Abstract
Nitric oxide is a short-lived intracellular and intercellular messenger. The first realisation that nitric oxide is important in physiology occurred in 1987 when its identity with the endothelium-derived relaxing factor was discovered. Subsequent studies have shown that nitric oxide possesses a number of physiological functions that are essential not only to vascular homeostasis but also to neurotransmission, such as in the processes of learning and memory and endocrine gland regulation, as well as inflammation and immune responses. The discovery in 1995 that a splice variant of the neuronal nitric oxide synthase is localised at the sarcolemma via the dystrophin–glycoprotein complex and of its displacement in Duchenne muscular dystrophy has stimulated a host of studies exploring the role of nitric oxide in skeletal muscle physiology. Recently, nitric oxide has emerged as a relevant messenger also of myogenesis that it regulates at several key steps, especially when the process is stimulated for muscle repair following acute and chronic muscle injuries. Here, we will review briefly the mechanisms and functions of nitric oxide in skeletal muscle and discuss its role in myogenesis, with specific attention to the promising nitric oxide-based approaches now being explored at the pre-clinical and clinical level for the therapy of muscular dystrophy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 1987, nitric oxide (NO) was identified as the gaseous messenger accounting for the vasodilating activity of the endothelium-derived relaxing factor originally described by Furchgott [1, 2], explaining also why organic nitrates and sodium nitroprusside have therapeutic efficacy in diseases affecting the cardiovascular system. Since then, thousands of papers have elucidated the molecular mechanisms of NO action and described its biological role not only in the cardiovascular system but also in neurones and virtually in all other mammalian cells and tissues. The discovery that a NO synthesising enzyme, a splice variant of the neuronal NO synthase, is expressed in skeletal muscle and that its localisation and activity are altered in Duchenne muscular dystrophy opened new perspectives on the physiological role of this messenger. In the last 20 years, the role of NO in skeletal muscle physiology has been investigated in detail; more recently, its role in myogenesis has also been explored. This review summarises our current understanding on the role of NO in skeletal muscle pathophysiology and describes how this new evidence is opening exciting perspectives for the use of NO-donating drugs as therapeutic agents for muscle repair in muscular dystrophies.
The Nitric Oxide System and Skeletal Muscle Physiology
Nitric Oxide Synthases in Skeletal Muscle
NO is synthesised from l-arginine and oxygen by NO synthases (NOS) in almost all mammalian cells and tissues [3, 4]. Three distinct isoforms of NOS have been identified, two of which, namely the endothelial (eNOS) and neuronal (nNOS) isoforms, are regulated by second messengers, whereas one is inducible by cytokines and bacterial products (iNOS).
All three NOS isoforms are expressed in skeletal muscle: nNOS has been detected in several human muscles, including gastrocnemius and quadriceps muscles, and in rodent diaphragma, soleus, tibialis anterior and extensor digitorum longus muscles. Neuronal NOS is abundant at the surface of type II fibres (fast twitch), whereas it is less represented in type I (slow twitch) fibres [5]. Likewise, eNOS has been described in several muscles as a peripheral membrane protein, which is bound to plasmalemmal caveolae through specific interaction with caveolin-1 and caveolin-3. Inducible NOS messenger RNA is absent or present at very low levels in skeletal muscles under physiological conditions. The three NOS isoforms differ in their mechanisms of activation, regulation and catalytic activity. Neuronal and endothelial NOS are constitutively expressed and require the Ca2+/calmodulin complex for their activation. Changes in the expression of these enzymes may occur: in skeletal muscle, expression of nNOS is increased by crush injury, muscle activity and ageing [6]; and that of eNOS, by chronic exercise and shear stress [7]. These changes, however, are usually of small extent. Both nNOS and eNOS produce NO at low, physiological levels (in the pico to nanomolar range) for short periods. Conversely, iNOS is expressed in skeletal muscle primarily under severe inflammatory conditions, such as in the course of autoimmune inflammatory myopathies [8] and after crash injury [6]. The activity of iNOS is independent of the Ca2+/calmodulin complex and generates NO at high concentrations (micromolar range) for prolonged periods.
Studies in recent years have uncovered an increasingly important role of physical association of the NOS isoforms with a variety of regulatory and structural proteins [9]. nNOS may be inhibited by interaction with caveolin-3 [10] or with PIN [11]; eNOS is activated by the interaction with the 90-kDa heat shock protein; and iNOS is inhibited by association with kalirin [12].
Of importance, these protein–protein interactions, as well as regulating the activity of NOSs often target them to cellular membranes. The N-terminus of nNOS contains a PDZ (post-synaptic density protein-95, discs-large, Z0-1) domain that allows interactions of the enzyme with other PDZ-containing proteins at the cellular plasma membrane. In skeletal muscle, the localisation of nNOS to the dystrophin–glycoprotein complex at sarcolemma, due to the binding via one of these PDZ-containing proteins, α1-syntrophin [13], is a key aspect that explains the coupling of NO generation with muscle contractile activity. Pathological features of muscular dystrophies are, in part, due to the displacement of nNOS from the sarcolemma as a consequence of the disruption of the dystrophin–glycoprotein complex [13]. Endothelial NOS is localised at both the plasma membrane and the Golgi complex through its ability to be myristoylated and palmitoylated [14]. In addition, both iNOS and eNOS may interact with caveolin 1 and/or 3, proteins responsible not only for the localisation of these enzymes at the plasma membrane but also for the regulation of their activity and expression in an inhibitory fashion [15, 16].
Nitric Oxide Action in Skeletal Muscle Physiology
The role of NO in the regulation of skeletal muscle physiological activity, including excitation–contraction coupling, auto-regulation of blood flow, calcium homeostasis and bioenergetics has been investigated extensively; several excellent reviews on it are already present in the literature. We will, thus, only briefly highlight here those effects of NO that contribute to its therapeutic role in muscle repair and concentrate our focus on its effects on myogenesis, which have not been reviewed to date.
NO exerts its effects in skeletal muscle by activation of the NO-dependent guanylyl cyclase, with formation of cyclic GMP, inhibition of cytochrome c oxidase in the mitochondrial respiratory chain and/or S-nitrosylation, the covalent attachment of a nitrogen monoxide group to the thiol side chain of cysteine. These three events in turn activate a variety of downstream signalling cascades that ultimately shape skeletal muscle responses to NO.
Generation of cyclic GMP appears of particular relevance. Alongside mediating most of NO effects on myogenesis, as outlined below, cyclic GMP-dependent signalling plays a major role in NO-dependent vasodilation and vascular responses and presides over complex intracellular crosstalk events involving calcium and sphingolipids, which are key players in muscle homeostasis [17, 18]. In addition, cyclic GMP mediates the NO-dependent biogenesis of mitochondria, which occurs via activation of a pathway involving sirtuin 1, the peroxisome proliferator-activated receptor-γ coactivator 1-α, the nuclear respiratory factor 1 and the mitochondrial transcription factor A [19]. Increased mitochondrial biogenesis leads to an enhanced ability by the skeletal muscle to generate ATP via mitochondrial respiration [20]. Such an effect is complemented by NO-dependent stimulation of glucose transport [7], both in the case of insulin [5, 21] and exercise-stimulated glucose uptake [21].
Inhibition of cytochrome c oxidase in mitochondria that occurs at physiological concentrations of NO is conceivably relevant in skeletal muscle although specific studies on this aspect are still missing. Whenever investigated, the binding of NO to cytochrome c oxidase is reversible, occurs in competition with oxygen and results in inhibition of enzyme activity [22, 23]. The interaction of NO with cytochrome c oxidase, together with regulation of the expression of the hypoxia-inducible factor 1 α, also dependent on the NO-cytochrome c oxidase interaction [24], may contribute to a fine-tuning of skeletal muscle cell metabolism, adapting it to low oxygen conditions.
