Abstract
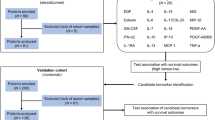
Early elevation of inflammatory cytokines, such as IL-6 or TNF-α, or CRP, which is a surrogate marker for IL-6, following commencement of PD-1/L1 inhibitors (PD1-I) may represent early activation of immune-cells. Serum IL-6 and TNF-α were measured in 10 non-small cell lung cancer patients who were evaluable within the 7 days before and after commencement of PD1-I. For CRP, medical records were reviewed and 34 patients with measured CRP within the 7 days before and after the treatment were evaluated. In the 10 patients analyzed for IL-6/TNF-α, the serum levels of IL-6/TNF-α were not significantly different between pre- and post-initial PD1-I [IL-6 20.3 (2.6–49.9) and 22.9 (3.6–96.1) pg/mL, p = 0.453; TNF-α 1.6 (0.7–6.3) and 3.3 (0.7–9.6) pg/mL, p = 0.329]; however, all four responses were observed among the 7 IL-6-elevated cases, resulting in a response rate of 57%. In the 34 patients analyzed for CRP, CRP was significantly increased after initial PD1-I [1.8 (0.1–17.8) mg/dL, 2.4 (0.0–27.8), p = 0.001]. Notably, in the 31 evaluable cases, all responses were again observed in either the IL-6 or CRP elevated groups and the response rate was 46% (11 of 24). The median overall survival time was not reached in the elevated group and was 112 days in the non-elevated group (p = 0.069). The early increase in inflammatory cytokines with PD1-I was indicated to be predictive for the efficacy in patients with non-small cell lung cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recent advances in metastatic non-small cell lung cancer (NSCLC) treatment have been dramatic and PD-1/PD-L1 inhibitors (PD1-I), either as a monotherapy or combination with chemotherapy, were clearly one of the central contributors for these advances [1,2,3,4,5,6,7,8,9]. However, although cytotoxic T cells were known to have a crucial role in exerting anti-tumor efficacy with PD1-I treatment, the detailed mechanisms of their anti-tumor effect were not fully understood.
Inflammatory cytokines are known to be one of the essential factors for raising protective immunity against infectious pathogens or neoplasms, and especially for connecting innate and adaptive immunity, and usually increase when host immunity is activated [10,11,12]. Regarding In preclinical models, inflammatory cytokines were reported to increase with PD-1/PD-L1 axis blockade through activation of T cells, natural killer cells, macrophages, or tumor infiltrating dendritic cells [13, 14]. However, little is known in humans.
Alterations to inflammatory cytokine levels after PD1-I were reported by Sanmamed et al. and showed that IL-8 reduction 2–4 weeks after treatment with PD1-I was associated with responses and an increase in overall survival time, while other cytokines, including IL-1β, IL-6, IL-10, IL-12, and TNF-α, did not significantly change in patients with melanoma or non-small cell lung cancer [15]. However, prediction in 2–4 weeks later is not early enough and IL-8 is not commonly measured in clinical practice. Furthermore, various factors including CRP at base-line, peripheral neutrophil lymphocyte ratio, LDH, and immune-related adverse events were indicated to be related to PD1-I efficacy [16,17,18,19,20,21,22,23], there is no generally accepted predictive clinical marker for PD1-I despite the recent robust pursuit.
Thus, we hypothesized that PD1-I activates immunity and impact on inflammatory cytokines in the very early phase after commencement of treatment and explored a possibility that the early alteration in inflammatory cytokines is predictive for the efficacy of PD1-I in patients with non-small cell lung cancer.
Materials and methods
Clinical records of 49 patients with non-small cell lung cancer who were treated with nivolumab or pembrolizumab from January 2016 to May 2017 at Seirei Mikatahara General Hospital, Japan, were reviewed. Among them, 34 non-small cell lung cancer patients with measured serum CRP within 7 days before and after commencement of nivolumab or pembrolizumab therapy were enrolled and analyzed. To evaluate CRP changes during the 30 days after commencement of PD1-I, 21 patients with serum CRP measurements at all of four time points, day − 7 to 0, day 1 to 7, day 8 to 15, and day 16 to 30, were included. When two or more measurements were available during the same interval, data from the closest day to the commencement of PD1-I for the day − 7 to 0 and data from the latest day for the other time points were chosen.
