Abstract
Biomarkers in blood have become increasingly appreciated in the diagnosis of glioma, but most of their diagnostic accuracy was not high enough to be used widely in a clinical context. MicroRNA-125b (miRNA-125b, miR-125b), a member of microRNA cluster, is widely considered as ideal biomarkers for clinical diagnosis in various human cancers. In the current study, we first explored the diagnostic value of serum miR-125b for glioma in a Chinese population, which has not been studied yet. Additionally, we conducted a meta-analysis to assess the diagnostic accuracy of miR-125b in human cancers. Serum miR-125b from the 33 patients with glioma (WHO grades I–IV) and 33 healthy controls were compared. Our results showed that the serum miR-125b level was significantly lower in glioma patients when compared with normal population, and an obvious decreasing trend of miR-125b level along tumor stages was found. The receiver operating characteristic (ROC) curve analysis of the accuracy in distinguishing glioma cancer patients from healthy controls yielded an area under the curve (AUC) value of 0.839 (95 % confidence interval (CI), 0.743–0.935). When glioma patients at different stages were compared with normal controls, the AUC values of WHO grade II (0.868) and WHO grade III–IV (0.959) were higher than WHO grade I (0.691). In the meta-analysis, the overall sensitivity, specificity, and AUC for miR-125b in human cancers diagnosis were 82 % (95 % CI, 76–87 %), 77 % (95 % CI, 70–84 %), and 0.84 (95 % CI, 0.81–0.87), respectively. The results of the present study suggested that miR-125b could be a potential biomarker with relatively high accuracy in the diagnosis of glioma as well as other human cancers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glioma accounts the cases of 40 % central nervous system cancers, whose morbidity reaches approximately 3.7 (male) and 2.6 (female) in every 100,000 people across the world [1, 2]. Among cancer-related deaths below the age of 70 per year, 7 % were caused by glioma [3]. Glioma can be histologically divided into grade I to IV in accordance with the World Health Organization (WHO) criterion [4]. The high mortality rate of glioma is considered to be related with late diagnosis at advanced stages, especially glioblastoma. Since the conventional therapies cannot be proven effective and glioblastoma has its infiltrative development pattern, the disease remains a clinical challenge with the median survival of only 12–15 months and a relatively low overall 5-year survival rate less than 9.8 % over the last decade [2]. However, early detection of glioma can reduce the mortality to a low level; thus, diagnostic methods with high accuracy are urgently needed for glioma patients.
Neuroimaging is a conventional method considered as gold standard for glioma detection, especially magnetic resonance imaging (MRI), which relies primarily on the observation of morphological features of tumors specimens. Although this imaging technique can be used in early stage diagnosis, it usually cannot provide reliable conclusion for glioma diagnosis and stage determination [5]. Besides, the expensive costs also hinder the widespread clinical application of MRI in clinical diagnosis. Over the last decades, biomarkers including proteins, DNA, and RNA markers have gained a lot of popularity in medical research and were used as indicators to monitor the glioma development. The most common used biomarkers are some proteins like cancer antigen-125 (CA-125), cytokeratin-21 fragment (CYFRA21-1), and carcinoembryonic antigen (CEA), which are supposed to be less invasive. However, the diagnostic performances of these biomarkers are unsatisfactory [6]. Recent studies have found some novel potential biomarkers, but their diagnostic accuracy remains to be further confirmed [7–9]. The restrictions of the present methods and the limited accuracy of current biomarkers force us to find more effective and less invasive biomarkers for early diagnosis of glioma, and microRNAs (miRNAs) may be such ideal biomarkers.
MiRNAs are a family of short non-coding RNA with 18–22 nucleotides at length, which function in regulation of gene expression and are involved in a variety of physiological processes, such as cellular proliferation, differentiation, and apoptosis [10]. Studies have indicated that the expression of miRNAs is implicated in tumor growth and carcinogenesis with a tissue-specific expression pattern [11, 12]. The significant role of miRNAs in the progression of human cancers, including glioma, makes them novel and important biomarkers to distinguish patients from healthy controls [13]. In addition, the high stability of miRNAs facilitates clinical cancer diagnosis. Moreover, miRNA can be found in various specimens including blood, tissue, urine, etc. and can be easily and accurately measured even in a very small quantity [14]. In general, miRNAs could be a promising diagnostic tool for early glioma detection according to the findings mentioned above.