The observation that nNOS is localised in close proximity with mitochondria suggests a tight coupling between NO generation and regulation of mitochondrial respiration and metabolism [25]. As a consequence of cytochrome c oxidase regulation [26, 27], NO controls the generation of reactive oxygen species preventing their excessive generation and ensuing toxicity. This is particularly relevant since small concentrations of these radicals, generated physiologically under NO control, may be beneficial and contribute to the maintenance of an antioxidant defence in tissues [26].
A significant contribution to regulation of NO concentrations in muscle, with consequence also on its bioenergetic role, comes from myoglobin that acts as a NO scavenger in skeletal muscle, thus regulating its delivery [28]. Myoglobin expression is developmentally regulated in skeletal muscle, and its expression is higher in oxidative, fatigue-resistant fibres [29]. In myoglobin-deficient mice there is an increased compensatory stimulation of skeletal muscle NO generation, associated with other changes relevant to metabolism such as fibre type transition (type I to type II in the soleus muscle), increased expression of the hypoxia-inducible factor 1 α, stress proteins such as heat shock protein 27, and the vascular endothelial growth factor that stimulates angiogenesis [30].
The third main mechanism of NO action, S-nitrosylation, regulates the activity of several enzymes that are important in skeletal muscle physiology, among which are phosphatases, caspases and oxidoreductases [31–35] as well as several transcription factors, such as p53 and NF-κB [36, 37] Two other important S-nitrosylation-dependent effects deserve mention: the regulation of oxygen binding to, and release from, haemoglobin [38] and thus the supply of oxygen to mitochondria, and the activity of type II histone deacetylases that is relevant to muscle repair, as will be explained below [39, 40].
Nitric Oxide in Myogenesis and Skeletal Muscle Repair
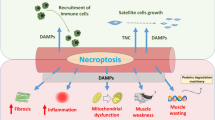
Post-natal skeletal muscle is able to continuously regenerate its fibres following damage. Such ability is mostly dependent on myogenic precursor cells. Among these cells, particularly relevant are the satellite cells (SC), which are located under the basal lamina of myofibres, although other interstitial stem cells may also play a role [41]. SC activate and differentiate upon muscle injury contributing significantly to its repair. In addition, SC are characterised by reversible quiescence and self-renewal capacities that are critical to maintain their reserve pool which is used to sustain tissue regeneration during numerous rounds of damage [42, 43]. Several studies in the last decade have shown that NO regulates these myogenic precursor cells through a variety of actions, mediated by different signal transduction pathways and downstream effectors. Of importance, it also appears that such regulation can be sustained by NO generated endogenously by these same cells, although NO produced by myofibres or endothelial cells may also play a role. These various actions of NO converge in stimulating, on the one hand, the process of proliferation, activation and differentiation of these cells; on the other hand, in maintaining their reserve pool so that it does not become exhausted during physiological muscle damage. Such mechanisms by NO, described below in detail, account not only for its physiological role in myogenesis but also explain, at least in part, why NO may have therapeutic efficacy in pathologies, such as muscular dystrophies, where the muscle is subject to repetitive rounds of damage. Figure 1 summarizes on the various actions through which NO stimulates muscle repair and the relevant mechanisms mediating its effect.
Schematic diagram summarising the various actions through which NO stimulates muscle repair and the relevant mechanisms mediating the effect of NO. The upper inset depicts how NO regulates the differentiation of the myogenic precursor cells pool leading to enhanced myogenesis, which is a key action of NO as a muscle healer (blue boxes, phases of myogenic differentiation regulated by NO; white boxes, mechanisms of NO-dependent control). In particular, NO stimulates the myogenic precursor cells proliferation in a way that the quiescent reserve pool is also maintained. This action is exerted via a combined stimulation of cell cycle and enhanced expression of Vangl-2, a key transcription factor in the Wnt non-canonical pathway. NO stimulates also activation of the myogenic precursor cells via hepatocyte growth factor release and favours the differentiation of these cells by inhibiting Drp-1 activity and thereby mitochondrial fission, with formation of bioenergetically competent elongated mitochondria. Finally, NO drives the fusion of the myogenic precursor cells between themselves and to the existing myofibres by enhancing the expression and release of follistatin. Several other effects, exerted directly on the skeletal muscle myofibres, synergise with the actions of NO on myogenesis towards muscle repair. NO generated by nNOS during muscle contractile activity induces vasodilation and thereby increases the supply of nutrients and oxygen to the contracting muscle. A relevant event in this respect is the increase in the expression of the glucose transporter GLUT4 leading to increased glucose uptake by the muscle. NO also exerts a relevant control of muscle bioenergetics, by increasing mitochondrial biogenesis in a pathway involving sirtuin-1-dependent increase in expression of the mitochondrial biogenetic transcription factors peroxisome proliferator-activated receptor-γ coactivator 1-α, nuclear respiratory factor 1 and mitochondrial transcription factor A. Such mitochondrial biogenesis is accompanied by a tight control of mitochondrial respiration through direct and reversible inhibition of cytochrome c oxidase in competition with oxygen, with reduced generation of noxious reactive oxygen species. NO has been reported also to control the activity of immune competent cells. This action may account for inhibition of inflammation in the damaged muscle observed with some NO-donating drugs such as molsidomine, even if muscle repair is best observed by combining NO donation with a frank inhibition of inflammation obtained by co-administration of NSAIDs
Nitric Oxide and Satellite Cells Proliferation: Maintenance of the Satellite Cells Reserve Pool
The state of quiescence of SC is characterised by the persistence of a G0 phase, the expression of several markers including M-cadherin, syndecans 3 and 4, CD34, α-7 integrin, Sca-1, SM/C 2.6 [44–47] and the expression of the paired-box protein Pax7, a regulator of cell survival and myogenic progression [48, 49]. Upon activation, SC proliferate and give rise to a population of myoblasts expressing myogenic regulatory factors among which is Myf5; activated SC progressively down-regulate Pax7 and, after multiple rounds of cell division, terminally differentiate to finally fuse and generate new fibres [50, 51]. A subset of SC maintains or re-expresses Pax7 and returns to quiescence by both symmetric and asymmetric division [52]. This “reserve cell” pool is particularly relevant as it is the one accounting physiologically for muscle repair throughout a lifespan.
Among the several factors involved in SC self-renewal identified so far, members of the canonical/β-catenin-dependent and of the non-canonical Wnt pathways appear to be relevant, the latter involving Wnt7a, its receptor Frizzled7 (Fzd7) and Vangl2, the mammalian homologue of the Drosophila Vangl2/Stbm [53–60].
We have recently demonstrated that NO acts both on proliferation of SC and the maintenance of their reserve pool; NO stimulates proliferation of SC via generation of cyclic GMP [61], while the maintenance of the pool of Pax7+Myf5− SC depends on the Vangl2-dependent Wnt non-canonical pathway. The cyclic GMP-dependent effect on proliferation is in line with previous reports about the mitogenic action of NO, for which the effectors downstream of cyclic GMP have been identified [62–64]. The effect of NO on Vangl2 signalling suggests that NO acts not only in adult skeletal muscle but also during embryonic muscle development, since the non-canonical Wnt pathway plays a role in differential activation of genes in epaxial or hypaxial progenitors [65, 66]. While the effect of NO on embryonic myogenesis needs to be investigated further, the role of NO on adult muscle appears of importance as it prevents the exhaustion of the SC pool in case of severe muscle damage, such as in muscular dystrophy [61]. In this conditions, genetic ablation of nNOS in fibres or treatment with NOS inhibitors is sufficient to induce progressive reduction of the muscle regenerative capacity [61], confirming the obligatory role of NO in maintaining the myogenic precursor pool in vivo.
