Abstract
The relationship between epidermal growth factor receptor (EGFR) mutation status and EGFR-tyrosine kinase inhibitors (TKI) efficacy in non-small cell lung cancer (NSCLC) patients has been well established. However, there is no available standard to define the optimal testing method and specimen type required for the detection of EGFR mutations. In this study, we compare results of ADx-amplification refractory mutation system (ARMS) and direct sequencing for the detection of EGFR mutation and prediction of EGFR-TKI efficacy for surgery and biopsy tumor tissues in 158 NSCLC patients. For 71 surgery samples, there were 13 and 17 positive samples detected by direct sequencing and ARMS, respectively. For 87 biopsy samples, direct sequencing and ADx-ARMS found 15 and 32 positive samples, respectively. For surgery samples, sensitivity of direct sequencing and ARMS was 72.2 % (13/18) and 94.4 % (17/18), respectively. For the biopsy samples, sensitivity of direct sequencing and ARMS was 44.1 % (15/34) and 94.1 % (32/34), respectively. For the biopsy and surgery samples, the ORRs for EGFR positive and negative patients detected by direct sequencing were 46.1 versus 16.7 and 66.7 versus 1.1 %, respectively. For ADx-ARMS, the ORR for EGFR positive patients was significantly higher than for negative patients (55.6 vs. 5.6 %). The median progression-free survival time of patients with EGFR wild type detected by direct sequencing (4.2 months) was significantly longer than that of patients with wild type detected by ARMS (1.7 months). ARMS has a higher sensitivity and specificity than direct sequencing for EGFR detection of mutation in both surgical and biopsy samples, and the results from ARMS are more consistent with the efficacy of EGFR-TKIs treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lung cancer is the leading cause of cancer-related deaths worldwide and causes over one million deaths per year [1]. Non-small cell lung cancer (NSCLC) is the most common histologic type, accounting for 80–85 % of all patients with lung cancer [2]. Although progress has been made in systematic chemotherapy for the treatment of advanced lung cancer, clinical outcomes are still limited by a tumor response rate of <35 %, and the median survival rate is only 8–11 months [3, 4].
In recent years, small-molecule tyrosine kinase inhibitors (TKIs), such as gefitinib (Iressa), erlotinib (Tarceva), and icotinib (Conmana), have shown great efficacy in NSCLC patients who have activation mutations in the epidermal growth factor receptor (EGFR) gene [5]. The relationship between EGFR mutation and therapeutic efficacy of EGFR-TKIs has been confirmed in several large-scale randomized clinical trials. Several studies (IPASS [6], WJTOG3405 [7], OPTIMAL [8] and First-Signal [9]) have found that the median progression-free survival time (mPFS) in EGFR-activating patients who received TKIs as the first-line treatment was more than 8 months, which is significantly longer than the mPFS (5 months) for patients receiving routine chemotherapy. In addition, the INTEREST [10] and INFORM [11] trials demonstrated that NSCLC patients with EGFR-activating mutations are also prone to achieve greater benefits from second-line and maintenance TKIs therapies. As a result, detection of EGFR mutation for predicting therapeutic efficacy of TKIs has played an essential role in therapeutic decision-making for NSLCL patients and has become a routine molecular test in an increasing number of hospitals.
At least 30 mutations have been found in exons 18–21 of the EGFR gene [12]. The in-frame deletions of exon 19 (E746-A750) and the point mutation at codon 858 in exon 21 (L858R) are the most common activating mutations, which account for approximately 90 % of all EGFR mutations and are closely related to the efficacy of EGFR-TKIs [13].
There are several methods to test for EGFR mutation, such as direct sequencing, denaturing high-performance liquid chromatography (DHPLC), and amplification refractory mutation system (ARMS). Direct sequencing and ARMS are the most commonly used methods worldwide. Compared to ARMS, direct sequencing is relatively inexpensive and easy to use, but time-consuming. However, ARMS has higher sensitivity and specificity for EGFR detection.