In recent years, accumulating studies have implied the possible connection between the irregular expression of microRNA-125b (miRNA-125b, miR-125b) and several types of cancers. One of these studies conducted by Mar-Aguilar et al. in 2013 proved that miR-125b can be a useful biomarker with high sensitivity and specificity in breast cancer diagnosis [15]. Another study suggested that overexpression of miR-125b was detected as a potential diagnostic tool for thyroid cancer [16]. Besides, miR-125b was also employed as a novel marker for the screening of non-small cell lung cancer and bladder cancer [17, 18]. However, there is no study focusing on the efficiency of miR-125b expression in detecting glioma so far. Since miR-125b evenly exists in astrocytes and neurons, this study was performed in order to explore the potential of miR-125b profiling in initial screening process for glioma [19]. Additionally, we conducted a meta-analysis assessing the diagnostic accuracy of miR-125b in cancer diagnosis.
The individual studies concentrating on miR-125b assay in several types of cancer detection have not arrived at a consistent conclusion in diagnostic accuracy. In some studies, a relatively high accuracy was found. For instance, Si et al. reported a sensitivity of 88 % and a specificity of 90 % by using miR-125b as biomarker for breast cancer diagnosis, and Mar-Aguilar found a sensitivity of 88.9 % and a specificity of 80 % in breast cancer detection [20, 14]. However, Vriens et al. found that employing tissue miR-125b as a biomarker for early stage thyroid cancer only produced a sensitivity of 63 % and a specificity of 72 %, and a specificity of 66.4 % was found for lung cancer in study by Ma et al. [16, 21]. Therefore, the meta-analysis was conducted after reviewing all the qualified diagnostic test studies, and we hoped to evaluate comprehensively the efficacy of miR-125b as a biomarker applied in various cancer detection.
Materials and Methods
Ethics Statement
We conducted this study by following the international ethical guidelines for biomedical research involving human subjects, and we also conformed to the agreement drawn up by Ethics Committee of Shengjing Hospital of China Medical University [22]. Every patient participated in the investigation gave us written informed consent before sample collections under the approval of the local institutional review board.
Study Design and Patients
The whole study was developed in two stages as follows. The first stage was performed to explore the potential of serum miR-125b as a biomarker in initial screening process for glioma in serum. Consecutive serum specimens were collected between April 2013 and July 2014 from 33 glioma patients and 33 healthy controls, and more details about the participants are listed in Table 1. The 33 patients were diagnosed and graded by gold method in accordance with the classification of WHO criteria, including 11 WHO grade I patients, 11 WHO grade II patients, and 11 WHO grades III–IV patients [4]. The non-cancer control population comprised 33 normal individuals of matched age, gender, and habits to patients recruited, without any signs and history of cancer.
In the second stage of our study, we conducted a meta-analysis to assess the diagnostic accuracy of miR-125b assay in various cancer diagnoses. We perform a computerized literature search in international databases (PubMed, Web of Science, the Cochrane Library, and Embase) and three Chinese databases (Chinese Biology Medicine, Chinese National Knowledge Infrastructure, and Wan Fang) for related articles published before August 12, 2014 without restrictions in language. Qualified articles should meet some inclusion criteria as follows: (1) focusing on the diagnostic value of miR-125b assay for human cancers; (2) involving sufficient number of subjects; (3) involving cancer patients confirmed by “gold standard” examinations; and (4) providing necessary unreplicated data for rebuilding the diagnostic 2 × 2 table and obtaining sensitivity and specificity (Table 2).
Sample Processing and MiRNA Extraction
For the purpose of measuring the differential expression of serum miR-125b in glioma cancer cases and normal controls, we utilize PAXgene Blood RNA tubes (BD Biosciences, Basel, Switzerland) to extract the sample blood, and 100-μm blood was collected for each subjects. The sample collection was conducted before radiotherapy, chemotherapy, or surgery, and intracranial lesions were left out of our study. The specimens were kept under room temperature within 45 min and then centrifuged at 2500g for 15 min at 4 °C. Serum in supernatants was reserved after temperature plummet at −80 °C in a tube until RNA extraction. The miRNeasy kit (Qiagen GmbH, Hombrechtikon, Switzerland) was used along with the manufacturer’s instruction to extract serum RNA [23]. Quantitative reverse transcription polymerase chain reaction (qRT-PCR) was then performed by employing a 7500 teal-time PCR system (Applied Biosystems). We analyzed the expression levels of the serum miR-125b by calculating Ct values as well as standard deviations by means of comparative cycle threshold (Ct) method. The quantity of target miRNA (miR-125b) was normalized corresponding to that of miR-24, which was selected as control miRNAs. The fold change was calculated according to the equation 2−△△Ct. The higher Ct value corresponds to the lower expression level of miR-125b. All the experiments were run in triplicate.