Nitric Oxide and Satellite Cells Activation
One of the initial reports about a role of NO in myogenesis was on its ability to induce activation of SC immediately upon damage [67]. Reduced NOS activity prevented the increase in myogenic cells yield, when they were isolated from the injured muscle, and delayed the activation of SC after isolation [67]. Further, a single administration of NOS inhibitors in rats subjected to muscle trauma prevented the increase of SC number [68]; rats in which NOS activity was inhibited also showed increased levels of collagen, suggesting that blocking NO signal in the early phase of injury impairs muscle repair, favouring fibrotic scar tissue production. The mechanism by which NO influences SC activation involves release of the hepatocyte growth factor from extracellular matrix [69]. The molecular mechanism leading to the release of this growth factor has not been investigated in detail, although it was reported that NO acted through metalloproteinases induction [69].
Nitric Oxide and Myogenic Differentiation
Alongside the control by NO of mitochondrial respiration and mitochondrial biogenesis, relevant for adult skeletal muscle homeostasis, a third action by NO on mitochondria more directly relevant for myogenesis has been recently described. During myogenic differentiation, the short mitochondria of the myoblasts change into the extensive elongated network observed in the myotubes [70], suggesting that they may have a role in myogenesis. Such an effect appears to initiate already in differentiating myoblasts prior to their fusion [71]. Physiological generation of NO was found to inhibit the activity of the dynamin-related protein 1 (Drp-1), a protein playing a key role in the process of mitochondrial fission. Inhibition of the synthesis of NO in myogenic precursors enhanced the activity, translocation and docking to mitochondria of Drp-1, leading to inhibition of mitochondrial elongation [71]. Under this condition, differentiating myoblasts displayed a latent mitochondrial dysfunction. These effects, due to NO synthesis blockade, were not observed when Drp-1 action was counteracted by its dominant negative form. This establishes a formal link between NO generation and inhibition of Drp-1 activity [71]. Both the NO-dependent repression of Drp-1 action and the maintenance of mitochondrial integrity are reversible (with a fast onset and offset) and mediated by generation of cyclic GMP. Of importance, the inhibition of mitochondrial fission by NO has physiological consequences as it allows myogenesis to occur [71]. This indicates that NO exerts a quality control check on differentiation by regulating mitochondrial morphology and function.
In neurones, high cytotoxic concentrations of NO have been reported to promote mitochondrial fission and apoptosis via S-nitrosylation of Drp-1 [72, 73], i.e. a mechanism different from the cyclic GMP-dependent phosphorylation described above, which activates rather than inhibits the enzyme. The findings in neurones are only apparently contradictory to the those in the skeletal muscle, in keeping with the concept that NO is a double-edged messenger that, depending on its concentration, mechanism and site of action, can have opposing effects on a particular mechanism or target [74, 75].
Why an elongated mitochondrial network is required in differentiating skeletal muscle, at variance with other tissues such as the liver where respiration is sustained by short mitochondria, remains to be established. A possibility resides in the specific architecture of the myotubes, especially in their need of sustaining the activity of the actin–myosin contractile apparatus [76].
The fact that mitochondrial volume and network extension correlate positively with the efficiency of mitochondrial respiratory function and myogenic differentiation of myogenic precursor cells has biological relevance also for the mature myofibres. The decrease in mitochondrial size observed in tissues from eNOS null mice [19] is likely to be a morphological correlate of the reduced mitochondrial function. Likewise, impaired oxidative phosphorylation has been reported in dystrophic muscles, which lack a functional nNOS [77–81].
Nitric Oxide and Myogenic Precursor Cells Fusion
The effect of NO on myogenic precursor cell fusion was described for the first time in 1994 when Lee and collaborators [82] showed a peak in NOS activity in chicken myoblast competent for fusion, but not in proliferating myoblasts and myotubes. In this fusion-competent myogenic precursor cells, NO induced early fusion, whereas inhibition of NO production delayed the time of fusion [82].
The mechanisms and biological relevance of the fusogenic action of NO on myogenic precursor cells was investigated further. In particular, NO was found to be crucial for the fusion of SC also in mammals [83]. Of importance, this effect was observed not only on adult SC but also on the presomitic mesoderm, further indicating that NO has an effect, still to be characterised in full detail, at critical stages of pre-postnatal muscle developmental life. The mechanism of NO action on fusion is mediated via cyclic GMP production and enhanced expression and release of follistatin [83].
Follistatin induction by NO/cGMP involves MyoD, NFAT and CREB. The fact that MyoD, CREB, and NFAT mediate the transcriptional effect of NO resembles the situation already described for stimulation of myoblast fusion by the deacteylase inhibitor trichostatin A [84]. Follistatin is also essential in mediating the effect of trichostatin A on muscle size and SC recruitment interacting with, and regulating the biological activity of, transforming growth factor-β family members and by blocking myostatin [84]. The similarity between the action of trichostatin A and NO and the evidence that trichostatin A up-regulates the expression of eNOS in non endothelial cells [85, 86], suggesting that NO is involved in regulating the process of acetylation. Indeed, it has now been demonstrated that NO inhibits the activity of class IIa histone deacetylases via S-nitrosylation [39, 40]. Of importance, the nitrosylation state of class IIa histone deacetylases influences the expression of specific microRNAs genes important for muscle regeneration [87], indicating that nNOS, follistatin, class IIa histone deacetylases and microRNAs are in the same regulatory pathway.
Neuronal, Inducible and Endothelial Nitric Oxide Synthases: Which Roles Do They Play in Myogenesis?
From the evidence reported in the paragraphs above, NO clearly emerges as a key messenger presiding over several crucial steps of myogenic differentiation important in muscle repair; still, the role of NO in muscle repair needs further clarification. In certain conditions, NO may be even detrimental. Rubinstein and collaborators [6] showed that muscle crush is associated with activation of the NO system, and that this is an important mechanism leading to muscle damage. The detrimental action by NO observed by these authors may be due to excessive NO production in their experimental system where iNOS and eNOS are up-regulated.
Studies are still needed also to clarify the role of the three NOS isoforms, in particular, the role of eNOS for which a function, if any, in muscle repair has not been established.
The role of iNOS has been investigated to some extent. This enzyme is up-regulated during muscle mechanical damage and has been shown to play a negative effect on regeneration [6, 68, 88]. Indeed, ablation of iNOS in dystrophin-deficient mice significantly reduces muscle membrane lysis, suggesting that iNOS promotes injury of dystrophic muscles, an effect that appears to be due to the enhanced infiltration of the diseased tissue by iNOS-expressing M1 macrophages [89]. Yet, in another study, the role played by this enzyme in dystrophy appears to be minor, if any [90].
The role of nNOS for muscle physiological repair appears instead more clearly defined. Alongside its absence from the sarcolemma of mdx mice and of patients affected by Duchenne muscular dystrophy [91], nNOS mislocalisation has been observed in models of other pathologies affecting muscle homeostasis and performance, such as in mouse models of limb-girdle muscular dystrophy (α, β and δ sarcoglycan null mice) [92] and in models of amyotrophic lateral sclerosis and catabolic stress [93, 94]. Neuronal NOS overexpression in mdx mice significantly ameliorates the dystrophic phenotype [95].
Indeed, nNOS null mice show reduced skeletal muscle mass, reduced maximum titanic force with a more severe phenotype in male mice compared to female [96]. Neuronal NOS null mice display an altered activation of SC [67], and even if they regenerate after myotoxic injury [97], no complete restitutio ad integrum of muscle tissue has been observed. Indeed, significant pathological alterations are still present, including a significantly reduced cross-sectional area of the newly regenerated myofibres [97].
