Abstract
We investigated the efficacy and safety of a new second-line chemotherapy of combining folinic acid, 5-fluorouracil and irinotecan (FOLFIRI) with both panitumumab and bevacizumab to treat patients with metastatic colorectal cancer (mCRC). Patients with mCRC and unsuccessful previous oxaliplatin-based chemotherapy were included in the study. The FOLFIRI arm was given FOLFIRI only. The FOLFIRI+PB arm was given panitumumab (3 mg/kg) and bevacizumab (3 mg/kg) plus FOLFIRI every other week. Between 2009 and 2013, 155 and 137 patients were included in the FOLFIRI arm and FOLFIRI+PB arm, respectively. The response rate was 40.1 % for FOLFIRI+PB arm versus 30.1 % for FOLFIRI arm. The disease-controlled rate in FOLFIRI+PB arm was improved to 62.2 from 50.2 % in FOLFIRI arm. The median overall survival was 13.9 months in FOLFIRI+PB arm as compared to 10.7 months in FOLFIRI arm. A series of adverse events were comparable between two arms, whereas some of the antibody therapy-associated toxicities were observed in FOLFIRI+PB arm. The new strategy of combining panitumumab and bevacizumab with FOLFIRI as second-line chemotherapy for patients with mCRC is safe and feasible.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Metastatic colorectal cancer (mCRC) is one of the leading causes of death in patients with colorectal cancer [1, 2]. The most efficient way to treat patients with mCRC is chemotherapy with various choices of chemotherapy regimens such as antimetabolite 5-fluorouracil (5-FU), leucovorin, oxaliplatin and folinic acid, 5-fluorouracil and irinotecan (FOLFIRI) [3–5].
Recently, the application of targeted reagents, including panitumumab, a human monoclonal antibody against epidermal growth factor receptor (EGFR) and bevacizumab, another human monoclonal antibody against vascular endothelial growth factor (VEGF), had shown improved prognosis in patients with mCRC [6–10]. However, the clinic results also revealed that treatments of biologically targeted compounds were often associated with their own limitations, or lacking sufficient data on clinical outcomes. For panitumumab, a randomized phase III clinical trial demonstrated that panitumumab with FOLFIRI, as compared to FOLFIRI alone, was efficient in improving the rate of progression-free survival as second-line therapy for patients with mCRC [11]. However, the same study also showed that panitumumab was ineffective in improving overall survival rate [11]. In addition, studies demonstrated that panitumumab was only effective in treating patients with wild-type KRAS tumors [8, 12]. In the case of bevacizumab, while it has been well recognized that the combination treatment of bevacizumab and FOLFIRI was an effective first-line treatment for patients with advanced CRC [13], more details are need to address its efficacy and patient outcomes, while it was used as a second-line therapy [14].
Between December 2009 and November 2013, we designed a new second-line chemotherapy, combining two regimens, panitumumab and bevacizumab with FOLFIRI (FOLFIRI+PB), to treat patients with mCRC at the First Affiliated Hospital of Zhejiang University School of Medicine, one of the largest gastrointestinal oncology centers in China. The aim of the study was to evaluate the safety and efficacy of FOLFIRI+PB after failure of first-line treatment of oxaliplatin or 5-FU in the clinical practice.
Patients and methods
Patients
Patients were included if they were ≥18 years of age, with Eastern Cooperative Oncology Group (ECOG) performance status of 0, 1, 2, with a diagnosis of adenocarcinoma of the colon or rectum, or a diagnosis of mCRC with lesion according to RECIST (version 1.1) [15]. In addition, to be qualified to receive second-line therapy, patient had undergone oxaliplatin plus 5-FU-based first-line chemotherapy, but re-diagnosed with disease relapse and progression in 6 months.
Patients were excluded if they had received prior panitumumab or bevacizumab therapy, hormonal therapy, immunotherapy, or major surgery (within 4 weeks) or radiotherapy (within 2 weeks).
The study protocol was performed in accordance with the Declaration of Helsinki and Good Clinical Practice Guidelines. All patients provided informed consent. In addition, the ethics committee at the First Affiliated Hospital of Zhejiang University School of Medicine (Hangzhou, China) reviewed and approved all clinical procedures included the present study.
