Abstract
Chemoresistance is the leading cause of limiting long-term treatment success in cancer cells. Anticancer drugs usually kill cells through apoptosis induction and defects in this signaling pathway lead to chemoresistance. Apoptotic protease activating factor 1 regulates cellular stress evoked by chemotherapeutic agents through facilitating apoptosome assembling but can be degraded by proteasome. This study examined the role of proteasome inhibitor Bortezomib in the cytotoxic effects of Docetaxel on MCF7 cells response and its correlation with Apaf-1 expression level. MTT assay, caspase 3/7 activity assay, propidium iodide staining, adenosine triphosphate and reactive oxygen species amount measurements were utilized to demonstrate the role of Bortezomib in Docetaxel efficacy with and without Apaf-1 overexpressing. Meanwhile, two-dimensional cell migration assay was performed by scratch wound assay. The combination of Docetaxel with Bortezomib was significantly more cytotoxic compared single drug, more effectively delayed cell growth, reduced ATP level and increased ROS production. In Apaf-1 overexpressing, Docetaxel was more efficient in preventing cell migration, however, Docetaxel plus Bortezomib were not significantly effective; and fluorescence images supported the interpretation. Our findings demonstrated MCF7 resistance to Docetaxel is due in part to low Apaf-1 level and Apaf-1 overexpression resulted in the increase of cell susceptibility to Docetaxel stimulus. We assume that proteasome inhibitor may restore apoptotic proteins like Apaf-1 and prevent the degradation of cytosolic cytochrome c released by Docetaxel, consequently triggering intrinsic apoptosis and promoting cancer cell death. Collectively, treating MCF7 breast cells with proteasome inhibitor sensitizes cells to Docetaxel-induced apoptosis and possibly overcomes chemoresistance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Apoptosis pathway is an essential event in the regulation of a variety of cellular processes [1, 2]. Intrinsic apoptosis is initiated by cytochrome c release from mitochondria into cytosol after apoptotic stimuli [3]. Cytochrome c forms a cytosolic complex with apoptotic protease activating factor 1 (Apaf-1) in the presence of dATP or ATP, termed apoptosome. The apoptosome complex binds with procaspase 9 and triggers signaling cascade of caspase family. Procaspase 9 is cleaved into active form, resulting in the activation of caspase 3/7 [3,4,5].
Apoptosis dysregulation leads to pathological conditions and undesirable cell responses. Disturbance of apoptotic machinery is implicated in many diseases, especially cancer [6], and failure to activate the apoptotic signaling can result in resistance to the anticancer drugs [7, 8].
Resistance to chemodrugs is one of the most important features of cancer cells [9]. Cancer chemoresistance is causally associated with apoptotic resistance and contributes to tumor recurrence and cell migration [6, 10]. In general, the development of most anticancer drugs relies on inducing apoptosis cascade [7], whereas the identification of inhibitors of apoptosis and properly induced apoptosis might be more useful in controlling cell responses. In most of cytotoxic anticancer drugs, cytochrome c appears to be released and apoptosome complex formed.
The ubiquitin proteasome is a significant pathway in the regulation of cellular function dealing with the survival and cell death. Generally it has been established that as a cell-protective mechanism, inhibition of proteasome activity plays an important role in apoptosis induction [11, 12]. Proteasome degradative enzyme complex is involved in the catabolism of about 70–90% of cellular proteins [13], therefore many cellular events are regulated by the proteasome as directly or indirectly. Substances that inhibit the proteasome activity can act as anticancer drugs. Bortezomib is the first approved proteasome inhibitor used in clinical for a variety of solid tumors [13,14,15] and acts by inhibiting the 26S proteasome [15, 16].
Taxanes like Docetaxel and Paclitaxel are widely used in treating breast cancer patients [17]. Docetaxel (Dtx) functions through disrupting the microtubular network of cells [18]. MCF7 as a well-known model of breast cancer cell line is extensively used to examine cytotoxic drugs in vitro. The current study aimed to investigate the cytotoxic effects of Dtx and to correlate with the proteasome inhibitor Bortezomib (Bor) and the expression level of Apaf-1 on cell apoptotic rate and cell migration in MCF7.
