Abstract
Cerebrolysin is a peptide mixture able to ameliorate symptomatology and delay progression of neurological disorders such as Alzheimer’s disease and dementia. The administration of this drug in humans presents several criticisms due to its short half-life, poor stability, and high doses needed to achieve the effect. This paper investigates the potential of polylactic-co-glycolide (PLGA) nanoparticles (NPs) as sustained release systems for iv administration of cerebrolysin in normal and brain injured rats. NPs were prepared by water-in-oil-in-water (w/o/w) double emulsion technique and characterized by light scattering for mean size and zeta potential and by scanning electron microscopy (SEM) for surface morphology. The NPs produced by double sonication under cooling at 60 W for 45 s, 12 mL of 1 % w:v of PVA, and 1:0.6 w:w drug/PLGA ratio (C-NPs4) displayed an adequate loading of drug (24 ± 1 mg/100 mg of NPs), zeta potential value (−13 mV), and average diameters (ranged from 250 to 330 nm) suitable to iv administration. SEM images suggested that cerebrolysin was molecularly dispersed into matricial systems and partially adhered to the NP surface. A biphasic release with an initial burst effect followed by sustained release over 24 h was observed. Long-term stability both at room and at low temperature of freeze-dried NPs was investigated. To gain deeper insight into NP stability after in vivo administration, the stability of the best NP formulation was also tested in serum. These PLGA NPs loaded with cerebrolysin were able to reduce brain pathology following traumatic brain injury. However, the size, the polydispersivity, and the surface properties of sample were significantly affected by the incubation time and the serum concentration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Owing to their potential in providing symptomatic relief and in acting as therapeutic agents, neurotropic factors (NTFs) play a key role in the “health and functionality” of the central nervous systems (CNS) and potentiality in the treatment of several neurodegenerative disorders like Parkinson’s (PD), Alzheimer’s (AD), Huntington’s (HD) disease, amyotrophic lateral sclerosis (ALS) [1]. Cerebrolysin, formulated as a mixture of neuropeptides all together mimicking the NTF action, is one of the most interesting products as it can induce neuroprotection and reduce the cellular stress produced by injuries of the CNS facilitating the neuron regeneration [2–4]. Despite the promising activity, therapeutic use of cerebrolysin is hampered by its poor biopharmaceutical properties. In fact, this drug is only partially capable of crossing the blood-brain barrier (BBB) since it is formed by 25 % of low molecular weight peptides [5]. Besides, the short half-life and the poor stability in the blood require the administration of high doses. The bioavailability of cerebrolysin could be improved both by reducing its degradation by endogenous enzymes and by modulating its release through encapsulation in suitable formulations. Among the various colloidal drug delivery systems, polymeric nanoparticles (NPs) represent a very promising approach to both stabilize and control the delivery of pharmacological agents [6] and, if appropriately engineered, to cross the BBB [7–9]. Polymeric NPs are versatile nanosized carriers (1–1000 nm), made of natural or synthetic polymers, into which drugs can be loaded in the solid state or in solution, adsorbed or chemically linked to the surface. Nowadays, aiming to produce NPs, few polymers can ensure safety profiles regarding biocompatibility and biodegradability of NPs. One of the few is polylactide-co-glycolide (PLGA), one of the most successful polymers used in the development of drug delivery systems [10, 11]. However, to design and develop PLGA NPs for drug controlled release, it is necessary to pay attention to both particle size and surface properties of the colloidal carriers in order to escape macrophages and achieving in vivo stability. Moreover, the distribution of drug loaded into NPs and its release rate and kinetics should be optimized in order to attain the protection and the action of the active agents at the required therapeutic rate.
On the basis of the above premises, this paper aims to investigate the cerebrolysin encapsulation into PLGA NPs prepared by double emulsion technique in order to obtain stable systems having an appropriate dimension for injectable use and able to deliver the neuroprotective compound inducing long-lasting beneficial effects in various models of central nervous system (CNS) injury. The formulation studies were carried out by fixing the polymer molecular weight, surfactant, output, and sonication time and modifying the polymer/drug and the polymer/surfactant ratios. The size, the size distribution (polydispersivity), the morphology of the NPs, and the influence of the theoretical drug loading on the drug encapsulation efficiency were investigated. The most appropriate formulation was lyophilized to overcome the hydrolytic instability of the polymer in aqueous suspension, and the effect of the freeze-drying parameters and storage temperature (4 and 25 °C) over 5 months was evaluated. Lastly, the interaction between the NPs and the serum components and the effect of this interaction on the colloidal stability were investigated. The best formulation of PLGA NPs loaded with cerebrolysin was administered in a traumatic brain injury model, and its neuroprotective effects were determined using a standard protocol [12–16].
Materials
Cerebrolysin® (Ever Neuro Pharma GmbH, Unterach, Austria) is a peptide preparation extracted from porcine brain available on the market at the concentration of 215.2 mg/mL in 1-mL vials. Cerebrolysin is constituted as formulation of peptides (25 % of peptides featured by low molecular weight (<10 kDa)) and free amino acids (75 %). The mixture also has a relatively high concentration of magnesium, potassium, selenium, and other elements [17, 18].
Poly(d,l-lactide-co-glycolide) (1:1 lactic/glycolic acid molar ratio) (PLGA; RG503H, inherent viscosity 0.38 dl/g) was used as the polymer (Boehringer-Ingelheim, Ingelheim am Rhein, Germany). According to the experimental titration results of the carboxylic end of the polymer (4.94 mg KOH/g of polymer), the molecular weight of RG503H was calculated to be 11,000. Polivinyl alcohol (PVA; MW 15,000) and fetal bovine serum (FBS) were purchased from Fluka (Milan, Italy) and Euroclone Celbio (Milan, Italy), respectively. Trehalose and the other chemicals were used as received from the manufacturer without further purification (Sigma-Aldrich, Milan, Italy). A MilliQ water system (Millipore, Bedford, MA, USA), supplied with distilled water, provided high-purity water (>18 MΩ).
