Abstract
Secretory phospholipase A2 (sPLA2s) are small secreted proteins (14–18 kDa) and require submillimolar levels of Ca2+ for liberating arachidonic acid from cell membrane lipids. In addition to the enzymatic function, sPLA2 can exert various biological responses by binding to specific receptors. Physiologically, sPLA2s play important roles on the neurotransmission in the central nervous system and the neuritogenesis in the peripheral nervous system. Pathologically, sPLA2s are involved in the neurodegenerative diseases (e.g., Alzheimer’s disease) and cerebrovascular diseases (e.g., stoke). The common pathology (e.g., neuronal apoptosis) of Alzheimer’s disease and stroke coexists in the mixed dementia, suggesting common pathogenic mechanisms of the two neurological diseases. Among mammalian sPLA2s, sPLA2-IB and sPLA2-IIA induce neuronal apoptosis in rat cortical neurons. The excess influx of calcium into neurons via l-type voltage-dependent Ca2+ channels mediates the two sPLA2-induced apoptosis. The elevated concentration of intracellular calcium activates PKC, MAPK and cytosolic PLA2. Moreover, it is linked with the production of reactive oxygen species and apoptosis through activation of the superoxide producing enzyme NADPH oxidase. NADPH oxidase is involved in the neurotoxicity of amyloid β peptide, which impairs synaptic plasticity long before its deposition in the form of amyloid plaques of Alzheimer’s disease. In turn, reactive oxygen species from NADPH oxidase can stimulate ERK1/2 phosphorylation and activation of cPLA2 and result in a release of arachidonic acid. sPLA2 is up-regulated in both Alzheimer’s disease and cerebrovascular disease, suggesting the involvement of sPLA2 in the common pathogenic mechanisms of the two diseases. Thus, our review presents evidences for pathophysiological roles of sPLA2 in the central nervous system and neurological diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Phospholipase A2 (PLA2) belongs to a family of enzymes that catalyze the cleavage of fatty acids from the sn-2 position of glycerophospholipids to produce free fatty acids and lysophospholipids. PLA2s participate in a wide variety of physiological processes, including phospholipid digestion, remodeling of cell membranes and host defense. According to their biochemical features such as cellular localization, requirement of Ca2+, substrate specificity and the primary structure, more than 19 different isoforms of mammalian PLA2 are classified into several families, including low molecular weight secretory PLA2 (sPLA2), Ca2+-sensitive arachidonoyl-specific 85-kDa cytosolic PLA2 (cPLA2), Ca2+-independent PLA2 (iPLA2), plasmalogen-selective PLA2 and platelet-activating factor-acetylhydrolase [1]. The common structural and catalytic properties of mammalian sPLA2s are: the presence of 6–8 disulfide bonds, highly conserved catalytical dyad His–Asp and “Ca binding loop”, a requirement for millimolar concentration of Ca2+ for catalysi, and a broad specificity for phospholipids with different polar head groups and fatty acid chains. In addition to the digestive function, sPLA2 can exert various biological responses through the binding to the cell surface PLA2 receptor [2]. In the mammalian nervous system, nine sPLA2 (IB, IIA, IIC, IIE, IIF, III, V, X and XII), cPLA2 (IV), iPLA2 (VI) and platelet-activating factor (PAF)-acetylhydrolase (VII, VIII) have been detected.
Occurrence of sPLA2s in Mammalian Nervous Tissues and Neural Cells
The sPLA2s are small secreted proteins (14–18 kDa) and use an active site histidine and absolutely require submillimolar levels of Ca2+ for catalysis. In close proximity to the catalytic histidine, there is a conserved aspartate. The two amino acids form a His/Asp dyad. Mammalian PLA2s do not show a distinct preference for particular fatty acids, whereas there is some specificity for certain head groups of the phospholipid substrate: generally, sPLA2s show a high activity with anionic phospholipid but only the sPLA2-V and sPLA2-X PLA2s also hydrolyze phosphatidylcholine vesicles.
sPLA2-IB
The human sPLA2-IB consists of 148 amino acids (calculated molecular mass [M r] = 16,800). The gene of sPLA2-IB maps to chromosome 12q23-24. sPLA2s are Ca2+-dependent for catalytic activity (generally requiring millimolar Ca2+ concentrations) [3], consistent with their extracellular activity and millimolar Ca2+ concentrations in the extracellular space [4]. Evidence also points to an intracellular functional role sPLA2 in caveolae-containing compartments around the nucleus of immune cells and in the nucleus of astrocytes and neurons [5]. sPLA2-IB has a unique five amino acid extension termed the pancreatic loop in the middle part of the molecule and a group I-specific disulfide between Cys11 and Cys77. sPLA2-IB is produced as an inactive pro-enzyme (pro-sPLA2-IB) and is activated by proteolytic enzymes such as trypsin and plasmin. Given its abundance in digestive organs, the major physiological function of sPLA2-IB has been thought to be the digestion of glycerophospholipids in nutrients [6]. Although sPLA2-IB is originally purified and sequenced from pancreas or pancreatic juice of various mammals, it is also found in the brain [7]. Its mRNA is most abundant in the cerebral cortex, followed by the temporal lobe (Table 1). sPLA2-IB is expressed in the neuronal cell body of cortex, hippocampus and cerebellum. Although sPLA2-IB is not detected in the outer layer of cortex, it is abundant in layers 2–4. In the hippocampus, sPLA2-IB is present in all CA regions as well as in the dentate gyrus [7].
sPLA2-IIA
The human sPLA2-IIA consists of 144 amino acids (M r = 16,083) and is most similar to sPLA2-IB with respect to the number and positions of cysteine residues as well as overall identity (51 %) [8]. The gene of human sPLA2-IIA maps to chromosome 1p35. Its enzymatic properties are almost identical to those of sPLA2-IB in terms of Ca2+ requirement, optimal pH, substrate specificity, as well as high susceptibility to the sPLA2 inhibitor indoxam. sPLA2-IIA mRNA is detected in all brain region (Table 1). It is highly expressed in the brainstem and midbrain, and lowly in cerebellum and corpus striatum [9].
sPLA2-IIC
The gene of human sPLA2-IIC maps to chromosome 1p35.12. sPLA2-IIC mRNA is exclusively expressed in the brain. As shown in Table 1, it is highly expressed in hypothalamus, cerebral cortex, midbrain, striatum, and hippocampus and lowly expressed in brainstem, thalamus and cerebellum [9]. However, protein of sPLA2-IIC has not yet been detected and its function not also detected. The gene encoding for sPLA2-IIC appears to be a pseudogene.
sPLA2-IIE
The human sPLA2-IIE consists of 123 amino acids (M r = 14,000) and is most similar to sPLA2-IIA with respect to the number and positions of cysteine residues as well as overall identity (51 %) [8]. Its enzymatic properties are almost identical to those of sPLA2-IIA in terms of Ca2+ requirement, optimal pH, substrate specificity, as well as high susceptibility to the sPLA2 inhibitor indoxam. sPLA2-IIE retains considerable catalytic activity at pH 5, with activity falling as the pH is raised above 6, suggesting its function in weakly acidic cellular compartments. No catalytic activity is detected for mouse sPLA2-IIE in the absence of calcium [10]. The gene of human sPLA2-IIE maps to chromosome 1p36.13. PLA2-IIE mRNA is detected by RT-PCR in rat brain as well as in primary neuronal cultures [11]. In situ hybridization is carried out to identify the location of the sPLA2 in rat brain. The mRNA expression of sPLA2-IIE is found in cortex, hippocampus and cerebellum (Table 1).
sPLA2-IIF
The full-length cDNA codes for a signal peptide of 20 amino acids followed by a mature protein of 148 amino acids containing all of the structural features of catalytically active sPLA2-IIs [12]. The gene of human sPLA2-IIF maps to chromosome 1p35. Its unique feature is the presence of a C-terminal extension of 23 amino acids containing a single cysteine. Human sPLA2-IIF has been detected in patients with rheumatoid arthritis, but not in the brain. Mouse sPLA2-IIF is strongly expressed during embryogenesis and in adult testis. In the mouse brain, Northern blot analysis reveals a very low level of sPLA2-IIF [10]. sPLA2-IIF retains considerable catalytic activity at pH 5, with activity falling as the pH is raised above 6, suggesting its function in weakly acidic cellular compartments. No catalytic activity is detected for mouse sPLA2-IIF in the absence of calcium [10].
sPLA2-III
Human sPLA2-III homologous to the bee venom group III is identified by a systematic homology search in nucleic data bases [13]. The sPLA2 domain is 31 % identical to bee venom sPLA2 and displays all features of group III sPLA2s including ten cysteines. The gene of sPLA2-III maps to chromosome 22q. Its mRNA is highly expressed in kidney, heart, liver and skeletal muscle, but only weakly in the brain. sPLA2-III is expressed in neuronal cells, such as peripheral neuronal fibers, spinal dorsal root ganglia neurons and cerebellar Purkinje cells [14]. sPLA2-III protein is highly expressed in the brainstem, spinal cord and cerebral cortex. sPLA2-III protein is present in the “light membrane/cytosol” fraction, but not the nucleus, synaptosomal membrane or synaptic vesicle-enriched fractions. sPLA2-III is immunolocalized to neurons in the cerebral cortex, Purkinje neurons in the cerebellar cortex, periaqueductal gray, red nucleus, spinal trigeminal nucleus and dorsal horn of the spinal cord. Electron microscopy of the spinal cord and cerebral cortex showed that sPLA2-III is localized in dendrites or dendritic spines, that formed asymmetrical synapses with unlabeled, putatively glutamatergic, axon terminals.