Statistical Analysis
In the first stage, GraphPad Prism 5 software was used to perform statistical analysis. Data were presented as the mean ± SD for the level of serum miR-125b. Significance of expression level of serum miR-125b between glioma cases and healthy controls was analyzed by using student’s t test or Mann–Whitney. Comparisons between more than two groups were performed using one-way analysis of variance (ANOVA), and the differences between groups were subsequently determined by the Fisher LSD test when appropriate. Two sides of P values were shown, and the result was considered statistically significant when P < 0.05. The standard formulas were referred to when calculating the sensitivity and specificity. The receiver operating characteristic (ROC) curves were constructed to calculate the area under the ROC curve (AUC) and assess the predictive power of serum miR-125b for glioma. The optimum sensitivity and specificity generated by ROC curves were resolved by a cost ratio and pre-test probability.
In meta-analysis, all statistical analyses were performed using STATA 12.0 statistical software [24]. We employed bivariate regression model to measure following parameters with their 95 % confidence intervals (95 % CIs): sensitivity, specificity, the positive likelihood ratio (PLR), diagnostic odds ratio (DOR), and negative likelihood ratio (NLR) [25–27]. The sensitivity and specificity of single study were used to plot the summary receiver operator characteristic (SROC) curve and calculate the corresponding area under the SROC curve (AUC) [28]. Furthermore, we also assessed publication bias by using Deeks’ funnel plots as a concern for meta-analyses of diagnostic studies, and the Fagan’s nomogram was depicted for calculating post-test probabilities [29].
Results
Baseline Characteristics of Patients
As shown in Table 1, a total of 33 glioma patients and 33 normal controls were selected. All of these 33 patients with glioma were histopathologically diagnosed with glioma by brain biopsy. As for three groups of patients with different grade of glioma (WHO grade I, II, and III–IV), each group includes 11 subjects. Before we started the process of sampling, the patients with glioma were newly diagnosed and confirmed. The mean age of control population and glioma study population are 43.7 and 44.5, respectively, and the sex ratio is basically matched. We also investigated habits (alcohol drinking and cigarette smoking), neurological disorders, and family history in all subjects, and no remarkable difference was observed between groups.
Expression Level of Serum miR-125b in Glioma and Healthy Subjects
We conducted a pilot study to select internal control miRNA from several candidate miRNAs (miR-15, miR-21, miR-24, miR-92, miR-145, and miR-221) by quantitative RT-PCR. The Ct values in glioma cases with grades I, II, III–IV, and normal cases of each candidate miRNA were recorded. The results of serum miR-24 assay showed a stabilized concentration without any noteworthy variation between healthy controls and cancer cases in any stages. Therefore, miR-24 was selected as an internal control for the normalization of miR-125b.
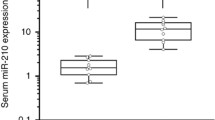
Figure 1 shows the expression level of serum miR-125b in glioma patients and controls. By quantitative RT-PCR, the median relative Ct values of miR-125b were 0.971 and 0.812 in normal cases and glioma cases, and median values in patients with grades I, II, and III–IV glioma were 0.882, 0.772, and 0.695, respectively. Consequently, serum miR-125b level was significantly higher in normal population than in glioma patients (P < 0.001). Relations between serum miR-125b level and stages of glioma were examined when patients separated based on WHO grades, and the gradual decrease in miR-125b levels was clearly discernible as the stage rose. Although expression values of serum miR-125b did not differ significantly between WHO grade I glioma and controls, it was decreased notably for patients with WHO grades II–IV compared with that in healthy people (P < 0.001).
Diagnostic Accuracy of Serum miR-125b in Glioma
In the next step, the ROC curve analysis was performed to assess potential usefulness of serum miR-125b as a noninvasive biomarker for glioma. As shown in Fig. 2, for identifying all glioma cancer patients from healthy controls, the sensitivity and specificity were 78.79 and 75.76 % and an AUC yielded a value of 0.839 (95 % CI, 0.743–0.935). We also explored whether serum miR-125b could distinguish glioma patients with different stages. The ROC curve results indicated a significant increase of AUC as the stages rose. The values went up from 0.691 to 0.868 for WHO grades I and II, and WHO grades III–IV had reached a very high level of an AUC value at 0.959, which suggest a towering diagnostic accuracy. Correspondingly, the sensitivity and specificity were 72.73 and 66.67 % for WHO I grade, 81.82 and 75.76 % for WHO II grade, 90.91 and 87.88 % for WHO grades III–IV.