Methods
Preparation of NPs
PLGA NPs were prepared by double emulsion water-in-oil-in-water (w/o/w) solvent evaporation method [19–21]. The different samples of unloaded NPs were prepared by varying the PVA concentration and the volume of water in the second emulsion. Briefly, 1 mL of water was mixed with 5 mL of dichloromethane (DCM) solution of PLGA (100 mg) under cooling (5 °C) by using a probe sonicator (Microson Ultrasonic cell disruptor, Misonix Inc. Farmingdale, NY, USA) at 60 W for 45 s to obtain a w/o emulsion (first inner emulsion). The first inner emulsion was rapidly added to different amounts of 1 % (w:v) PVA aqueous solution (8, 12, and 24 mL). Then, the first inner emulsion and the PVA aqueous solution were emulsified under cooling (5 °C) by sonication (60 W for 45 s). The resulting w/o/w emulsion was mechanically stirred (1500 rpm) for at least 1 h (RW20DZM, Janke & Kunkel, IKA-Labortechnik, Staufen, Germany) at room temperature until the complete solvent evaporation.
Cerebrolysin-loaded nanoparticles (C-NPs) were prepared adding to the PLGA organic solution different amounts of freeze-dried cerebrolysin (10, 50, 100, 160 mg achieving a drug/polymer ratio of 1:10, 1:2, 1:1, 1:0.6 w:w, respectively) solubilized in 1 mL of water. Then, the first inner emulsion was formed as previously described. The second emulsion was obtained by using 12 mL of 1 % (w:v) PVA aqueous solution as outer phase with the same sonication conditions previously described. The resulting C-NP samples were named as reported in Table 1. All the loaded and unloaded NP samples were prepared in at least three lots.
Purification and Collection of the NPs
To remove the unloaded drug and the PVA residual from the NPs, all the samples were collected by centrifugation at 15,000 rpm for 10 min (Sorvall RC28S, Dupont, Brussels, Belgium), washed several times with water, and resuspended in water. The purified NP suspensions were freeze dried (−60 °C, 1.10−3 mm/Hg, for 48 h; LyoLab 3000, Heto-Holten, Allerod, Denmark) using trehalose as cryoprotectant (1:1 w:w polymer/trehalose ratio).
The yield of NPs (Yield %) was calculated as the percentage between the weight of the NPs recovered after the freeze-drying procedure and the weight of PLGA and drug used in the preparation process as follows: Yield (%) = (NPs recovered after freeze-dried—anidre trehalose—PVA residue) weight ×100/[(PLGA + cerebrolysin) weight]. All the samples were stored for long-term stability in the dark at the temperature of 4 or 25 °C. Before their use, freeze-dried NPs were weighed and resuspended in water at the concentration of 10 mg/mL (stock solution) by bath sonication for 3 min at r.t.
Morphology of NPs
The surface morphology of NPs was observed by scanning electron microscopy (SEM) (XL-40 Philips, Eindhoven, The Netherlands). Samples were prepared by placing a drop of an aqueous NP suspension (about 10 μg of NPs/mL) on a coverslip adhered to a stub and allowing water to evaporate at r.t. for approximately 24 h. The dried samples were coated under argon atmosphere with a 10-nm gold palladium thickness (Emitech K550 Supper Coated, Emitech Ltd., UK).
Size and Zeta Potential of NPs
Mean particle size (Z-average) and polydispersivity index (PDI) of the NPs were determined at 25 °C using a Zetasizer Nano ZS (Malvern, UK; Laser 4 mW He–Ne, 633 nm, Laser attenuator Automatic, transmission 100–0.0003 %, Detector Avalanche photodiode, Q.E. >50 % at 633 nm, T = 25 °C). Freeze-dried NPs were reconstituted in water (10 μg/mL) and analyzed normalizing the results with respect to a polystyrene standard solution. The zeta potential (ζ-pot) was measured using the same equipment with a combination of laser Doppler velocimetry and phase analysis light scattering (PALS). All the data are expressed as mean of at least three determinations carried out for each preparation lot (three lots for each sample).
Moreover, to evaluate the aggregation phenomena and the destabilization of the preparations, size and ζ-pot measurements were carried out on samples during the storage. Particularly, freeze-dried samples (with and without drug), stored at 4 and 25 °C, were reconstituted and tested at fixed time intervals (1, 3, and 5 months). The size was expressed also as intensity distribution, i.e., the size below which is placed the 10 % [D(10)], 50 % [D(50)], and 90 % [D(90)] of the NPs.
Determination of the Amount of PVA Residual
The residual amount of PVA on the NP surface was determined by a colorimetric method based on the formation of a colored complex between two adjacent hydroxyl groups of PVA and an iodine molecule [22]. Briefly, 5 mg of a freeze-dried NPs sample were solubilized in 1 mL of DCM. Then, 2 mL of water were added and the organic solvent was completely evaporated at r.t. under stirring (about 2 h). The aqueous suspension was filtered (cellulose nitrate filter, porosity 0.45 μm, Sartorius, Firenze, Italy) to remove insoluble PLGA residue. One milliliter of the filtered aqueous solution was treated with 2 mL of 0.5 M NaOH for 15 min at 60 °C. The solution was neutralized with 900 μL of 1 N HCl and the volume adjusted to 5 mL with water. Then, 3 mL of a 0.65 M solution of boric acid, 0.5 mL of a solution of I2/KI (0.05 M/0.15 M), and 1.5 mL of water were added. The PVA concentration was determined spectrophotometrically (Model V-530 Spectrophotometer, Jasco, Easton, MD, USA) at 690 nm after 15 min of incubation at r.t.
Determination of Cerebrolysin Content
Freeze-dried NPs (5 mg) were dissolved in 1 mL of DCM. Then, 3 mL of water was added to extract the cerebrolysin and the organic solvent was evaporated at r.t. under stirring (1500 rpm for at least 1 h; RW20DZM, Janke & Kunkel, IKA-Labortechnik, Staufen, Germany). The aqueous solution was filtered (cellulose acetate filter, porosity 0.2 μm, Sartorius) to remove the polymer residue and spectrophotometrically analyzed at 273 nm to evaluate the cerebrolysin concentration. The drug loading was expressed as milligram of cerebrolysin encapsulated per 100 mg of NPs (cerebrolysin and nanoparticles) and as encapsulation efficiency, i.e., the percentage of encapsulated drug related to the initial amount of drug used in the preparation. Moreover, the drug loss during the storage was evaluated considering the drug content of the freeze-dried NPs stored at 4 and 25 °C for 1, 3, and 5 months. All the data are expressed as the means of at least three determinations carried out for each preparation lot.