sPLA2-V
Human sPLA2-V shows a high level of identity with sPLA2-IIA, and its gene is located in chromosome 1 close to the gene of sPLA2-IIA [15]. However, sPLA2-V lacks one of the seven disulfide bridges found in similar sPLA2 and, therefore, represents a class of enzymes distinct from sPLA2-IIA. Cloned human sPLA2-V has a signal peptide of 20 amino acids, and the matured protein (M r = 13,692) consists of 118 residues. sPLA2-V effectively hydrolyzes phosphatidylcholine vesicles and the outer plasma membrane of mammalian cells. The gene of sPLA2-V maps to chromosome 1p36–p34. Rat sPLA2-V mRNA is detected in all brain regions, and highly expressed in the hippocampus [9]. Its protein is also found in the neurons in cerebral cortex and dentate gyrus [11], and in the Bergman glial cells in cerebellum [16]. Immunofluorescence analysis of isolated rat brain nuclei reveals that the enzyme is mainly localized in the nucleoplasm [17].
sPLA2-X
Human sPLA2-X shows a high level of identity with, and its gene is located in chromosome 16p13.1–p12 [18]. sPLA2-X contains unique structures: (1) a long prepropeptide ending with an arginine doublet, (2) 16 cysteines located at positions that are characteristic of both sPLA2-I and II, (3) a C-terminal extension typical of sPLA2-IIs, and (4) the absence of elapid and pancreatic loops that are characteristic of sPLA2-Is. Cloned human sPLA2-X has a matured protein (calculated molecular mass of 13.6 kDa) consists of 123 residues. Contrary to the other sPLA2, human sPLA2-X is very acidic (pI = 5.3) and possesses disulfide bridges typical to sPLA2-IB and sPLA2-IIA. Substrate preferences of sPLA2-X are phosphatidylethanolamine and phosphatidylcholine liposomes rather than phosphatidylserine. sPLA2-X is detected in neurons in cerebral cortex and dentate gyrus (Table 1). The level of sPLA2-X is lower than those of other neuronal sPLA2s in the central nervous system [11]. On the other hand, sPLA2-X is expressed in the peripheral neuronal fibers and in the primary culture of dorsal root ganglia neurons.
sPLA2-XII
The human sPLA2-XII cDNA codes for a signal peptide of 22 amino acids followed by a mature protein of 167 amino acids that displays a poor sequence homology with other known sPLA2s apart from the active site region [19]. The gene of human sPLA2-XII maps to chromosome 4q25. The Northern blot analysis of tissue distribution of human sPLA2-XII reveals a major transcript in heart, skeletal muscle, and kidney and lower levels in other tissues including the brain.
Physiological Roles of Secretory Phospholipase A2 in the Central Nervous System
Neuritogenesis
The enrichment of cytoplasmic PLA2 in growth cones suggests its plausible involvement in the regulation of growth cone function [20]. Rat pheochromocytoma PC12 cells are often used for the detailed analysis of neuronal functions (Table 2). They are differentiated into adherent cells similar to sympathetic neurons in response to nerve growth factor. Nerve growth factor induces neurite outgrowth and extends processes of PC 12 cells similar to neurites. Adenoviral expression of human sPLA2-III in PC12 cells or dorsal root ganglia explants facilitates neurite-like outgrowth, whereas expression of a catalytically inactive sPLA2-III mutant or use of sPLA2-III-directed small interfering RNA (siRNA) reduces nerve growth factor-induced the extension of process [14]. Mammalian sPLA2-V and -X also exhibit this effect in PC12 cells [21], and the extension is correlated to its activity rather than to a receptor-mediated mechanism [21]. The neuritogenic activity of sPLA2 is mediated by generation of lysophosphatidylcholine and subsequent activation of G2A [22]. A G-protein-coupled receptor G2A mediates the signaling of lysophosphatidylcholine. Overproduction or suppression of G2A results in the enhancement or reduction of outgrowth induced by the treatement with sPLA2 and lysophosphatidylcholine treatment. However, to our knowledge, mammalian sPLA2 has not yet been reported to contribute to the neuritogenesis in the central nervous system. Rather than sPLA2, cPLA2-IV and iPLA2-VI have been reported to be involved in the neuritogenesis in the central nervous system [23].
Bee venom sPLA2-III also promotes the processes of PC 12 cells [21], but the enzyme induces neuronal apoptosis [24]. Snake venom sPLA2-I or II also promotes the processes of PC 12 cells [25], but the enzyme induces neuronal apoptosis [26]. Furthermore, mammalian sPLA2-IB [27] and sPLA2-IIA [28] induce neuronal apoptosis, but they do not promote the processes of PC 12 cells [21, 22]. Since neurons and PC12 cells are differentiated and proliferative cells, respectively, it is no wonder that results obtained from neurons are not in accordance with those from PC12 cells. Thus, the neuritogenic effect of sPLA2 should be confirmed in the central nervous system.
Neurotransmission
sPLA2-IIA is contained in rat brain synaptosomes and released from the synaptosomes in response to depolarization evoked by a high concentration of potassium in the presence of Ca2+ [29]. When neuronally differentiated PC12 cells were stimulated with carbamylcholine or potassium, sPLA2-IIA is released into the medium. sPLA2-IIA inhibitors suppress catecholamine secretion from the carbamylcholine-activated PC12 cells. Exogenous sPLA2-IIA alone elicits catecholamine secretion [29]. Furthermore, the localization of mature/cleaved form of sPLA2-III in postsynaptic structures suggests a physiological role of the enzyme in neurotransmission or synaptic plasticity [30].
The activities of cPLA2 and sPLA2 increase upon exposure of cortical neurons to glutamate [31]. These studies support a functional link between PLA2 activity and stimulation of glutamate receptors. Furthermore, sPLA2 shows a synergistic effect on the increase of transient Ca2+ in hippocampal neurons [32], and the release of arachidonic acid (AA) in primary cortical neurons [33] induces by non-toxic and toxic glutamate concentrations. In primary cortical neurons, the combination of exogenous sPLA2 and glutamate also potentiates the release of AA from phosphatidylcholine and phosphatidylethanolamine [34].
Long-Term Potentiation
Long-term potentiation (LTP) has been proposed as one of mechanisms for memory formation, and is associated with amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptors activation and release of AA [35]. Influx of calcium ions through N-methyl-d-aspartate (NMDA) receptors into the postsynaptic spine triggers biochemical processes associated with LTP, which is believed to underlie memory formation in the CNS including the hippocampus and amygdalae (Fig. 1). The increased calcium concentration in the spine activates key enzymes such as CaMK II [36] and MAPK [37]. AMPA receptors are activated by phosphorylation by CaMKII, resulting in an increase of Ca2+ entry into postsynaptic neurons.
Physiological roles of PLA2 on the synaptic plasticity. Calcium plays a well-defined role in the biochemical transduction of signals from the synapse to the nucleus. In response to synaptic activity and neurotransmitter release, extracellular calcium flows into the postsynaptic cell through synaptic and extrasynaptic ligand- and voltage-gated calcium channels. Major routes of entry with well-established effects on nuclear gene expression are the NMDA receptor (NMDAR). Calcium-permeable AMPA receptors (AMPAR) may play a role at developing synapses or after the induction of synaptic plasticity. Calcium signals can also be amplified by calcium-induced release of calcium from intracellular stores, triggered by activation of inositol triphosphate receptors (IP 3 R). Calcium at the mouth of the channel, in the cytoplasm, or within the nucleus can signal to activity-dependent transcription factors. Alterations in calcium influx into the postsynaptic cell during development or as a result of mutation modulate the induction of gene expression in response to neuronal activity. ER denotes endoplasmic reticulum
PLA2 is distributed in synaptic vesicles, and its activity is neutralized completely by an antibody raised against sPLA2-IIA [29]. sPLA2-IIA immunoreactive with anti-sPLA2-IIA antibody is released from synaptosomes in response to depolarization evoked by a high concentration of potassium in the presence of Ca2+. In rat brain membranes, bee venom sPLA2-III produces a significant increase in the binding of [3H]AMPA to the AMPA/quisqualate receptor. sPLA2 increases the affinity of the AMPA/quisqualate receptor without changing the maximum number of sites. In contrast, sPLA2 does not detectably modify the binding of [3H]kainate to the kainate receptor and of [3H]glutamate and [3H]glycine to the NMDA receptor complex [38]. The increased sensitivity of the AMPA/quisqualate receptors contributes to the expression of LTP in area CA1 of hippocampus. NMDA receptor activation increases AA release as a result of calcium influx through the NMDA receptor channel and thereby stimulation cPLA2 [39].