Diagnostic Performance of miR-125b With Various Cancers in Meta-Analysis
In our meta-analysis, 695 patients with various kinds of cancers and 370 healthy controls from 8 qualified studies (including our study of glioma) were adopted to further examine the diagnostic accuracy of miR-125b in cancer detection [14–18, 20, 21]. The overall sensitivity and specificity were 82 % (95 % CI, 76–87 %) and 77 % (95 % CI, 70–84 %), respectively. Other overall parameters calculated were pooled PLR, 3.5 (95 % CI, 2.5–4.8), NLR, 0.23 (95 % CI, 0.16–0.33), and DOR, 15 (95 % CI, 8–28). Furthermore, we generated the SROC curve. The value of AUC was 0.84, and its 95 % CI was 0.81–0.87 (Fig. 3). The relative high AUC implied that miR-125b had a good level of overall correctness. Goodness of fit and bivariate normality analyses (Fig. 4a, b) suggested each included study had only minimal influence on the overall estimates. Influence analysis (Fig. 4c) and outlier detection (Fig. 4d) identified no outlier studies. Besides, the Deeks’ funnel plot asymmetry test was used and a P value of 0.2, suggesting no significant publication bias. Figure 5 depicted the Fagan’s nomogram, which describes how to use diagnostic finding from miR-125b assay to calculate post-test probability of cancers. Specifically, for any people with a pre-test probability of 25 % to have cancers, if a positive result with PLR value at 3, the post-test probability to have cancers would rise to 54 %; by contrast, a negative result with NLR value at 0.23 would lower the post-test probability to 7 % in the same condition.
Discussion
Glioma is a representative central nervous system cancer with a quite low 5-year survival rate as the grade gets higher, especially in WHO grades III–IV. Conventional method for glioma detection is neuroimaging, which is considered as gold standard but can hardly avoid limitations such as invasive process, expensive cost, and unwarrantable accuracy. To overcome these shortcomings, biomarkers in blood have become a hot research field. Since most current protein biomarkers cannot reach certain level of sensitivities or specificities, miRNAs are widely studied as ideal biomarkers for clinical applications which can be sampled noninvasively and cost-effectively. Among these miRNAs, miR-125b has been recently searched and irregular expression was found in various cancers. Nevertheless, we haven’t found any study concerning the diagnostic efficiency of miR-125b assay in glioma detection. Consequently, the first stage present study was performed to explore the potential of serum miR-125b profiling in initial screening process for glioma.
In our study, the promising role of serum miR-125b in glioma diagnosis were supported by the evidence that the expression level of serum miR-125b decreased notably in glioma patients compared with healthy controls. Besides, the expression level declined as stages went higher, and the level of WHO II/III–IV became fairly low compared with that of normal cases (both P < 0.001), which indicated a desired discriminating power of serum miR-125b in glioma patients especially at upper-middle stages. Furthermore, we generated ROC curves to examine the diagnostic value of serum miR-125b for glioma in different stages. The AUC displayed a global summary of the trial performance, and the value of 0.839 in all glioma patients shown a relatively fine overall accuracy in diagnosis. When WHO grades I, II, and III–IV glioma patients were compared with normal population, the AUC yielded a value of 0.691, 0.868, and 0.959, respectively. The markedly high AUC values of WHO grades II–IV particularly (associated with 90.91 % sensitivity and 87.88 % specificity for WHO grades III–IV) demonstrated the accuracy of serum miR-125b as a steady biomarker in stratifying glioma patients. All in all, the results of our analysis here are clinically meaningful, showing that serum miR-125b could diagnose patients with glioma in a relatively high accuracy especially at upper-middle stages.
Furthermore, the meta-analysis was conducted to assess the diagnostic accuracy of miR-125b in cancer diagnosis. Overall, the results revealed that employing miR-125b as biomarkers for cancer detection achieved a summary sensitivity of 82 % (95 % CI, 76–87 %), specificity of 77 % (95 % CI, 70–84 %), which may turn out 18 % false-negative and 24 % false-positive test results but is more accurate than other conventional biomarkers. The high AUC of 0.84 reflects an overall high level of diagnostic accuracy. We also obtained the pooled PLR and NLR, the values of which were 3.5 and 0.23, respectively. These two likelihood ratios are considered clinically meaningful, which represent that the cancer patients commit a 3.5-fold higher chance of being miR-125b assay-positive than healthy controls, and a miR-125b assay-negative result is 23 % likely to be a false-negative, showing a moderate ability for clinical discrimination. Plus, the Fagan’s nomogram showed the importance of miR-125b assay as initial screening method to calculate post-test probabilities of cancers. Taken together, miR-125b can be employed as invasive and efficient clinical biomarkers with a comparative correctness in cancer diagnosis.