Study design and treatment schedule
Patients were randomly divided into two arms. The patients in the FOLFIRI+PB arm were given 3 mg/kg panitumumab, 3 mg/kg bevacizumab plus FOLFIRI, whereas the patients in the FOLFIRI arm were given FOLFIRI alone, every 2 weeks. Panitumumab and bevacizumab were initially administrated by a 60-min infusion before chemotherapy. If the initial administration was tolerated by patients, the subsequent infusions would be conducted every 30 min. Patients in both arms received FOLFIRI on day one, including 180 mg/m2 irinotecan, 200 mg/m2 l-leucovorin and FU 400 mg/m2 IV bolus by intravenous (IV) infusion on day 1, followed by 2,400 mg/m2 continuous infusion in day 1 and 2. Patients received chemotherapy until disease progression or intolerability.
Efficacy of regimen was examined by investigators of the current study, as well as an independent experienced radiologist on computed tomography (CT) or magnetic resonance imaging (MRI), according to a modification of Response Evaluation Criteria in Solid Tumors (RECIST) every 8 weeks. Patients were followed up on safety for at least 30 days, and on survival every 3 months after the last administration. Adverse events (AEs) were assessed during both treatment and follow-ups and graded using the National Cancer Institute Common Terminology Criteria for Adverse Events version 3.0.
Statistical analysis
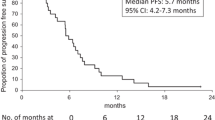
Response rate (RR) was the primary endpoint. Overall survival (OS), progression-free survival (PFS) and toxicity were secondary endpoints. Statistical analysis was conducted by SPSS software (version 13.0). OS and PFS were analyzed based on the Kaplan–Meier method, with a confidence interval (CT) of 95 %.
Results
Patients
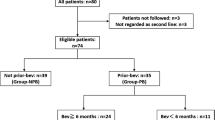
From December 2009 to November 2013, there were total of 292 mCRC patients registered in the present study, with 155 in FOLFIRI arm and 137 in FOLFIRI+PB arm, respectively. Baseline demographics and disease characteristics of the patients were shown in Table 1. The median ages were 58 years, ranging from 21 to 86 years, for FOLFIRI arm, and 61 years, ranging from 23 to 85 years for FOLFIRI+PB arm. For Eastern Cooperative Oncology Group performance status (ECOG PS), 122 (78.7 %) patients had grade 0–1 and 33 (21.2 %) patients had grade 2 in FOLFIRI arm. For the patients in FOLFIRI+PB arm, 98 (71.5 %) were graded between 0–1 and 39 (28.5 %) were graded at 2. The chemotherapy regimens used for the first-line treatment include FOLFOX (103 in FOLFIRI arm and 52 in FOLFIRI+PB arm, respectively) and XELOX (82 in FOLFIRI arm and 55 in FOLFIRI+PB arm, respectively).
Efficacy
The response rates for the patients in two arms were assessed (Table 2). Overall, the objective response (OR) rate was improved from 30.1 % in FOLFIRI arm to 40.1 % in FOLFIRI+PB arm. The disease control rate (DCR) was improved from 50.2 % in FOLFIRI arm to 62.2 % in FOLFIRI+PB arm. Also, the progressive disease (PD) rate was decreased from 45.2 % in FOLFIRI arm to 30.7 % in FOLFIRI+PB arm.
The survivals of patients were demonstrated in Fig. 1. For the primary analysis of progression-free survival (PFS), the median PFS was improved from 4.2 months in FOLFIRI arm to 5.5 months in FOLFIRI+PB arm. For the primary analysis of overall survival (OS), the median OS was improved from 10.7 months in FOLFIRI arm to 13.9 months in FOLFIRI+PB arm.
Safety
Grade 3 and 4 AEs for the patients in two arms were shown in Table 3. The total incidence rates of grade 3 and 4 AEs were 80.0 % for the patients in FOLFIRI+PB arm, and 52.6 % for the patients in FOLFIRI arm, respectively. Also, the patients in FOLFIRI+PB arm experienced more incidences of antibody treatment-associated AEs, than the patients in FOLFIRI arm, including 12.9 versus 1.5 % for hypertension, 11.6 versus 0 % for bleeding and 9.0 versus 1.5 % for proteinuria.