Material and methods
Cell line, plasmids and drugs
Human breast cancer cell line MCF7 from ATCC was cultured in DMEM supplemented with 10% FBS and 100 units/ml penicillin/streptomycin antibiotics. Plasmid pcDNA3.1 from Invitrogen and pcDNA3.1/Apaf-1 generated by our team previously were extracted by Qiagen plasmid extraction kit. Dtx was obtained from Sigma and Bor (Velcade) purchased from Janssen-Cilag and the desired concentrations prepared.
Cell transfection and drug treatment
Plasmid pcDNA3.1/Apaf-1 was transient transfected into MCF7 cells using polyethylenimine (PEI, 25 KD) in serum-free medium. After 3–4 h, medium was exchanged with fresh 10% FBS media. Western blotting was utilized to confirm the expression level of Apaf-1 with transfection [19, 20]. About 24 h after transfection, cell treatment by fresh medium containing drug was performed. In drug combination, following 2 h treatment with Bor (5 nM), Dtx (100 nM) was added.
Cell viability and proliferation assay
Cell viability was measured based on colorimetric MTT assay [21]. Briefly, growth media was removed from the cells plated in 96-well 24 h after treatment, next 5 mg/ml of 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) was added and incubated for 4 h. Then supernatant was removed and dissolved by DMSO and absorbance measured at 570 nm. Proliferation assay was also carried out by trypan blue. Cell suspension of treated cells was mixed with equal volume of trypan blue solution, incubated for 5 min and then the ratio of number of viable cells to total cells was calculated.
ATP assay
Following treatment, cells were washed with PBS and lysed in hypotonic lysis buffer containing 20 mM HEPES, 10 mM KCl, 1.5 mM MgCl2, 1 mM EDTA, 1 mM DTT, 0.1 mM PMSF, and 1 mM Sucrose, pH 7.6 [19, 22]. Following centrifugation, same protein concentration of supernatants as cytosolic extract were used for ATP assay by the firefly luciferase assay, then normalized based on ATP standard curve [19, 23].
ROS amount measurement
Cells were incubated in presence or absence of drug for the desired times. Changes in the intracellular levels of reactive oxygen species (ROS) were measured using 2′-7′-dichloro-dihydro-fluorescein diacetate (DCF-DA). Cells were rinsed with PBS and incubated in 5 μmol/l of DCF-DA for 30 min, excited at 480 nm and emission evaluated at 530 nm, as reported previously [19, 23].
Caspase 3/7 activity assay
At 24 h post-treatment, cytosolic extracts were prepared by hypotonic lysis buffer. Three wells in each treatment group were mixed, cell extract was centrifuged and protein concentration estimated using Bradford method [24]. Equal protein concentration was incubated with the luminescent-based Caspase-Glo 3/7 reagent (Promega) on ice and activity measured with a luminometer (Berthold) based on light production as relative light unit (RLU) per second (RLU/Sec) [19, 23].
Cell survival assay by PI staining
Assays employing propidium iodide (PI, Sigma) were done as follows: cells were seeded in 24-well plates, treated with drug for 24 h, attached cells rinsed with PBS and then stained with PI solution (1 μg/ml) for 5 min. Following washing, fluorescence imaging was done at excitation 535 and emission 620 nm wavelengths by fluorescence microscopy [23].
Scratching assay analysis
At 24 h post-transfection, cells were scratched and after about 2 h, treatment with drug performed. At the desired times, cells were photographed and the cells motility monitored. The distance of each scratch closure was assessed by images analysis by Image J and calculated as percent cell invasion of 0 h [23, 25].
Statistical considerations
All graphs represent mean and independent data from three independent experiments. All statistical assessments were obtained by a student’s t test. P values < 0.05 were considered significant.