In summary, we have defined the first serum miR-125b signature in glioma. Our results suggested that serum miR-125b may serve as a platform for glioma biomarker development, especially for WHO grades II–IV glioma. Furthermore, results from present meta-analysis also suggested that the miR-125b could be a potential biomarker with relatively high accuracy in the diagnosis of other human cancers.
References
Parkin DM, Pisani P, Ferlay J (1999) Global cancer statistics. CA: Cancer J Clin 49(1):33–64, 31
Turner JD, Williamson R, Almefty KK, Nakaji P, Porter R, Tse V, Kalani MY (2010) The many roles of microRNAs in brain tumor biology. Neurosurg Focus 28(1):E3. doi:10.3171/2009.10.FOCUS09207
Gladson CL, Prayson RA, Liu WM (2010) The pathobiology of glioma tumors. Annu Rev Pathol 5:33–50. doi:10.1146/annurev-pathol-121808-102109
Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, Scheithauer BW, Kleihues P (2007) The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol 114(2):97–109. doi:10.1007/s00401-007-0243-4
Ilhan-Mutlu A, Wagner L, Preusser M (2013) Circulating biomarkers of CNS tumors: an update. Biomark Med 7(2):267–285. doi:10.2217/bmm.13.12
Mann DV, Edwards R, Ho S, Lau WY, Glazer G (2000) Elevated tumour marker CA19-9: clinical interpretation and influence of obstructive jaundice. Eur J Surg Oncol: J Eur Soc Surg Oncol Br Assoc Surg Oncol 26(5):474–479. doi:10.1053/ejso.1999.0925
Roy S, Josephson SA, Fridlyand J, Karch J, Kadoch C, Karrim J, Damon L, Treseler P, Kunwar S, Shuman MA, Jones T, Becker CH, Schulman H, Rubenstein JL (2008) Protein biomarker identification in the CSF of patients with CNS lymphoma. J Clin Oncol: Off J Am Soc Clin Oncol 26(1):96–105. doi:10.1200/JCO.2007.12.1053
Kersten MJ, Evers LM, Dellemijn PL, van den Berg H, Portegies P, Hintzen RQ, van Lier RA, von dem Borne AE, van Oers RH (1996) Elevation of cerebrospinal fluid soluble CD27 levels in patients with meningeal localization of lymphoid malignancies. Blood 87(5):1985–1989
Schroers R, Baraniskin A, Heute C, Kuhnhenn J, Alekseyev A, Schmiegel W, Schlegel U, Pels HJ (2010) Detection of free immunoglobulin light chains in cerebrospinal fluids of patients with central nervous system lymphomas. Eur J Haematol 85(3):236–242. doi:10.1111/j.1600-0609.2010.01475.x
Lagos-Quintana M, Rauhut R, Lendeckel W, Tuschl T (2001) Identification of novel genes coding for small expressed RNAs. Science 294(5543):853–858. doi:10.1126/science.1064921
Jovanovic M, Hengartner MO (2006) miRNAs and apoptosis: RNAs to die for. Oncogene 25(46):6176–6187. doi:10.1038/sj.onc.1209912
Volinia S, Calin GA, Liu CG, Ambs S, Cimmino A, Petrocca F, Visone R, Iorio M, Roldo C, Ferracin M, Prueitt RL, Yanaihara N, Lanza G, Scarpa A, Vecchione A, Negrini M, Harris CC, Croce CM (2006) A microRNA expression signature of human solid tumors defines cancer gene targets. Proc Natl Acad Sci U S A 103(7):2257–2261. doi:10.1073/pnas.0510565103
Hwang HW, Mendell JT (2007) MicroRNAs in cell proliferation, cell death, and tumorigenesis. Br J Cancer 96(Suppl):R40–R44
Mar-Aguilar F, Mendoza-Ramirez JA, Malagon-Santiago I, Espino-Silva PK, Santuario-Facio SK, Ruiz-Flores P, Rodriguez-Padilla C, Resendez-Perez D (2013) Serum circulating microRNA profiling for identification of potential breast cancer biomarkers. Dis Markers 34(3):163–169. doi:10.3233/dma-120957