Although surgical resection of the tumor tissue (gross specimen) is considered to produce the best specimen type for EGFR mutation detection, most NSCLC patients who are diagnosed at advanced stages or who are in poor physical condition are not suitable for surgery. For those patients, small specimen samples, such as those from bronchoscopy and percutaneous lung puncture, are usually relatively easy to obtain and less invasive and give repeatable results.
Whether biopsy samples can be used instead of surgical sample for EGFF detection remains unclear. In particular, it is not known whether test results of these two specimen types are affected by different detection methods. In addition, the effect of using different methods to predict the efficacy of EGFR-TKIs in patients who have had surgical and biopsy samples tested has not been investigated. In this study, we compare EGFR detection results and analyze the clinical outcome of EGFR-TKI treatment determined by direct sequencing and by ARMS for surgical and biopsy specimens with the goal of providing data for clinical physicians to choose methods for EGFR detection for the different types of tumor specimens.
Materials and methods
Patients and materials
Patients who were newly diagnosed with stage I–IV NSCLC from October 2009 to December 2012 at Guangxi Medical University Affiliated Tumor Hospital were enrolled in this study. The study was reviewed and approved by the Institutional Ethics Committee of the hospital. Written informed consent was obtained from each patient prior to testing. Demographic, epidemiologic, pathological, and stage information for enrolled patients were extracted from their medical records. Tumor histology was classified by the criteria of the 3rd World Health Organization/International Association for the Study of Lung Cancer (IASCL) [14]. Tumor stages were determined using version 7 of the IASCL. Nonsmokers were defined as patients who had smoked <100 cigarettes in their lifetime. Smokers were current smokers or individuals who had stopped smoking for <1 year before diagnosis. All patients received no chemotherapy, radiotherapy, or targeted therapy before sample collection. Gross specimens are defined as tumor tissues obtained from various surgeries. A tiny or small biopsy specimen includes tissue obtained from transbronchial and percutaneous biopsies. Advanced patients who failed to respond to first-line chemotherapy were given 250 mg gefitinib or 150 mg erlotinib daily or 125 mg icotinib three times per day as second-line treatment on the basis of the EGFR mutation results or the patients’ willingness to use these drugs. Chest CT scans were performed monthly from the beginning of administration of EGFR-TKI. The response to EGFR-TKI was evaluated according to the response evaluation criteria in solid tumor (RECIST) criteria. Evaluations of complete response (CR) or partial response (PR) and stable disease (SD) or progression disease (PD) to treatment were validated 4 weeks later. Progression-free survival (PFS) was calculated from the date of the beginning of EGFR-TKI treatment to the date of tumor progression.
DNA extraction
Formalin-fixed and paraffin-embedded slices were deparaffinized in xylene and rehydrated in descending grades of ethanol. DNA was extracted using a SK1261 kit (Sangon, Shanghai, China), following the manufacturers’ instructions. The DNA quality was verified by formaldehyde agarose gel electrophoresis. The extracted DNA was stored at −20 °C until use.
Detection of E746-A750 del in exon 19 and L858R in exon 21 by direct sequencing
EGFR exons 19 and 21 were amplified by a polymerase chain reaction (PCR). Briefly, EGFR-19F (Forward: 5′-GCATCGCTGGTAACATCCAC-3′), 19R (Reverse: 5′-AGATGAGCAGGGTCTAGAGC-3′) and EGFR-21F (Forward: 5′-TGACCCTGAATTCGGATGCA-3′), 21R (Reverse: 5′-ATACAGCTAGTGGGAAGGCA-3′) were used as primers of exon 19 and 21, respectively. Total DNA extracted from tumor specimens was transferred into a single tube for amplification. The 50-μl PCR reaction system consisted of 25 μl Mix, 2 μl forward primer, 2 μl reverse primer (10 μmol/l), 2 μl template DNA, and 19 μl deionized water. PCR was performed with initial denaturation at 94 °C for 5 min, followed by 35 cycles of amplification (at 94 °C for 30 s, 58 °C for 30 s, and 68 °C for 1 min), and final extension at 68 °C for 10 min. The PCR amplification protocols for exon 21 were the same as those for exon 19. The PCR products were sequenced using an ABI 3730XL DNA analyzer (Applied Biosystems, Foster City, CA, USA) in both the forward and reverse directions. Results of direct sequencing were analyzed by Chromas software. Comparison between amplified sequences and the GenBank-archived human EGFR sequence (Accession No. AY588246) was performed by two independent investigators. In cases of disagreement, a third investigator made the final decision.