PLA2 inhibitors block LTP expression in the CA1 area of hippocampal slices [40] and AA [41] or its metabolites, PAF [42, 43], have been proposed as potential messenger signals released by postsynaptic cells to modify transmitter release in LTP. Exogenously applied AA facilitates LTP formation induced by high-frequency stimulation, and AA applied during low-frequency stimulation may result in slowly developing LTP [44]. In hippocampal slices, PAF induces a stable and concentration-dependent increase in LTP [43]. The PAF effect is blocked by the PAF receptor antagonists [42, 43]. Furthermore, observations that AA- [45] and PAF-induced LTP [43] are blocked by an NMDA receptor antagonist suggest that AA and PAF do not act as a retrograde messenger, but rather they likely serves to modify the functional properties of both NMDA and AMPA subtypes of glutamate receptor [46].
A potent and selective inhibitor of iPLA2, bromoenol lactone (BEL), completely suppresses the induction of LTP, suggesting a pivotal role of iPLA2 in the induction of LTP [35]. Although iPLA2 liberates linoleic acids from phosphatidylcholine, linoleic acid affected neither the induction nor maintenance of LTP [47]. PLA2 serves as a key enzyme to produce free fatty acids including docosahexaenoic acid (DHA). Although the content of DHA is slightly lower than AA in the central nervous system, DHA is also one of the major components of membrane phospholipids in the brain and is a good substrate of PLA2 partly because it is mainly localized in the 2-position of the phospholipids, particularly in phosphatidylethanolamine [48]. Therefore, as a result of the activation of PLA2, DHA may be predominantly released and accumulated in extracellular spaces. Thus, DHA may possibly contribute to the induction of LTP. Products of PLA2 may modulate glutamate release, postsynaptic receptor activation, and presynaptic responses [46]. In addition to lipid mediators (i.e., AA, eicosanoids and PAF), the released sPLA2 from the presynaptic neuron may directly participate in the induction and/or maintenance of LTP through a receptor-mediated mechanism or alternatively through its uptake by the presynaptic neuron [49].
Pathological Roles of Secretory Phospholipase A2 in Neurological Diseases
Alzheimer’s Disease
AD is a neurodegenerative disease characterized primarily by cognitive impairment and secondarily by motor dysfunction. AD is the most common cause of late life dementia [50]. Although most cases of AD are thought to be sporadic, the risk factors for AD include stroke [51]. As well as stroke [52], sPLA2 is expressed in the brain of AD patients [53]. All these conditions have a vascular involvement and reduce cerebral perfusion. AD is defined pathologically by extracellular neuritic plaques comprised of fibrillar deposits of a 4-kDa hydrophobic polypeptide known as amyloid β (Aβ) and neurofibrillary tangles (NFTs) consisting of paired helical filaments of hyperphosphorylated tau (Fig. 2). Other pathologic hallmarks of AD are activated microglia, reactive astrocytes and neuronal cell loss [51].
Steps involved in neurodegeneration of Alzheimer’s disease (AD) and cerebrovascular disease (CVD). Scheme showing the Aβ hypothesis in AD, which is based on the role of arachidonate cascade. AMPA/KAR Ν-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid/kainate receptor, APP amyloid precursor protein, cPLA 2 cytosolic phospholipase A2, fAβ fibrillar amyloid β protein, GSK glycogen synthase kinase, HP-Tau hyperphosphorylated tau, MAPK mitogen-activated protein kinase, Na + /GluT Na+-dependent glutamate transporter, NFTs neurofibrillary tangles, NMDAR N-methyl-d-aspartate receptor, Aβ amyloid β protein oligomers, PL phospholipids, ROS reactive oxygen species, sAβ soluble amyloid β protein, Glu glutamate, sPLA 2 secretory phospholipase A2, sPLA 2 R secretory phospholipase A2 receptor
The Ca2+ hypothesis suggests that intracellular calcium increase in response to Aβ oligomer formation may lead to neuronal cell dysfunction and death in AD [54]. As shown in Fig. 5, mechanisms that perturb normal neuronal Ca2+ homeostasis include aberrant Ca2+ influx through plasma membrane channels including l-VDCCs [55] and NMDA receptors [56]. Although soluble Aβ exhibits low toxicity, fibrillar Aβ (fAβ), an Aβ conformation similar to that found in the AD brain, greatly increase Aβ toxicity in neuronal cultures [57]. sPLA2-IIA mRNA is up-regulated in AD brains as compared to non-demented elderly brains [53]. A higher percentage of sPLA2-IIA-immunoreactive astrocytes present in AD hippocampus and inferior temporal gyrus. In inferior temporal gyrus, the majority of sPLA2-IIA-positive astrocytes are associated with Aβ-containing plaques. Studies with human astrocytes in culture demonstrated the ability of oligomeric Aβ1-42 and interleukin-1β (IL-1β) to induce sPLA2-IIA mRNA expression, indicating that this gene is among those induced by inflammatory cytokines (Fig. 2).
fAβ [55] and sPLA2-IIA [58] generate reactive oxygen species (ROS), which cause membrane lipid peroxidation and disturb the integrity of neuronal membranes (Fig. 2). These free radicals stimulate l-VDCC [59], and potentiate the influx of Ca2+ into neurons [55, 58]. Increased oxidative stress is an early event in AD that decreases with disease progression and formation of characteristic lesions [60]. Products of lipid peroxidation show a significant increase of intracellular Aβ production [61]. Aβ causes neuronal apoptosis via the activation of caspase [62]. sPLA2-IB exerts its apoptotic activity via the release of cytochrome c, which results in triggering the activation of caspase cascade and poly(ADP-ribose) polymerase cleavage [63].
Cerebrovascular Disease
CVD is caused by vascular lesions, cerebral infarctions, multiple lacunar infarctions and ischemic periventricular leukoencephalopathy. CVD can result from ischemic or hemorrhagic brain damage. The three most common mechanisms causing this disease are single, strategically placed infarcts; multiple cortical infarcts; and subcortical small-vessel disease [64]. Stroke, the potent risk factor for CVD, is caused by a critical alteration of blood flow to a region of the brain [65]. An acute obstruction of an artery results in ischemia, i.e., insufficient blood flow to the tissue [66]. The ischemic brain suffers from a mismatch between its cellular energy demands and the ability of the vascular system to supply substrate, most importantly, oxygen. Subsequently, neurologic malfunctions and neuronal cell death are caused by increased intracellular calcium, excessive extracellular glutamate, free radicals, and inflammation (Fig. 2). At the beginning of the stroke, there is a definite gradation of injury — a central area or core, with low blood flow already showing signs of massive cell death, and an outer area, the penumbra, that is still alive, but will malfunction after several days. A rat with the middle cerebral artery occlusion has been established as an animal model for stroke [67]. The occlusion causes irreversible necrosis and infarction in the core [68]. On the other hand, cell death is induced not only via necrosis, but also via apoptosis, and cells remain viable for several hours in the penumbra [69].
PLA2 inhibitors terminate the reversible proapoptotic state in the penumbra. Therefore, interventions designed to terminate the reversible proapoptotic state are expected to reduce the ischemic damage and lead to successful treatment of stroke. The cortical sPLA2 is induced in response to focal cerebral ischemia [27, 28, 52, 70]. sPLA2 activity is elevated in the cortex, in which the ischemic core and the penumbra coexist [28]. sPLA2-IB [71] and sPLA2-IIA [58] induces neuronal apoptosis via l-VDCC (Fig. 2). A few minutes after uncompensated brain ischemia, cell death pathways overcome survival-promoting pathways, leading to neuronal death through three interacting mechanisms: excitotoxicity attributable to excess glutamate, oxidative stress, and/or stimulation of apoptotic-like pathways [51].
Multiple Sclerosis and Experimental Autoimmune Encephalomyelitis
The pathology of multiple sclerosis involves both antigen specific mechanisms and the innate immune system, including elements of the acute inflammatory response [72]. Since axonal loss is likely to begin at disease onset, the inflammation that accompanies this degeneration may be a persistent contributing factor in multiple sclerosis, as it all disorders in which there is destruction of nervous tissue. Rodent experimental autoimmune encephalomyelitis models of multiple sclerosis suggest PLA2 enzymes are involved in the onset and genesis of this disease [73]. Systemic infusion of anchored lipid conjugates, targeting sPLA2s, attenuates aspects of the autoimmune response and experimental autoimmune encephalomyelitis clinical disease. Multiple Sclerosis patients also show elevations in sPLA2 enzyme activity [74]. Enzymatically active sPLA2 in the urine increases following immunization and peaked between days 8 and 10 PI, which is just prior to the onset of experimental autoimmune encephalomyelitis symptoms [74].
Spinal Cord Injury
Spinal cord injury starts with the primary injury phase, characterized by an initial damage core generally induced by the application of mechanical forces [75]. The secondary injury phase is characterized by the activation of a complex network of cellular processes, such as microglial and astroglial reactivity, leukocyte infiltration and mobilization of neural precursors. The activation of the secondary injury phase usually leads to the massive death of neural cells via apoptosis as well as necrosis and to the disruption of neural circuits that surround the primary injury core, and these cause most of the functional deficits associated with spinal cord injury [75]. The neurochemical changes include a rise in glutamate and intracellular calcium, degradation of membrane phospholipids with generation of free fatty acids, diacylglycerols, eicosanoids, and lipid peroxides, and activation of phospholipases and lipases [2]. After the initial mechanical insult of spinal cord injury, secondary mediators propagate a massive loss of oligodendrocytes. Following spinal cord injury, both the total phospholipase activity and cytosolic cPLA2 α protein expression are increased. Cervical spinal cord injury markedly up-regulated mRNA of sPLA2-IIA and IIE. In contrast, spinal cord injury induces down regulation of sPLA2-X, and no change in sPLA2-IB, IIC, V, and XIIA expression. At the lesion site, sPLA2-IIA and IIE expression are localized to oligodendrocytes. sPLA2-IIA exhibit cytotoxicity in differentiated adult oligodendrocyte precursor cells but not primary astrocytes or Schwann cells [76].
