Abstract
Whether circulating levels of specific cytokines at baseline link with treatment efficacy of immune checkpoint blockade (ICB) therapy in patients with non-small cell lung cancer remains unknown. In this study, serum samples were collected in two independent, prospective, multicenter cohorts before the initiation of ICB. Twenty cytokines were quantified, and cutoff values were determined by receiver operating characteristic analyses to predict non-durable benefit. The associations of each dichotomized cytokine status with survival outcomes were assessed. In the discovery cohort (atezolizumab cohort; N = 81), there were significant differences in progression-free survival (PFS) in accordance with the levels of IL-6 (log-rank test, P = 0.0014), IL-15 (P = 0.00011), MCP-1 (P = 0.013), MIP-1β (P = 0.0035), and PDGF-AB/BB (P = 0.016). Of these, levels of IL-6 and IL-15 were also significantly prognostic in the validation cohort (nivolumab cohort, N = 139) for PFS (log-rank test, P = 0.011 for IL-6 and P = 0.00065 for IL-15) and overall survival (OS; P = 3.3E-6 for IL-6 and P = 0.0022 for IL-15). In the merged cohort, IL-6high and IL-15high were identified as independent unfavorable prognostic factors for PFS and OS. The combined IL-6 and IL-15 status stratified patient survival outcomes into three distinct groups for both PFS and OS. In conclusion, combined assessment of circulating IL-6 and IL-15 levels at baseline provides valuable information to stratify the clinical outcome of patients with non-small cell lung cancer treated with ICB. Further studies are required to decipher the mechanistic basis of this finding.




Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ALK:
-
Anaplastic lymphoma kinase
- AUC:
-
Area under the curve
- CI:
-
Confidence interval
- DCB:
-
Durable clinical benefit
- EGF:
-
Epidermal growth factor
- EGFR:
-
Epidermal growth factor receptor
- GM-CSF:
-
Granulocyte–macrophage colony-stimulating factor
- HR:
-
Hazard ratio
- ICB:
-
Immune checkpoint blockade
- IFN:
-
Interferon
- IL:
-
Interleukin
- IL-1RA:
-
IL-1 receptor antagonist
- IP-10:
-
IFN-γ-inducible protein 10
- LIPI:
-
Lung immune prognostic index
- MCP-1:
-
Monocyte chemoattractant protein-1
- MIG:
-
Monokine induced by IFN-γ
- MIP-1β:
-
Macrophage inflammatory protein-1β
- NDB:
-
Non-durable benefit
- OS:
-
Overall survival
- PDGF:
-
Platelet-derived growth factor
- PD-1:
-
Programmed cell death protein 1
- PD-L1:
-
Programmed death-ligand 1
- PFS:
-
Progression-free survival
- PS:
-
Performance status
- ROC:
-
Receiver operating characteristic
- TNF:
-
Tumor necrosis factor
- TPS:
-
Tumor proportion score
References
Brahmer J, Reckamp KL, Baas P et al (2015) Nivolumab versus docetaxel in advanced squamous-cell non-small-cell lung cancer. N Engl J Med 373:123–135
Borghaei H, Paz-Ares L, Horn L et al (2015) Nivolumab versus docetaxel in advanced nonsquamous non-small-cell lung cancer. N Engl J Med 373:1627–1639
Reck M, Rodriguez-Abreu D, Robinson AG et al (2016) Pembrolizumab versus chemotherapy for PD-L1-positive non-small-cell lung cancer. New Engl J Med 375:1823–1833
Mok TSK, Wu YL, Kudaba I et al (2019) Pembrolizumab versus chemotherapy for previously untreated, PD-L1-expressing, locally advanced or metastatic non-small-cell lung cancer (KEYNOTE-042): a randomised, open-label, controlled, phase 3 trial. Lancet 393:1819–1830
McGrail DJ, Pilie PG, Rashid NU et al (2021) High tumor mutation burden fails to predict immune checkpoint blockade response across all cancer types. Ann Oncol 32:661–672
Iwai Y, Ishida M, Tanaka Y, Okazaki T, Honjo T, Minato N (2002) Involvement of PD-L1 on tumor cells in the escape from host immune system and tumor immunotherapy by PD-L1 blockade. Proc Natl Acad Sci U S A 99:12293–12297
Karayama M, Inoue Y, Yoshimura K et al (2022) Association of the geriatric nutritional risk index with the survival of patients with non-small cell lung cancer after nivolumab therapy. J Immunother 45:125–131