Mar-Aguilar F, Luna-Aguirre CM, Moreno-Rocha JC, Araiza-Chavez J, Trevino V, Rodriguez-Padilla C, Resendez-Perez D (2013) Differential expression of miR-21, miR-125b and miR-191 in breast cancer tissue. Asia-Pacific J Clin Oncol 9(1):53–59. doi:10.1111/j.1743-7563.2012.01548.x
Vriens MR, Weng J, Suh I, Huynh N, Guerrero MA, Shen WT, Duh QY, Clark OH, Kebebew E (2012) MicroRNA expression profiling is a potential diagnostic tool for thyroid cancer. Cancer 118(13):3426–3432. doi:10.1002/cncr.26587
Ichimi T, Enokida H, Okuno Y, Kunimoto R, Chiyomaru T, Kawamoto K, Kawahara K, Toki K, Kawakami K, Nishiyama K, Tsujimoto G, Nakagawa M, Seki N (2009) Identification of novel microRNA targets based on microRNA signatures in bladder cancer. International journal of cancer Journal international du cancer 125(2):345–352. doi:10.1002/ijc.24390
Zhang Y, Jiang L (2014) CRP 1059 G/C and 1846G/A polymorphisms and cancer risk: A meta-analysis of 26,634 subjects. Clin Res Hepatol Gastroenterol. doi:10.1016/j.clinre.2014.04.002
Smirnova L, Grafe A, Seiler A, Schumacher S, Nitsch R, Wulczyn FG (2005) Regulation of miRNA expression during neural cell specification. Eur J Neurosci 21(6):1469–1477. doi:10.1111/j.1460-9568.2005.03978.x
Si H, Sun X, Chen Y, Cao Y, Chen S, Wang H, Hu C (2013) Circulating microRNA-92a and microRNA-21 as novel minimally invasive biomarkers for primary breast cancer. J Cancer Res Clin Oncol 139(2):223–229. doi:10.1007/s00432-012-1315-y
Ma Y, Tian Z, Zhang W (2012) Circulating miR-125b is a novel biomarker for screening non-small-cell lung cancer and predicts poor prognosis. J Cancer Res Clin Oncol 138(12):2045–2050. doi:10.1007/s00432-012-1285-0
(2002) International ethical guidelines for biomedical research involving human subjects. Bull Med Ethics 182:17–23
Baraniskin A, Kuhnhenn J, Schlegel U, Maghnouj A, Zollner H, Schmiegel W, Hahn S, Schroers R (2012) Identification of microRNAs in the cerebrospinal fluid as biomarker for the diagnosis of glioma. Neuro-Oncology 14(1):29–33. doi:10.1093/neuonc/nor169
Zamora J, Abraira V, Muriel A, Khan K, Coomarasamy A (2006) Meta-DiSc: a software for meta-analysis of test accuracy data. BMC Med Res Methodol 6:31. doi:10.1186/1471-2288-6-31
Mitchell AJ, Vaze A, Rao S (2009) Clinical diagnosis of depression in primary care: a meta-analysis. Lancet 374(9690):609–619. doi:10.1016/S0140-6736(09)60879-5
Deeks JJ (2001) Systematic reviews in health care: Systematic reviews of evaluations of diagnostic and screening tests. BMJ 323(7305):157–162
Monzo M, Navarro A, Bandres E, Artells R, Moreno I, Gel B, Ibeas R, Moreno J, Martinez F, Diaz T, Martinez A, Balague O, Garcia-Foncillas J (2008) Overlapping expression of microRNAs in human embryonic colon and colorectal cancer. Cell Res 18(8):823–833. doi:10.1038/cr.2008.81
Walter SD (2002) Properties of the summary receiver operating characteristic (SROC) curve for diagnostic test data. Stat Med 21(9):1237–1256. doi:10.1002/sim.1099
Chan JA, Krichevsky AM, Kosik KS (2005) MicroRNA-21 is an antiapoptotic factor in human glioblastoma cells. Cancer Res 65(14):6029–6033. doi:10.1158/0008-5472.CAN-05-0137
Conflict of Interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wei, X., Chen, D., Lv, T. et al. Serum MicroRNA-125b as a Potential Biomarker for Glioma Diagnosis. Mol Neurobiol 53, 163–170 (2016). https://doi.org/10.1007/s12035-014-8993-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-014-8993-1