Epilepsy
In the pentylenetetrazol-induced model of epilepsy, sPLA2 activity is significantly elevated in cortical, hippocampal, and cerebellar regions compared with the control group in rat brain. The increase in sPLA2 activity is more pronounced in hippocampal and cortical regions than in the cerebellar region [77]. PLA2 activity is increased in the brain, as frequently reported in schizophrenia, is also related to psychosis in epilepsy. The prevalence of schizophrenia-like psychosis in patients with temporal lobe epilepsy secondary to mesial temporal sclerosis is higher than that in patients with other forms of epilepsy. Temporal lobe epilepsy secondary to mesial temporal sclerosis in patients with psychosis shows a significantly higher brain iPLA2 activity as compared to patients without psychosis. No significant differences were found between both groups regarding sPLA2 and cPLA2 activities. Epileptic seizures are known to stimulate cPLA2 activity and its expression with the accumulation of AA [78]. More studies are needed on the involvement of PLA2 isoforms in the pathogenesis of epilepsy.
Pathological Functions of Phospholipase A2
Secretory Phospholipase A2 Receptor
Certain types of snake venom sPLA2 have specific binding proteins similar to the mannose receptor in mammals [79]. Two main types of high affinity receptors for Taipan snake venom sPLA2s are identified as N-type and M-type (Fig. 3). N-type sPLA2 receptors are first identified in rat brain membranes [80]. These receptors have high affinities for neurotoxic sPLA2s such as OS2 and the bee venom sPLA2 (sPLA2-III) but not for nontoxic sPLA2s such as OS1, suggesting that N-type receptors contribute to the neurotoxic effects of venom sPLA2s. M-type sPLA2 receptors are first identified in rabbit skeletal muscle cells. In porcine cerebral cortex, a receptor for long-nosed viper venom ammodytoxin C (AtxC) is identified [81]. In its molecular mass and pharmacological profile, the AtxC receptor resembles the M-type receptor for sPLA2 from rabbit skeletal muscle (a C-type multilectin, homologous to macrophage mannose receptor), yet in terms of relative abundance in brain and antigenicity, these two receptors are completely different. The AtxC receptor consists of a single 180-kDa subunit and recognizes with high affinity OS2 but not the neurotoxic sPLA2-III. On the other hand, 125I-labeled ppPLA2-IB has revealed two classes of high-affinity binding sites in the rat brain [82]. Their binding profile is different from that of binding sites of OS2, suggesting the existence of a novel class of sPLA2 N-type binding sites.
Secretory phospholipase A2 receptors. Mammalian sPLA2s generate ROS, open l-VDCCs, but not glutamate receptors and incorporates Ca2+ into neurons. Snake venom sPLA2s also generates ROS, opens l-VDCCs, activate NMDA receptors and uptake Ca2+ into neurons. The elevated level of intracellular calcium concentration activates Ca2+-dependent enzymes such as cPLA2, nucleases, kinases and proteases, and induced neuronal apoptosis
Mammalian sPLA2 can only bind to the M-type receptor, which is not restricted to muscles but also expressed in various tissues [83]. Mammalian sPLA2-IB are not only digestive enzymes, but also involved in a number of other important physiological processes such as cell contraction [84], lipid mediator release [85] and cell proliferation [86] via its specific receptors. The receptor of porcine pancreatic sPLA2-IB (sPLA2R) is composed of a single glycosylated polypeptide chain with an apparent molecular mass of 190 kDa [87]. The sPLA2R for porcine pancreatic sPLA2-IB is structurally related to the macrophage mannose receptor, a unique member of Ca2+-dependent (C-type) animal lectin family [88]. The sPLA2-IB receptor carries a region consisting of eight tandem carbohydrate-recognition-domain-(CRD)-like domains as in the case of the mannose receptor; this region is responsible for sPLA2-IB binding, not sugar binding, in the sPLA2-IB receptor. Although the sPLA2R has not yet been detected in the CNS, sPLA2-IB is distributed in rat brain and human brain [7].
Secretory PLA2-Induced Neuronal Cell Death
Porcine pancreatic sPLA2-IB induces neuronal cell death in primary cultures of rat cortical neurons [70]. sPLA2-IB shrinks neuronal cell bodies and shortens neurites. In the early stage of cell death, it becomes difficult to resolve the plasma membrane, whereas features in the cytosol and the nucleus are unaltered. In the middle stage, microtubules, neurofilaments, and ribosomes are condensed as the neurons continued to shrink. Moreover, a decrease of the rough endoplasmic reticulum (ER) and progressive swelling of the Golgi cisternae are observed within the cytoplasm. The nuclei shrink progressively, and chromatin clumps become increasingly electron-dense. In the late stage, intracellular organelles such as the ER and the Golgi apparatus are lost, but the mitochondria remained intact. Condensation and fragmentation of chromatin are noted in the nucleus. The dying cells finally are fragmented into small pieces. The sPLA2-IB-induced neuronal cell death exhibits apoptotic features with blebbed membrane, condensed chromatin, and fragmented DNA. The ultrastructural disruption in sPLA2-IB-treated neurons is suppressed completely by a sPLA2 inhibitor, indoxam [70].
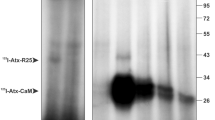
Porcine pancreatic sPLA2-IB induces neuronal apoptosis via its high-affinity binding sites in the rat brain [27]. The specific binding sites of [125I]sPLA2-IB are recognized by an anti-sPLA2R antibody. The anti-sPLA2R IgG also causes neuronal cell death as well as sPLA2-IB. By Scatchard analysis, number of maximal binding sites (B max) and dissociation constant (K d) values of [125I]sPLA2-IB is 3.1 fmol/106 cells and 0.84 nM, respectively [27]. Although 40 % of [125I]sPLA2-IB bound to neurons is displaced by 100 nM sPLA2-IB, bee venom sPLA2-III, a potent inhibitor of N-type binding sites of OS2 [80], significantly increases the binding of [125I]sPLA2-IB to neurons. The specific binding sites of [125I]sPLA2-IB are distinguishable from the N-type binding sites. sPLA2-IB appears to cause neuronal cell death via the specific binding sites, which are different from the sPLA2R and the N-type binding sites of OS2.
Human recombinant and rat spleen sPLA2-IIA causes disruption of neurites and cell bodies rather than their shrink in a different fashion to sPLA2-IB. However, as evidenced by condensed chromatin and fragmented DNA [28], ultrastructural characteristics of neuronal cell death by sPLA2-IIA are apoptotic. The M-type receptor binds toxic and non-toxic sPLA2 of either group I or II [81], giving rise to a possibility that sPLA2-IB and sPLA2-IIA might induce neuronal apoptosis via the AtxC receptor. The above two sPLA2s-induced neuronal apoptosis is suppressed by a reversible sPLA2 inhibitor, indoxam, as well as a putative irreversible sPLA2 inhibitor [28, 70]. Under the optimal conditions of each sPLA2 reaction with 1-palmitoyl-2-oleoyl-sn-glycero-3- phosphocholine as a substrate, IC50 values of indoxam against sPLA2-IIA, -IID, and -IIE are 1–2 nM [89]. On the other hand, the other isoforms (sPLA2-IB, -V, and -X) are less sensitive to indoxam with over 100-fold higher IC50 values. Indoxam does not only inhibit the enzymatic activity of sPLA2s, but also blocks the binding to its murine receptor (K i = 30 nM) [89], suggesting that sPLA2s might cause apoptosis via its high affinity binding sites and its enzymatic activity.
sPLA2-Induced Neuronal Apoptosis via l-type Voltage-Dependent Ca2+ Channels
Calcium is an intracellular second messenger in many cell types, and regulates many complicated cellular processes, including cell activation, proliferation and apoptosis. In resting cells, the intracellular Ca2+ concentration ([Ca2+]i) is maintained at a low level (50–150 nM) compared with the levels present in the extracellular space (2 mM). However, agonists including hormones, growth factors and neurotransmitters induce changes in the intracellular Ca2+ dynamics, including elevation of [Ca2+]i via mobilization of Ca2+ from intracellular stores such as the ER and mitochondria as well as the extracellular fluid. The calcium chelator attenuates the neurotoxicity of mammalian and non-mammalian sPLA2s, suggesting that calcium mobilization might contribute to the apoptosis. Actually, these sPLA2s elevate the influx of Ca2+ persistently before apoptosis [58, 71].
Neuronal cell death is induced synergistically by non mammalian sPLA2s (bee venom sPLA2 and Taipan snake venom sPLA2-OS2) glutamate in rat cortical neurons [33]. Glutamate receptors have been classified as ionotropic and metabotropic. Ionotropic glutamate (AMPA, kainate and NMDA) receptors are ligand-gated cation channels, whereas metabotropic glutamate receptors are coupled to various signal transduction systems. NMDARs are unique in that their activation is governed by a strong voltage-dependence due to receptor channel blockade by Mg2+ at hyperpolarized membrane potentials. Mg2+ blockade gives NMDA receptors their characteristic negative slope conductance.