Detection of E746-A750 del in exon 19 and L858R in exon 21 by ARMS
Amplification refractory mutation system (ARMS) is a highly sensitive real-time PCR-based test that uses the principle of ARMS and covers the 29 EGFR mutation hotspots from exon 18–21. The assay was carried out according to the manufacturer’s protocol for the ADx EGFR29 Mutation Kit (Amoy Diagnostics, Xiamen, China) with the MX3000P (Stratagene, La Jolla, USA) real-time PCR system. The 25-μl RT-PCR reaction system consisted of 0.4 μl template DNA, 3.6 μl deionized water, and 16 μl other reaction components. PCR was performed with initial denaturation at 95 °C for 10 min, followed by 40 cycles of amplification (at 95 °C for 30 s and 61 °C for 1 min). The results were analyzed according to the criteria defined by the manufacturer’s instructions. Positive results were defined as Ct (sample) − Ct(control) < Ct(cut-off).
Statistical analyses
Surgical and biopsy samples were analyzed by chi-square or Fisher’s exact test to determine whether a statistically significant difference existed in sensitivity and specificity of detection of EGFR mutations between DNA sequencing and ARMS. EGFR mutation status, clinical pathological characteristics, and clinical response rate (RR) after TKI treatment were also analyzed by chi-square or Fisher’s exact test. The Kaplan–Meier method was used to estimate the median PFS after TKIs therapy between two follow-up groups with different EGFR status. P values and 95 % confidence intervals (CI) were calculated. The data were analyzed using SPSS version 14.0 Statistical Software (SPSS Inc., Chicago, USA), and P < 0.05 was considered to indicate statistical significance.
Results
Clinicopathologic characteristics of patients
A total of 158 tumor tissues were collected from patients with newly diagnosed NSCLC from October 2009 to December 2012, which included 71 biopsy specimens and 87 surgical specimens. The 71 biopsy specimens consisted of 59 transbronchial biopsies and 12 percutaneous biopsies. Clinical and pathological profiles of the enrolled patients are listed in Table 1.
Comparison of EGFR mutation status detected by direct sequencing and by ARMS for surgery samples and biopsy samples
Of 158 total samples, 28 (17.7 %) were found to have EGFR mutations by direct sequencing. Using ADx-ARMS, 49 of the 158 samples were mutation positive (31.0 %). Thus, the EGFR mutation rate was found to be higher using ARMS than direct sequencing (P = 0.003). Among 71 surgery samples, 13 were positive by direct sequencing (18.3 %) (Fig. 1). Using the ADx-ARMS method, 17 samples were found to be positive for mutation (23.9 %) (Fig. 2). There is no statistical difference in the detection of the EGFR mutation in the surgery samples using the two methods (P = 0.538). Of the 87 biopsy samples, 15 samples (17.2 %) were positive by direct sequencing and 32 mutations (36.8 %) were detected by ADx-ARMS. ARMS had a higher mutation detection rate in the biopsy samples than direct sequencing (P = 0.006).