Serum IL-6 and TNF-α were measured by chemiluminescence enzyme immunoassay and enzyme-linked immunosorbent assay, respectively, by SRL. Inc. (Tokyo, Japan), in 10 non-small cell lung cancer patients who had evaluable serums taken within 7 days before and after commencement of PD1-I. Informed consent was obtained from the participants for the cytokine analysis according to the outline of ethical guidelines for medical and health research involving human subjects in Japan. The Seirei Mikatahara General Hospital ethics committee approved the current study (#17-7).
Changes in IL-6, TNF-α and CRP levels before and after commencement of PD1-I were compared by two sided paired t test. The relationship between IL-6, TNF-α, and CRP changes (elevated or not elevated) to the response rate and frequency of all or severe (≥ grade 3) adverse events (SAEs) was analyzed with Fisher’s exact test. The responses were evaluated according to the RECIST ver. 1.1[24], and the severity of adverse events was graded based on common terminology criteria for adverse events ver. 4.0. Overall survival was defined from the day of initial commencement of PD1-I to death or the final observed day and calculated according to the Kaplan–Meier method and compared with the log-rank test. All statistical analyses were performed with JMP version 5.01a (SAS Inc., Cary, NC, USA).
Results
Early serum IL-6 and TNF-α changes and the responses to PD-1 inhibitors
Clinical characteristics of the 10 patients analyzed for serum IL-6 and TNF-α are shown in Table 1. Their median age was 68, and all had a performance status of 1 or 0. The median cytokine measurements occurred 0 (range 0–7) days ahead and 3.5 (2–7) days behind commencement of PD1-I. All PD1-Is were nivolumab, and 6, 2, and 2 patients received a second, third, and fifth line, respectively.
Serum concentrations of IL-6 and TNF-α were 20.3 pg/ml (2.6–49.9) and 1.6 pg/ml (0.7–6.3)-treatment, and 22.9 pg/ml (3.6–96.1) and 3.3 pg/ml (0.7–9.6) post-treatment. There were no significant differences between pre- and post-initial PD1-I administration (p = 0.45, 0.33). Partial or complete responses were observed in 4 of 7 (57%) and 0 of 3 (0%) IL-6 elevated and non-elevated cases, respectively (p = 0.20), and the response rate between TNF-α elevated and non-elevated cases was similar, 33% (2 of 6) and 50% (2 of 4) (p = 0.60) (Table 2). The frequency of SAEs was 43% in IL-6 elevated cases and 50% in TNF-α elevated cases, while no SAEs were observed in IL-6 or TNF-α non-elevated cases.
Early CRP changes and the efficacy to PD-1 inhibitors
The clinical characteristics of 34 patients, including the 10 patients with measured cytokines, analyzed for serum CRP alterations are shown in Table 3. Median age was 67 (45–89), and 30 of 34 patients were at PS 0 or 1. CRP was measured 1 (range 0–7) day before and 3 (2–7) days after the commencement of PD1-I.
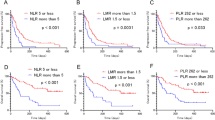
CRP was significantly increased after initial PD1-I administration from 1.8 mg/dl (0.1–17.8) to 2.4 mg/dl (0.0–27.8) (p = 0.001) (Fig. 1), and in 31 efficacy-evaluable cases, more responses were observed when CRP was elevated, 10 of 22 (45%), compared to 1 of 9 (11%) in non-elevated CRP- cases, although the difference was not statistically significant (p = 0.11). Of note, because the patient who responded in the non-elevated CRP group showed IL-6 elevation, all responding patients showed elevation of either of CRP or IL-6 within 7 days. The response rate was 46% (11 of 24) in cases with either elevated CRP or IL-6, which was significantly higher than in patients where neither was elevated (none of 7) (p = 0.03) (Table 2). Furthermore, patients with an increase in either IL-6 or CRP showed a tendency to live longer than patients where neither was elevated (p = 0.07) and the median survival time was not reached and 112 days, respectively (Fig. 2). The frequency of SAEs between either IL-6 or CRP elevated and non-elevated patients was similar 29% vs. 43% (p = 0.39) and that between CRP-elevated and non-elevated patients was 28% vs. 44% (p = 0.26). Immuno-staining with PD-L1 (clone 22C3) was performed in nine patients. Eight were ≧ 50% and one was 0%, and CRP was elevated seven of the eight with staining and in the one without.
