Abstract
Osteosarcomas of the jaws are rare mesenchymal tumors frequently diagnosed in the fourth decade of life which account for 6 % of all osteosarcomas. This study evaluated the efficacy on the patients outcome of multimodality treatment consisting of surgery, chemotherapy and radiotherapy. The records of 22 patients affected by jaw osteosarcoma treated with a combination of surgery, poly-chemotherapy and adjuvant radiotherapy in selected cases were reviewed. Response rate, progression-free survival and overall survival were evaluated. Neoadjuvant chemotherapy resulted in an overall response rate of 83.3 %, necrosis of grade I or II was obtained, respectively, in 44.4 and 55.6 % of the patients, and surgery was radical in all patients. At a median follow-up of 60 months, the 5-year progression-free survival and overall survival were 73.5 and 77.4 %, respectively. These outcome parameters significantly correlated with age at diagnosis and grade of chemotherapy-induced necrosis. A complex multimodality approach including chemotherapy and radiotherapy, along with radical surgery, can maximize the outcome of patients affected by osteosarcoma of the jaws.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Osteosarcomas (OSs) are rare bone tumors defined by the presence of malignant mesenchymal cells producing osteoid or immature bone. They are highly malignant and account approximately for 40–60 % of all primary malignant bone tumors [1–3]. The peak incidence is in the fourth decade, and males are affected more frequently than females. Osteosarcoma of the jaws (JOS) is extremely rare, representing about 7 % of all OSs and 1 % of all head and neck malignancies [1, 2, 4–9]. Mandible and maxilla are involved almost equally. JOS is diagnosed about two decades later than their long bone counterparts, which have a peak of incidence during adolescence [6]. Previous radiotherapy (RT) of the maxillofacial region is a predisposing factor [3, 6]. Microscopically, approximately 50 % of JOS are chondroblastic, with a minimal production of osteoid matrix or osteoblastic. Less frequent histological subtypes are myxoid and fibroblastic OSs [1–5].
The prognosis depends on different factors: histological subtype, grade of malignancy, tumor size, age, and response to chemotherapy (CHT) [6, 9–13]. Previous studies carried out on long bones sarcomas have shown that the grade of CHT-induced necrosis, classified on the basis of tumor vital tissue found in the surgical sample [10, 12, 13], is the most important prognostic indicator, being the grading as follows: grade I, necrosis less than 50 % (no therapeutic efficacy); grade II, necrosis 50–89 % (poor therapeutic efficacy); grade III, necrosis 90–99 % (good therapeutic efficacy); grade IV, total tumor necrosis (excellent therapeutic efficacy).
Head and neck OSs have a tendency to recur locally and are associated with a metastatic rate of 20–30 %, lower than OSs of the extremities [1, 2, 6–8, 14]. Since the introduction of multimodal treatment consisting of a combination of surgery, CHT and/or RT, the prognosis has impressively improved.
Surgery has a crucial role; aggressive surgical resection and advanced reconstruction techniques are the mainstay of treatment, as the single most important factor for cure is radical resection [6–10, 13–25]. Because of the complex anatomy of the maxillofacial region, clear margins may be technically difficult to achieve, mostly in the maxilla [15, 16, 22–25].
The role of CHT has still to be defined [15, 16, 21–26]. Micrometastases of JOS can be present at diagnosis. Perioperative CHT can offer some potential benefit: It might enable less destructive surgery and eventually increase the chance to obtain clear margins, eradicate micrometastases and give some information about the chemosensitivity of the tumor, so improving loco-regional and distal control. Two meta-analyses reported conflicting results. Kassir et al. [25] found no advantage for adjuvant CHT or RT after surgery, while in the report by Smeele et al. [16] both disease-free survival (DFS) and overall survival (OS) were significantly improved by CHT but not by RT. The role of RT is not yet clear in the multimodal strategy, but it has to be considered in case of positive margins or high-grade tumors [14, 15, 23, 27, 30]. Here, we report a monoistitutional experience on a treatment strategy including pre- and postoperative CHT, surgery and RT for selected cases.