Results
Bor enhances Dtx-induced cell death level in MCF7 cells
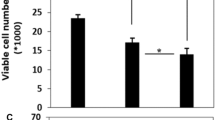
Blocking proteasome activity by inhibitors results in the death of different cells [13, 26, 27]. The mode of cell death induced by anticancer drug Dtx was investigated here in MCF7 cell line alone and in combination of proteasome inhibitor Bor. The primary step was to establish the cell viability and cell proliferation of Bor and Dtx treatment alone in MCF7 cells. The secondary step was to assess MCF7 cells response rate to Dtx in combination with Bor; evaluate cell viability using MTT analysis and cell proliferation by trypan blue assay. These results indicated the potency of each agents in cell death induction. However, as shown in Fig. 1a, b, MCF7 cells were appeared to be more sensitive to dual treatment of the proteasome inhibitor Bor plus Dtx.
Effects of Dtx and Bor alone and combined on cell viability and proliferation, and in vitro assay of Dtx with and without Bor on intracellular ROS and ATP levels of MCF7 cell line. a Cell viability effects of Dtx or/and Bor were determined by MTT assay. b Anti-proliferative impacts were measured by trypan blue assay. c The level of intracellular ATP was measured in cells treated with Dtx or/and Bor for 24 h. d Intracellular ROS amounts of cells were determined by DCF-DA after treatment. Data are representative results from three independent experiments as means ± S, (*P < 0.05; **P < 0.01; ***P < 0.001 compared to 0 as the control)
Bor accelerates ROS generation and ATP depletion in apoptosis induced by Dtx
The level of intracellular ATP indicates the cell viability and cell death. Depletion of cellular ATP results in apoptotic cell death [28]. Moreover, cell death stimuli lead to the loss of cell membrane integrity, enhance mitochondrial membrane permeability and increase ROS production [29]. To further determine the role of proteasome inhibition in chemo drug Dtx-induced cell death, intracellular ATP and ROS levels were evaluated. The total ATP level in MCF7 cells undergoing apoptosis was measured by a luciferin-luciferase assay following lysis of the cells, and the level of ROS determined using cell permeable DCF-DA in intact cells [19, 23]. As demonstrated in Fig. 1c and d, the inhibition of proteasome with Dtx treatment caused a decrease in the level of ATP, as well as an increase in ROS content.
Bor plus Dtx promotes caspase 3/7 activation in MCF7 cells
In apoptosis pathways, various caspases are implicated in the initiation or execution process. Caspase 3/7 is necessary factor for stimuli-induced apoptotic cell death [5]. To further evaluate the apoptosis induced by proteasome inhibition by Bor and cytotoxic drug Dtx, caspase 3/7 activity was measured. The results showed that the pretreatment of MCF7 cells with Bor caused elevated caspase 3/7 activity of Dtx (Fig. 2a).
Effect on the caspase 3/7 activity of the MCF7 cells after 24 h of treatment with Dtx or/and Bor alone and combined with Apaf-1 overexpression. a The activation of caspase 3/7 was evaluated upon Dtx or/and Bor treatment in MCF7 cells. b Caspase 3/7 activity of MCF7 cells was determined after Apaf-1 transfection and Dtx treatment with and without Bor. Data are representative results from three independent experiments as means ± S, (*P < 0.05; **P < 0.01; ***P < 0.001 compared to 0 as the control)
Dtx-induced cell death increases in Apaf-1 transfected MCF7 cells
Low efficacy of chemodrugs is often correlated with dysregulation of apoptotic pathways, and overexpression of apoptotic effectors might enhance drug sensitivity [7]. To investigate the effects of proteasome inhibitor and expression levels of each apoptotic factor on cytotoxic drug efficacy, Apaf-1 overexpression with Bor were examined in apoptosis induction rate by Dtx. At first, to confirm the expression levels of exogenous Apaf-1 in cells, western blot analysis was performed (data not shown). Next, the caspase 3/7 activity in pcDNA transfected and pcDNA/Apaf-1 transfected MCF7 cells was checked. As displayed in Fig. 2b, Apaf-1 transfected MCF7 cells contained significant levels of the active caspase 3/7 in each drugs alone and combined. Taken together, these results indicate that more caspase 3/7 activity was stimulated in Apaf-1 transfected MCF7 cells thereby indicating that apoptosome level and apoptotic rate enhanced by addition of exogenous Apaf-1.