Neuronal NOS deficiency causes also an increased susceptibility to contraction-induced fatigue both in male and female mice. Thus, aberrant nNOS signalling impairs three important clinical features common to dystrophinopathies and sarcoglycanopathies: maintenance of muscle bulk, force generation and fatigability. Finally, nNOS plays a significant role in muscle auto-regulation of blood flow. While normal blood flow and exercise-induced hyperaemia are generally preserved in nNOS null mice, they lack contraction-induced suppression of adrenergic vasoconstriction [98, 99]. Strikingly, contraction fails to suppress adrenergic vasoconstriction also in mdx mice, consistent with their reduced NOS function [99]. Because of these haemodynamic effects, nNOS deficiency has been associated with induction of inactivity after mild exercise, and it has been clearly shown that the lack of normal cyclic GMP response as a consequence of reduced NO generation leads to narrowing of vasculature and reduced muscle nutrient supply [100]. In dystrophic patients with an already altered muscle homeostasis, these haemodynamic effects may contribute to the worsening of muscle structure [98].
Nitric Oxide and the Therapy of Muscular Dystrophies
The need for novel therapeutic strategies for muscular dystrophies is particularly urgent. The therapeutic protocols currently in use are still based on corticosteroid administration. These drugs, while delaying the progression of the disease, are associated with severe side effects [101], such that optimisation of their use is still being actively pursued, and a clinical trial to this end has just been initiated. Therapies that substitute corticosteroids or at least may act as corticosteroid-sparing drugs are, thus, being actively investigated.
Whereas exon skipping and stem cell approaches appear to be significant steps forward to a resolutive therapy, they are expensive and still not really available, as the results of the last clinical trials indicate [102–105]. In addition, they target only specific subsets of patients (e.g. about 13 % in the case of exon 51 skipping). “Classical” pharmacological approaches appear therefore still attractive and of significant value, as they address all patients and at affordable costs.
The well-known regulation by NO of skeletal muscle force excitation–contraction coupling, auto-regulation of blood flow and glucose homeostasis [106], alongside the newly characterised role of NO in myogenesis and muscle repair outlined above, suggests a possible use of NO as a tool for therapeutic strategies in Duchenne, Becker and limb-girdle muscular dystrophies, where genetic alterations in genes coding for structural muscle proteins lead to repeated and enhanced muscle damage during physiological activity. The role of NO as a therapeutic is also supported by the evidence that rescue of function in mdx and dystrophin/utrophin double-knockout mice does not require a strict nNOS localisation to, and generation of, NO at the sarcolemma [95, 107]. The efficacy of therapies based on the administration of NO has, thus, been investigated by several groups in mouse models of muscular dystrophy.
Approaches with only NO donors or the NOS substrate l-arginine yielded some amelioration of the mdx mouse dystrophic phenotype; however, none of these studies reported long-term observations. Thus, the assessment of the validity of NO donation/generation as a therapeutic strategy yielding persistent beneficial effects could not be defined [108–113]. Recently, the efficacy of two NO donors, the organic nitrate isosorbide dinitrate and molsidomine, has been investigated. Isosorbide dinitrate alone was not effective, and molsidomine showed a moderate long-term efficacy [61]. Why molsidomine is more effective than the other NO donors tested so far remains to be established. A likely possibility is that molsidomine is particularly effective in increasing SC number [61]. Such an action may depend on the pharmacokinetic profile of NO release by molsidomine or on the fact that it releases also biologically active nitrites and nitrates [114], which have beneficial functions in skeletal muscle [115, 116]. Notwithstanding the positive results with molsidomine, a strategy based on NO donation alone appears not endowed with the characteristics of clinical efficacy needed for an effective pharmacological therapy.
An alternative strategy is to use NO donation in combination with anti-inflammatory drugs. A study in mdx mice indeed reported functional recovery using the association of l-arginine and the corticosteroid drug deflazacort on muscle voluntary exercise [117]. Despite the validity of such an approach, it still implies the use of corticosteroids. At variance with this approach, a different strategy has been tested, in which the anti-inflammatory activity was obtained using non-steroidal anti-inflammatory agents (NSAIDs).
Two approaches were used, one in which the NO-donating agent is a different molecular entity with respect to the NSAID, in particular, a combination of isosorbide dinitrate and ibuprofen; the other approach consisted of compounds of the CINOD class (cyclooxygenase-inhibiting nitric oxide (NO) donators) in which the two activities are combined in a single molecular entity [118]. All these drugs or drug combinations exerted significant therapeutic effects in both the α-sarcoglycan null and the mdx mouse models in the absence of relevant side effects or signs of toxicity. They significantly slowed disease progression and maintained the functional capacity of muscles. Of importance, the beneficial effects were found to persist long term, i.e. up to the end of the observation period, which was set at 12 months to mimic a chronic treatment in a clinical setting with patients. Several mechanisms synergised to yield the therapeutic effect of the combined therapy: significant reduction in both fibre damage and inflammation and increases in the myogenic precursor cells number and differentiation capacity, which preserve the long-term regeneration capacity of muscle [119–121]. Other actions of NO on skeletal muscle such as vasodilation and thus reduction of the ischaemia induced by nNOS displacement, increase in glucose uptake and in energy generation [106] may also have contributed to muscle repair. In addition, NO is a potent angiogenic factor [122], and angiogenesis may also significantly contribute to muscle repair [123]. An additional interesting aspect of these therapies is that they significantly enhance the homing of exogenously added myogenic stem cells to dystrophic muscles [119, 124]. This observation suggests the possibility of obtaining synergic effects by combining pharmacological with cell therapy approaches. Whereas no significant differences in the efficacy of CINOD vs. the combination of NO-donating drugs plus NSAID were observed, an advantage in therapeutic perspective of the use of a combination of drugs is the possibility of titrating the two active principles independently, thus optimising their use of single patients.
The therapeutic potential of the combination of the drugs isosorbide dinitrate and ibuprofen was also tested on dystrophic patients in an open-label pilot study in a cohort of adult patients affected by Duchenne, Becker and limb-girdle muscular dystrophies. The trial was designed mainly to evaluate safety and tolerability of the drug combination, but exploratory measures of efficacy, such as the motor function measure scale, were also applied. Good safety and tolerability profiles of the long-term co-administration of the drugs were demonstrated with only few and transient side effects. Of importance, the exploratory efficacy measures evidenced a trend towards amelioration that was significant in the D1 dimension of the motor function measure scale (assessing muscle standing and transfers) [125]. These results strongly indicate that the systemic administration of a combination of NO-donating drugs and NSAIDs (and possibly of CINODs) is of potential clinical relevance and should be optimised and further investigated in future clinical studies.
Concluding Remarks
The discovery of a role of NO in myogenesis and muscle repair and, thus, the possibility of using NO-based approaches in muscular dystrophies opens novel perspective for NO as a therapeutic molecule beyond cardiovascular disorders, which have been, to date, the only widely recognised field of application of NO donors in humans. The use of NO-donating molecules in muscular dystrophy brings about some important considerations. Firstly, NO donation alone appears insufficient to yield a full therapeutic benefit, which can be only obtained by combining the properties of NO with the anti-inflammatory activity of NSAIDs. Secondly, the pharmacological approach with NO (plus NSAIDs), while efficacious per se, may also constitute the basis for combinatorial therapies in which the pharmacological therapy is associated with stem cell approaches to obtain an enhanced therapeutic benefit. These aspects bring new life to NO donors as drugs, highlighting their use in novel therapeutic applications; in addition, they suggest that the use of NO donors in combination with cell and possibly gene therapies yields synergic effects that can be likely exploited also beyond the muscular systems.