Discussions
Our study presented the clinical data of a novel second-line chemotherapy to treat patients with mCRC. We combined FOLFIRI with two additional human monoclonal antibodies, panitumumab (P) and bevacizumab (B), targeting both the ligand of VEGF and the receptor of EGFR. The results of our study showed improved prognosis in patients treated with FOLFIRI+PB, as compared to those treated with FOLFIRI alone.
First, we showed that the clinical outcomes of FOLFIRI alone treatment were very comparable to those in previous studies using traditional chemotherapy regimens, including an overall response rate ranging from ~20 to ~50 %, or an overall survival ranging from 7 to 10 months [3, 4, 16, 17]. These results demonstrated that ethnic variances were unlikely to cause differences in chemotherapy outcomes, as Chinese population in the present study showed similar outcomes as those of western populations in previous studies.
Second, we demonstrated that the clinical outcomes were significantly improved in the patients received FOLFIRI+PB treatment, as compared to FOLFIRI alone treatment. For example, the response rate was increased to 40.1 % (vs. 30.1 %), disease-controlled rate was increased to 62.2 % (vs. 50.2 %), and the median overall survival was increased to 13.9 months (vs. 10.7 months) in patients treated with FOLFIRI+PB (vs. FOLFIRI alone). Those results strongly suggested that combining two targeted regimens of panitumumab and bevacizumab plus FOLFRI could very well be an effective second-line chemotherapy to treat patients with mCRC.
Third, since it is a new study with two different antibody regimens, patient safety was closely monitored in our study. As a precautious measurement, the intake of panitumumab or bevacizumab in the present study (3 mg/kg) was only partial the amount of those used in prior single-reagent chemotherapy (~6–10 mg/kg). Grade 3 and 4 adverse events were then measured and compared between patients treated with FOLFIRI+PB and FOLFIRI alone. As a result, we noticed that antibody-associated adverse events were mostly seen in the patients in FOLFIRI+PB arm. This result could be attributed to the additive effects of two antibodies in the present study, despite the fact that reduced amount were applied. Also, we noticed that the overall grade 3 and 4 adverse responses were moderate and tolerable in the patients treated with FOLFIRI+PB. This is very encouraging, as it suggested that combining two antibody regimens as second-line chemotherapy could be a safe choice to treat patients with mCRC. It may also suggest that more clinic data are needed to further define the safety profile to optimize the administration strategy of combining different regimens in treating mCRC patients.
Overall, the results of our study, for the first time, presented that combining panitumumab, bevacizumab plus FOLFIRI, was an effective and safe second-line chemotherapy strategy to treat patients with mCRC. The combinational chemotherapy may benefit patients with failed first-line therapy with traditional reagents, or even the patients with failed chemotherapy of single-targeted regimen such as panitumumab or bevacizumab. Future randomized, multi-center studies with large patients size would certainly help to further develop the combinational-targeted therapy to treat patients with mCRC.
References
Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010;60(5):277–300.
Huxley RR, Ansary-Moghaddam A, Clifton P, Czernichow S, Parr CL, Woodward M. The impact of dietary and lifestyle risk factors on risk of colorectal cancer: a quantitative overview of the epidemiological evidence. Int J Cancer. 2009;125(1):171–80.
Fuchs CS, Marshall J, Mitchell E, Wierzbicki R, Ganju V, Jeffery M, Schulz J, Richards D, Soufi-Mahjoubi R, Wang B, et al. Randomized, controlled trial of irinotecan plus infusional, bolus, or oral fluoropyrimidines in first-line treatment of metastatic colorectal cancer: results from the BICC-C Study. J Clin Oncol. 2007;25(30):4779–86.
Fuchs CS, Moore MR, Harker G, Villa L, Rinaldi D, Hecht JR. Phase III comparison of two irinotecan dosing regimens in second-line therapy of metastatic colorectal cancer. J Clin Oncol. 2003;21(5):807–14.
Roque IFM, Sola I, Martin-Richard M, Lopez JJ, Bonfill Cosp X. Second-line chemotherapy in advanced and metastatic CRC. Cochrane Database Syst Rev. 2009;2:CD00687.
Cohn AL, Shumaker GC, Khandelwal P, Smith DA, Neubauer MA, Mehta N, Richards D, Watkins DL, Zhang K, Yassine MR. An open-label, single-arm, phase 2 trial of panitumumab plus FOLFIRI as second-line therapy in patients with metastatic colorectal cancer. Clin Colorectal Cancer. 2011;10(3):171–7.