Apaf-1 overexpressing with Bor potentiates apoptotic DNA-fragmentation proceed by Dtx
To compare the cellular characteristics of Dtx-induced cell death, with or without Apaf-1 expression and/or proteasome inhibitor, PI staining was used to assess the nuclear morphology of MCF7 cells. As would be expected, fluorescence images showed that both Apaf-1 transfected and control MCF7 cells exhibited relatively strong red fluorescence signals after treatment with Dtx; negligible staining was also observed in untreated cells (Fig. 3). However, it was found that there were notable differences in damaged cell membranes in Apaf-1 expression with Dtx/Bor compared to Dtx alone without Apaf-1.
Bor enhances Dtx-effect on cell migration inhibition but not significant in Apaf-1 overexpressing cells
The common method for assessing 2D cell migration is to use scratch wound assay for measuring cells ability to movement in response to external signals [30, 31]. To evaluate the involvement of proteasome inhibition and Apaf-1 levels in Dtx-induced apoptosis, scratching assay was carried out. In a first set of experiments, Dtx and Bor alone were examined in MCF7 cells migration as represented in Fig. 4a. Then, cells were treated with Dtx in combination with Bor. Dtx/Bor exhibited synergistic effect on inhibition of migration. In the second test, to further determine the role of Apaf-1 with cytotoxic drugs on cell motility, the effect of exogenous Apaf-1 on the cell migration in the presence of Dtx/Bor was investigated. The findings demonstrated Dtx treatment in Apaf-1 transfected cells was more effective in preventing of migration, however, Bor/Dtx treatments did not significantly affect MCF7 cell migration (Fig. 4b).
Effect of Dtx treatment alone or combined Bor on the cell migration of Apaf-1 transfected MCF7 cells and untransfected control. a Migration was estimated using comparing cell-covered regions at 30 and 60 h afterwards of scratching and drug treatment. b Apaf-1 transfected MCF7 cells response to Dtx or/and Bor were measured using scratching analysis at given time points according to image analysis using Image J. Data are representative results from three independent experiments as means ± S, (*P < 0.05; **P < 0.01; ***P < 0.001 compared to 0 as the control, and ns means non-significant)
Discussion
A basic factor limiting long-term treatment success in cancer therapy is chemoresistance. Combining cytotoxic drugs with unique mechanism of action may improve potential efficacy and overcome drug resistance. Inhibition of the catalytic core of 26S proteasome has emerged as an anti-neoplastic strategy. Bor as boronate-based dipeptide proteasome inhibitor targets the chymotrypsin-like activity of proteasome complex [15, 32]. Disrupting the ubiquitin–proteasome proteolytic system can affect tumor cell homeostasis through multiple mechanisms, hence is an attractive target for cancer cell sensitization to chemotherapeutic drugs [12, 16, 33]. Dtx is one of the most extensively used cytotoxic drugs in treating breast cancer [17]. There is no evidence of a drug interaction between Dtx and Bor [34].
In the present study, some experiments were designed to investigate the lethal effects of anticancer drug Dtx and proteasome inhibitor Bor on the human breast cancer MCF7 cells as alone and in combination with each other. The first study examined the effect of Dtx and Bor on the viability of MCF7 cells to determine the effect of each drugs. As indicated in Fig. 1a, Dtx and Bor alone induced apoptosis in MCF7 cells and viability was decreased. Following, combined Dtx/Bor treatment demonstrated a degree of apoptosis that was only achievable at much higher doses of either drug alone. Likewise, it was observed synergistic growth inhibition induced by Dtx/Bor in MCF7 cell line (Fig. 1b).
Apoptosis signaling is an energy-dependent process and cytotoxic drugs-triggered apoptotic cell death accompanied with ATP depletion [19, 28, 35]. Furthermore, apoptotic cell death can lead to mitochondrial damage and accumulation of reactive oxygen species [23, 29, 36]. To reflect cell death levels in chemodrug Dtx with and without proteasome inhibition, the treated MCF7 cells were analyzed by ATP assay and ROS measurements. These findings showed that Dtx or Bor-induced apoptosis was associated with reduction of ATP content (Fig. 1c) and increased ROS production (Fig. 1d). These results indicated that, as compared with either drug alone, the combination of Dtx and Bor showed an enhanced lethal effect on cells by lower ATP and higher ROS levels.