In Vitro Drug Release
A membrane diffusion method was used to evaluate the in vitro release of cerebrolysin from NPs. Each sample (60 mg of purified NPs suspended in 1 mL of water) was placed in a dialysis bag (CelluSep MWCO 60 kDa, Membrane Filtration Products, Seguin, TX, USA). The dialysis bag (cutoff 60 Kda), permeable to drug but not to the NPs, was closed at both ends using closure devices (Spectrum Medical Industries, Houston, TX, USA) and placed in 25 mL of PBS pH 7.4 at 37 ± 0.1 °C to be gently shaken at 100 rpm with a magnetic stirrer. At fixed time intervals, an exact volume (2.5 mL) of the receiving phase was withdrawn and the drug content was determined spectrophotometrically at 273 nm. The removed PBS aliquot was immediately replaced with an equal volume of PBS pH 7.4 to keep constant the volume of the receiving phase. The release studies were carried out in triplicate.
Stability of the NPs in Serum
To evaluate the NP stability and simulate their behavior after iv administration, freeze-dried NPs (1.67 mg) were suspended in 0.5 mL of 5, 10, 20, and 50 % v:v fetal bovine serum (FBS) aqueous solutions. The suspensions were incubated at 37 °C, and the size and ζ-pot of the NPs were determined at fixed time intervals (0, 30, 60, 120, and 240 min) in order to assess the aggregations, the change in physical properties (particularly the ζ-pot), and the dimensional growth produced by the deposition of serum proteins on the particles surface.
In Vivo Administration of NPs with Cerebrolysin in Traumatic Brain Injury
To understand the role of nanolabelled cerebrolysin on neuroprotection, we used our traumatic brain injury model in rats (see as follows).
Animals
Experiments were carried out on Sprague Dawley male rats housed at controlled room temperature (21 ± 1 °C) with 12-h light and dark schedule. Food pellets and tap water were provided ad libitum before experiments. All experiments were carried out according to the National Institute of Health (NIH) guidelines for care and handling of experimental animals and approved by Institutional Ethics Committee [12–16].
Traumatic Brain Injury
Traumatic brain injury (TBI) was inflicted in rats under Equithesin anesthesia (3 ml/kg, i.p.) as described earlier [12–16]. In brief, under anesthesia, the skull was opened ascetically and the surface was freed from any underlying skin muscles and dried. A burr hole was made using a dental automatic drill over the right parietal bone (4 mm2) under constant application of cold physiological saline (4 °C) so that the cortical or bone temperature did not rise due to friction of drilling [13, 14]. Extreme care was taken during drilling not to damage dura mater. If the dura was damaged accidently, the animals were not included in subsequent experimental analysis.
After making the circular drill (4 mm2), the skull flap was removed using forceps to avoid underlying cortical damage. The open cortical area was closed with cotton soaked saline at room temperature for 30 min to stabilize the animal from the stress of drilling [12–16].
Under stereotaxic guidance, a 3-mm deep and 4-mm long cortical incision was performed on the open parietal cerebral cortex and the wound is covered with cotton soaked saline [13, 14]. Sham animals were drilled exactly under identical conditions except the lesion was not performed.
A group of intact control rats were used to compare drilling-induced brain damage, if any, using standard procedures [see 12–16].
Cerebrolysin Administration
In control or TBI groups, normal or nanolabeled cerebrolysin was administered in a dose of 5 ml/kg, i.v. 30 min, 1 h, and 2 h after TBI. The animals were allowed to survive 8 h after injury [23–26].
Blood-Brain Barrier Breakdown
The blood-brain barrier (BBB) breakdown to protein tracers, e.g., Evans blue albumin (EBA) and [131]-iodine, was used [27, 28]. These tracers when administered into the circulation will bind to serum proteins. When these tracers are seen in the brain, it means leakage of tracer-protein complex has occurred. Leakage of proteins across the BBB is largely responsible for brain edema formation [29, 30].
Brain Edema Formation
To confirm brain edema formation, brain water content was measured from the differences between wet and dry weight of the brain samples after injury [31]. For this purpose, immediately after the experiment, brain samples from desired regions were taken out and weighed to record their wet weight. After that, the tissue samples were placed in an incubator maintained at 90 °C for 72 h. After this period, the water from the tissue is evaporated completely and the samples were weighed to record their dry weight [32]. The brain water content was calculated from the differences between the wet and dry weights of the samples. In addition, volume swelling from the differences between brain water content in control or experimental animals was calculated according to the formula of Elliott and Jasper (1949) as described earlier [33, 34].
Statistical Analysis
Statistical analysis in this paper was performed using Microsoft Excel for Macintosh and tested for significance using t tests followed by ANOVA with an α level of significance set at 0.05 (p < 0.05).
Results
Effect of PVA Concentration on NPs Formation
Firstly, the investigations were focused on the optimization of the parameters of w/o/w NP preparation. PVA is the surfactant typically employed in the preparation procedure of NPs. The concentration of the water-soluble polymer in the outer phase must be carefully studied because it plays a key role in the achievement of stable emulsions leading to the NP formation. The particle size, PDI, and morphology of the NPs were affected by the variation of the PLGA/PVA ratio and by the volume of the outer phase (Fig. 1). The attempts to obtain a stable nanoemulsion using a 1:0.8 w:w PLGA/PVA ratio was unsuccessful. An improvement of the preparation process was reached using a PLGA/PVA ratio near to 1:1.2 (w:w). This formulative condition with standardized PLGA/PVA ratio leads to the obtainment of the most stable and homogeneous (monomodal peak size) nanoemulsions. Thus, after solvent evaporation, a monodispersed NP population with a homogeneous size distribution, a mean diameter of about 200 nm, a PDI <0.2, and a ζ-pot value of about −20 mV was acquired. These NPs were efficiently purified by centrifugation (7 % w:w of PVA residual) and resuspended with a yield of about 70 %. When the concentration of PVA increases, the yield dropped below 40 %, owing to problems connected to the purification procedure and the recovery by centrifugation. When the 1:2.4 (w:w) PLGA/PVA ratio was used, the PVA residual was about 20 % w:w, even if both NP diameter and PDI values decreased, as the consequence of the favoring effect of PVA on the emulsion.