CRP changes for 30 days after commencement of PD-1 inhibitors
CRP data for 30 days after commencement of PD1-I in 21 patients who had CRP data for all of four time points, day − 7–0, 1–7, 8–15, and 16–28, are shown in Fig. 3. After short-term surge within the first week, CRP reverted to the baseline by day 8–15. CRP at day 16–28 did not increase and was equivalent to day − 7–0, although 17 of the patients received second administration of PD1-I.
Discussion
Our study showed that CRP increased significantly within a week after initiation of PD1-I and that early inflammatory cytokine elevation was related to the efficacy of PD-1-I in patients with non-small cell lung cancer. Of note, none of the cases who did not have either elevated IL-6 or CRP responded to PD1-I.
IL-6, which most immune cells including dendritic cells, macrophages, and lymphocytes secret, is a common inflammatory cytokines and is known to be pleiotropic [11]. Although IL-6 is protective against infection through promoting survival of lymphocytes, antibody production, or bridging innate and adaptive immunity, it also functions as an immune-suppressant through various mechanisms, including induction of regulatory T cell, myeloid derived suppressor cells, and type 2 macrophages, or exhaustion of lymphocytes [11]. Further, a recent report that a combination of IL-6 inhibitors and PD-1/L1-inhibitors enhances anti-tumor efficacy [25], together with the negative impact of pre-treatment serum CRP levels on ICI efficacy [21], indicates the superiority of the suppressive role of IL-6 on the induction of anti-tumor immunity. In the current study, we used IL-6 and CRP, a surrogate marker of IL-6, as an indicator for the activation of immune cells and showed a correlation between elevation of IL-6 or CRP and an anti-tumor effect, which indicates the importance of early immune activation, rather than a role of IL-6 on immunity. Recently, several studies reported that early development of immune-related adverse events (irAEs) was predictive for the efficacy of PD1-I in patients with non-small cell lung cancer. Of note, Teraoka et al. showed that the development of irAEs 2 to 6 weeks after commencement of PD1-I, mostly pyrexia and rashes, was correlated with better efficacy of nivolumab [18]. These results also suggest very early immune-activation after PD1-I administration. According to the nature of the immune-system, inflammatory cytokine production is expected to precede irAEs development while, to the best of our knowledge, the present study is the first to reveal an association between short-term inflammatory cytokine elevation and anti-tumor efficacy in PD1-I treatment.
In some patients, IL-6 or CRP not only increased but also reduced after PD1-I administration. One possible explanation for this is that the host immune system did not recognize the tumor as foreign, also known as immune ignorance. However, considering a report by Franceschini et al. that showed regulatory T cells in mouse infected with hepatitis C virus was activated and inhibited cytotoxic immunity with PD1-I [26], there is also a possibility that PD-1 inhibitors adversely interrupted and suppressed the immune reaction through activation of immunosuppressive cells like regulatory T cells. These also explain that none of the 7 patients without increases in either IL-6 or CRP within a week responded to PD1-I and showed tendency to survive shorter. Because of expected suppressive mechanism of cytotoxic agents on regulatory T cells [27] and hopeful results of clinical trials with a combination therapy of PD-1 or PD-L1 inhibitors and cytotoxic agents [1, 6, 7], the combination, not monotherapy of PD1-I could be better choice for these patients.
After early elevation, CRP decreased over time, reverted to the baseline level in 2 weeks and did not increase again, although 17 of 21 patients received a second administration of PD1-I. This indicates two things; first, cytokine assessment later than 2 weeks after commencement of PD1-I may be too late to assess the impact of PD1-I on cytokine production, and second, immune-reaction after initial PD1-I is something distinctive from that after additional PD1-I administrations. Although the detailed mechanism remains unknown, Yamazaki et al. reported that the numbers of CD3+, CD4+, and CD8+ cells significantly decreased on day 3 after initial PD1-I administration and they all recovered on day 43 [28]. More attention should be paid to the very early immune-reaction after initial PD1-I.