Comparison of sensitivity, consistency, and specificity of surgery samples and biopsy samples detected by direct sequencing and arms
For the entire 158 samples, sensitivity for direct sequencing and for ADx-ARMS was 53.8 % (28/52) and 94.2 % (49/52), respectively (P = 0.000). For the 71 surgery samples, sensitivity for direct sequencing and for ADx-ARMS was 72.2 % (13/18) and 94.4 % (17/18), respectively, which are not statistically different (P = 0.177). For the 87 biopsy samples, sensitivity for direct sequencing and ADx-ARMS was 44.1 % (15/34) and 94.1 % (32/34), respectively (P = 0.000). Specificities of both methods were 100 %. For the 71 surgery samples, 6 samples showed inconsistent results for the detection by the two methods, with inconsistency and consistency rates of 8.5 % (6/71) and 91.5 % (65/71), respectively. Of the 87 biopsy samples, 22 showed inconsistent results, with an inconsistency of 25.2 % and a consistency of only 74.8 %. The inconsistency for the biopsy samples is higher than that for the surgery samples (P = 0.006). Comparisons of sensitivity, consistency, and specificity between surgery samples and biopsy samples are listed in Table 2.
Correlation between EGFR mutation status and clinicopathologic characteristics
Among all the clinicopathologic parameters, smoking history and pathological type demonstrate a correlation with EGFR mutation status detected by both methods. Frequencies of EGFR mutations were higher in patients who had never smoked and in adenocarcinomas patients. However, the patients’ age, gender, and clinical stage failed to correlate with their EGFR mutation status. The relationships between exon 19 and 21 mutations detected by both methods and the clinicopathologic characteristics are listed in Table 3.
Correlation between EGFR mutation status and EGFR-TKI efficacies
From the 158 total patients, the 45 who received EGFR-TKI as second-line treatment and had measurable tumors and complete follow-up data were included for efficacy analysis. Of these patients, 21 received gefitinib, 11 received erlotinib, and 13 received icotinib. For direct sequencing, the objective response rate in patients who had the EGFR-activating mutation was 52.6 %, which is significantly higher than that for EGFR wild-type patients (15.4 %, P < 0.05). In the biopsy and surgery samples, the ORRs in EGFR positive and negative patients were 46.1 versus 16.7 and 66.7 versus 12.5 %, with P values of 0.114 and 0.091, respectively, showing no statistical significance. Similar to the ORR of direct sequencing, the ORR of ARMS in EGFR positive patients was significantly higher than that of negative patients (55.6 vs. 5.6 %, P < 0.01). In biopsy samples, the ORR difference between EGFR positive and negative patients was also statistically significant (P < 0.01) (Table 4).
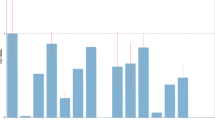
Comparisons were also made between PFS and EGFR mutation status detected by the two methods for the surgical and biopsy samples. The median progression-free survival time (mPFS) of the 19 patients who were assessed as mutation positive by direct sequencing was 10.3 months (95 % CI 7.0–13.6), while the mPFS of the 26 mutation negative patients was 4.2 months (95 % CI 3.7–4.4), which are statistically different (P < 0.01). For mutations assessed by ARMS, the mPFS of 27 mutation positive patients and 18 mutation negative patients was 10.3 months (95 % CI 7.2–13.3) and 1.7 months (95 % CI 0.3–4.2), respectively, also significantly different (P < 0.01) (Fig. 3). Further analysis of mPFS in wild-type patients showed that mPFS for patients identified by direct sequencing was significantly higher than for those identified by ARMS (4.2 vs. 1.7 months, P < 0.05), indicating the inclusion of false-negative results in the direct sequencing samples. It should also be noted that no difference was found in mPFS or ORR between 19-del mutation patients and L858R mutation patients, determined either by direct sequencing or by ARMS (P > 0.05). PFS and ORR of 19-del mutation and L858R mutation patients were 11.0 months, 61.0 % and 9.6 months, 65.5 %, respectively. Details are given in Table 5.