Effect of Drug/Polymer Ratio on the Formation, Loading, and Release Properties of NPs
The physicochemical characterization data of all NPs are reported in Table 1. The effect of the cerebrolysin/PLGA ratio on drug loading was studied since it is well known that both high amounts of cerebrolysin are necessary for the therapeutic effect and the drug/polymer ratio remarkably impacts on the stability of the encapsulated drug [35]. Therefore, the PLGA/PVA ratio (1:1.2 w:w) and the volume of the outer phase (12 mL) were kept constant whereas the drug/PLGA ratio was changed from 1:10 (w:w) until the unusual 1:0.6 (w:w) ratio.
For all formulations (C-NPs1, C-NPs2, C-NPs3, and C-NPs4), the size generally ranged from 200 to 400 nm (Table 1). Increasing the amount of drug (from C-NPs1 to C-NPs4), the Z-average of NPs linearly increased and the homogeneity of the samples decreased as the PDI and Di90 values show (Table 1). The SEM microphotographs (Fig. 2) revealed that cerebrolysin, being a mix of peptide, was not able to organize itself into a stable matricial structure (Fig. 2a).
NPs with different drug/PLGA ratios exhibited several morphological and structural differences. Spherical NPs with a regular smooth surface were observed when drug/PLGA ratio ranged between 1:10 (w:w) (C-NPs1) and 1:1 (w:w) (C-NPs3) (Fig. 2c, d, respectively). NPs were also formed when the drug/PLGA was drastically increased to 1:0.6 w:w (C-NPs4). However, this experimental condition promoted the formation of a complicated and heterogeneous structure (Fig. 2e, f) produced by a fragmented framework in which the cerebrolysin seems to display some sort of organization. However, this finding could be dependent on an artifact. The sample appeared as a hybrid structure between matricial spheres, characterized by a porous/alveolar structure, and collapsed reservoir systems that can be the consequence of the preparation procedure of the sample for the microscopical analysis.
Moreover, the C-NPs4 ζ-pot value (about −13.0 ± 3 mV) was less negative than that of the unloaded NPs (−20.0 ± 1 mV) and of the C-NPs1, C-NPs2, and C-NPs3 (ζ-pot approximately −16 mV) (Table 1). The increase of the ζ-pot could be the evidence of the presence of an increasing amount of drug adsorbed on the NP surface.
Drug content (mg of drug/100 mg of NPs) increased as the drug/PLGA ratio increased (Fig. 3), while the encapsulation efficiency showed greater variability. The content and the encapsulation efficiency of C-NPs1 (drug/PLGA ratio 1:10 w:w) were approximately 7 ± 1 mg/100 mg (Fig. 3) of NPs and 79 ± 3 %, respectively (Table 1). When the drug/PLGA ratio reached 1:2 w:w (C-NPs2), a limited increase in drug content (10 ± 1 mg/100 mg) was observed while the encapsulation efficiency decreased (31 ± 3 %). These values were observed also in C-NPs3. Using 1:0.6 w:w drug/PLGA ratio (C-NPs4), an adequate loading of drug (24 ± 1 mg/100 mg of NPs) was reached. Cerebrolysin (that was a mixture of peptides very sparingly soluble in water) should be poorly encapsulated in PLGA NPs, but increasing the drug concentration during formulation, a satisfactory amount of drug can be embedded in the NPs as evident in C-NPs4 with the encapsulation efficiency close to 38 ± 2 %. This level of encapsulation efficiency could be justified by hypothesizing that cerebrolysin could be molecularly dispersed in the PLGA matricial structure. After having reached the saturation concentration in the NPs, the excess of cerebrolysin could adhere to the NP surface.
Owing to the suitable drug loading, C-NPs4 sample was selected for the stability studies even if this sample was characterized by a heterogeneous particle population and by the presence of a little amount of unformed PLGA polymer.
In Vitro Release of Cerebrolysin from NPs
The diffusion through a dialysis membrane of the cerebrolysin released from C-NPs4 was compared with the free cerebrolysin diffusion (Fig. 4). The release from NPs showed a first burst period (30 min) during which approximately 40 % of the drug diffused in the receiving phase. After this time period, a slower release was observed. As the diffusion of free drug is very fast, the burst effect could be evidence of the desorption of the drug fraction associated to the surface and not firmly incorporated into the NPs. On the contrary, the controlled profile of release recorded over the second period of time (from 60 min up to 24 h) can be rightly considered as the evidence of the release of the embedded drug from PLGA matrix. This hypothesis is confirmed by the fact that only the 60 % of the entrapped drug diffused after 6 h, while more than 90 % of the free drug reached the acceptor compartment in the same time.
Effect of Trehalose on Reconstitution of the Freeze-Dried NPs
NPs (unloaded NPs and C-NPs4) were lyophilized to improve their long-term stability as the poor stability in aqueous medium of polymeric NPs hampered their clinical application [36]. The hydrophilic layer of PVA residual on the NP surface helps in the reconstitution of the freeze-dried NP dispersion [36, 37]. Our findings showed that the layer of the hydrophilic polymer seems to be adequate to allow unloaded NPs and C-NPs4 to be resuspended after the purification process (Fig. 5a). On the contrary, the layer does not appear satisfactory to avoid NP aggregation after the freeze-drying process. To overcome this drawback, amounts of trehalose ranging from 0.5:1 to 2:1 (w:w) were added to the NP aqueous suspensions before the freeze-drying process. The values of Di and the reproducibility of data of particle size after reconstruction of both freeze-dried free NPs (Fig. 5b, up) and C-NPs4 (Fig. 5b, down) suggested that an adequate dispersion of samples occurred using an 1:1 w:w NP/trehalose ratio.