This study has some limitations. Although all serum samples for cytokine and CRP measurements were taken within a week after commencement of PD1-I, the time points at which they were taken varied. Samples of 8/10 (80%) for cytokine analysis and 29/34 (85%) for CRP analysis were collected between day 2 and 4, while 15% of the CRP samples were taken from day 5 to 7. It should also be considered that a very limited range of cytokines, IL-6 and TNF-α, were measured as representative of inflammatory cytokines. Type of immune-cells mainly responsible for producing IL-6 and the detailed mechanism of immune-activation by PD1-I remains unknown, and further analysis with other cytokines such as IL-1β, IL-2, IL-10, TGF-β, MCP-1, etc. could be more informative and enable study of the specific mechanisms involved. Furthermore, the number of cases was small and differences in patient background could bias the results. Together with the inherent limitations in any retrospective study, further studies with more of cases are needed to confirm these results.
In conclusion, initial PD1-I administration increased CRP within a week in patients with non-small cell lung cancer, which indicated early immune-activation, and the early elevation of inflammatory cytokine was predictive for the efficacy of PD1-I. Further analysis focusing on early immune-activation after initial PD1-I is warranted.
References
Socinski MA, Jotte RM, Cappuzzo F, Orlandi F, Stroyakovskiy D, Nogami N, et al. Atezolizumab for first-line treatment of metastatic nonsquamous NSCLC. N Engl J Med. 2018;378:2288–301.
Rittmeyer A, Barlesi F, Waterkamp D, Park K, Ciardiello F, von Pawel J, et al. Atezolizumab versus docetaxel in patients with previously treated non-small-cell lung cancer (OAK): a phase 3, open-label, multicentre randomised controlled trial. Lancet. 2017;389:255–65.
Hellmann MD, Ciuleanu TE, Pluzanski A, Lee JS, Otterson GA, Audigier-Valette C, et al. Nivolumab plus ipilimumab in lung cancer with a high tumor mutational burden. N Engl J Med. 2018;378:2093–104.
Borghaei H, Paz-Ares L, Horn L, Spigel DR, Steins M, Ready NE, et al. Nivolumab versus docetaxel in advanced nonsquamous non-small-cell lung cancer. N Engl J Med. 2015;373:1627–39.
Brahmer J, Reckamp KL, Baas P, Crino L, Eberhardt WE, Poddubskaya E, et al. Nivolumab versus docetaxel in advanced squamous-cell non-small-cell lung cancer. N Engl J Med. 2015;373:123–35.
Paz-Ares L, Luft A, Vicente D, Tafreshi A, Gumus M, Mazieres J, et al. Pembrolizumab plus chemotherapy for squamous non-small-cell lung cancer. N Engl J Med. 2018.
Gandhi L, Rodriguez-Abreu D, Gadgeel S, Esteban E, Felip E, De Angelis F, et al. Pembrolizumab plus chemotherapy in metastatic non-small-cell lung cancer. N Engl J Med. 2018;378:2078–92.
Reck M, Rodriguez-Abreu D, Robinson AG, Hui R, Csoszi T, Fulop A, et al. Pembrolizumab versus chemotherapy for PD-L1-positive non-small-cell lung cancer. N Engl J Med. 2016;375:1823–33.
Herbst RS, Baas P, Kim DW, Felip E, Perez-Gracia JL, Han JY, et al. Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. Lancet. 2016;387:1540–50.
Apetoh L, Ghiringhelli F, Tesniere A, Obeid M, Ortiz C, Criollo A, et al. Toll-like receptor 4-dependent contribution of the immune system to anticancer chemotherapy and radiotherapy. Nat Med. 2007;13:1050–9.
Hunter CA, Jones SA. IL-6 as a keystone cytokine in health and disease. Nat Immunol. 2015;16:448–57.
Patidar A, Selvaraj S, Sarode A, Chauhan P, Chattopadhyay D, Saha B. DAMP-TLR-cytokine axis dictates the fate of tumor. Cytokine. 2018;104:114–23.
Barber DL, Wherry EJ, Masopust D, Zhu B, Allison JP, Sharpe AH, et al. Restoring function in exhausted CD8 T cells during chronic viral infection. Nature. 2006;439:682–7.