Caspases are the essential proteins that induce biochemical changes through apoptotic pathways, and caspase 3/7 is major factor involved in the apoptosis [37]. MCF7 cells are caspase 3 deficient but apoptosis induction is possible via activation of caspase 7 and/or 6 that are expressed [38, 39]. Actually, MCF7 cells act through sequential activation of caspases 9 and 7 or 6 [40]. Hence in the next section, the specific substrate of caspase 3/7 was used to detect whether this cysteine protease was involved in the cell death induced by the treatment of Dtx and/or Bor. The results indicated that caspase 3/7 was involved in the apoptosis of the MCF7 cells by Dtx and/or Bor (Fig. 2a), suggesting that the treatment of Dtx and/or Bor induced apoptosis through the intrinsic pathway. According to these results, while Dtx activated caspase 3/7, its combination with Bor enhance caspase 3/7 activity even more.
Furthermore, the overall effective cell killing by cytotoxic drugs and proteasome inhibition may correlate with the level of apoptosome formation, and overexpression of apoptosome component like Apaf-1 may enhance chemosensitivity. Apoptosome level has important biological significance in the progression of tumor treatment, and numerous chemotherapy cytotoxic drugs exert an antitumor effect by inducing the apoptosome formation. So, transfection of apoptotic component Apaf-1 was performed and the impact of relative expression of Apaf-1 on drug sensitivity and cell response measured, which allowed to compare efficiently both low and high level of Apaf-1 in drug efficacy. Western blotting revealed that MCF7 contained relatively low endogenous amount of Apaf-1, while this level significantly altered by transfection of pcDNA/Apaf-1 (data not shown). Caspase 3/7 activity assay was also carried out with same approach and the results clearly showed the association of the Apaf-1 expression levels with the response to induction treatment. As demonstrated in Fig. 2b, our data displayed synergistic effect of Apaf-1 overexpressing and Dtx and/or Bor on MCF7 cells and transfected cells with proteasome inhibition showed higher response to Dtx.
Assessing cell membrane integrity is one of the most widely used approaches to viability assessment. As already mentioned above, the drug resistance of MCF7 cells is probably due to a decrease at the apoptosome levels and an increase in cell viability. To investigate the effect of Apaf-1 levels on the cell function after Dtx and Bor treatment alone and also combined, PI imaging as an indicator dye for dead cells was evaluated. PI is used as a DNA stain to evaluate cell viability and to visualize the nucleus, as PI was believed to only stain cells with irreparably damaged membranes that can be described as nonviable cells. PI staining data were interestingly showed that, Apaf-1-transfected MCF7 cells were more sensitive to cytotoxic drug Dtx as compared with pcDNA-transfected control (Fig. 3). Moreover, the fluorescent images demonstrated that after Apaf-1 expression, inducing death of cells by Dtx/Bor occurred a little more intense. This indicated that the treatment of Dtx with high Apaf-1 level like Dtx/Bor synergistically improved the rate of cell death.
It is noteworthy that, Dtx or Bor treatment showed that either of the drug alone have the inhibitory effect on MCF7 cells migration. Furthermore, Dtx in combination with Bor was more effective than each drug alone on cell migration. Indeed, the combinatorial use of proteasome inhibitor Bor with Dtx was improved drug efficiency and prevented or delayed cell motility (Fig. 4a). More importantly, when compared to drug treatment, Apaf-1 overexpression combined Dtx treatment was significantly more effective in preventing of the cells migration. As can be seen in Fig. 4b, Apaf-1 expression in combination with Dtx treatment was strongly decreased the migration of cells. However, Apaf-1 expression with combined Dtx/Bor treatments did not significantly affect the level of cell motility than the Apaf-1 with Dtx alone. It seems that in Apaf-1 overexpression mode, this key apoptotic protein not only sensitized cells to Dtx-induced apoptosis, but also significantly increased background apoptosis (Fig. 3b) and decreased cell migration (Fig. 4b) in the transfected MCF7 cells.