Long-Term Storage Stability of Freeze-Dried NPs
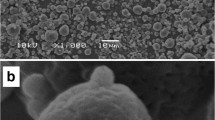
The physical stability of NPs dispersed in water is an essential issue for assuring that the formulation can maintain its properties until their clinical employment. Therefore, it is pivotal for NP application to monitor the size modifications and the loss of the drug produced by the reconstruction after the long-term storage of the freeze-dried NPs. The mean diameter values in reconstituted dispersions of freeze-dried unloaded NPs and C-NPs4 increase as the storage time at 25 °C increases (Fig. 6a). After 3 months, it is extremely difficult to disperse the NPs. In fact, some aggregates are visible yet at the naked eye. The SEM microphotographs (Fig. 6b) showed other typical evidences of destabilization, i.e., a broader size distribution as the increase of the polydispersivity index pointed out (Fig. 6a). After 5 months of storage, a remarkable decrease of the drug content was observed (Fig. 6c) probably as the consequence of the humidity absorption.
a Storage time versus Z-average of free NPs4 and C-NPs4. Samples were freeze dried, stored at 4 and 25 °C for 5 months and reconstituted just before the analysis. PDI values (±SD) were reported for samples stored at 25 °C both at time 0 and 5 months. The analyses were carried out after reconstitution in water. b SEM images of reconstituted C-NPs4 stored for 3 months at 25 °C and c drug content of C-NPs4 during storage both at 4 and 25 °C
When freeze-dried samples were stored at 4 °C, the overall stability was improved as compared to that of NPs stored at 25 °C. After 5 months, the freeze-dried NPs stored at 4 °C were easily resuspended and the chemical-physical parameter (mean diameter, size distribution, etc.) were maintained (Fig. 6a). Also freeze-dried C-NPs4 dispersions were easily reconstructed and the maintenance of an appropriate content (close to 16 mg/100 mg of formulation) was observed. These findings are the evidence of the improving effect of low temperature storage in the protein protection and NP stabilization.
Stability in Serum
To further predict the feasibility of iv administration, the NPs stability in serum was evaluated. In fact, different amounts of serum can modify some characteristics (size, PDI, and ζ-pot) of both the unloaded and cerebrolysin-loaded NPs that are considered as pivotal indicators of the stability of colloidal dispersions [38].
With addition of aqueous solution of serum (time 0), size, PDI, and ζ-pot of unloaded nanoparticles (free NPs) did not change except for Z-average of the suspension in 50 % (v:v) of serum that slightly increased (Fig. 7a). Generally, from 10 to 50 % v:v of serum, the PDI values of the suspensions ranged between 0.2 and 0.1, indicating the maintenance of the homogeneous dispersion characteristics of the NPs.
Serum stability of free NPs (a) and C-NPs4 (b). SEM images describe the C-NPs4 sample after 4 h of incubation on different amounts of serum (10 and 50 % v:v). Legend: □ time 0;  , time 0.5 h;
, time 0.5 h;  time 1 h;
time 1 h;  time 2 h; ■ time 4 h. *p < 0.05 time 0–50 % v:v of serum vs time 0–25 % v:v of serum vs time 0–10 % v:v of serum vs time 0–5 % v:v of serum vs time 0–0 % v:v of serum; #
p < 0.05 time 4 h vs time 0 (related % of serum); ○p < 0.05 time 2 h vs time 0 (related % of serum);
time 2 h; ■ time 4 h. *p < 0.05 time 0–50 % v:v of serum vs time 0–25 % v:v of serum vs time 0–10 % v:v of serum vs time 0–5 % v:v of serum vs time 0–0 % v:v of serum; #
p < 0.05 time 4 h vs time 0 (related % of serum); ○p < 0.05 time 2 h vs time 0 (related % of serum);  p < 0.05 time 1 h vs time 0 (related % of serum);◊ p < 0.05 time 1/2 h vs time 0 (related % of serum); ● p < 0.05 time 4 h vs time 1/2 h (related % of serum); ▲ p < 0.05 time 4 h vs time 1 h (related % of serum); ■ p < 0.05 time 4 h vs time 2 h (related % of serum)
p < 0.05 time 1 h vs time 0 (related % of serum);◊ p < 0.05 time 1/2 h vs time 0 (related % of serum); ● p < 0.05 time 4 h vs time 1/2 h (related % of serum); ▲ p < 0.05 time 4 h vs time 1 h (related % of serum); ■ p < 0.05 time 4 h vs time 2 h (related % of serum)
Similarly, loaded nanoparticles (C-NPs4) were stable in serum (time 0). Also in this case, PDI values ranged between 0.15 and 0.22 until 25 % v:v of serum concentration. A significant increase of PDI value was observed after suspension in high serum concentration (50 % v:v), indicating an initial destabilization of the sample.
The size, PDI value, and ζ-pot of NPs and C-NPs4 were significantly affected by the incubation time, chiefly using high serum concentrations (25–50 % v:v). The unloaded NPs seemed to be more stable than cerebrolysin-loaded NPs during the incubation (Fig. 7). During incubation with 50 % v:v of serum, PDI values of unloaded NPs significantly increased indicating the destabilization of this sample. The exposition of NPs at high serum concentrations modified also the surface properties such as the ζ-pot that shifts to the neutrality value (Fig. 8).
Already with 5 % v:v of serum, significant differences (p < 0.05) were observed for the Z-average values of C-NPs4 detected at the different incubation times. Surprisingly, a remarkable decrease of Z-average was observed during the incubation time of C-NPs4 with low concentrations of serum (5 and 10 % v:v) (Fig. 7b). This finding could be the consequence of the hybrid structure (matrix and reservoir) of the particles along with the high loading (24 mg/100 mg of PLGA) of cerebrolysin forming in part a layer on the NP surface. In fact, the decrease in particle size can be associated to the dissolution of cerebrolysin on the surface and to the collapse the hybrid structure owing to the release of the cerebrolysin embedded. Moreover, the decrease of the diameter of this sample in serum could be the consequence of the osmotic effect exerted by salts in solution. Both these phenomena lead to the “squeeze” of the NPs, not otherwise justifiable, as PLGA is not a swelling polymer. The irregular change of physical properties (shape, porosity, and surface charge) due to these phenomena could be the reason of the wide range of both PDI and ζ-pot values of C-NPs4 observed during the incubation process (Fig. 8).