Discussion
The relationship between EGFR mutation status and EGFR-TKI efficacy in NSCLC patients is well established. Many factors, such as sensitivity and specificity of the detection method and quality and type of samples used for detection, can influence the detection results and affect clinical decision-making. At present, there is no specific guideline or gold standard available to define the optimal testing method and specimen type for the detection of EGFR mutations, although the different methods and suitable specimen types are currently under investigation [15–17].
Direct sequencing of specimens from all 158 patients identified 28 (17.7 %) EGFR mutations. This result is consistent with the INTEREST trial [18], in which a median positive rate of 30–40 % in gross specimens in Asian ethnic NSCLC patients was obtained by the same method. Using ARMS, the EGFR positive rate was found to be 31 % (49/158), which is higher than that from direct sequencing (P < 0.01). Similar to the meta-analysis conducted by Wu et al. [19], we found that EGFR mutations identified by the two methods were more common in patients who had adenocarcinoma histology as well as a history of nonsmoking. In addition, 19-del and L858R, the most common activating mutation types of the EGFR gene, showed nearly the same percentage in all patients. Zhang et al. [20] and Masago et al. [21] previously reported that 19-Del and L858R can coexist in the same individual. In our study, dual mutations were detected in three patients (1.9 %, 3/158) by ARMS. Two of three (1.3 %, 2/158) were detected by direct sequencing. These data (1.9 %, 3/158) confirm that the existence of both activating mutations is rare.
The detection rate obtained from the two methods with the surgical and biopsy specimens indicates that direct sequencing has a lower detection rate in biopsy specimens than ARMS (17.2 vs. 36.8 %, P < 0.01). In addition, direct sequencing has a lower level of sensitivity than ARMS (44.1 vs. 94.1 %, P < 0.01). Twenty-four specimens that were identified as wild type by direct sequencing were found to be positive by ARMS. Of those 24 specimens, 19 were biopsy specimens (79.2 %).
It has been reported that the sensitivity of direct sequencing is limited [22]. When the amount of tumor tissues in the specimen is <20 % or there are large numbers of normal cells mixed with the tumor tissues, the detection ability of direct sequencing is decreased [23]. Unlike direct sequencing, ARMS, which is based on quantitative PCR, identifies and amplifies EGFR mutation sequences by using specific probes, and normal cells in the sample do not interfere with this method. With its high selectivity and sensitivity, ARMS can detect <1 % mutant tumor tissue.
The primary reason for the significant differences in the detection of EGFR mutations in the biopsy and surgical specimens lies in the lower percentage of tumor cells in the biopsy specimens. Surgical samples have a large volume than biopsy samples, which allows tumor cells to be more easily separated from normal tissues. With the aid of micro-resection, the percentage of tumor tissues in surgical specimens can be >90 % after separation. In clinical practice, the lesions are biopsied at multiple sites in order to ensure an accurate diagnosis. This practice not only leads to scattered tumor cells in the biopsy samples but also results in a large number of normal cells in the samples. Because of this, use of the highly sensitive ARMS method instead of direct sequencing for EGFR detection in biopsy samples is likely to lead to more reliable results.
The purpose of determining the EGFR mutation status in the clinic is to screen all NSCLC patients for those who might benefit from EGFR-TKI treatment. Therefore, an evaluation of the usefulness of these detection methods depends on whether the results are consistent with TKI efficacy. The results of this study show that ARMS is a more sensitive method than direct sequencing and might detect more positive patients. However, some researchers believe that lung cancer is a heterogeneous disease, which includes both wild-type and mutant EGFR cells. If the mutant cells represent a minority of the whole tumor and are detected by more sensitive methods, the results may influence the final clinical outcome of TKIs. For example, the ORR for mutation positive patients in OPTIMAL using direct sequencing was 83 %, higher than that of IPASS using the ARMS method (71 %). Zhou Qing et al. [13] postulated that the differences in ORR might be attributed to relative EGFR mutant abundance rather than a difference in EGFR detection. However, our results show that ORR for mutation positive patients detected by direct sequencing and by ARMS was similar with 52.6 and 55.6 %, respectively. Interestingly, by using ARMS, three patients (1.9 %) were detected with double mutations involving both 19-del and L858R, whose clinical evaluations were all PR. These results indicate that patients with double activating mutations are more sensitive to EGFR-TKI than single activating mutation patients, which is consistent with the results of Zhang et al. [20].