Materials and methods
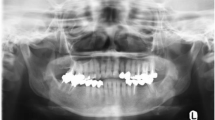
The clinical and pathological records of patients with a first diagnosis of JOS at the Department of Oncology, San Paolo University Hospital, from January 2001 to January 2011 have been analyzed. Twenty-two cases of JOS were identified, and records were reviewed for demographics, risk factors, presenting symptoms, imaging, treatment, follow-up and survival. Patients received a thorough clinical examination and appropriate imaging including computerized tomography (CT) or magnetic resonance (MR), to evaluate regional invasion or disseminated disease. Response rates were evaluated according to response evaluation criteria in solid tumors (RECIST) [28].
Written informed consent was obtained from all patients who underwent CHT, RT, radical surgery and reconstruction. In 18 patients (80 %), surgery was preceded by neoadjuvant CHT consisting of a complex sequence of agents, namely cisplatin (C) 100 mg/m2 day 1, doxorubicin (D) 75 mg/m2 day 1,49, ifosfamide (I) d 22,49 and methotrexate (M) 6 g/m2 day 22,49, administered before surgery. All patients completed the scheduled treatment and, after 1 month on average, were operated. Four patients did not receive neoadjuvant CHT because they refused this option and decided to proceed with surgery immediately. All patients were treated with adjuvant CHT up to 30 weeks consisting of the same agents administered alternatively in order to reach a total dose of 375 mg/m2 for D and 600 mg/m2 for C, 54 g/m2 for I. The maximum dose of MTX was 36 g/m2.
Seven patients were given adjuvant RT up to a total dose of 60 Gy, because either they skipped neoadjuvant CHT or had only stable disease (SD) as the best result from neoadjuvant CHT. From the end of treatment, patients were followed every 3 months for the first 2 years, every 6 months for the next 3 years and then yearly. CT/MR of the head and neck region was planned every 6 months and CT of the chest yearly. The median follow-up was 60 months (range 9–132 months).
Toxicity was graded according to Common Terminology Criteria for Adverse Events v3.0 (CTCAE) [29] and recorded for all patients included in the analysis. Age, sex, site, histological subtype and grade of CHT-induced necrosis were analyzed for correlations with OS and progression-free survival (PFS).
Statistical analysis
OS was calculated from the time of diagnosis until death or last follow-up. PFS was calculated from the end of treatment to relapse. Survival curves were estimated by the method of Kaplan–Meier that is used to estimate the survival function from lifetime data and to measure the fraction of patients living for a certain amount of time after treatment. In accordance with the statistical design, a stratified, one-sided, long-rank test adjusting for age and CHT-induced necrosis was used to compare OS and PFS between groups.
Results
Twenty-two patients were evaluated. Median age at diagnosis was 38 years (17–76 years), 10 were females and 12 males (ratio 0, 8:1). The mandible was involved in 12 cases and the maxilla in 10 cases. Histological subtypes were chondroblastic in 11 cases, (50 %), osteoblastic in nine cases (41 %) and fibroblastic or myxoid subtype in two cases (9 %). No patient had lymph node involvement at diagnosis. Median tumor volume was 133 cm3 (2.1–268.1) (Table 1). No patient had been previously exposed to radiation therapy. The most common presenting symptoms were swelling at the site of disease (n = 22, 100 %), pain (n = 15, 68 %), facial dysesthesia (n = 7, 32 %) and loosening of the teeth (n = 3, 14 %). Overall, at the end of neoadjuvant treatment, eight patients (44.4 %) had a complete response (CR) and seven patients (38.9 %) a partial response (PR), while three patients (16.7 %) had stable disease SD) (Table 2).