On the contrary, at 25 and 50 % v:v serum concentrations, the incubation of C-NPs4 produced a significant increase of the Z-average values. In fact, the size increased from 300 ± 17 nm to 361 ± 13 nm already after 2 h reaching 395 ± 32 nm after 4 h of incubation in a 25% v:v serum solution (Fig. 7b). At the same manner, the Z-average of particles increased from 293 ± 20 nm to 399 ± 45 nm during the 4 h of incubation with 50 % v:v of serum.
This increase in particle size and, particularly, the fluctuation of the PDI values owing to the incubation time could be explained by the association and dissociation process of serum protein molecules on the particle surface.
The absorption of serum proteins on the particle surface leads to the slow, but progressive, neutralization of the surface charge of the samples (NPs and C-NPs4) (Fig. 8). The charge neutralization by the macromolecules further reduced the repulsion energy among the NPs. This may also progressively facilitate the agglomeration process promoting the formation of larger structures. The colloidal stability in serum of these nanocarriers determines the successful delivery of protein/peptides preventing particle aggregation or embolism occurring in the systemic circulation [22, 39].
The huge variability in the surface charge after 4 h of incubation can be deduced by the high standard deviations of ζ-pot values. This finding could be described as a consequence of continuous attraction/repulsion processes with positive and negative charges quickly shifting between the particle surface and serum components capable to stabilize the NPs in serum medium.
Effect of PLGA-Labeled Cerebrolysin in Traumatic Brain Injury
Cerebrolysin loaded into PLGA NPs was able to thwart BBB breakdown to EBA and radioiodine most effectively after 8 h of concussive head injury (CHI). This effect was most marked in the right injured cortex as compared to the left uninjured side. The effect of nanolabeled cerebrolysin was evident when the drug was administered even 4 h after TBI (Table 2). On the other hand, normal cerebrolysin administration was able to thwart edema formation and the BBB breakdown when the drug was given 30 min to 1 h after TBI (Table 2). Untreated traumatized rats showed a progressive breakdown of the BBB and edema formation in both the half after TBI from 1 to 8 h after trauma (Table 2).
Discussion
Traumatic brain injury is a serious clinical situation for which no suitable therapeutic strategies have been developed so far. Thus, there is an urgent need to explore suitable drug therapy and/or its delivery in adequate quantity to the brain to achieve good neuroprotection. Our laboratory is involved in development of suitable therapeutic strategies using nanodrug delivery to the CNS in various diseases conditions in animal models including TBI [12–16, 27–37].
As nanodrug delivery could be obtained by a number of approaches (as examples, nanowired or encapsulation into soft nanoparticles). A major issue would be to compare the effect/benefit of different drug delivery strategies on the same injury model [23–25]. In a neurotrauma model, for example, cerebrolysin was not shown to be efficient in neuroprotection when formulated into TiO2 nanowires [see 27, 28]. Thus, in this paper, we can compare these above-mentioned results with the delivery of cerebrolysin by means of encapsulation into PLGA NPs. Thus, a possibility exists whether PLGA delivery of cerebrolysin could also achieve similar neuroprotection in TBI. Previous observation showed that PLGA-nanolabeled cerebrolysin is quite effective in reducing CHI in our rat model [24]. In this investigation, we for the first time examined in details the storage and other physicochemical factors of PLGA-labeled cerebrolysin and its stability in plasma that is needed for good drug delivery to the brain.
The salient novel findings in this investigation clearly show that PLGA-labeled cerebrolysin is able to reduce TBI-induced brain edema and BBB breakdown in rats 8 h after injury. (Table 2). Moreover, PLGA-labeled cerebrolysin is effective even if administered 4 h after TBI to induce neuroprotection at 8 h after injury, whereas normal cerebrolysin delivered in identical conditions was not that effective. This finding is relevant and strongly suggests that cerebrolysin loaded into PLGA NPs should need at least a few hours to treat TBI cases in clinical situations as well. For this purpose, the details of physicochemical properties of PLGA-labeled cerebrolysin are needed.
Thus, in this study, influence of formulative variables on the efficiency of cerebrolysin encapsulation in PLGA NPs produced by w/o/w double emulsion method was investigated. Preliminary results highlighted a remarkable influence of the nature and concentration of surfactant (PLGA/PVA ratio of 1:1.2 w:w) and volume of the outer aqueous phase on the formulability, size, and recovery of PLGA NPs.
To achieve a more efficient encapsulation of cerebrolysin, the ratio between drug and polymer should be increased up to 1:0.6 (C-NPs4), creating systems in which the polymer and the protein formed a complicated matrix. The release of the drug from these particles appeared to be biphasic due to the initial desorption of drug from the surface of NPs and the subsequent prolonged release of the drug embedded in the matrix.
Moreover, aiming to both design standardized and optimized nanoformulation and to clarify the fate of these nanodevices after administration, the colloidal stability of C-NPs4 (long-term stability) and in biological environment (serum) is a critical issue [40]. For this reason, long-term stability was evaluated in water on freeze-dried product stored for 3 months both at 4 and 25 °C and reconstituted only before the analysis. On the contrary, the stability in serum was evaluated for 4 h, i.e., for the time of persistence in the blood stream. While freeze-dried C-NPs4 remained stable during storage at 4 °C for 5 months, the same NPs stored at 25 °C modified and aggregated with loss of drug. Also in serum, the equilibrium due to absorption/desorption of serum proteins on NPs surface decreased during the 4 h of experiments leading to variability and instability of colloidal systems. Moreover, these data confirmed that PCS, combined with SEM analysis, is a powerful tool to evaluate NP colloidal stability during in vitro experiments.