We also found that ORR for wild-type patients determined by direct sequencing was 15.4 %, which is significantly higher than that determined using ARMS (5.6 %). The difference in ORR in wild-type patients between the two methods is due primarily to the biopsy samples. The ORR of biopsy samples simultaneously with wild type detected by direct sequencing reached 16.7 %. The PFS for the two methods in wild-type patients gives similar results (4.2 months for direct sequencing and 1.7 months for ARMS). This finding indicates that some wild-type patients, as determined by direct sequencing, still might obtain clinical benefit from EGFR-TKI treatment due to false-negative results, which is consistent with the results of the IPASS and the First-Signal trials. The ORR for mutation positive patients using ARMS in IPASS was only 1.1 %, significantly lower than that of First-SIGNAL, which used the direct sequencing method (25 %).
In conclusion, our findings suggest that gross specimen obtained from surgery is the best material for the detection of EGFR mutations. However, under conditions in which surgical specimens cannot be obtained, it is important to be aware that the test results may be influenced by the detection method with biopsy specimens. Using direct sequencing for the detection of mutation in biopsy specimens could reduce the ability to detect mutation detections. In this case, the reliability of these results to predict TKI efficacy is decreased. This problem can be minimized by using highly sensitive methods such as ARMS to minimize false-negative results.
References
Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010;60:277–300.
Govindan R, Page N, Morgensztern D, Read W, Tierney R, et al. Changing epidemiology of small-cell lung cancer in the United States over the last 30 years: analysis of the surveillance, epidemiologic, and end results database. J Clin Oncol. 2006;24:4539–44.
Sweeney CJ, Zhu J, Sandler AB, Schiller J, Belani CP, et al. Outcome of patients with a performance status of 2 in Eastern Cooperative Oncology Group Study E1594: a phase II trial in patients with metastatic non small cell lung carcinoma. Cancer. 2001;92:2639–47.
Schiller JH, Harrington D, Belani CP, Langer C, Sandler A, et al. Comparison of four chemotherapy regimens for advanced non-small-cell lung cancer. N Engl J Med. 2002;346:92–8.
Paez JG, Jänne PA, Lee JC, Tracy S, Greulich H, et al. EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science. 2004;304:1497–500.
Mok TS, Wu YL, Thongprasert S, Yang CH, Chu DT, et al. Gefitinib or carboplatin–paclitaxel in pulmonary adenocarcinoma. N Engl J Med. 2009;361:947–57.
Mitsudomi T, Morita S, Yatabe Y, Negoro S, Okamoto I, et al. Gefitinib versus cisplatin plus docetaxel in patients with non-small-cell lung cancer harbouring mutations of the epidermal growth factor receptor (WJTOG3405): an open label, randomised phase 3 trial. Lancet Oncol. 2010;11:121–8.
Zhou C, Wu YL, Chen G, Feng J, Liu XQ, et al. Erlotinib versus chemotherapy as first-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer (OPTIMAL, CTONG-0802): a multicentre, open-label, randomised, phase 3 study. Lancet Oncol. 2011;12:735–42.
Han JY, Park K, Kim SW, Lee DH, Kim HY, et al. First-SIGNAL: first-line single-agent iressa versus gemcitabine and cisplatin trial in never-smokers with adenocarcinoma of the lung. J Clin Oncol. 2012;30:1122–8.
Kim ES, Hirsh V, Mok T, Socinski MA, Gervais R, et al. Gefitinib versus docetaxel in previously treated non-small-cell lung cancer (INTEREST): a randomised phase III trial. Lancet. 2008;372:1809–18.