Surgery consisted of hemimandibulectomy or hemimaxillectomy and was radical in all patients. The forearm flap and fibula free flap were the most common flaps in soft and hard tissue reconstruction of the defects. Eighteen surgical specimens from patients treated with neoadjuvant CHT were evaluated for the grade of CHT-induced necrosis. Eight patients (44.4 %) had grade I, and ten patients (55.6 %) grade II necrosis. No patient had grade III or IV necrosis. In addition to CHT, adjuvant RT was offered to seven patients (32 %). The first reason was surgery not preceded by neoadjuvant CHT in the four patients who refused it. Among these, one went into progression developing a solitary cerebellar metastasis treated by stereotactic RT, which stabilized the disease up to 24 months. The remaining three patients had no local recurrence, nodal or distant involvement. The second reason was SD as the best response after the neoadjuvant phase of CHT, occurring in three patients. Two of them died within 2 years because of local recurrence.
In the majority of patients (n = 15, 68.2 %), adjuvant RT was not employed. Three patients in this group died within 2 years with local or metastatic recurrence (pulmonary metastases), and 12 patients remained disease-free during the follow-up period.
At a median follow-up of 60 months (range 9–132), PFS and OS were 73.5 and 77.4 %, respectively (Figs. 1, 2). PFS and OS were not statistically different according to the site (mandibular vs. maxillary), the histological subtype (osteoblastic vs. chondroblastic vs. fibroblastic/myxoid), the tumor volume and the use of adjuvant RT. A statistically significant difference was found in OS and PFS between patients under or over 40 years (5-year OS 93 vs. 50 %, p = 0.0206; 5-year PFS 93 vs. 37.5 %, p = 0.0068, respectively) (Figs. 3, 4).
A significant difference was also found between grade I and grade II CHT-induced necrosis (OS 43 vs. 89 %, p = 0.0032; PFS 43 vs. 89 %, p = 0.0334, respectively) (Figs. 5, 6).
The main grade 3–4 toxicities during CHT were hematological (25 %), gastrointestinal (20 %) and neurological (15 %). Oropharyngeal mucositis was the most frequent grade 3–4 toxicity during RT (40 %) as shown in Table 3. No toxic deaths were observed during the treatment period.
Discussion
JOS is a rare and highly malignant disease [1, 2, 4–9]. In the last 20 years, few retrospective studies on small series of patients have been published and the treatment regimens reported are highly variable. Bertoni et al. [17] reported the Istituto Rizzoli-Beretta experience with JOS concerning 28 patients who underwent surgery (26 patients) or RT (2 patients) as first treatment. Only three patients received adjuvant treatment (2 RT and 1 CHT): The 5-year OS rate for the whole group was a disappointing 23 % and the recurrence rate as high as 85.7 %. These findings might be related to the high percentage of patients inadequately operated (13 out of 26; 50 %) and to the modest efficacy of surgery as a unique treatment.
Two small retrospective studies on OS of the jaws from Panizzoni et al. [30] and Doval et al. [31] using different CHT protocols based on cyclophosphamide, D, C, vincristine and M in addition to surgery demonstrated that CHT could favorably impact on survival, but still in the former report 2-year OS was only 37 %.
The innovative concepts coming out from these studies about the role of CHT were further supported by a systematic review on 201 patients from 20 uncontrolled series [16]. Out of 180 patients, various CHT regimens were given to 60 patients prior to (neoadjuvant, 18 patients) or after surgery (adjuvant, 42 patients). Eleven patients did not undergo surgery. Surgical resection was complete in 105 cases (58.3 %). RT was used in 69 patients. The 5-year OS and PFS in patients treated with a multimodal treatment (surgery and neoadjuvant and/or adjuvant CHT, n = 27) were 80 and 75 %, respectively. The 5-year OS and DFS in those patients who underwent radical surgery alone (n = 78) were 40 and 33 %, respectively; CHT significantly improved survival when combined with radical surgery while the effect of RT was not significant [17]. A few more studies have demonstrated the importance of the status of resection margins. In a retrospective analysis of a Canadian multicentre study that included 35 patients with osteogenic sarcoma of the jaws, the 5-year OS and PFS were significantly greater (hazard ratio = 3.5, p < 0.04) for patients whose resections showed clear surgical margins (n = 25); a trend toward a better prognosis was shown with adjuvant CHT [18].