Kauffmann-Guerrero D, Kahnert K, Kiefl R et al (2021) Systemic inflammation and pro-inflammatory cytokine profile predict response to checkpoint inhibitor treatment in NSCLC: a prospective study. Sci Rep 11:10919
Gopalakrishnan V, Helmink BA, Spencer CN, Reuben A, Wargo JA (2018) The influence of the gut microbiome on cancer, immunity, and cancer immunotherapy. Cancer Cell 33:570–580
Briukhovetska D, Dorr J, Endres S, Libby P, Dinarello CA, Kobold S (2021) Interleukins in cancer: from biology to therapy. Nat Rev Cancer 21:481–499
Propper DJ, Balkwill FR (2022) Harnessing cytokines and chemokines for cancer therapy. Nat Rev Clin Oncol 19:237–253
Lim SY, Lee JH, Gide TN et al (2019) Circulating cytokines predict immune-related toxicity in melanoma patients receiving anti-PD-1-based immunotherapy. Clin Cancer Res 25:1557–1563
Laino AS, Woods D, Vassallo M et al (2020) Serum interleukin-6 and C-reactive protein are associated with survival in melanoma patients receiving immune checkpoint inhibition. J Immunother Cancer 8:e000842
Schalper KA, Carleton M, Zhou M et al (2020) Elevated serum interleukin-8 is associated with enhanced intratumor neutrophils and reduced clinical benefit of immune-checkpoint inhibitors. Nat Med 26:688–692
Yuen KC, Liu LF, Gupta V et al (2020) High systemic and tumor-associated IL-8 correlates with reduced clinical benefit of PD-L1 blockade. Nat Med 26:693–698
Kang DH, Park CK, Chung C et al (2020) Baseline serum interleukin-6 levels predict the response of patients with advanced non-small cell lung cancer to PD-1/PD-L1 inhibitors. Immune Netw 20:e27
Huseni MA, Wang L, Klementowicz JE et al (2023) CD8(+) T cell-intrinsic IL-6 signaling promotes resistance to anti-PD-L1 immunotherapy. Cell Rep Med 4:100878
Liu C, Yang L, Xu H et al (2022) Systematic analysis of IL-6 as a predictive biomarker and desensitizer of immunotherapy responses in patients with non-small cell lung cancer. BMC Med 20:187
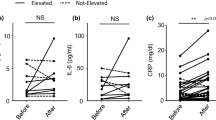
Inoue Y, Inui N, Karayama M et al (2022) Serum immune modulators associated with immune-related toxicities and efficacy of atezolizumab in patients with non-small cell lung cancer. J Cancer Res Clin Oncol (in press)
Inoue Y, Yoshimura K, Nishimoto K et al (2020) Evaluation of programmed death ligand 1 (PD-L1) gene amplification and response to nivolumab monotherapy in non-small cell lung cancer. JAMA Netw Open 3:e2011818
Mukama T, Fortner RT, Katzke V et al (2022) Prospective evaluation of 92 serum protein biomarkers for early detection of ovarian cancer. Br J Cancer 126:1301–1309
Mezquita L, Auclin E, Ferrara R et al (2018) Association of the lung immune prognostic index with immune checkpoint inhibitor outcomes in patients with advanced non-small cell lung cancer. JAMA Oncol 4:351–357
Wei C, Wang M, Gao Q et al (2022) Dynamic peripheral blood immune cell markers for predicting the response of patients with metastatic cancer to immune checkpoint inhibitors. Cancer Immunol Immunother 72:23–37
Kanda Y (2013) Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant 48:452–458
Lutgendorf SK, Weinrib AZ, Penedo F et al (2008) Interleukin-6, cortisol, and depressive symptoms in ovarian cancer patients. J Clin Oncol 26:4820–4827
Knupfer H, Preiss R (2010) Serum interleukin-6 levels in colorectal cancer patients–a summary of published results. Int J Colorectal Dis 25:135–140
Johnson DE, O’Keefe RA, Grandis JR (2018) Targeting the IL-6/JAK/STAT3 signalling axis in cancer. Nat Rev Clin Oncol 15:234–248
Tsukamoto H, Fujieda K, Miyashita A et al (2018) Combined blockade of IL6 and PD-1/PD-L1 signaling abrogates mutual regulation of their immunosuppressive effects in the tumor microenvironment. Cancer Res 78:5011–5022
Leu CM, Wong FH, Chang C, Huang SF, Hu CP (2003) Interleukin-6 acts as an antiapoptotic factor in human esophageal carcinoma cells through the activation of both STAT3 and mitogen-activated protein kinase pathways. Oncogene 22:7809–7818
Hong C, Schubert M, Tijhuis AE et al (2022) cGAS-STING drives the IL-6-dependent survival of chromosomally instable cancers. Nature 607:366–373