References
Palmer RM, Ferrige AG, Moncada S (1987) Nitric oxide release accounts for the biological activity of endothelium-derived relaxing factor. Nature 327(6122):524–526
Furchgott RF, Zawadzki JV (1980) The obligatory role of endothelial cells in the relaxation of arterial smooth muscle by acetylcholine. Nature 288(5789):373–376
Alderton WK, Cooper CE, Knowles RG (2001) Nitric oxide synthases: structure, function and inhibition. Biochem J 357(Pt 3):593–615
Moncada S, Palmer RM, Higgs EA (1991) Nitric oxide: physiology, pathophysiology, and pharmacology. Pharmacol Rev 43(2):109–142
Kapur S, Bedard S, Marcotte B, Cote CH, Marette A (1997) Expression of nitric oxide synthase in skeletal muscle: a novel role for nitric oxide as a modulator of insulin action. Diabetes 46(11):1691–1700
Rubinstein I, Abassi Z, Coleman R, Milman F, Winaver J, Better OS (1998) Involvement of nitric oxide system in experimental muscle crush injury. J Clin Invest 101(6):1325–1333
Balon TW, Nadler JL (1997) Evidence that nitric oxide increases glucose transport in skeletal muscle. J Appl Physiol 82(1):359–363
Tews DS, Goebel HH (1998) Cell death and oxidative damage in inflammatory myopathies. Clin Immunol Immunopathol 87(3):240–247
Kone BC, Kuncewicz T, Zhang W, Yu ZY (2003) Protein interactions with nitric oxide synthases: controlling the right time, the right place, and the right amount of nitric oxide. Am J Physiol 285(2):F178–F190
Venema VJ, Ju H, Zou R, Venema RC (1997) Interaction of neuronal nitric-oxide synthase with caveolin-3 in skeletal muscle. Identification of a novel caveolin scaffolding/inhibitory domain. J Biol Chem 272(45):28187–28190
Jaffrey SR, Snyder SH (1996) PIN: an associated protein inhibitor of neuronal nitric oxide synthase. Science 274(5288):774–777
Ratovitski EA, Alam MR, Quick RA, McMillan A, Bao C, Kozlovsky C, Hand TA, Johnson RC, Mains RE, Eipper BA, Lowenstein CJ (1999) Kalirin inhibition of inducible nitric-oxide synthase. J Biol Chem 274(2):993–999
Brenman JE, Chao DS, Gee SH, McGee AW, Craven SE, Santillano DR, Wu Z, Huang F, Xia H, Peters MF, Froehner SC, Bredt DS (1996) Interaction of nitric oxide synthase with the postsynaptic density protein PSD-95 and alpha1-syntrophin mediated by PDZ domains. Cell 84(5):757–767
Fulton D, Fontana J, Sowa G, Gratton JP, Lin M, Li KX, Michell B, Kemp BE, Rodman D, Sessa WC (2002) Localization of endothelial nitric-oxide synthase phosphorylated on serine 1179 and nitric oxide in Golgi and plasma membrane defines the existence of two pools of active enzyme. J Biol Chem 277(6):4277–4284
Fulton D, Gratton JP, Sessa WC (2001) Post-translational control of endothelial nitric oxide synthase: why isn’t calcium/calmodulin enough? J Pharmacol Exp Ther 299(3):818–824
Felley-Bosco E, Bender FC, Courjault-Gautier F, Bron C, Quest AF (2000) Caveolin-1 down-regulates inducible nitric oxide synthase via the proteasome pathway in human colon carcinoma cells. Proc Natl Acad Sci U S A 97(26):14334–14339
Clementi E (1998) Role of nitric oxide and its intracellular signalling pathways in the control of Ca2+ homeostasis. Biochem Pharmacol 55(6):713–718
Clementi E, Borgese N, Meldolesi J (2003) Interactions between nitric oxide and sphingolipids and the potential consequences in physiology and pathology. Trends Pharmacol Sci 24(10):518–523
Nisoli E, Tonello C, Cardile A, Cozzi V, Bracale R, Tedesco L, Falcone S, Valerio A, Cantoni O, Clementi E, Moncada S, Carruba MO (2005) Calorie restriction promotes mitochondrial biogenesis by inducing the expression of eNOS. Science 310(5746):314–317
Nisoli E, Falcone S, Tonello C, Cozzi V, Palomba L, Fiorani M, Pisconti A, Brunelli S, Cardile A, Francolini M, Cantoni O, Carruba MO, Moncada S, Clementi E (2004) Mitochondrial biogenesis by NO yields functionally active mitochondria in mammals. Proc Natl Acad Sci U S A 101(47):16507–16512
Roberts CK, Barnard RJ, Scheck SH, Balon TW (1997) Exercise-stimulated glucose transport in skeletal muscle is nitric oxide dependent. Am J Physiol 273(1 Pt 1):E220–E225
Clementi E, Brown GC, Foxwell N, Moncada S (1999) On the mechanism by which vascular endothelial cells regulate their oxygen consumption. Proc Natl Acad Sci U S A 96(4):1559–1562
Clementi E, Nisoli E (2005) Nitric oxide and mitochondrial biogenesis: a key to long-term regulation of cellular metabolism. Comp Biochem Physiol A Mol Integr Physiol 142(2):102–110
Hagen T, Taylor CT, Lam F, Moncada S (2003) Redistribution of intracellular oxygen in hypoxia by nitric oxide: effect on HIF1alpha. Science 302(5652):1975–1978
Persichini T, Mazzone V, Polticelli F, Moreno S, Venturini G, Clementi E, Colasanti M (2005) Mitochondrial type I nitric oxide synthase physically interacts with cytochrome c oxidase. Neurosci Lett 384(3):254–259
Taylor CT, Moncada S (2010) Nitric oxide, cytochrome C oxidase, and the cellular response to hypoxia. Arterioscler Thromb Vasc Biol 30(4):643–647
Moncada S, Erusalimsky JD (2002) Does nitric oxide modulate mitochondrial energy generation and apoptosis? Nat Rev Mol Cell Biol 3(3):214–220
Brunori M (2001) Nitric oxide moves myoglobin centre stage. Trends Biochem Sci 26(4):209–210
Garry DJ, Bassel-Duby RS, Richardson JA, Grayson J, Neufer PD, Williams RS (1996) Postnatal development and plasticity of specialized muscle fiber characteristics in the hindlimb. Dev Genet 19(2):146–156
Grange RW, Meeson A, Chin E, Lau KS, Stull JT, Shelton JM, Williams RS, Garry DJ (2001) Functional and molecular adaptations in skeletal muscle of myoglobin-mutant mice. Am J Physiol Cell Physiol 281(5):C1487–C1494
Mannick JB, Hausladen A, Liu L, Hess DT, Zeng M, Miao QX, Kane LS, Gow AJ, Stamler JS (1999) Fas-induced caspase denitrosylation. Science 284(5414):651–654
Mannick JB, Schonhoff C, Papeta N, Ghafourifar P, Szibor M, Fang K, Gaston B (2001) S-Nitrosylation of mitochondrial caspases. J Cell Biol 154(6):1111–1116
Mikkelsen RB, Wardman P (2003) Biological chemistry of reactive oxygen and nitrogen and radiation-induced signal transduction mechanisms. Oncogene 22(37):5734–5754
Haendeler J, Hoffmann J, Tischler V, Berk BC, Zeiher AM, Dimmeler S (2002) Redox regulatory and anti-apoptotic functions of thioredoxin depend on S-nitrosylation at cysteine 69. Nat Cell Biol 4(10):743–749
Clementi E, Brown GC, Feelisch M, Moncada S (1998) Persistent inhibition of cell respiration by nitric oxide: crucial role of S-nitrosylation of mitochondrial complex I and protective action of glutathione. Proc Natl Acad Sci U S A 95(13):7631–7636