A recent retrospective study on patients with JOS (n = 30) by Granowski-Le Cornu et al. [32] showed an overall 5-year survival of 68 % with a significant difference between patients treated before and after 1991. In the former cohort, the 5-year OS was 52 %, while in the latter it was 77 %, a result in line with our own. The difference was ascribed to earlier diagnosis, improved imaging and more aggressive treatment, including neoadjuvant CHT and better reconstructive options.
In the retrospective study of Herrmann et al. [33], surgery alone resulted in a 5-year OS rate of 20 %. Granados-Garcia et al. [34] achieved a similar overall 5-year survival rate of 20 % on 20 patients, although they treated 12 cases with surgery alone, and the others with a combination of CHT, radiation and surgery.
In the small retrospective study of Thiele et al. [24] on 12 patients, the 5-year OS and PFS were 100 and 90 %, respectively, in the five patients treated with neoadjuvant and adjuvant CHT. In the group of seven patients who underwent surgery alone, the 5-year rates were much lower (almost 30 %). Obviously so few patients in the series are of limited value.
The role of RT in the multimodal treatment is not yet completely clear. Guadagnolo et al. [14] evaluated the role of RT in the combined modality treatment. They studied 119 patients affected by JOS. Of these patients, 92 underwent surgery alone, whereas 27 were treated with surgery and RT. Five-year OS and DFS rates were 63 and 67 %. Stratified analysis by resection margin status demonstrated that the combined use of surgery and RT compared with surgery alone improved OS (80 vs. 31 %) and DFS (80 vs. 35 %) in patients with positive or uncertain margins. However, a 40 % 5-year rate of RT-induced complications has to be taken into account when considering the combined approach. The results of the study indicate that RT in addition to surgery improves OS and PFS in patients with positive or uncertain margins, while no advantage is expected for patients with negative margins.
Our data refer to 22 patients treated with a multimodal approach consisting of CHT, surgery, notably radical in all patients, and RT added only in selected cases (surgery not preceded by CHT or stable disease after neoadjuvant CHT). At a median follow-up of 60 months, 17 patients are still alive without any sign of local recurrence or systemic disease. The 5-year OS and PFS are 77 and 73 %, respectively, that favorably compare with previous published reports.
Most retrospective reviews stressed the prognostic importance of CHT-induced necrosis for local control of patients with JOS [10, 12, 13]. In our study, this factor was statistically significant too; all the patients who died for tumor progression had ≤50 % necrosis, and in three cases <10 %.
Metastases in regional lymph nodes are reported to be extremely unlike [24], and accordingly, no patient in our series showed any sign of regional lymph node metastases.
Kassir et al. [25] found no statistical difference in survival between maxillary and mandibular osteosarcomas. In our analysis, the mandible was involved more often than the maxilla, but the difference in survival between these two areas was not statistically significant.
In a retrospective review, August et al. [6] evaluated 30 cases of JOS. They noted that patients’ age may influence prognosis with survivors being on average 27 year-old and non-survivors 40 year-old. In our study, a statistically significant increased survival was evident among patients younger than 40 years. This may be likely due to a better tolerance to CHT and a higher dose intensity in this subgroup of patients. In conclusion, our data, together with the results of previous studies, suggest that patients affected by JOS treated with neoadjuvant CHT, radical surgery and postoperative CHT can maximize disease-free and overall survival. While adjuvant RT can be useful in selected cases, the crucial positive prognostic factor remains completeness of surgery, being clear margins the most important target to be achieved. Over the years, the chance of surviving for these patients has greatly improved as a result of an aggressive systemic approach and the improvement of surgical techniques. Nowadays, we can reasonably hope to cure 3 out of 4 patients suffering from such treacherous malignant tumors, and nonetheless, all the efforts should still go in the direction of further clinical and biological research.