Snake venom sPLA2s are neurotoxic in vivo and in vitro, causing synergistic neurotoxicity to cortical cultures when applied with toxic concentrations of glutamate [33]. Antagonists for NMDA receptor and AMPA receptor prevent neurons from the Tipan snake venom sPLA2-OS2-induced neuronal cell death [90]. Snake venom sPLA2-IA also induces neuronal cell death via apoptosis. sPLA2-IA disrupts cell bodies and fragmented neurites, accompanied with chromatin condensation and DNA fragmentation [26]. NMDA receptor blockers such as PCP and DCKA, but not AMPA receptor blocker, prevent neurons from undergoing the sPLA2-IA-induced neuronal cell death (Fig. 4). However, neither NMDA receptor nor AMPA/kinate receptor are involved in the neurotoxicity of mammalian sPLA2-IB (porcine pancreas) and sPLA2-IIA (human recombinant) [58, 71] (Fig. 4). Moreover, neither N-type nor P/Q-type VDCCs affects the mammalian and non-mammalian sPLA2s-induced neuronal cell death (Fig. 5A). An l-type voltage-dependent Ca2+ channels (l-VDCC) blocker, nimodipine, completely prevent neurons from undergoing the mammalian sPLA2IB- and sPLA2IIA-induced cell deaths, whereas it does partially neurons from undergoing the non-mammalian cobra venom sPLA2IA (Naja naja)-induced cell death (Fig. 5B). The elevation of Ca2+ uptake by these sPLA2s is significantly reduced by l-VDCC blockers [26, 58, 71]. Neither an N-type VDCC blocker nor P/Q-type VDCC blockers affects sPLA2-increased Ca2+ influx. l-VDCC blockers ameliorate mammalian and non-mammalian sPLA2s-induced morphological changes as well as biochemical apoptotic features [26, 58, 71]. Thus, mammalian sPLA2s induce neuronal apoptosis via the influx of Ca2+ into neurons through l-VDCC, whereas non-mammalian sPLA2 does through the glutamate receptor and the l-VDCC (Fig. 3).
NMDA receptor blockers rescued neuron from undergoing the sPLA2s-induced neuronal cell death. Glutamate receptor blockers: cortical neurons were treated with 20 pM sPLA2-IA (open columns), 50 nM sPLA2-IB (dotted columns) or 1 μM sPLA2-IIA (hatched columns) in the absence or presence of 30 μM PCP, DCKA, AP-7, CPP or NBQX. MTT reducing activity was determined 24 h (sPLA2-IA and sPLA2-IB) or 48 h (sPLA2-IIA) later. Data are expressed as means ± SEM (n = 4). **P < 0.01, compared with control; # P < 0.05, ## P < 0.01, compared with sPLA2-IA or sPLA2-IB alone by ANOVA followed by Dunnett’s test
l-VDCC blockers rescued neuron from undergoing the sPLA2s-induced neuronal cell death. a VDCC blockers: Cortical neurons were treated with 20 pM sPLA2-IA (open columns), 50 nM sPLA2-IB (dotted columns) or 1 μM sPLA2-IIA (hatched columns) in the absence or presence of 10 μM Nimodipine, 1 μM ω-Aga GVIA, ω-CgTX GVIA or ω-CgTX-MVIIC. b Concentration: cortical neurons were treated with S-312d or nimodipine at the indicated concentrations in the presence of 20 pM sPLA2-IA (circles), 50 nM sPLA2-IB (triangles) or 1 μM sPLA2-IIA (squares). MTT reducing activity was determined 24 h (sPLA2-IA and sPLA2-IB) or 48 h (sPLA2-IIA) later. Data are expressed as means ± SEM (n = 4). **P < 0.01, compared with control; # P < 0.05, ## P < 0.01, compared with sPLA2-IA or sPLA2-IB or sPLA2-IIA alone by ANOVA followed by Dunnett’s test
The l-VDCC is activated by ROS [55], which is generated by sPLA2-IIA before neuronal cell death [58]. ROS are reduced significantly by radical scavengers, including vitamin E, probucol, butylated hydroxytoluene and chlorpromazine. On the other hand, nimodipine does not affect the production of ROS after sPLA2-IIA treatment. Vitamin E also suppresses Ca2+ influx as well as the l-VSCC blocker. In addition, the above radical scavengers significantly prevent neurons from undergoing sPLA2-IIA-induced neuronal cell death [58]. As the common pathway, the excess influx of calcium via l-VDCC contributes the neurotoxicity of mammalian and non-mammalian sPLA2s (Fig. 3).
Pathological Calcium Signaling
VDCCs play pathophysiological roles in coordination with the LGCCs and the intracellular stores (Fig. 2). The elevation of [Ca2+]i activation Ca2+-dependent enzymes such as protein kinases, proteinases, DNases, and PLA2s. Calcium mediated activation of calpain is also reported to cause cell death in various neuropathological conditions including CVD and AD [91]. The requirement for calcium and protein kinases (MAPK and PKC) for cPLA2 suggests that cPLA2 is under tight control by intracellular signaling pathways. The elevation of [Ca2+]i through l-VDCC and NMDA receptor activates PKC, MAPK ad cPLA2 (Fig. 2). Moreover, it is linked with the production of ROS and apoptosis through activation of the superoxide producing enzyme NADPH oxidase (NOX). There are at least seven known isoforms, NOX1-5, Duox1 and 2, each with a unique combination of subunits [92]. NOX2 is well studied in phagocytic cells, macrophages, and endothelial cells and is comprised of the subunits p47phox, p67phox, p40phox, and Rac 1 in the cytosol and gp91phox and p22phox in the membrane fraction (plasma membranes or other subcellular membranes). Activation of NOX2 is dependent on phosphorylation of the cytosolic subunits, e.g., phosphorylation of p47phox by protein kinase C in human monocytes [93]. Subsequently, the cytosolic subunits form a complex and translocated to the membrane-associated gp91phox subunit. NOX1, 2, and 4 are expressed in neurons, astrocytes, and microglia in the CNS [92]. NOX is involved in excitotoxicity induced by ionotropic glutamate receptors, including the NMDA subtype [94]. NMDA-induced activation of NOX can trigger signaling pathways leading to activation of ERK1/2, the protein kinase required for activation of cPLA2 (Fig. 2). Oligomeric Aβ can induce ROS production through NOX. In turn, ROS from NOX can stimulate ERK1/2 phosphorylation and activation of cPLA2 and result in a release of AA [95]. The excitotoxic effect of Aβ is inhibited by NMDA receptor antagonists, including memantine, a drug used to treat AD patients [96].
Conclusions
sPLA2s cause neuritogenesis in peripheral neurons, whereas cPLA2s and iPLA2s — rather than sPLA2 — are involved in the neuritogenesis in central neurons. sPLA2s are localized at synapse and secret catecholamine from neuronally differentiated PC12 cells, suggesting that the enzymes may release neurotransmitters from neurons. iPLA2s play a pivotal role in the induction of LTP. Although linoleic acid is preferentially produced by iPLA2, it does not induce and maintain LTP. Since PAF induces LTP and PLA2 inhibitors block the induction of LTP, sPLA2 released from the presynaptic neuron appears to directly participate in the induction and maintenance of LTP.
The abnormal genetic and environmental processes interfere with normal brain maturation and result in dysfunctional monoaminergic neurotransmission associated with the phenotype of schizophrenia. Genetic variation in sPLA2-IIA, cPLA2-IVA and iPLA2-VIA is possibly involved in both brain maturational processes and neurotransmission [97]. The elevation of PLA2 activity is correlated with structural changes in schizophrenic brains [98]. The increased activity of iPLA2 in the brain of schizophrenic patients has been suggested to accelerate the breakdown of membrane phospholipids and alter the properties of neuronal membranes, which in turn contribute to a hypodopaminergy [99]. A genetic variant of cPLA2 gene has been reported to increase risk for schizophrenia through an increment of PLA2 activity [100]. Since the elevation of PLA2 activity is correlated with structural changes in schizophrenic brains [98], its activity and protein may be altered in the disease.