How is cerebrolysin able to reduce brain edema formation and/or BBB breakdown in TBI? This is not well known from our investigation [23–26]. However, available evidences suggests that cerebrolysin could induce neuroprotection or neurorepair because of exogenous supply of selective neurotrophic factors, e.g., brain-derived neurotrophic factor (BDNF), glial-derived neurotrophic factor (GDNF), nerve growth factor (NGF), and insulin-like growth factor 1 (IGF-1) along with many active peptide fragments needed for nutrition of neurons and glial cells [23–26]. Since TBI results in reduction in several neurotrophic factors, exogenous supplement of needed growth factors will help in neuroprotection after TBI.
Interestingly, PLGA-labeled cerebrolysin was most effective in reducing the TBI pathology after injury, a feature that was not seen effectively by normal cerebrolysin given alone. This suggests that nanodelivery of cerebrolysin has superior effects in TBI compared to normal cerebrolysin alone.
What are the possible mechanisms of nanodelivered cerebrolysin in inducing superior neuroprotective effects in TBI? The answer to this question is not apparent from this investigation. However, it appears that cerebrolysin-loaded NPs could rapidly access into the brain up to an efficacious amount and there produce a prolonged release of its content, i.e., cerebrolysin. This effect was reached after a single administration, but it could be also improved by using a constant infusion pump that may help in obtaining a better neurotherapeutic effect of cerebrolysin-loaded PLGA NPs in comparison with free drug [see 27–29]. Another key factor for superior neuroprotective effects of PLGA-labeled cerebrolysin could be due to the fact that nanolabeled cerebrolysin is more resistant to degradation by endogenous biological enzymes because of the drug binding with the nanoparticles [23–26]. This could be one of the reasons that even the PLGA-labeled cerebrolysin was given 4 h after the nanodrug complex effectively reduced the brain pathology after TBI at 8 h period.
Conclusions
In conclusion, our results show that cerebrolysin-loaded PLGA NPs is very stable in the circulation and has superior neuroprotective effects in TBI as compared to normal cerebrolysin. Our investigation thus opens a new avenue supporting the idea that cerebrolysin-loaded PLGA NPs could easily be used in clinical condition to treat TBI cases. However, further studies on long-term and repeated use of cerebrolysin-loaded PLGA NPs are needed to further confirm this point. Additionally, neurotoxicity of cerebrolysin-loaded PLGA NPs also needs to be evaluated before this combination could be used in clinical situation in patients.
References
Ruozi B, Belletti D, Bondioli L, De Vita A, Forni F, Vandelli MA, Tosi G (2012) Neurotrophic factors and neurodegenerative diseases: a delivery issue. Int Rev Neurobiol 102:207–247
Sharma HS, Johanson CE (2007) Intracerebroventricularly administered neurotrophins attenuate blood–cerebrospinal fluid barrier breakdown and brain pathology following whole-body hyperthermia an experimental study in the rat using biochemical and morphological approaches. Ann NY Acad Sci 1122:112–129
Sharma HS, Zimmermann-Meinzingen S, Johanson CE (2010) Cerebrolysin reduces blood-cerebrospinal fluid barrier permeability change, brain pathology, and functional deficits following traumatic brain injury in the rat. Ann NY Acad Sci 1199:125–137
Sharma HS, Zimmermann-Meinzingen S, Johanson CE (2010) Cerebrolysin attenuates blood-brain barrier and brain pathology following whole body hyperthermia in the rat. Acta Neurochir Suppl 106:321–325
Hartbauer M, Hutter-Paier B, Skofitsch G, Windisch M (2001) Antiapoptotic effects of the peptidergic drug cerebrolysin on primary cultures of embryonic chick cortical neurons. J Neural Transm 108:459–473
Feczkó T, Toth J, Dosa G, Gyensis J (2011) Optimization of protein encapsulation in PLGA nanoparticles. Chem Eng Process 50:757–765
Costantino L, Gandolfi F, Tosi G, Rivasi F, Vandelli MA, Forni F (2005) Peptide-derivatized biodegradable nanoparticles able to cross the blood brain barrier. J Control Release 108:84–96
Tosi G, Vergoni AV, Ruozi B, Bondioli L, Badiali L, Rivasi F, Costantino L, Forni F, Vandelli MA (2010) Sialic-acid and glycopeptides conjugated PLGA nanoparticles for central nervous system targeting: in vivo pharmacological evidence and biodistribution. J Control Release 145:49–57
Tosi G, Badiali L, Ruozi B, Vergoni AV, Bondioli L, Ferrari A, Rivasi F, Forni F, Vandelli MA (2012) Can Leptin-derived sequence-modified nanoparticles be suitable tools for brain delivery? Nanomedicine 7:365–382
Zhang Y, Chan HF, Leong KW (2013) Advanced materials and processing for drug delivery: the past and the future. Adv Drug Deliv Rev 65:104–120
Naahidi S, Jafari M, Edalat F, Raymond K, Khademhosseini A, Chen P (2013) Biocompatibility of engineered nanoparticles for drug delivery. J Control Release 166:182–194
Sharma HS (2010) Selected combination of neurotrophins potentiate neuroprotection and functional recovery following spinal cord injury in the rat. Acta Neurochir Suppl 106:295–300
Dey PK, Sharma HS (1983) Ambient temperature and development of traumatic brain oedema in anaesthetized animals. Indian J Med Res 77:554–563
Mohanty S, Dey PK, Sharma HS, Singh S, Chansouria JP, Olsson Y (1989) Role of histamine in traumatic brain edema. An experimental study in the rat. J Neurol Sci 90:87–97
Sharma HS, Wiklund L, Badgaiyan RD, Mohanty S, Alm P (2006) Intracerebral administration of neuronal nitric oxide synthase antiserum attenuates traumatic brain injury-induced blood-brain barrier permeability, brain edema formation, and sensory motor disturbances in the rat. Acta Neurochir Suppl 96:288–294