Hoejberg L, Bastholt L, Johansen JS, Christensen IJ, Gehl J, Schmidt H (2012) Serum interleukin-6 as a prognostic biomarker in patients with metastatic melanoma. Melanoma Res 22:287–293
Ashizawa T, Okada R, Suzuki Y et al (2005) Clinical significance of interleukin-6 (IL-6) in the spread of gastric cancer: role of IL-6 as a prognostic factor. Gastric Cancer 8:124–131
Martin F, Santolaria F, Batista N et al (1999) Cytokine levels (IL-6 and IFN-gamma), acute phase response and nutritional status as prognostic factors in lung cancer. Cytokine 11:80–86
Hailemichael Y, Johnson DH, Abdel-Wahab N et al (2022) Interleukin-6 blockade abrogates immunotherapy toxicity and promotes tumor immunity. Cancer Cell 40:509–523
Waldmann TA (2018) Cytokines in cancer immunotherapy. Cold Spring Harb Perspect Biol 10(12):a028472
Conlon KC, Lugli E, Welles HC et al (2015) Redistribution, hyperproliferation, activation of natural killer cells and CD8 T cells, and cytokine production during first-in-human clinical trial of recombinant human interleukin-15 in patients with cancer. J Clin Oncol 33:74–82
Miller JS, Morishima C, McNeel DG et al (2018) A first-in-human phase i study of subcutaneous outpatient recombinant human IL15 (rhIL15) in adults with advanced solid tumors. Clin Cancer Res 24:1525–1535
Wrangle JM, Velcheti V, Patel MR et al (2018) ALT-803, an IL-15 superagonist, in combination with nivolumab in patients with metastatic non-small cell lung cancer: a non-randomised, open-label, phase 1b trial. Lancet Oncol 19:694–704
Kurz E, Hirsch CA, Dalton T et al (2022) Exercise-induced engagement of the IL-15/IL-15Ralpha axis promotes anti-tumor immunity in pancreatic cancer. Cancer Cell 40:720–737
Felices M, Lenvik AJ, McElmurry R et al (2018) Continuous treatment with IL-15 exhausts human NK cells via a metabolic defect. JCI Insight 3:e96219
Tinhofer I, Marschitz I, Henn T, Egle A, Greil R (2000) Expression of functional interleukin-15 receptor and autocrine production of interleukin-15 as mechanisms of tumor propagation in multiple myeloma. Blood 95:610–618
Williams MT, Yousafzai Y, Cox C et al (2014) Interleukin-15 enhances cellular proliferation and upregulates CNS homing molecules in pre-B acute lymphoblastic leukemia. Blood 123:3116–3127
Wang H, Zhu JY, Liu CC et al (2015) Increased serum levels of interleukin-15 correlate with negative prognostic factors in extranodal NK/T cell lymphoma. Med Oncol 32:370
Kuniyasu H, Oue N, Nakae D et al (2001) Interleukin-15 expression is associated with malignant potential in colon cancer cells. Pathobiology 69:86–95
Argiles JM, Lopez-Soriano FJ, Busquets S (2009) Therapeutic potential of interleukin-15: a myokine involved in muscle wasting and adiposity. Drug Discov Today 14:208–213
Busquets S, Figueras MT, Meijsing S et al (2005) Interleukin-15 decreases proteolysis in skeletal muscle: a direct effect. Int J Mol Med 16:471–476
Acknowledgements
The authors would like to thank the patients, their families, and all the investigators who participated in this study. We thank Gabrielle White Wolf, PhD, from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Funding
This work was supported by Chugai Pharmaceutical Co., Ltd. (Tokyo, Japan). The funder had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
YI was involved in conceptualization, acquisition of data, data curation, formal analysis, investigation, methodology, project administration, resources, supervision, validation, visualization, writing—original draft, and writing—review and editing. NI was involved in conceptualization, acquisition of data, data curation, funding acquisition, investigation, methodology, project administration, resources, supervision, validation, visualization, writing—original draft, and writing—review and editing. MK, KA, MF, SM, TU, DH, TM, MI, HY, HH, YS, KF, NE, TF and TS were responsible for acquisition of data, data curation, supervision, validation, writing—review and editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts to declare.