The importance of PLA2 in the pathogenesis of the neuronal degeneration in prion diseases has been indicated by the use of PLA2 inhibitors that reduced the misfolding of the normal prion protein, caspase-3 activity and prostaglandin E2 production [101]. Since cPLA2 plays a vital role in the progress of prion diseases [102], sPLA2 might be also associated to the prion diseases. iPLA2 is the causative gene for early-onset PARK14-linked dystonia–parkinsonism [103]. Mice deficient in cPLA2 activity are resistant to 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine neurotoxicity, suggesting that cPLA2 is closely associated with the pathophysiology of Parkinson’s diseases [104]. A PLA2 inhibitor, quinacrine, protects do dopaminergic neurons from neurodegeneration in the 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine-induced model of parkinsonism [105], suggesting the plausible involvement of sPLA2 in Parkinson’s diseases.
sPLA2s are up-regulated in the cerebrovascular disease, stroke, and the neurodegenerative diseases, AD, in which the neuronal apoptosis is the common pathology. sPLA2s induce neuronal apoptosis via l-VDCC, but not via NMDAR, whereas non-mammalian sPLA2s induce neuronal apoptosis via l-VDCC and NMDAR [26]. Although mammalian sPLA2s bind M type-like receptor in the brain, it has not yet been clarified how M type-like receptor contributes to the apoptosis. To this end, the neurotoxicity of sPLA2s is needed to be analyzed in the M type-like receptor knock-out mouse. Among arachidonate metabolites, 15-deoxy-Δ12,14-PGJ2 can be contributed to the neurotoxicity of sPLA2s. Prior to neuronal apoptosis, sPLA2s enhance the influx of Ca2+ and produce PGD2. Although PGD2 receptors have not yet been detected on the neuronal surface, PGD2 can be non-enzymatically metabolized to 15-deoxy-Δ12,14-PGJ2. 15-deoxy-Δ12,14-PGJ2 possesses dual functions as a neuroprotectant and a neurotoxicant. 15-deoxy-Δ12,14-PGJ2 has been reported to exhibit the neuroprotective effect via its nuclear receptor, peroxysome proliferators-activated receptor γ [106] and the neurotoxic effect via its specific binding sites in the plasma membrane of neurons [107]. One of problems to be resolved is whether the receptor binding and/or the enzymatic activity are required to the neurotoxicity of sPLA2s.
Abbreviations
- AA:
-
Arachidonic acid
- AD:
-
Alzheimer’s disease
- AMPA:
-
Amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid
- APP:
-
Amyloid precursor protein
- CaMK II:
-
Calcium/calmodulin-dependent protein kinase II
- COX:
-
Cyclooxygenase
- CVD:
-
Cerebrovascular disease
- iPLA2 :
-
Ca2+-independent cytosolic phospholipase A2
- ER:
-
Endoplasmic reticulum
- FAβ:
-
Fibrillar Aβ
- [Ca2+]i :
-
Intracellular Ca2+ concentration
- IL-1β:
-
Interleukin-1β
- LGCC:
-
Ligand-gated calcium channel
- LTP:
-
Long-term potentiation
- l-VDCC:
-
l-Type voltage-dependent Ca2+ channels
- MAPK:
-
Mitogen-activated protein kinases
- NMDA:
-
N-Methyl-d-aspartate
- NFTs:
-
Neurofibrillary tangles
- PAF:
-
Platelet activating factor
- PLA2 :
-
Phospholipase A2
- PG:
-
Prostaglandin
- ROS:
-
Reactive oxygen species
- sPLA2 :
-
Secreted phospholipase A2
- sPLA2R:
-
Secretory phospholipase A2 receptor
References
Goracci G, Ferrini M, Nardicchi V (2010) Low molecular weight phospholipases A2 in mammalian brain and neural cells: roles in functions and dysfunctions. Mol Neurobiol 41(2–3):274–289
Farooqui AA, Ong WY, Horrocks LA (2006) Inhibitors of brain phospholipase A2 activity: their neuropharmacological effects and therapeutic importance for the treatment of neurologic disorders. Pharmacol Rev 58(3):591–620
Laychock SG (1982) Phospholipase A2 activity in pancreatic islets is calcium-dependent and stimulated by glucose. Cell Calcium 3(1):43–54
Clapham DE (1995) Calcium signaling. Cell 80(2):259–268
Rosa AO, Rapoport SI (2009) Intracellular- and extracellular-derived Ca(2+) influence phospholipase A(2)-mediated fatty acid release from brain phospholipids. Biochim Biophys Acta 1791(8):697–705
Grataroli R, De Caro A, Guy O, Amic J, Figarella C (1981) Isolation and properties of prophospholipase A2 from human pancreatic juice. Biochimie 63(8–9):677–684
Kolko M, Christoffersen NR, Varoqui H, Bazan NG (2005) Expression and induction of secretory phospholipase A2 group IB in brain. Cell Mol Neurobiol 25(7):1107–1122
Suzuki N, Ishizaki J, Yokota Y, Higashino K, Ono T, Ikeda M, Fujii N, Kawamoto K, Hanasaki K (2000) Structures, enzymatic properties, and expression of novel human and mouse secretory phospholipase A(2)s. J Biol Chem 275(8):5785–5793
Molloy GY, Rattray M, Williams RJ (1998) Genes encoding multiple forms of phospholipase A2 are expressed in rat brain. Neurosci Lett 258(3):139–142
Valentin E, Koduri RS, Scimeca JC, Carle G, Gelb MH, Lazdunski M, Lambeau G (1999) Cloning and recombinant expression of a novel mouse-secreted phospholipase A2. J Biol Chem 274(27):19152–19160
Kolko M, Christoffersen NR, Barreiro SG, Miller ML, Pizza AJ, Bazan NG (2006) Characterization and location of secretory phospholipase A2 groups IIE, V, and X in the rat brain. J Neurosci Res 83(5):874–882
Valentin E, Singer AG, Ghomashchi F, Lazdunski M, Gelb MH, Lambeau G (2000) Cloning and recombinant expression of human group IIF-secreted phospholipase A(2). Biochem Biophys Res Commun 279(1):223–228
Valentin E, Ghomashchi F, Gelb MH, Lazdunski M, Lambeau G (2000) Novel human secreted phospholipase A(2) with homology to the group III bee venom enzyme. J Biol Chem 275(11):7492–7496
Masuda S, Yamamoto K, Hirabayashi T, Ishikawa Y, Ishii T, Kudo I, Murakami M (2008) Human group III secreted phospholipase A2 promotes neuronal outgrowth and survival. Biochem J 409(2):429–438
Chen J, Engle SJ, Seilhamer JJ, Tischfield JA (1994) Cloning and recombinant expression of a novel human low molecular weight Ca(2+)-dependent phospholipase A2. J Biol Chem 269(4):2365–2368
Shirai Y, Ito M (2004) Specific differential expression of phospholipase A2 subtypes in rat cerebellum. J Neurocytol 33(3):297–307
Nardicchi V, Macchioni L, Ferrini M, Goracci G (2007) The presence of a secretory phospholipase A2 in the nuclei of neuronal and glial cells of rat brain cortex. Biochim Biophys Acta 1771(11):1345–1352
Cupillard L, Koumanov K, Mattei MG, Lazdunski M, Lambeau G (1997) Cloning, chromosomal mapping, and expression of a novel human secretory phospholipase A2. J Biol Chem 272(25):15745–15752
Gelb MH, Valentin E, Ghomashchi F, Lazdunski M, Lambeau G (2000) Cloning and recombinant expression of a structurally novel human secreted phospholipase A2. J Biol Chem 275(51):39823–39826
Negre-Aminou P, Nemenoff RA, Wood MR, de la Houssaye BA, Pfenninger KH (1996) Characterization of phospholipase A2 activity enriched in the nerve growth cone. J Neurochem 67(6):2599–2608
Nakashima S, Kitamoto K, Arioka M (2004) The catalytic activity, but not receptor binding, of sPLA2s plays a critical role for neurite outgrowth induction in PC12 cells. Brain Res 1015(1–2):207–211
Ikeno Y, Konno N, Cheon SH, Bolchi A, Ottonello S, Kitamoto K, Arioka M (2005) Secretory phospholipases A2 induce neurite outgrowth in PC12 cells through lysophosphatidylcholine generation and activation of G2A receptor. J Biol Chem 280(30):28044–28052
Forlenza OV, Mendes CT, Marie SK, Gattaz WF (2007) Inhibition of phospholipase A2 reduces neurite outgrowth and neuronal viability. Prostaglandins Leukot Essent Fatty Acids 76(1):47–55
DeCoster MA (2003) Group III secreted phospholipase A2 causes apoptosis in rat primary cortical neuronal cultures. Brain Res 988(1–2):20–28
Makarova YV, Osipov AV, Tsetlin VI, Utkin YN (2006) Influence of phospholipases A2 from snake venoms on survival and neurite outgrowth in pheochromocytoma cell line PC12. Biochemistry (Mosc) 71(6):678–684
Yagami T, Yamamoto Y, Koma H, Nakamura T, Takasu N, Okamura N (2013) L-type voltage-dependent calcium channel is involved in the snake venom group IA secretory phospholipase A2-induced neuronal apoptosis. Neurotoxicology 35:146–153