Rui Y, Honjo T, Chikuma S. Programmed cell death 1 inhibits inflammatory helper T-cell development through controlling the innate immune response. Proc Natl Acad Sci USA. 2013;110:16073–8.
Sanmamed MF, Perez-Gracia JL, Schalper KA, Fusco JP, Gonzalez A, Rodriguez-Ruiz ME, et al. Changes in serum interleukin-8 (IL-8) levels reflect and predict response to anti-PD-1 treatment in melanoma and non-small-cell lung cancer patients. Ann Oncol. 2017;28:1988–95.
Haratani K, Hayashi H, Chiba Y, Kudo K, Yonesaka K, Kato R, et al. Association of immune-related adverse events with nivolumab efficacy in non-small-cell lung cancer. JAMA Oncol. 2018;4:374–8.
Sato K, Akamatsu H, Murakami E, Sasaki S, Kanai K, Hayata A, et al. Correlation between immune-related adverse events and efficacy in non-small cell lung cancer treated with nivolumab. Lung Cancer. 2018;115:71–4.
Teraoka S, Fujimoto D, Morimoto T, Kawachi H, Ito M, Sato Y, et al. Early immune-related adverse events and association with outcome in advanced non-small cell lung cancer patients treated with nivolumab: a prospective cohort study. J Thorac Oncol. 2017;12:1798–805.
Nakamura Y, Kitano S, Takahashi A, Tsutsumida A, Namikawa K, Tanese K, et al. Nivolumab for advanced melanoma: pretreatment prognostic factors and early outcome markers during therapy. Oncotarget. 2016;7:77404–15.
Tanizaki J, Haratani K, Hayashi H, Chiba Y, Nakamura Y, Yonesaka K, et al. Peripheral blood biomarkers associated with clinical outcome in non-small cell lung cancer patients treated with nivolumab. J Thorac Oncol. 2018;13:97–105.
Oya Y, Yoshida T, Kuroda H, Mikubo M, Kondo C, Shimizu J, et al. Predictive clinical parameters for the response of nivolumab in pretreated advanced non-small-cell lung cancer. Oncotarget. 2017;8:103117–28.
Heppt MV, Heinzerling L, Kahler KC, Forschner A, Kirchberger MC, Loquai C, et al. Prognostic factors and outcomes in metastatic uveal melanoma treated with programmed cell death-1 or combined PD-1/cytotoxic T-lymphocyte antigen-4 inhibition. Eur J Cancer. 2017;82:56–65.
Diem S, Kasenda B, Spain L, Martin-Liberal J, Marconcini R, Gore M, et al. Serum lactate dehydrogenase as an early marker for outcome in patients treated with anti-PD-1 therapy in metastatic melanoma. Br J Cancer. 2016;114:256–61.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45:228–47.
Mace TA, Shakya R, Pitarresi JR, Swanson B, McQuinn CW, Loftus S, et al. IL-6 and PD-L1 antibody blockade combination therapy reduces tumour progression in murine models of pancreatic cancer. Gut. 2016.
Franceschini D, Paroli M, Francavilla V, Videtta M, Morrone S, Labbadia G, et al. PD-L1 negatively regulates CD4+ CD25+ Foxp3+ Tregs by limiting STAT-5 phosphorylation in patients chronically infected with HCV. J Clin Invest. 2009;119:551–64.
Roselli M, Cereda V, di Bari MG, Formica V, Spila A, Jochems C, et al. Effects of conventional therapeutic interventions on the number and function of regulatory T cells. Oncoimmunology. 2013;2:e27025.
Yamazaki N, Kiyohara Y, Uhara H, Iizuka H, Uehara J, Otsuka F, et al. Cytokine biomarkers to predict antitumor responses to nivolumab suggested in a phase II study for advanced melanoma. Cancer Sci. 2017;108:1022–31.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ozawa, Y., Amano, Y., Kanata, K. et al. Impact of early inflammatory cytokine elevation after commencement of PD-1 inhibitors to predict efficacy in patients with non-small cell lung cancer. Med Oncol 36, 33 (2019). https://doi.org/10.1007/s12032-019-1255-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-019-1255-3