, Kreutz MR (2009) Interretinal transduction of injury signals after unilateral optic nerve crush. Neuroreport 20(3):301–305. https://doi.org/10.1097/WNR.0b013e32832027e6
Ahmed Z, Suggate EL, Brown ER, Dent RG, Armstrong SJ, Barrett LB, Berry M, Logan A (2006) Schwann cell-derived factor-induced modulation of the NgR/p75NTR/EGFR axis disinhibits axon growth through CNS myelin in vivo and in vitro. Brain 129(Pt 6):1517–1533. https://doi.org/10.1093/brain/awl080
Frank M, Wolburg H (1996) Cellular reactions at the lesion site after crushing of the rat optic nerve. Glia 16(3):227–240. https://doi.org/10.1002/(SICI)1098-1136(199603)16:3<227::AID-GLIA5>3.0.CO;2-Z
Yiu G, He Z (2006) Glial inhibition of CNS axon regeneration. Nat Rev Neurosci 7(8):617–627. https://doi.org/10.1038/nrn1956
Butt AM, Pugh M, Hubbard P, James G (2004) Functions of optic nerve glia: axoglial signalling in physiology and pathology. Eye (Lond) 18(11):1110–1121. https://doi.org/10.1038/sj.eye.6701595
Greenwood K, Butt AM (2003) Evidence that perinatal and adult NG2-glia are not conventional oligodendrocyte progenitors and do not depend on axons for their survival. Mol Cell Neurosci 23(4):544–558
Tirassa P, Maccarone M, Carito V, De Nicolo S, Fiore M (2015) Ocular nerve growth factor administration counteracts the impairment of neural precursor cell viability and differentiation in the brain subventricular area of rats with streptozotocin-induced diabetes. Eur J Neurosci 41(9):1207–1218. https://doi.org/10.1111/ejn.12854
Carito V, Nicolo S, Fiore M, Maccarone M, Tirassa P (2015) Ocular nerve growth factor administration (oNGF) affects disease severity and inflammatory response in the brain of rats with experimental allergic encephalitis (EAE). Can J Physiol Pharmacol 94:1–8. https://doi.org/10.1139/cjpp-2015-0133
Berry M, Carlile J, Hunter A, Tsang W, Rosenstiel P, Sievers J (1999) Optic nerve regeneration after intravitreal peripheral nerve implants: trajectories of axons regrowing through the optic chiasm into the optic tracts. J Neurocytol 28(9):721–741
Leon S, Yin Y, Nguyen J, Irwin N, Benowitz LI (2000) Lens injury stimulates axon regeneration in the mature rat optic nerve. J Neurosci 20(12):4615–4626
Fischer D, He Z, Benowitz LI (2004) Counteracting the Nogo receptor enhances optic nerve regeneration if retinal ganglion cells are in an active growth state. J Neurosci 24(7):1646–1651. https://doi.org/10.1523/JNEUROSCI.5119-03.2004
Yin Y, Cui Q, Li Y, Irwin N, Fischer D, Harvey AR, Benowitz LI (2003) Macrophage-derived factors stimulate optic nerve regeneration. J Neurosci 23(6):2284–2293
Fischer D, Heiduschka P, Thanos S (2001) Lens-injury-stimulated axonal regeneration throughout the optic pathway of adult rats. Exp Neurol 172(2):257–272. https://doi.org/10.1006/exnr.2001.7822
Acknowledgements
This study was supported by an unrestricted research Grant from Dompé pharmaceuticals Spa. We thank CNPq Brazil (Conselho Nacional de Pesquisa e Desenvolvimento) for providing a scholarship for Louise A. Mesentier-Louro; and Anna Lorusso for technical support. Pamela Rosso and Valentina Carito are recipient of CNR fellowships founded by Paola Tirassa’s grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Electronic Supplementary Material
ESM 1
(PDF 815 kb)
Rights and permissions
About this article
Cite this article
Mesentier-Louro, L.A., Rosso, P., Carito, V. et al. Nerve Growth Factor Role on Retinal Ganglion Cell Survival and Axon Regrowth: Effects of Ocular Administration in Experimental Model of Optic Nerve Injury. Mol Neurobiol 56, 1056–1069 (2019). https://doi.org/10.1007/s12035-018-1154-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-018-1154-1