Yagami T, Ueda K, Asakura K, Hata S, Kuroda T, Sakaeda T, Kishino J, Sakaguchi G, Itoh N, Hori Y (2002) Group IB secretory phospholipase A(2)induces cell death in the cultured cortical neurons: a possible involvement of its binding sites. Brain Res 949(1–2):197–201
Yagami T, Ueda K, Asakura K, Hata S, Kuroda T, Sakaeda T, Takasu N, Tanaka K, Gemba T, Hori Y (2002) Human group IIA secretory phospholipase A2 induces neuronal cell death via apoptosis. Mol Pharmacol 61(1):114–126
Matsuzawa A, Murakami M, Atsumi G, Imai K, Prados P, Inoue K, Kudo I (1996) Release of secretory phospholipase A2 from rat neuronal cells and its possible function in the regulation of catecholamine secretion. Biochem J 318(Pt 2):701–709
Yang H, Siddiqi NJ, Alhomida AS, Ong WY (2013) Expression and localization of sPLA2-III in the rat CNS. Neurochem Res 38(4):753–760
Kim DK, Rordorf G, Nemenoff RA, Koroshetz WJ, Bonventre JV (1995) Glutamate stably enhances the activity of two cytosolic forms of phospholipase A2 in brain cortical cultures. Biochem J 310(Pt 1):83–90
DeCoster MA, Lambeau G, Lazdunski M, Bazan NG (2002) Secreted phospholipase A2 potentiates glutamate-induced calcium increase and cell death in primary neuronal cultures. J Neurosci Res 67(5):634–645
Kolko M, DeCoster MA, de Turco EB, Bazan NG (1996) Synergy by secretory phospholipase A2 and glutamate on inducing cell death and sustained arachidonic acid metabolic changes in primary cortical neuronal cultures. J Biol Chem 271(51):32722–32728
Rodriguez De Turco EB, Jackson FR, DeCoster MA, Kolko M, Bazan NG (2002) Glutamate signalling and secretory phospholipase A2 modulate the release of arachidonic acid from neuronal membranes. J Neurosci Res 68(5):558–567
Wolf MJ, Izumi Y, Zorumski CF, Gross RW (1995) Long-term potentiation requires activation of calcium-independent phospholipase A2. FEBS Lett 377(3):358–362
Malinow R, Schulman H, Tsien RW (1989) Inhibition of postsynaptic PKC or CaMKII blocks induction but not expression of LTP. Science 245(4920):862–866
English JD, Sweatt JD (1997) A requirement for the mitogen-activated protein kinase cascade in hippocampal long term potentiation. J Biol Chem 272(31):19103–19106
Massicotte G, Baudry M (1990) Modulation of dl-alpha-Amino-3-hydroxy-5-methylisoxazole-4-propionate (AMPA)/quisqualate receptors by phospholipase A2 treatment. Neurosci Lett 118(2):245–248
Dumuis A, Sebben M, Haynes L, Pin JP, Bockaert J (1988) NMDA receptors activate the arachidonic acid cascade system in striatal neurons. Nature 336(6194):68–70
Okada D, Yamagishi S, Sugiyama H (1989) Differential effects of phospholipase inhibitors in long-term potentiation in the rat hippocampal mossy fiber synapses and Schaffer/commissural synapses. Neurosci Lett 100(1–3):141–146
Drapeau C, Pellerin L, Wolfe LS, Avoli M (1990) Long-term changes of synaptic transmission induced by arachidonic acid in the CA1 subfield of the rat hippocampus. Neurosci Lett 115(2–3):286–292
Arai A, Lynch G (1992) Antagonists of the platelet-activating factor receptor block long-term potentiation in hippocampal slices. Eur J Neurosci 4(5):411–419
Wieraszko A, Li G, Kornecki E, Hogan MV, Ehrlich YH (1993) Long-term potentiation in the hippocampus induced by platelet-activating factor. Neuron 10(3):553–557
Williams JH, Errington ML, Lynch MA, Bliss TV (1989) Arachidonic acid induces a long-term activity-dependent enhancement of synaptic transmission in the hippocampus. Nature 341(6244):739–742
O’Dell TJ, Hawkins RD, Kandel ER, Arancio O (1991) Tests of the roles of two diffusible substances in long-term potentiation: evidence for nitric oxide as a possible early retrograde messenger. Proc Natl Acad Sci U S A 88(24):11285–11289
Miller B, Sarantis M, Traynelis SF, Attwell D (1992) Potentiation of NMDA receptor currents by arachidonic acid. Nature 355(6362):722–725
Fujita S, Ikegaya Y, Nishikawa M, Nishiyama N, Matsuki N (2001) Docosahexaenoic acid improves long-term potentiation attenuated by phospholipase A(2) inhibitor in rat hippocampal slices. Br J Pharmacol 132(7):1417–1422
Hadjiagapiou C, Spector AA (1987) Docosahexaenoic acid metabolism and effect on prostacyclin production in endothelial cells. Arch Biochem Biophys 253(1):1–12
Praznikar ZJ, Kovacic L, Rowan EG, Romih R, Rusmini P, Poletti A, Krizaj I, Pungercar J (2008) A presynaptically toxic secreted phospholipase A2 is internalized into motoneuron-like cells where it is rapidly translocated into the cytosol. Biochim Biophys Acta 1783(6):1129–1139
Wisniewski T, Frangione B (1996) Molecular biology of brain aging and neurodegenerative disorders. Acta Neurobiol Exp (Wars) 56(1):267–279
Yagami T (2006) Cerebral arachidonate cascade in dementia: Alzheimer’s disease and vascular dementia. Curr Neuropharmacol 4(1):87–100
Lin TN, Wang Q, Simonyi A, Chen JJ, Cheung WM, He YY, Xu J, Sun AY, Hsu CY, Sun GY (2004) Induction of secretory phospholipase A2 in reactive astrocytes in response to transient focal cerebral ischemia in the rat brain. J Neurochem 90(3):637–645
Moses GS, Jensen MD, Lue LF, Walker DG, Sun AY, Simonyi A, Sun GY (2006) Secretory PLA2-IIA: a new inflammatory factor for Alzheimer’s disease. J Neuroinflammation 3:28
Bezprozvanny I, Mattson MP (2008) Neuronal calcium mishandling and the pathogenesis of Alzheimer’s disease. Trends Neurosci 31(9):454–463
Ueda K, Shinohara S, Yagami T, Asakura K, Kawasaki K (1997) Amyloid beta protein potentiates Ca2+ influx through L-type voltage-sensitive Ca2+ channels: a possible involvement of free radicals. J Neurochem 68(1):265–271
Mattson MP, Cheng B, Davis D, Bryant K, Lieberburg I, Rydel RE (1992) beta-Amyloid peptides destabilize calcium homeostasis and render human cortical neurons vulnerable to excitotoxicity. J Neurosci 12(2):376–389
Ueda K, Fukui Y, Kageyama H (1994) Amyloid beta protein-induced neuronal cell death: neurotoxic properties of aggregated amyloid beta protein. Brain Res 639(2):240–244
Yagami T, Ueda K, Asakura K, Nakazato H, Hata S, Kuroda T, Sakaeda T, Sakaguchi G, Itoh N, Hashimoto Y, Hori Y (2003) Human group IIA secretory phospholipase A2 potentiates Ca2+ influx through l-type voltage-sensitive Ca2+ channels in cultured rat cortical neurons. J Neurochem 85(3):749–758
Viola HM, Arthur PG, Hool LC (2007) Transient exposure to hydrogen peroxide causes an increase in mitochondria-derived superoxide as a result of sustained alteration in l-type Ca2+ channel function in the absence of apoptosis in ventricular myocytes. Circ Res 100(7):1036–1044
Nunomura A, Perry G, Aliev G, Hirai K, Takeda A, Balraj EK, Jones PK, Ghanbari H, Wataya T, Shimohama S, Chiba S, Atwood CS, Petersen RB, Smith MA (2001) Oxidative damage is the earliest event in Alzheimer disease. J Neuropathol Exp Neurol 60(8):759–767
Paola D, Domenicotti C, Nitti M, Vitali A, Borghi R, Cottalasso D, Zaccheo D, Odetti P, Strocchi P, Marinari UM, Tabaton M, Pronzato MA (2000) Oxidative stress induces increase in intracellular amyloid beta-protein production and selective activation of betaI and betaII PKCs in NT2 cells. Biochem Biophys Res Commun 268(2):642–646
Harada J, Sugimoto M (1999) Activation of caspase-3 in beta-amyloid-induced apoptosis of cultured rat cortical neurons. Brain Res 842(2):311–323
Lee C, Park DW, Lee J, Lee TI, Kim YJ, Lee YS, Baek SH (2006) Secretory phospholipase A2 induces apoptosis through TNF-alpha and cytochrome c-mediated caspase cascade in murine macrophage RAW 264.7 cells. Eur J Pharmacol 536(1–2):47–53
Black SE (2005) Vascular dementia. Stroke risk and sequelae define therapeutic approaches. Postgrad Med 117(1):15–16, 19–25
in’t Veld BA, Ruitenberg A, Hofman A, Stricker BH, Breteler MM (2001) Antihypertensive drugs and incidence of dementia: the Rotterdam Study. Neurobiol Aging 22(3):407–412
Schehr RS (1996) New treatments for acute stroke. Nat Biotechnol 14(11):1549–1554
Umemura K, Kawai H, Ishihara H, Nakashima M (1995) Inhibitory effect of clopidogrel, vapiprost and argatroban on the middle cerebral artery thrombosis in the rat. Jpn J Pharmacol 67(3):253–258
Hallenbeck JM (1994) Blood-damaged tissue interaction in experimental brain ischemia. Acta Neurochir Suppl (Wien) 60:233–237