Reynaert NL, Ckless K, Korn SH, Vos N, Guala AS, Wouters EF, van der Vliet A, Janssen-Heininger YM (2004) Nitric oxide represses inhibitory kappaB kinase through S-nitrosylation. Proc Natl Acad Sci U S A 101(24):8945–8950
Schonhoff CM, Daou MC, Jones SN, Schiffer CA, Ross AH (2002) Nitric oxide-mediated inhibition of Hdm2-p53 binding. Biochemistry 41(46):13570–13574
Wolzt M, MacAllister RJ, Davis D, Feelisch M, Moncada S, Vallance P, Hobbs AJ (1999) Biochemical characterization of S-nitrosohemoglobin. Mechanisms underlying synthesis, no release, and biological activity. J Biol Chem 274(41):28983–28990
Colussi C, Mozzetta C, Gurtner A, Illi B, Rosati J, Straino S, Ragone G, Pescatori M, Zaccagnini G, Antonini A, Minetti G, Martelli F, Piaggio G, Gallinari P, Steinkulher C, Clementi E, Dell’aversana C, Altucci L, Mai A, Capogrossi MC, Puri PL, Gaetano C (2008) HDAC2 blockade by nitric oxide and histone deacetylase inhibitors reveals a common target in Duchenne muscular dystrophy treatment. Proc Natl Acad Sci U S A 105(49):19183–19187
Colussi C, Gurtner A, Rosati J, Illi B, Ragone G, Piaggio G, Moggio M, Lamperti C, D’Angelo G, Clementi E, Minetti G, Mozzetta C, Antonini A, Capogrossi MC, Puri PL, Gaetano C (2009) Nitric oxide deficiency determines global chromatin changes in Duchenne muscular dystrophy. FASEB J 23(7):2131–2141
Paylor B, Natarajan A, Zhang RH, Rossi F (2011) Nonmyogenic cells in skeletal muscle regeneration. Curr Top Dev Biol 96:139–165
Kuang S, Gillespie MA, Rudnicki MA (2008) Niche regulation of muscle satellite cell self-renewal and differentiation. Cell Stem Cell 2(1):22–31
Buckingham M, Bajard L, Daubas P, Esner M, Lagha M, Relaix F, Rocancourt D (2006) Myogenic progenitor cells in the mouse embryo are marked by the expression of Pax3/7 genes that regulate their survival and myogenic potential. Anat Embryol (Berl) 211(Suppl 1):51–56
Fukada S, Uezumi A, Ikemoto M, Masuda S, Segawa M, Tanimura N, Yamamoto H, Miyagoe-Suzuki Y, Takeda S (2007) Molecular signature of quiescent satellite cells in adult skeletal muscle. Stem Cells 25(10):2448–2459
Zammit PS (2008) All muscle satellite cells are equal, but are some more equal than others? J Cell Sci 121(Pt 18):2975–2982
Tedesco FS, Dellavalle A, Diaz-Manera J, Messina G, Cossu G (2010) Repairing skeletal muscle: regenerative potential of skeletal muscle stem cells. J Clin Invest 120(1):11–19
Relaix F, Marcelle C (2009) Muscle stem cells. Curr Opin Cell Biol 21(6):748–753
Zammit PS, Partridge TA, Yablonka-Reuveni Z (2006) The skeletal muscle satellite cell: the stem cell that came in from the cold. J Histochem Cytochem 54(11):1177–1191
Buckingham M (2007) Skeletal muscle progenitor cells and the role of Pax genes. C R Biol 330(6–7):530–533
Scime A, Rudnicki MA (2006) Anabolic potential and regulation of the skeletal muscle satellite cell populations. Curr Opin Clin Nutr Metab Care 9(3):214–219
Zammit PS, Relaix F, Nagata Y, Ruiz AP, Collins CA, Partridge TA, Beauchamp JR (2006) Pax7 and myogenic progression in skeletal muscle satellite cells. J Cell Sci 119(Pt 9):1824–1832
Collins CA, Olsen I, Zammit PS, Heslop L, Petrie A, Partridge TA, Morgan JE (2005) Stem cell function, self-renewal, and behavioral heterogeneity of cells from the adult muscle satellite cell niche. Cell 122(2):289–301
Perez-Ruiz A, Ono Y, Gnocchi VF, Zammit PS (2008) beta-Catenin promotes self-renewal of skeletal-muscle satellite cells. J Cell Sci 121(Pt 9):1373–1382
Le Grand F, Jones AE, Seale V, Scime A, Rudnicki MA (2009) Wnt7a activates the planar cell polarity pathway to drive the symmetric expansion of satellite stem cells. Cell Stem Cell 4(6):535–547
Brack AS, Conboy IM, Conboy MJ, Shen J, Rando TA (2008) A temporal switch from notch to Wnt signaling in muscle stem cells is necessary for normal adult myogenesis. Cell Stem Cell 2(1):50–59
Brack AS, Conboy MJ, Roy S, Lee M, Kuo CJ, Keller C, Rando TA (2007) Increased Wnt signaling during aging alters muscle stem cell fate and increases fibrosis. Science 317(5839):807–810
Ou CY, Kim JH, Yang CK, Stallcup MR (2009) Requirement of cell cycle and apoptosis regulator 1 for target gene activation by Wnt and beta-catenin and for anchorage-independent growth of human colon carcinoma cells. J Biol Chem 284(31):20629–20637
Otto A, Schmidt C, Luke G, Allen S, Valasek P, Muntoni F, Lawrence-Watt D, Patel K (2008) Canonical Wnt signalling induces satellite-cell proliferation during adult skeletal muscle regeneration. J Cell Sci 121(Pt 17):2939–2950
Seale P, Polesskaya A, Rudnicki MA (2003) Adult stem cell specification by Wnt signaling in muscle regeneration. Cell Cycle 2(5):418–419
Brack AS, Murphy-Seiler F, Hanifi J, Deka J, Eyckerman S, Keller C, Aguet M, Rando TA (2009) BCL9 is an essential component of canonical Wnt signaling that mediates the differentiation of myogenic progenitors during muscle regeneration. Dev Biol 335(1):93–105
Buono R, Vantaggiato C, Pisa V, Azzoni E, Bassi MT, Brunelli S, Sciorati C, Clementi E (2012) Nitric oxide sustains long-term skeletal muscle regeneration by regulating fate of satellite cells via signaling pathways requiring Vangl2 and Cyclic GMP. Stem Cells 30(2):197–209
Lincoln TM, Wu X, Sellak H, Dey N, Choi CS (2006) Regulation of vascular smooth muscle cell phenotype by cyclic GMP and cyclic GMP-dependent protein kinase. Front Biosci 11:356–367
Pilz RB, Broderick KE (2005) Role of cyclic GMP in gene regulation. Front Biosci 10:1239–1268
Sciorati C, Nistico G, Meldolesi J, Clementi E (1997) Nitric oxide effects on cell growth: GMP-dependent stimulation of the AP-1 transcription complex and cyclic GMP-independent slowing of cell cycling. Br J Pharmacol 122(4):687–697
Cossu G, Borello U (1999) Wnt signaling and the activation of myogenesis in mammals. EMBO J 18(24):6867–6872
Brunelli S, Relaix F, Baesso S, Buckingham M, Cossu G (2007) Beta catenin-independent activation of MyoD in presomitic mesoderm requires PKC and depends on Pax3 transcriptional activity. Dev Biol 304(2):604–614
Anderson JE (2000) A role for nitric oxide in muscle repair: nitric oxide-mediated activation of muscle satellite cells. Mol Biol Cell 11(5):1859–1874
Filippin LI, Cuevas MJ, Lima E, Marroni NP, Gonzalez-Gallego J, Xavier RM (2011) Nitric oxide regulates the repair of injured skeletal muscle. Nitric Oxide 24(1):43–49