Sharma HS (2004) Influence of serotonin on the blood-brain and blood-spinal cord barriers. In: Sharma HS, Westman J (eds) The blood-spinal cord and brain barriers in health and disease. Elsevier Academic Press, San Diego, pp 117–158
Liu W, Leng H, Zhu Z, Chen G (2001) Analysis of the content of ten kinds of metal elements in cerebrolysin by atomic absorption spectrophotometry. Guang Pu Xue Yu Guang Pu Fen Xi 21:397–399
Gromova OA, Kudrin AV, Kataev SI, Mazina SS, Volkov A (2003) Effects of cerebrolysin on trace element homeostasis in the brain. Zh Nevrol Psikhiatr Im SS Korsakova 103:59–61
Bodmeier R, McGinity RW (1987) The preparation and evaluation of drug containing poly(dl-lactide) microspheres formed by the solvent evaporation method. Pharm Res 4:465–471
Rosca ID, Watari F, Uo M (2004) Microparticle formation and its mechanism in single and double emulsion solvent evaporation. J Control Release 99:271–280
Belletti D, Tosi G, Forni F, Gamberini MC, Baraldi C, Vandelli MA, Ruozi B (2012) Chemico-physical investigation of tenofovir loaded polymeric nanoparticles. Int J Pharm 436:753–763
Heurtault B, Saulnier P, Pech B, Proust JE, Benoit JP (2003) Physico-chemical stability of colloidal lipid particles. Biomaterials 24:4283–4300
Dobson J (2006) Gene therapy progress and prospects: magnetic nanoparticle-based gene delivery. Gene Ther 13:283–287
Sharma HS, Sharma A, Mössler H, Muresanu DF (2012) Neuroprotective effects of cerebrolysin, a combination of different active fragments of neurotrophic factors and peptides on the whole body hyperthermia-induced neurotoxicity: modulatory roles of co-morbidity factors and nanoparticle intoxication. Int Rev Neurobiol 102:249–276
Ruozi B, Belletti D, Forni F, Sharma A, Muresanu DF, Mossler H, Vandelli MA, Tosi G, Sharma HS (2014) Poly (D, L-lactide-co-glycolide) nanoparticles loaded with cerebrolysin display neuroprotective activity in a rat model of concussive head injury. CNS Neurol Disord Drug Targets 13:1475–1482
Sharma HS, Menon PK, Lafuente JV, Aguilar ZP, Wang YA, Muresanu DF, Mössler H, Patnaik R, Sharma A (2014) The role of functionalized magnetic iron oxide nanoparticles in the central nervous system injury and repair: new potentials for neuroprotection with cerebrolysin therapy. J Nanosci Nanotechnol 14:577–595
Sharma A, Muresanu DF, Mössler H, Sharma HS (2012) Superior neuroprotective effects of cerebrolysin in nanoparticle-induced exacerbation of hyperthermia-induced brain pathology. CNS Neurol Disord Drug Targets 11:7–25
Sharma HS, Dey PK (1986) Influence of long-term immobilization stress on regional blood-brain barrier permeability, cerebral blood flow and 5-HT level in conscious normotensive young rats. J Neurol Sci 72:61–76
Sharma HS, Dey PK (1986) Probable involvement of 5-hydroxytryptamine in increased permeability of blood-brain barrier under heat stress in young rats. Neuropharmacology 25:161–167
Sharma HS, Dey PK (1987) Influence of long-term acute heat exposure on regional blood-brain barrier permeability, cerebral blood flow and 5-HT level in conscious normotensive young rats. Brain Res 424:153–162
Sharma HS (1987) Effect of captopril (a converting enzyme inhibitor) on blood-brain barrier permeability and cerebral blood flow in normotensive rats. Neuropharmacology 26:85–92
Sharma HS, Olsson Y (1990) Edema formation and cellular alterations following spinal cord injury in the rat and their modification with p-chlorophenylalanine. Acta Neuropathol 79:604–610
Sharma HS (2007) Methods to produce hyperthermia-induced brain dysfunction. Prog Brain Res 162:173–199
Sharma HS, Olsson Y, Persson S, Nyberg F (1995) Trauma-induced opening of the blood-spinal cord barrier is reduced by indomethacin, an inhibitor of prostaglandin biosynthesis. Experimental observations in the rat using [131I]-sodium, Evans blue and lanthanum as tracers. Restor Neurol Neurosci 7:207–215
Joshi DP, Lan-Chun-Fung YL, Pritchard JG (1979) Determination of poly (vinyl alcohol) via its complex with boric acid and iodine. Anal Chim Acta 104:153–160
Biswal I, Dinda A, Das D, Si S, Chowdary KA (2011) Encapsulation protocol for highly hydrophilic drug using non biodegradable polymer. Int J Pharm Pharm Sci 3:256–259
Abdelwahed W, Degobert G, Stainmesse S, Fessi H (2006) Freeze-drying of nanoparticles: formulation, process and storage considerations. Adv Drug Deliv Rev 58:1688–1713
Menon JU, Kona S, Wadajkar AS, Desai F, Vadla A, Nguyen KT (2012) Effects of surfactants on the properties of PLGA nanoparticles. J Biomed Mater Res A 100:1998–2005
Elliott KA, Jasper HH (1949) Measurement of experimentally induced brain swelling and shrinkage. Am J Physiol 157:122–129
Katas H, Hussain Z, Awang SA (2013) Bovine serum albumin-loaded chitosan/dextran nanoparticles: preparation and evaluation of ex vivo colloidal stability in serum. J Nanomater. doi:10.1155/2013/536291
Acknowledgments
This investigation is supported in part by grants from the Air Force Office of Scientific Research (EOARD, London, UK), and Air Force Material Command, USAF, under grant number FA8655-05-1-3065; Swedish Medical Research Council (Nr 2710-HSS), Swedish Strategic Research Foundation, Stockholm, Sweden; Göran Gustafsson Foundation, Stockholm, Sweden (HSS), Astra Zeneca, Mölndal, Sweden (HSS/AS), The University Grants Commission, New Delhi, India (HSS/AS), Ministry of Science and Technology, Govt. of India and Govt. of Sweden (HSS/AS), Indian Medical Research Council, New Delhi, India (HSS/AS); and India-EU Research Co-operation Program (AS/HSS).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ruozi, B., Belletti, D., Sharma, H.S. et al. PLGA Nanoparticles Loaded Cerebrolysin: Studies on Their Preparation and Investigation of the Effect of Storage and Serum Stability with Reference to Traumatic Brain Injury. Mol Neurobiol 52, 899–912 (2015). https://doi.org/10.1007/s12035-015-9235-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-015-9235-x