Cytosolic cytochrome c attached to Apaf-1 cannot degrade, while cytochrome c that is unable to bind Apaf-1 is targeted for ubiquitination and degradation by proteasome [41, 42]. According to the information obtained from this study, we propose that the proteasome inhibition via Bor resulting in accumulation of cytosolic cytochrome c released by Dtx, which in turn leads to apoptosome formation. The enhanced susceptibility of Apaf-1 overexpressing cells can be explained by the findings that Apaf-1 adaptor molecule is involved in cytochrome c absorption thereby multiplying the impact of a drug death stimulus. Our findings suggest that increase expression of Apaf-1 may be prevent the ubiquitination and degradation of cytosolic cytochrome c, without proteasome inhibition, and Dtx stimulus cytochrome c release is sufficient to induce apoptosis.
References
Kerr F, Wyllie AH, Currie AR. Apoptosis: a basic biological phenomenon with wide-ranging implications in tissue kinetics. Br J Cancer. 1972;26:239–57. https://doi.org/10.1038/bjc.1972.33.
Yuan J, Yankner BA. Apoptosis in the nervous system. Nature. 2000;407:802–9. https://doi.org/10.1046/j.1471-4159.2000.0740001.x.
Brenner D, Mak TW. Mitochondrial cell death effectors. Curr Opin Cell Biol. 2009;21:871–7. https://doi.org/10.1016/j.ceb.2009.09.004.
Li P, Nijhawan D, Budihardjo I, et al. Cytochrome c and dATP-dependent formation of Apaf-1/caspase-9 complex initiates an apoptotic protease cascade. Cell. 1997;91:479–89. https://doi.org/10.1016/s0092-8674(00)80434-1.
Zou H, Henzel WJ, Liu X, Lutschg A, Wang X. Apaf-1, a human protein homologous to C. elegans CED-4, participates in cytochrome c-dependent activation of caspase-3. Cell. 1997;90:405–13. https://doi.org/10.1016/s0092-8674(00)80501-2.
Green DR, Kroemer G. Pharmacological manipulation of cell death: clinical applications in sight? J Clin Invest. 2005;15:2610–7. https://doi.org/10.1172/JCI26321.
Fox F, MacFarlane M. Targeting cell death signalling in cancer: minimising ‘Collateral damage.’ Br J Cancer. 2016;115:5–11. https://doi.org/10.1038/bjc.2016.111.Epub2016May3.
Jia L, Macey MG, Yin Y, Newland AC, Kelsey SM. Subcellular distribution and redistribution of Bcl-2 family proteins in human leukemia cells undergoing apoptosis. Blood. 1999;93:2353–9.
El-Khattouti A, Selimovic D, Haikel Y, Hassan M. Crosstalk between apoptosis and autophagy: molecular mechanisms and therapeutic strategies in cancer. J Cell Death. 2013;6:37–55. https://doi.org/10.4137/JCD.S11034.
Long JS, Ryan KM. New frontiers in promoting tumor cell death: targeting apoptosis, necroptosis and autophagy. Oncogene. 2012;31:5045–60. https://doi.org/10.1038/onc.2012.7.Epub2012Feb6.
Zhang HG, Wang J, Yang X, Hsu HC, Mountz JD. Regulation of apoptosis proteins in cancer cells by ubiquitin. Oncogene. 2004;23:2009–15. https://doi.org/10.1038/sj.onc.1207373.
Frankland-Searby S, Bhaumik SR. The 26S proteasome complex: an attractive target for cancer therapy. Biochem Biophys Acta. 2012;1825:64–76. https://doi.org/10.1016/j.bbcan.2011.10.003.
Rock KL, Gramm C, Rothstein L, Clark K, Stein R, Dick L, Hwang D, Goldberg AL. Inhibitors of the proteasome block the degradation of most cell proteins and the generation of peptides presented on MHC class I molecules. Cell. 1994;78:761. https://doi.org/10.1016/S0092-8674(94)90462-6.
Kisselev AF, Goldberg AL. Proteasome inhibitors: from research tools to drug candidates. Chem Biol. 2001;8:739–58. https://doi.org/10.1016/S1074-5521(01)00056-4.