Wozniak AC, Kong J, Bock E, Pilipowicz O, Anderson JE (2005) Signaling satellite-cell activation in skeletal muscle: markers, models, stretch, and potential alternate pathways. Muscle Nerve 31(3):283–300
Bach D, Pich S, Soriano FX, Vega N, Baumgartner B, Oriola J, Daugaard JR, Lloberas J, Camps M, Zierath JR, Rabasa-Lhoret R, Wallberg-Henriksson H, Laville M, Palacin M, Vidal H, Rivera F, Brand M, Zorzano A (2003) Mitofusin-2 determines mitochondrial network architecture and mitochondrial metabolism. A novel regulatory mechanism altered in obesity. J Biol Chem 278(19):17190–17197
De Palma C, Falcone S, Pisoni S, Cipolat S, Panzeri C, Pambianco S, Pisconti A, Allevi R, Bassi MT, Cossu G, Pozzan T, Moncada S, Scorrano L, Brunelli S, Clementi E (2010) Nitric oxide inhibition of Drp1-mediated mitochondrial fission is critical for myogenic differentiation. Cell Death Differ 17(11):1684–1696
Barsoum MJ, Yuan H, Gerencser AA, Liot G, Kushnareva Y, Graber S, Kovacs I, Lee WD, Waggoner J, Cui J, White AD, Bossy B, Martinou JC, Youle RJ, Lipton SA, Ellisman MH, Perkins GA, Bossy-Wetzel E (2006) Nitric oxide-induced mitochondrial fission is regulated by dynamin-related GTPases in neurons. EMBO J 25(16):3900–3911
Cho DH, Nakamura T, Fang J, Cieplak P, Godzik A, Gu Z, Lipton SA (2009) S-nitrosylation of Drp1 mediates beta-amyloid-related mitochondrial fission and neuronal injury. Science 324(5923):102–105
Moncada S, Bolanos JP (2006) Nitric oxide, cell bioenergetics and neurodegeneration. J Neurochem 97(6):1676–1689
Thippeswamy T, McKay JS, Quinn JP, Morris R (2006) Nitric oxide, a biological double-faced janus–is this good or bad? Histol Histopathol 21(4):445–458
Rambourg A, Segretain D (1980) Three-dimensional electron microscopy of mitochondria and endoplasmic reticulum in the red muscle fiber of the rat diaphragm. Anat Rec 197(1):33–48
Rando TA, Disatnik MH, Yu Y, Franco A (1998) Muscle cells from mdx mice have an increased susceptibility to oxidative stress. Neuromuscul Disord 8(1):14–21
Even PC, Decrouy A, Chinet A (1994) Defective regulation of energy metabolism in mdx-mouse skeletal muscles. Biochem J 304(Pt 2):649–654
Nardin RA, Johns DR (2001) Mitochondrial dysfunction and neuromuscular disease. Muscle Nerve 24(2):170–191
Kuznetsov AV, Winkler K, Wiedemann FR, von Bossanyi P, Dietzmann K, Kunz WS (1998) Impaired mitochondrial oxidative phosphorylation in skeletal muscle of the dystrophin-deficient mdx mouse. Mol Cell Biochem 183(1–2):87–96
Scholte HR, Luyt-Houwen IE, Busch HF, Jennekens FG (1985) Muscle mitochondria from patients with Duchenne muscular dystrophy have a normal beta oxidation, but an impaired oxidative phosphorylation. Neurology 35(9):1396–1397
Lee KH, Baek MY, Moon KY, Song WK, Chung CH, Ha DB, Kang MS (1994) Nitric oxide as a messenger molecule for myoblast fusion. J Biol Chem 269(20):14371–14374
Pisconti A, Brunelli S, Di Padova M, De Palma C, Deponti D, Baesso S, Sartorelli V, Cossu G, Clementi E (2006) Follistatin induction by nitric oxide through cyclic GMP: a tightly regulated signaling pathway that controls myoblast fusion. J Cell Biol 172(2):233–244
Iezzi S, Di Padova M, Serra C, Caretti G, Simone C, Maklan E, Minetti G, Zhao P, Hoffman EP, Puri PL, Sartorelli V (2004) Deacetylase inhibitors increase muscle cell size by promoting myoblast recruitment and fusion through induction of follistatin. Dev Cell 6(5):673–684
Fish JE, Matouk CC, Rachlis A, Lin S, Tai SC, D’Abreo C, Marsden PA (2005) The expression of endothelial nitric oxide synthase is controlled by a cell-specific histone code. J Biol Chem 280(26):24824–24838
Gan Y, Shen YH, Wang J, Wang X, Utama B, Wang XL (2005) Role of histone deacetylation in cell-specific expression of endothelial nitric-oxide synthase. J Biol Chem 280(16):16467–16475
Cacchiarelli D, Martone J, Girardi E, Cesana M, Incitti T, Morlando M, Nicoletti C, Santini T, Sthandier O, Barberi L, Auricchio A, Musaro A, Bozzoni I (2010) MicroRNAs involved in molecular circuitries relevant for the Duchenne muscular dystrophy pathogenesis are controlled by the dystrophin/nNOS pathway. Cell Metabol 12(4):341–351
Filippin LI, Cuevas MJ, Lima E, Marroni NP, Gonzalez-Gallego J, Xavier RM (2011) The role of nitric oxide during healing of trauma to the skeletal muscle. Inflamm Res 60(4):347–356
Villalta SA, Nguyen HX, Deng B, Gotoh T, Tidball JG (2009) Shifts in macrophage phenotypes and macrophage competition for arginine metabolism affect the severity of muscle pathology in muscular dystrophy. Hum Mol Genet 18(3):482–496
Li D, Shin JH, Duan D (2011) iNOS ablation does not improve specific force of the extensor digitorum longus muscle in dystrophin-deficient mdx4cv mice. PLoS One 6(6):e21618
Brenman JE, Chao DS, Xia H, Aldape K, Bredt DS (1995) Nitric oxide synthase complexed with dystrophin and absent from skeletal muscle sarcolemma in Duchenne muscular dystrophy. Cell 82(5):743–752
Crosbie RH, Barresi R, Campbell KP (2002) Loss of sarcolemma nNOS in sarcoglycan-deficient muscle. FASEB J 16(13):1786–1791
Finanger Hedderick EL, Simmers JL, Soleimani A, Andres-Mateos E, Marx R, Files DC, King L, Crawford TO, Corse AM, Cohn RD (2011) Loss of sarcolemmal nNOS is common in acquired and inherited neuromuscular disorders. Neurology 76(11):960–967
Suzuki N, Mizuno H, Warita H, Takeda S, Itoyama Y, Aoki M (2010) Neuronal NOS is dislocated during muscle atrophy in amyotrophic lateral sclerosis. J Neurol Sci 294(1–2):95–101
Wehling M, Spencer MJ, Tidball JG (2001) A nitric oxide synthase transgene ameliorates muscular dystrophy in mdx mice. J Cell Biol 155(1):123–131
Percival JM, Anderson KN, Gregorevic P, Chamberlain JS, Froehner SC (2008) Functional deficits in nNOSmu-deficient skeletal muscle: myopathy in nNOS knockout mice. PLoS One 3(10):e3387
Church JE, Gehrig SM, Chee A, Naim T, Trieu J, McConell GK, Lynch GS (2011) Early functional muscle regeneration after myotoxic injury in mice is unaffected by nNOS absence. Am J Physiol Regul Integr Comp Physiol 301(5):R1358–R1366
Bredt DS (1998) NO skeletal muscle derived relaxing factor in Duchenne muscular dystrophy. Proc Natl Acad Sci U S A 95(25):14592–14593
Thomas GD, Sander M, Lau KS, Huang PL, Stull JT, Victor RG (1998) Impaired metabolic modulation of alpha-adrenergic vasoconstriction in dystrophin-deficient skeletal muscle. Proc Natl Acad Sci U S A 95(25):15090–15095
Kobayashi YM, Rader EP, Crawford RW, Iyengar NK, Thedens DR, Faulkner JA, Parikh SV, Weiss RM, Chamberlain JS, Moore SA, Campbell KP (2008) Sarcolemma-localized nNOS is required to maintain activity after mild exercise. Nature 456(7221):511–515