Consent to participate
All patients provided written informed consent to participate in the study.
Ethical approval
This study was approved by the institutional review board at each site (Hamamatsu University School of Medicine, #18–164 for the discovery cohort and E16-051 for the validation cohort) and was conducted in accordance with the International Council for Harmonisation Good Clinical Practice guidelines and the Declaration of Helsinki. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines. This study was registered at the UMIN Clinical Trials Registry as UMIN000035616 and UMIN000022505.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
262_2023_3453_MOESM1_ESM.tif
Supplementary Figure S1. Receiver operating characteristic (ROC) curve analyses of serum IL-6 and IL-15 levels for the prediction of non-durable benefit. a ROC curve analysis of IL-6 levels in the discovery cohort. b ROC curve analysis of IL-15 levels in the discovery cohort. c ROC curve analysis of IL-6 levels in the validation cohort. d ROC curve analysis of IL-15 levels in the validation cohort. (TIF 869 KB)
262_2023_3453_MOESM2_ESM.tif
Supplementary Figure S2. Survival outcomes on the basis of baseline MCP-1, MIP-1β, or PDGF-AB/BB status in the discovery cohort. a Kaplan–Meier survival curves for PFS (left) and OS (right) on the basis of MCP-1 status (log-rank, P = 0.013 for PFS and P = 0.11 for OS). b Kaplan–Meier survival curves for PFS (left) and OS (right) on the basis of MIP-1β status (log-rank, P = 0.0035 for PFS and P = 0.42 for OS). c Kaplan–Meier survival curves for PFS (left) and OS (right) on the basis of PDGF-AB/BB status (log-rank, P = 0.016 for PFS and P = 0.41 for OS). MCP-1, monocyte chemoattractant protein-1; MIP-1β, macrophage inflammatory protein-1β; OS, overall survival; PDGF-AB/BB, platelet-derived growth factor-AB/BB; PFS, progression-free survival. (TIF 1303 KB)
262_2023_3453_MOESM3_ESM.tif
Supplementary Figure S3. Progression-free survival on the basis of baseline MCP-1 (a), MIP-1β (b), or PDGF-AB/BB (c) status in the validation cohort. P values were calculated by the log-rank test. (TIF 690 KB)
262_2023_3453_MOESM4_ESM.tif
Supplementary Figure S4. Patient and tumor characteristics on the basis of baseline IL-6 and IL-15 status in the merged cohort. a Proportion of patients who ever smoked or never smoked on the basis of IL-6 and IL-15 levels classified as both low, either high, or both high. P value was calculated by the Fisher exact test. b Proportion of patients with PD-L1 expression of ≥50% or <50% on the basis of IL-6 and IL-15 levels classified as both low, either high, or both high. P value was calculated by the Fisher exact test. c Proportion of patients harboring tumors with EGFR mutations or without on the basis of IL-6 and IL-15 levels classified as both low, either high, or both high. P value was calculated by the Fisher exact test. Among the patients in the merged cohort (N = 220), information regarding PD-L1 expression and EGFR mutations was available in 205 and 176 patients, respectively. EGFR, epidermal growth factor receptor; PD-L1, programmed death-ligand 1. (TIF 700 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Inoue, Y., Inui, N., Karayama, M. et al. Cytokine profiling identifies circulating IL-6 and IL-15 as prognostic stratifiers in patients with non-small cell lung cancer receiving anti-PD-1/PD-L1 blockade therapy. Cancer Immunol Immunother 72, 2717–2728 (2023). https://doi.org/10.1007/s00262-023-03453-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-023-03453-z