Adams J, Kauffman M. Development of the proteasome inhibitor Velcade (Bortezomib). Cancer Invest. 2004;22:304–11. https://doi.org/10.1081/cnv-120030218.
Shah SA, Potter MW, McDade TP, Ricciardi R, Perugini RA, Elliott PJ, Adams J, Callery MP. 26S proteasome inhibition induces apoptosis and limits growth of human pancreatic cancer. J Cell Biochem. 2001;82:110–22. https://doi.org/10.1002/jcb.1150.
Jones SE, Erban J, Overmoyer B, et al. Randomized phase III study of docetaxel compared with paclitaxel in metastatic breast cancer. J Clin Oncol. 2005;23:5542–51. https://doi.org/10.1200/JCO.2005.02.027.
Eisenhauer EA, Vermorken JB. The toxoids. Comparative clinical pharmacology and therapeutic potential. Drugs. 1998;55:5–30. https://doi.org/10.2165/00003495-199855010-00002.
Karimzadeh S, Hosseinkhani S, Fathi A, Ataei F, Baharvand H. Insufficient Apaf-1 expression in early stages of neural differentiation of human embryonic stem cells might protect them from apoptosis. Eur J Cell Biol. 2018;97:126–35. https://doi.org/10.1016/J.EJCB.2018.01.005.
Amroudie MN, Ataei F. Experimental and theoretical study of IBC domain from human IP3R2; molecular cloning, bacterial expression and protein purification. Int J Biol Macromol. 2019;124:1321–7. https://doi.org/10.1016/j.ijbiomac.2018.09.117.
Ataei F, Torkzadeh-Mahani M, Hosseinkhani S. A novel luminescent biosensor for rapid monitoring of IP3 by split-luciferase complementary assay. Biosen Bioelectron. 2013;41:642–8. https://doi.org/10.1016/J.BIOS.2012.09.037.
Abazari R, Mahjoub AR, Ataei F, Morsali A, Carpenter-Warren CL, Mehdizadeh K, Slawin AMZ. Chitosan immobilization on Bio-MOF nanostructures: a biocompatible pH-responsive nanocarrier for doxorubicin release on MCF-7 cell lines of human breast cancer. Inorg Chem. 2018;57:13364–79. https://doi.org/10.1021/acs.inorgchem.8b01955.
Mehdizadeh K, Ataei F, Hosseinkhani S. Effects of doxorubicin and docetaxel on susceptibility to apoptosis in high expression level of survivin in HEK and HEK-S cell lines as in vitro models. Biochem Biophys Res Commun. 2020;532:139–44. https://doi.org/10.1016/j.bbrc.2020.08.028.
Bradford MM. A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem. 1976;72:248–54. https://doi.org/10.1006/abio.1976.9999.
Pakravan K, Babashah S, Mowla SJ, Mossahebi-Mohammad M, Ataei F, Dana N, Javan M. MicroRNA-100 shuttled by mesenchymal stem cell-derived exosomes suppresses in vitro angiogenesis through modulating the mTOR/HIF-1α/VEGF signaling axis in breast cancer cells. Cell Oncol. 2017;40:457–70. https://doi.org/10.1007/s13402-017-0335-7.
Wang X, Luo H, Chen H, Duguid W, Wu J. Role of proteasomes in T cell activation and proliferation. J Immunol. 1998;160:788–801.
Marshansky V, Wang X, Bertrand R, Luo H, Duguid W, Chinnadurai G, Kanaan N, Diem VM, Wu J. Proteasomes modulate balance among proapoptotic and antiapoptotic Bcl-2 family members and compromise functioning of the electron transport chain in leukemic cells. J Immunol. 2001;166:3130–42. https://doi.org/10.4049/jimmunol.166.5.3130.
Zamaraeva MV, Sabirov RZ, Maeno E, Ando-Akatsuka Y, Bessonova SV, Okada Y. Cells die with increased cytosolic ATP during apoptosis: a bioluminescence study with intracellular luciferase. Cell Death Differ. 2005;12:1390–7. https://doi.org/10.1038/sj.cdd.4401661.