Dubowitz V (2005) Prednisone for Duchenne muscular dystrophy. Lancet Neurol 4(5):264
Pichavant C, Aartsma-Rus A, Clemens PR, Davies KE, Dickson G, Takeda S, Wilton SD, Wolff JA, Wooddell CI, Xiao X, Tremblay JP (2011) Current status of pharmaceutical and genetic therapeutic approaches to treat DMD. Mol Ther 19(5):830–840
Goemans NM, Tulinius M, van den Akker JT, Burm BE, Ekhart PF, Heuvelmans N, Holling T, Janson AA, Platenburg GJ, Sipkens JA, Sitsen JM, Aartsma-Rus A, van Ommen GJ, Buyse G, Darin N, Verschuuren JJ, Campion GV, de Kimpe SJ, van Deutekom JC (2011) Systemic administration of PRO051 in Duchenne’s muscular dystrophy. New Engl J Med 364(16):1513–1522
Bowles DE, McPhee SW, Li C, Gray SJ, Samulski JJ, Camp AS, Li J, Wang B, Monahan PE, Rabinowitz JE, Grieger JC, Govindasamy L, Agbandje-McKenna M, Xiao X, Samulski RJ (2011) Phase 1 gene therapy for duchenne muscular dystrophy using a translational optimized AAV vector. Mol Ther 20(2):443–455
Cirak S, Feng L, Anthony K, Arechavala-Gomeza V, Torelli S, Sewry C, Morgan JE, Muntoni F (2012) Restoration of the dystrophin-associated glycoprotein complex after exon skipping therapy in Duchenne muscular dystrophy. Mol Ther 20(2):462–467
Stamler JS, Meissner G (2001) Physiology of nitric oxide in skeletal muscle. Physiol Rev 81(1):209–237
Wehling-Henricks M, Tidball JG (2011) Neuronal nitric oxide synthase-rescue of dystrophin/utrophin double knockout mice does not require nNOS localization to the cell membrane. PLoS One 6(10):e25071
Voisin V, Sebrie C, Matecki S, Yu H, Gillet B, Ramonatxo M, Israel M, De la Porte S (2005) L-arginine improves dystrophic phenotype in mdx mice. Neurobiol Dis 20(1):123–130
Wang G, Burczynski FJ, Hasinoff BB, Zhang K, Lu Q, Anderson JE (2009) Development of a nitric oxide-releasing analogue of the muscle relaxant guaifenesin for skeletal muscle satellite cell myogenesis. Mol Pharm 6(3):895–904
Barton ER, Morris L, Kawana M, Bish LT, Toursel T (2005) Systemic administration of L-arginine benefits mdx skeletal muscle function. Muscle Nerve 32(6):751–760
Hnia K, Gayraud J, Hugon G, Ramonatxo M, De La Porte S, Matecki S, Mornet D (2008) L-arginine decreases inflammation and modulates the nuclear factor-kappaB/matrix metalloproteinase cascade in mdx muscle fibers. Am J Pathol 172(6):1509–1519
Benabdellah F, Yu H, Brunelle A, Laprevote O, De La Porte S (2009) MALDI reveals membrane lipid profile reversion in MDX mice. Neurobiol Dis 36(2):252–258
Marques MJ, Luz MA, Minatel E, Neto HS (2005) Muscle regeneration in dystrophic mdx mice is enhanced by isosorbide dinitrate. Neurosci Lett 382(3):342–345
Feelisch M, Ostrowski J, Noack E (1989) On the mechanism of NO release from sydnonimines. J Cardiovasc Pharmacol 14(Suppl 11):S13–S22
Bailey SJ, Fulford J, Vanhatalo A, Winyard PG, Blackwell JR, DiMenna FJ, Wilkerson DP, Benjamin N, Jones AM (2010) Dietary nitrate supplementation enhances muscle contractile efficiency during knee-extensor exercise in humans. J Appl Physiol 109(1):135–148
Larsen FJ, Schiffer TA, Borniquel S, Sahlin K, Ekblom B, Lundberg JO, Weitzberg E (2011) Dietary inorganic nitrate improves mitochondrial efficiency in humans. Cell Metabol 13(2):149–159
Archer JD, Vargas CC, Anderson JE (2006) Persistent and improved functional gain in mdx dystrophic mice after treatment with L-arginine and deflazacort. FASEB J 20(6):738–740
Wallace JL, Viappiani S, Bolla M (2009) Cyclooxygenase-inhibiting nitric oxide donators for osteoarthritis. Trends Pharmacol Sci 30(3):112–117
Brunelli S, Sciorati C, D’Antona G, Innocenzi A, Covarello D, Galvez BG, Perrotta C, Monopoli A, Sanvito F, Bottinelli R, Ongini E, Cossu G, Clementi E (2007) Nitric oxide release combined with nonsteroidal antiinflammatory activity prevents muscular dystrophy pathology and enhances stem cell therapy. Proc Natl Acad Sci U S A 104(1):264–269
Sciorati C, Miglietta D, Buono R, Pisa V, Cattaneo D, Azzoni E, Brunelli S, Clementi E (2011) A dual acting compound releasing nitric oxide (NO) and ibuprofen, NCX 320, shows significant therapeutic effects in a mouse model of muscular dystrophy. Pharmacol Res 64:210–217
Sciorati C, Buono R, Azzoni E, Casati S, Ciuffreda P, D’Angelo G, Cattaneo D, Brunelli S, Clementi E (2010) Co-administration of ibuprofen and nitric oxide is an effective experimental therapy for muscular dystrophy, with immediate applicability to humans. Br J Pharmacol 160(6):1550–1560
Ziche M, Morbidelli L, Masini E, Amerini S, Granger HJ, Maggi CA, Geppetti P, Ledda F (1994) Nitric oxide mediates angiogenesis in vivo and endothelial cell growth and migration in vitro promoted by substance P. J Clin Invest 94(5):2036–2044
Schgoer W, Theurl M, Jeschke J, Beer AG, Albrecht K, Gander R, Rong S, Vasiljevic D, Egger M, Wolf AM, Frauscher S, Koller B, Tancevski I, Patsch JR, Schratzberger P, Piza-Katzer H, Ritsch A, Bahlmann FH, Fischer-Colbrie R, Wolf D, Kirchmair R (2009) Gene therapy with the angiogenic cytokine secretoneurin induces therapeutic angiogenesis by a nitric oxide-dependent mechanism. Circ Res 105(10):994–1002
Sciorati C, Galvez BG, Brunelli S, Tagliafico E, Ferrari S, Cossu G, Clementi E (2006) Ex vivo treatment with nitric oxide increases mesoangioblast therapeutic efficacy in muscular dystrophy. J Cell Sci 119(Pt 24):5114–5123
D’Angelo MG, Gandossini S, Boneschi FM, Sciorati C, Bonato S, Brighina E, Comi GP, Turconi AC, Magri F, Stefanoni G, Brunelli S, Bresolin N, Cattaneo D, Clementi E (2012) Nitric oxide donor and non steroidal anti inflammatory drugs as a therapy for muscular dystrophies: evidence from a safety study with pilot efficacy measures in adult dystrophic patients. Pharmacol Res 65:472–479
Acknowledgments
The original work described in this review was supported by the European Community’s framework programme FP7/2007-2013 under grant agreement nos. 241440 (ENDOSTEM) and 223098 (OPTISTEM), Telethon (GGP07006), the Italian Ministry of Health Ricerca Corrente 2012, the Associazione Italiana Ricerca sul Cancro (AIRC-11365) and the Parent Project Italia Onlus.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
De Palma, C., Clementi, E. Nitric Oxide in Myogenesis and Therapeutic Muscle Repair. Mol Neurobiol 46, 682–692 (2012). https://doi.org/10.1007/s12035-012-8311-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-012-8311-8