Conclusion
JOS is a highly malignant tumor whose successful treatment requires an integrated cooperation between surgery, CHT and RT. Complete surgical resection and reconstruction are the cornerstone of therapy, while the role of perioperative CHT and adjuvant RT deserves further studies.
References
Campanacci M. Bone and soft tissue tumors. Wien: Springer; 1999.
Dahlin DC, Unni KK. Osteosarcoma bone tumors. Springfield: CC Thomas; 1986.
Klein MJ, Siegal GP. Osteosarcoma: anatomic and histologic variants. Am J Clin Pathol. 2006;125:555–81.
Nakayama E, Sugiura K, Kobayashi I, Oobu K, Ishibashi H, Kanda S. The association between the computed tomography findings, histologic features, and outcome of osteosarcoma of the jaw. J Oral Maxillofac Surg. 2005;63:311–8.
Paparella ML, Olvi LG, Brandizzi D, Keszler A, Santini-Araujo E, Cabrini RL. Osteosarcoma of the jaw: an analysis of a series of 74 cases. Histopathology. 2013;63(4):551–7.
August M, Magennis P, Dewitt D. Osteogenic sarcoma of the jaws: factors influencing prognosis. Int J Oral Maxillofac Surg. 1997;26:198–204.
Clark JL, Unni KK, Dahlin DC, Devine KD. Osteosarcoma of the jaw. Cancer. 1983;51:2311–6.
Dahlin DC. Prognostic factors in osteosarcoma. Int J Radiat Oncol Biol Phys. 1980;6:175.
Vadillo RM, Contreras SJ, Canales JO. Prognostic factors in patients with jaw sarcomas. Braz Oral Res. 2011;25(5):421–42.
Garrington GE, Scofield HH, Cornyn J, Hooker SP. Osteosarcoma of the jaws: analysis of 56 cases. Cancer. 1967;20:377–91.
Coindre JM, Trojani M, Contesso G, David M, Rouesse J, Bui NB, Bodaert A, De Mascarel I, et al. Reproducibility of a histopathologic grading system for adult soft tissue sarcoma. Cancer. 1986;58(2):306–30.
Picci P, Sangiorgi L, Rougraff BT, Neff JR, Casadei R, Campanacci M. Relationship of chemotherapy-induced necrosis and surgical margins to local recurrence in osteosarcoma. J Clin Oncol. 1994;12:2699–705.
Rosen G, Capparos B, Huvos AG, Kosloff C, Nirenberg A, Cacavio A, et al. Preoperative chemotherapy for sarcoma: selection of postoperative adjuvant chemotherapy based on the response of the primary tumor preoperative chemotherapy. Cancer. 1982;49:1221–3.
Guadagnolo BA, Zagars GK, Raymond AK, Benjamin RS, Sturgis EM. Osteosarcoma the jaw/craniofacial region: outcomes after multimodality treatment. Cancer. 2009;115:3262–70.
Jasnau S, Meyer U, Potratz J, Jundt G, Kevric M, Joos UK, Jürgens H, et al. Craniofacial osteosarcoma: experience of the cooperative German–Austrian–Swiss osteosarcoma study group. Oral Oncol. 2008;44:286–90.
Smeele LE, Kostense PJ, Van der Waal I, Snow GB. Effect of chemotherapy on survival of craniofacial osteosarcoma: a systematic review of 201 patients. J Clin Oncol. 1997;15:363–7.
Bertoni F, Dallera P, Bacchini P, Marchetti C, Campobassi A. The Istituto Rizzoli-Beretta experience with osteosarcoma of the jaw. Cancer. 1991;68:1555–6.