Stintzing S, Fischer von Weikersthal L, Decker T, Vehling-Kaiser U, Jager E, Heintges T, Stoll C, Giessen C, Modest DP, Neumann J, et al. FOLFIRI plus cetuximab versus FOLFIRI plus bevacizumab as first-line treatment for patients with metastatic colorectal cancer-subgroup analysis of patients with KRAS: mutated tumours in the randomised German AIO study KRK-0306. Ann Oncol 2012;23(7):1693–99.
Mitchell EP, Piperdi B, Lacouture ME, Shearer H, Iannotti N, Pillai MV, Xu F, Yassine M. The efficacy and safety of panitumumab administered concomitantly with FOLFIRI or Irinotecan in second-line therapy for metastatic colorectal cancer: the secondary analysis from STEPP (Skin Toxicity Evaluation Protocol With Panitumumab) by KRAS status. Clin Colorectal Cancer. 2011;10(4):333–9.
Hurwitz HI, Fehrenbacher L, Hainsworth JD, Heim W, Berlin J, Holmgren E, Hambleton J, Novotny WF, Kabbinavar F. Bevacizumab in combination with fluorouracil and leucovorin: an active regimen for first-line metastatic colorectal cancer. J Clin Oncol. 2005;23(15):3502–8.
Moriwaki T, Bando H, Takashima A, Yamazaki K, Esaki T, Yamashita K, Fukunaga M, Miyake Y, Katsumata K, Kato S, et al. Bevacizumab in combination with irinotecan, 5-fluorouracil, and leucovorin (FOLFIRI) in patients with metastatic colorectal cancer who were previously treated with oxaliplatin-containing regimens: a multicenter observational cohort study (TCTG 2nd-BV study). Med Oncol. 2012;29(4):2842–8.
Peeters M, Price TJ, Cervantes A, Sobrero AF, Ducreux M, Hotko Y, Andre T, Chan E, Lordick F, Punt CJ, et al. Randomized phase III study of panitumumab with fluorouracil, leucovorin, and irinotecan (FOLFIRI) compared with FOLFIRI alone as second-line treatment in patients with metastatic colorectal cancer. J Clin Oncol. 2010;28(31):4706–13.
Hocking CM, Price TJ. Panitumumab in the management of patients with KRAS wild-type metastatic colorectal cancer. Therap Adv Gastroenterol. 2014;7(1):20–37.
Petrelli F, Borgonovo K, Cabiddu M, Ghilardi M, Lonati V, Maspero F, Sauta MG, Beretta GD, Barni S. FOLFIRI-bevacizumab as first-line chemotherapy in 3500 patients with advanced colorectal cancer: a pooled analysis of 29 published trials. Clin Colorectal Cancer. 2013;12(3):145–51.
Beretta GD, Petrelli F, Stinco S, Cabiddu M, Ghilardi M, Squadroni M, Borgonovo K, Barni S. FOLFIRI+bevacizumab as second-line therapy for metastatic colorectal cancer pretreated with oxaliplatin: a pooled analysis of published trials. Med Oncol. 2013;30(1):486.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–47.
Tournigand C, Andre T, Achille E, Lledo G, Flesh M, Mery-Mignard D, Quinaux E, Couteau C, Buyse M, Ganem G, et al. FOLFIRI followed by FOLFOX6 or the reverse sequence in advanced colorectal cancer: a randomized GERCOR study. J Clin Oncol. 2004;22(2):229–37.
Muro K, Boku N, Shimada Y, Tsuji A, Sameshima S, Baba H, Satoh T, Denda T, Ina K, Nishina T, et al. Irinotecan plus S-1 (IRIS) versus fluorouracil and folinic acid plus irinotecan (FOLFIRI) as second-line chemotherapy for metastatic colorectal cancer: a randomised phase 2/3 non-inferiority study (FIRIS study). Lancet Oncol. 2010;11(9):853–60.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Xie, S., Han, G., Fan, Z. et al. Safety and efficacy of second-line treatment with folinic acid, 5-fluorouracil and irinotecan (FOLFIRI) in combination of panitumumab and bevacizumab for patients with metastatic colorectal cancer. Med Oncol 31, 35 (2014). https://doi.org/10.1007/s12032-014-0035-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-014-0035-3