Le Bras M, Clément MV, Pervaiz S, Brenner C. Reactive oxygen species and the mitochondrial signaling pathway of cell death. Histol Histopathol. 2005;20:205–19. https://doi.org/10.14670/HH-20.205.
Liang CC, Park AY, Guan JL. In vitro scratch assay: a convenient and inexpensive method for analysis of cell migration in vitro. Nat Protoc. 2007;2:329–33. https://doi.org/10.1038/nprot.2007.30.
Houshdarpour R, Ataei F, Hosseinkhani S. Efficient stable cell line generation of survivin as an in vitro model for specific functional analysis in apoptosis and drug screening. Mol Biotechnol. 2021. https://doi.org/10.1007/s12033-021-00313-y.
Richardson PG, Barlogie B, Berenson J, et al. A phase 2 study of bortezomib in relapsed, refractory myeloma. N Engl J Med. 2003;348:2609–17. https://doi.org/10.1056/NEJMoa030288.
Adams J, Palombella VJ, Elliott PJ. Proteasome inhibition: a new strategy in cancer treatment. Invest New Drugs. 2000;18:109–21. https://doi.org/10.1023/a:1006321828515.
Messersmith WA, Baker SD, Lassiter L, Sullivan RA, Dinh K, Almuete VI, Wright JJ, Donehower RC, Carducci MA, Armstrong DK. Phase I trial of bortezomib in combination with docetaxel in patients with advanced solid tumors. Clin Cancer Res. 2006;12:1270–5. https://doi.org/10.1158/1078-0432.CCR-05-1942.
Tsujimoto Y. Apoptosis and necrosis: intracellular ATP level as a determinant for cell death modes. Cell Death Differ. 2007;4:429–34. https://doi.org/10.1038/sj.cdd.4400262.
Panieri E, Santoro MM. ROS homeostasis and metabolism: a dangerous liason in cancer cells. Cell Death Dis. 2016;9:e2253. https://doi.org/10.1038/cddis.2016.105.
Brentnall M, Rodriguez-Menocal L, De Guevara RL, Cepero E, Boise LH. Caspase-9, caspase-3 and caspase-7 have distinct roles during intrinsic apoptosis. BMC Cell Biol. 2013;9:32. https://doi.org/10.1186/1471-2121-14-32.
Essmann F, Engels IH, Totzke G, Schulze-Osthoff K, Janicke RU. Apoptosis resistance of MCF-7 breast carcinoma cells to ionizing radiation is independent of p53 and cell cycle control but caused by the lack of caspase-3 and a caffeine-inhibitable event. Cancer Res. 2004;64:7065–72. https://doi.org/10.1158/0008-5472.CAN-04-1082.
Janick RU. MCF-7 breast cancer cells do not express caspase-3. Breast Cancer Res Treat. 2009;117:219–21. https://doi.org/10.1007/s10549-008-0217-9.
Liang Y, Yan C, Schor NF. Apoptosis the in the absence of caspase 3. Oncogene. 2001;20:6570–8. https://doi.org/10.1038/sj.onc.1204815.
Anichini A, Mortarini R, Sensi M, Zanon M. APAF-1 signaling in human melanoma. Cancer Lett. 2006;238:168–79. https://doi.org/10.1016/j.canlet.2005.06.034.
Gama V, et al. PARC/CUL9 mediates the degradation of mitochondrial-released cytochrome c and promotes survival in neurons and cancer cells. Sci Signal. 2014;7:ra67. https://doi.org/10.1126/scisignal.2005309.
Acknowledgements
We would like to thank the research council of Tarbiat Modares University through a grant (#D/2003) to cell death and differentiation research program, and Iranian National Science Foundation (INSF, project 93043373) for the financial support of this investigation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest to disclose.
Informed consent
All authors agree to submit this article for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mehdizadeh, K., Ataei, F. & Hosseinkhani, S. Treating MCF7 breast cancer cell with proteasome inhibitor Bortezomib restores apoptotic factors and sensitizes cell to Docetaxel. Med Oncol 38, 64 (2021). https://doi.org/10.1007/s12032-021-01509-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-021-01509-7