Canadian Society of Otolaryngology-Head and Neck Surgery Oncology Study Group. Osteogenic sarcoma of the mandible and maxilla: a Canadian review (1980–2000). J Otolaryngol. 2004;33:139–40.
Ha PK, Eisle DW, Frassica FJ, Zahurak ML, McCarthy EF. Osteosarcoma of the head and neck: a review of the Johns Hopkins experience. Laryngoscope. 1999;109:964–96.
Smeele LE, Van der Wal JE, Van Diest PJ, Van der Waal I, Snow GB. Radical surgical treatment in craniofacial osteosarcoma gives excellent survival: a retrospective cohort study of 14 patients. Eur J Cancer B Oral Oncol. 1994;30:374–6.
Sturgis EM, Potter BO. Sarcomas of the head and neck region. Curr Opin Oncol. 2003;15:239–50.
Carrle D, Bielack SS. Current strategies of chemotherapy in osteosarcoma. Int Orthop. 2006;30:445–50.
Fernandes R, Nikitakis NG, Pazoki A, Ord RA. Osteogenic sarcoma of the jaw: a 10-year experience. J Oral Maxillofac Surg. 2007;65:1286–91.
Thiele OC, Freier K, Bacon C, Egerer G, Hofele CM. Interdisciplinary combined treatment of craniofacial osteosarcoma with neoadjuvant and adjuvant chemotherapy and excision of the tumour: a retrospective study. Br J Oral Maxillofac Surg. 2008;46:533–53.
Kassir RR, Rassekh CH, Kinsella JB, Segas J, Carrau RL, Hokanson JA. Osteosarcoma of the head and neck: meta-analysis of nonrandomized studies. Laryngoscope. 1997;107:56–60.
Colville RJ, Charlton F, Kelly CG, Nicoll JJ, McLean NR. Multidisciplinary management of head and neck sarcomas. Head Neck. 2005;27:814–20.
DeLaney TF, Park L, Goldberg SI, Hug EB, Liebsch NJ, Munzenrider JE, et al. Radiotherapy for local control of osteosarcoma. Int J Radiat Oncol Biol Phys. 2005;61:492–8.
Therasse P, Arbuck SG, Eisenhauer EA, et al. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst. 2000;92:205–16.
Cancer Therapy Evaluation Program, Common Terminology Criteria for Adverse Events, Version 3.0, DCTD, NCI, NIH, DHHS. 2003. (http://ctep.cancer.gov), Publish date 9 Aug 2006. Accessed 24 Jul 2014.
Panizzoni GA, Gasparini G, Clauser L, Barasti P, Pozza F, Curioni C. Osteosarcoma of the facial bones. Ann Oncol. 1992;3:S47–50.
Doval DC, Kumar RV, Kannar V, Sabitha KS, Misra S, Vijay Kumar M, et al. Osteosarcoma of the jaw bones. Br J Oral Maxillofac Surg. 1997;35:357–62.
Granowski-LeCornu M, Chuang SK, Kaban LB, August M. Osteosarcoma of the jaws: factor influencing prognosis. J Oral Maxillofac Surg. 2011;69:2368–75.
Herrmann A, Zoller J. Clinical features and treatment of osteogenic sarcoma of the jaws. Dtsch Z Mund Kiefer Gesichtschir. 1990;14:180–6.
Granados-Garcia M, Luna-Ortiz K, Castillo-Oliva HA, Villavicencio-Valencia V, Herrera-Gómez A, Mosqueda-Taylor A, et al. Free osseous and soft tissue surgical margins as prognostic factors in mandibular osteosarcoma. Oral Oncol. 2006;42:172–6.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ferrari, D., Codecà, C., Battisti, N. et al. Multimodality treatment of osteosarcoma of the jaw: a single institution experience. Med Oncol 31, 171 (2014). https://doi.org/10.1007/s12032-014-0171-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-014-0171-9