Li Y, Sharov VG, Jiang N, Zaloga C, Sabbah HN, Chopp M (1995) Ultrastructural and light microscopic evidence of apoptosis after middle cerebral artery occlusion in the rat. Am J Pathol 146(5):1045–1051
Yagami T, Ueda K, Asakura K, Hayasaki-Kajiwara Y, Nakazato H, Sakaeda T, Hata S, Kuroda T, Takasu N, Hori Y (2002) Group IB secretory phospholipase A2 induces neuronal cell death via apoptosis. J Neurochem 81(3):449–461
Yagami T, Ueda K, Asakura K, Sakaeda T, Hata S, Kuroda T, Sakaguchi G, Itoh N, Hashimoto Y, Hori Y (2003) Porcine pancreatic group IB secretory phospholipase A2 potentiates Ca2+ influx through l-type voltage-sensitive Ca2+ channels. Brain Res 960(1–2):71–80
Prat A, Antel J (2005) Pathogenesis of multiple sclerosis. Curr Opin Neurol 18(3):225–230
Pinto F, Brenner T, Dan P, Krimsky M, Yedgar S (2003) Extracellular phospholipase A2 inhibitors suppress central nervous system inflammation. Glia 44(3):275–282
Cunningham TJ, Yao L, Oetinger M, Cort L, Blankenhorn EP, Greenstein JI (2006) Secreted phospholipase A2 activity in experimental autoimmune encephalomyelitis and multiple sclerosis. J Neuroinflammation 3:26
Profyris C, Cheema SS, Zang D, Azari MF, Boyle K, Petratos S (2004) Degenerative and regenerative mechanisms governing spinal cord injury. Neurobiol Dis 15(3):415–436
Titsworth WL, Cheng X, Ke Y, Deng L, Burckardt KA, Pendleton C, Liu NK, Shao H, Cao QL, Xu XM (2009) Differential expression of sPLA2 following spinal cord injury and a functional role for sPLA2-IIA in mediating oligodendrocyte death. Glia 57(14):1521–1537
Yegin A, Akbas SH, Ozben T, Korgun DK (2002) Secretory phospholipase A2 and phospholipids in neural membranes in an experimental epilepsy model. Acta Neurol Scand 106(5):258–262
Visioli F, Rodriguez de Turco EB, Kreisman NR, Bazan NG (1994) Membrane lipid degradation is related to interictal cortical activity in a series of seizures. Metab Brain Dis 9(2):161–170
Lambeau G, Ancian P, Barhanin J, Lazdunski M (1994) Cloning and expression of a membrane receptor for secretory phospholipases A2. J Biol Chem 269(3):1575–1578
Lambeau G, Barhanin J, Schweitz H, Qar J, Lazdunski M (1989) Identification and properties of very high affinity brain membrane-binding sites for a neurotoxic phospholipase from the Taipan venom. J Biol Chem 264(19):11503–11510
Copic A, Vucemilo N, Gubensek F, Krizaj I (1999) Identification and purification of a novel receptor for secretory phospholipase A(2) in porcine cerebral cortex. J Biol Chem 274(37):26315–26320
Dev KK, Foged C, Andersen H, Honore T, Henley JM (1997) High-affinity binding sites for 125I-labelled pancreatic secretory phospholipase A2 in rat brain. Brain Res Mol Brain Res 49(1–2):120–126
Higashino K, Ishizaki J, Kishino J, Ohara O, Arita H (1994) Structural comparison of phospholipase-A2-binding regions in phospholipase-A2 receptors from various mammals. Eur J Biochem 225(1):375–382
Nakajima M, Hanasaki K, Ueda M, Arita H (1992) Effect of pancreatic type phospholipase A2 on isolated porcine cerebral arteries via its specific binding sites. FEBS Lett 309(3):261–264
Kishino J, Ohara O, Nomura K, Kramer RM, Arita H (1994) Pancreatic-type phospholipase A2 induces group II phospholipase A2 expression and prostaglandin biosynthesis in rat mesangial cells. J Biol Chem 269(7):5092–5098
Arita H, Hanasaki K, Nakano T, Oka S, Teraoka H, Matsumoto K (1991) Novel proliferative effect of phospholipase A2 in Swiss 3T3 cells via specific binding site. J Biol Chem 266(29):19139–19141
Hanasaki K, Arita H (1992) Characterization of a high affinity binding site for pancreatic-type phospholipase A2 in the rat. Its cellular and tissue distribution. J Biol Chem 267(9):6414–6420
Ishizaki J, Hanasaki K, Higashino K, Kishino J, Kikuchi N, Ohara O, Arita H (1994) Molecular cloning of pancreatic group I phospholipase A2 receptor. J Biol Chem 269(8):5897–5904
Yokota Y, Hanasaki K, Ono T, Nakazato H, Kobayashi T, Arita H (1999) Suppression of murine endotoxic shock by sPLA2 inhibitor, indoxam, through group IIA sPLA2-independent mechanisms. Biochim Biophys Acta 1438(2):213–222
Kolko M, de Turco EB, Diemer NH, Bazan NG (2002) Secretory phospholipase A2-mediated neuronal cell death involves glutamate ionotropic receptors. Neuroreport 13(15):1963–1966
Ray SK, Banik NL (2003) Calpain and its involvement in the pathophysiology of CNS injuries and diseases: therapeutic potential of calpain inhibitors for prevention of neurodegeneration. Curr Drug Targets CNS Neurol Disord 2(3):173–189
Sorce S, Krause KH (2009) NOX enzymes in the central nervous system: from signaling to disease. Antioxid Redox Signal 11(10):2481–2504
Bey EA, Xu B, Bhattacharjee A, Oldfield CM, Zhao X, Li Q, Subbulakshmi V, Feldman GM, Wientjes FB, Cathcart MK (2004) Protein kinase C delta is required for p47phox phosphorylation and translocation in activated human monocytes. J Immunol 173(9):5730–5738
Simonyi A, He Y, Sheng W, Sun AY, Wood WG, Weisman GA, Sun GY (2010) Targeting NADPH oxidase and phospholipases A2 in Alzheimer’s disease. Mol Neurobiol 41(2–3):73–86
Brennan AM, Suh SW, Won SJ, Narasimhan P, Kauppinen TM, Lee H, Edling Y, Chan PH, Swanson RA (2009) NADPH oxidase is the primary source of superoxide induced by NMDA receptor activation. Nat Neurosci 12(7):857–863
Shelat PB, Chalimoniuk M, Wang JH, Strosznajder JB, Lee JC, Sun AY, Simonyi A, Sun GY (2008) Amyloid beta peptide and NMDA induce ROS from NADPH oxidase and AA release from cytosolic phospholipase A2 in cortical neurons. J Neurochem 106(1):45–55
Sherry ST, Ward M, Sirotkin K (1999) dbSNP-database for single nucleotide polymorphisms and other classes of minor genetic variation. Genome Res 9(8):677–679
Eckert GP, Schaeffer EL, Schmitt A, Maras A, Gattaz WF (2011) Increased brain membrane fluidity in schizophrenia. Pharmacopsychiatry 44(4):161–162
Schaeffer EL, Gattaz WF, Eckert GP (2012) Alterations of brain membranes in Sshizophrenia: impact of phospholipase A2. Curr Top Med Chem
Barbosa NR, Junqueira RM, Vallada HP, Gattaz WF (2007) Association between BanI genotype and increased phospholipase A2 activity in schizophrenia. Eur Arch Psychiatry Clin Neurosci 257(6):340–343
Bate C, Reid S, Williams A (2004) Phospholipase A2 inhibitors or platelet-activating factor antagonists prevent prion replication. J Biol Chem 279(35):36405–36411
Bate C, Tayebi M, Williams A (2008) Sequestration of free cholesterol in cell membranes by prions correlates with cytoplasmic phospholipase A2 activation. BMC Biol 6:8
Yoshino H, Tomiyama H, Tachibana N, Ogaki K, Li Y, Funayama M, Hashimoto T, Takashima S, Hattori N (2010) Phenotypic spectrum of patients with PLA2G6 mutation and PARK14-linked parkinsonism. Neurology 75(15):1356–1361
Klivenyi P, Beal MF, Ferrante RJ, Andreassen OA, Wermer M, Chin MR, Bonventre JV (1998) Mice deficient in group IV cytosolic phospholipase A2 are resistant to MPTP neurotoxicity. J Neurochem 71(6):2634–2637
Tariq M, Khan HA, Al Moutaery K, Al Deeb S (2001) Protective effect of quinacrine on striatal dopamine levels in 6-OHDA and MPTP models of Parkinsonism in rodents. Brain Res Bull 54(1):77–82
Pereira MP, Hurtado O, Cardenas A, Bosca L, Castillo J, Davalos A, Vivancos J, Serena J, Lorenzo P, Lizasoain I, Moro MA (2006) Rosiglitazone and 15-deoxy-Delta12,14-prostaglandin J2 cause potent neuroprotection after experimental stroke through noncompletely overlapping mechanisms. J Cereb Blood Flow Metab 26(2):218–229
Yagami T, Ueda K, Asakura K, Takasu N, Sakaeda T, Itoh N, Sakaguchi G, Kishino J, Nakazato H, Katsuyama Y, Nagasaki T, Okamura N, Hori Y, Hanasaki K, Arimura A, Fujimoto M (2003) Novel binding sites of 15-deoxy-Delta12,14-prostaglandin J2 in plasma membranes from primary rat cortical neurons. Exp Cell Res 291(1):212–227
Conflicts of interest
The authors have declared that no competing interests exist.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yagami, T., Yamamoto, Y. & Koma, H. The Role of Secretory Phospholipase A2 in the Central Nervous System and Neurological Diseases. Mol Neurobiol 49, 863–876 (2014). https://doi.org/10.1007/s12035-013-8565-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-013-8565-9