Zhang L, Ma S, Song X, Han B, Cheng Y, et al. Gefitinib versus placebo as maintenance therapy in patients with locally advanced or metastatic non-small-cell lung cancer (INFORM; C-TONG 0804): a multicentre, double-blind randomised phase 3 trial. Lancet Oncol. 2012;13:466–75.
Kosaka T, Yatabe Y, Endoh H, Kuwano H, Takahashi T, et al. Mutations of the epidermal growth factor receptor gene in lung cancer: biological and clinical implications. Cancer Res. 2004;64:8919–23.
Zhou Q, Zhang XC, Chen ZH, Yin XL, Yang JJ, et al. Relative abundance of EGFR mutations predicts benefit from gefitinib treatment for advanced non-small-cell lung cancer. J Clin Oncol. 2011;29:3316–21.
Beasley MB, Brambilla E, Travis WD. The 2004 World Health Organization classification of lung tumors. Semin Roentgenol. 2005;40:90–7.
Zhang X, Zhao Y, Wang M, Yap WS, Chang AY. Detection and comparison of epidermal growth factor receptor mutations in cells and fluid of malignant pleural effusion in non-small cell lung cancer. Lung Cancer. 2008;60:175–82.
Bai H, Mao L, Wang HS, Zhao J, Yang L, et al. Epidermal growth factor receptor mutations in plasma DNA samples predict tumor response in Chinese patients with stages IIIB to IV non-small-cell lung cancer. J Clin Oncol. 2009;27:2653–9.
Santis G, Angell R, Nickless G, Quinn A, Herbert A, et al. Screening for EGFR and KRAS mutations in endobronchial ultrasound derived transbronchial needle aspirates in non-small cell lung cancer using COLD-PCR. PLoS ONE. 2011;6:e25191.
Douillard JY, Shepherd FA, Hirsh V, Mok T, Socinski MA, et al. Molecular predictors of outcome with gefitinib and docetaxel in previously treated non-small-cell lung cancer: data from the randomized phase III INTEREST trial. J Clin Oncol. 2010;28:744–52.
Wu YL, Zhong WZ, Li LY, Zhang XT, Zhang L, et al. Epidermal growth factor receptor mutations and their correlation with gefitinib therapy in patients with non-small cell lung cancer: a meta-analysis based on updated individual patient data from six medical centers in mainland China. J Thorac Oncol. 2007;2:430–9.
Zhang GC, Lin JY, Wang Z, Zhou Q, Xu CR, et al. Epidermal growth factor receptor double activating mutations involving both exons 19 and 21 exist in Chinese non-small cell lung cancer patients. Clin Oncol. 2007;19:499–506.
Masago K, Fujita S, Kim YH, Ichikawa M, Hatachi Y, et al. Epidermal growth factor receptor (EGFR) double-activating somatic mutations in exons 19 and 21 in Japanese non-small cell lung cancer patients. Cancer Genet Cytogenet. 2009;195:179–82.
Li J, Wang L, Mamon H, Kulke MH, Berbeco R, Makrigiorgos GM. Replacing PCR with COLD-PCR enriches variant DNA sequences and redefines the sensitivity of genetic testing. Nat Med. 2008;14:579–84.
Ellison G, Donald E, McWalter G, Knight L, Fletcher L, et al. A comparison of ARMS and DNA sequencing for mutation analysis in clinical biopsy samples. J Exp Clin Cancer Res. 2010;29:132.
Acknowledgments
The authors thank the Bureau of Science and Technology, Guangxi Zhuang Autonomous Zone, China, Grant number: 201017.
Conflict of interest
No potential conflicts of interest were disclosed.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shaozhang, Z., Ming, Z., Haiyan, P. et al. Comparison of ARMS and direct sequencing for detection of EGFR mutation and prediction of EGFR-TKI efficacy between surgery and biopsy tumor tissues in NSCLC patients. Med Oncol 31, 926 (2014). https://doi.org/10.1007/s12032-014-0926-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-014-0926-3