Abstract
The purpose of this study was to assess the prognostic value of 18F-fluoro-2-deoxy-glucose positron emission tomography (FDG-PET) in therapy for non-small cell lung cancer (NSCLC) and to further analyze the possible risk factors contributing to overall survival (OS) and progression-free survival (PFS). We retrospectively analyzed fifty patients between June 2007 and June 2010 with NSCLC who underwent positron emission tomography/computed tomography. We examined the correlation of the maximum standardized uptake value (SUVmax) in FDG-PET of the primary tumor with other possible factors. The FDG uptake in the primary tumor was also compared for the different Union for International Cancer Control (UICC) staging groups and further correlation was analyzed. We divided the patients into two groups by the receiver operating characteristic curve of SUVmax: SUVmax < 5.45 (low-SUV) and ≥ 5.45 (high-SUV). The prognostic value of each parameter for OS and PFS was determined by using univariate and multivariate analysis. There were significant correlations between SUVmax and Tumor length, N stage, UICC stage, histologic differentiation (r = 0.298, 0.855, 0.345, 0.435). The comparison between the low- and high-SUV groups was evaluated. Statistically significant differences were found in the SUVmax of the primary tumors among different UICC staging groups, and the correlation between stages I–II and stages III–IV for OS and PFS was also statistically significant. Univariate analysis showed that performance status (PS-ZPS score), histologic differentiation, UICC stages, and SUVmax of the primary tumor were significantly associated with OS and PFS. Multivariate logistic analysis showed that histologic differentiation and SUVmax of primary tumor might be considered as significant predictive factors for OS and PFS in patients with NSCLC. Our results showed that there was a significant relationship between the SUVmax of the primary tumor and OS and PFS. FDG uptake by the primary tumor may be an independent outcome predictor for patients with NSCLC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 2012, lung cancer is still the most prevailing cancer worldwide, with an estimated 226,000 new cases and 160,000 deaths every year [1]. The prognosis of non-small lung cancer (NSCLC) remains poor despite recent improvements in diagnosis and treatment. As a molecular and quantitative imaging technique, positron emission tomography (PET)/computed tomography (CT) has been proven useful, especially in diagnosis and staging of lung cancer [2]. The standardized uptake value (SUV) is a quantified index of FDG uptake. Several studies have shown that FDG uptake reflects the metabolic activity of the patients with primary NSCLC which can be a prognostic factor [3]. The maximum standardized uptake value (SUVmax) was assigned to an abnormality in the primary tumor with the highest SUV. SUVmax could largely represent the malignant behavior of the tumor with a higher reproductivity; thus, SUVmax is more commonly used in current clinical practice. FDG-PET has been established as a functional imaging technique before treatment which plays an important role in predicting the treatment outcome for NSCLC patients.
In order to provide more information for clinical practice to predict the outcome of NSCLC, we analyzed the possible risk factors affecting overall survival (OS) and progression-free survival (PFS) and determined whether the quantitative degree of FDG uptake by the primary tumor is an independent predictor for the prognosis in NSCLC. This approach might also represent an independent factor to evaluate and predict outcome of patients with NSCLC.
Materials and methods
Patient enrollment
We retrospectively collected a total of 50 patients with non-small cell lung cancer in the study between June 2007 and June 2010. A whole-body scan of FDG-PET/CT was performed before treatment for all patients. All patients received neither chemotherapy nor radiation prior to FDG-PET/CT scan. The patients’ characteristics are shown in Table 1. The median age of the patients was 65 years old (age range 45–87 years old); 31 were male and 19 were female. As for histologic types, 25 were adenocarcinoma cases and 25 were squamous cell lung carcinoma cases. The median tumor length was 23 mm (range 5–79 mm). The 7th edition of the UICC (International Union Against Cancer) staging system was used for staging [4]. Written informed consents were obtained from all patients enrolled.
FDG-PET image acquisition
All patients fasted for at least 4 h before PET/CT examination. After confirmation of the serum glucose level (<1.4 g/L), patients were administered with an intravenous injection of FDG at 3.7–4.0 MBq/kg and then rested about 60 min before undergoing the body scan, as recommended for tumor PET imaging [5].
All patients underwent a PET/CT scan through the Hi-Rez Biograph 16 (Siemens Medical Solutions, Germany), which consisted of a high-resolution three-dimensional LSO PET scanner and a 16-row CT scanner. Based on our study protocols, the patients took a whole-body PET/CT scan from the skull base to the mid-thigh level. Low-dose CT (tube voltage 120 kV; effective tube current 30–250 mA; per tube rotation 0.5 s) was performed for attenuation correction and identifying the tumor’s precise anatomical location before PET acquisition. Immediately after CT, PET was performed in an identical transverse field of view with a section thickness of 5 mm and using 3 min per table position and three-dimensional acquisitions. Patients were allowed to take normal shallow respiration during the image acquisition procedure.
FDG-PET image analysis
PET images were reconstructed using an ICS Navigator with four iterations, eight subsets and a Gaussian filter (4.8 mm). A single-scatter simulation model was used for scatter correction [6]. Attenuation correction was performed based on the CT data. No post-reconstruction smoothing filter was used. The reconstructed spatial resolution was 5 mm in the center of the field of view.
For determination of the SUV, a cylindrical region of interest (ROI) was manually placed over the tumor site on the hottest trans-axial slice. The ROI for each SUV calculation was manually drawn around a focal increased FDG as small as possible on the transaxial image. The maximum SUV (SUVmax) within the ROI was used as the reference measurement. SUVs were calculated from the counts-per-pixel and normalized to body weight:
where injected activity was decay-corrected from the delay between injection and image acquisition.
Treatment
In our study, pursuant to NCCN Guidelines, for those patients who were rendered inoperable by personal factors or iatrogenic factors, precise radiotherapy was adopted alone for early-stage NSCLC. The total dose of the primary tumor ranged from 60 to 70 Gy (median 65 Gy) in stage I. We adopted synchronized chemoradiotherapy to treat stages II–III NSCLC. For synchronized chemotherapy regimen, radiotherapy and chemotherapy started at the same time: platinum-based doublet chemotherapy was adopted once every 3 weeks for 4–6 cycles; a total of 45–60 Gy was administered in radiotherapy based on patients’ general conditions in stages II–III NSCLC. For the stage IV lung cancer patients with PS scores exceeding 2, supportive treatment was used for palliative care. The platinum-based doublet first-line chemotherapy was given with PS scores below 2. We adopted single agent chemotherapy as PS equal to 2. Patients were treated with chemotherapy which was composed of 4–6 cycles. For some of the stage IV patients, radiotherapy was used for palliative care against primary focus or metastatic focus, for example, partial pain killing effect, etc., and radiotherapy dose was 30–45 Gy.
The regimen of all patients referred to NCCN guide, first-line chemotherapy regimens were implemented without second-line chemotherapy regimens, and all patients did not use targeted drug in order for more comparability among experimental subjects. The specific implementation was assessed by the patient’s performance status, lung function status and cardiac status. The follow-up time was measured from the date of ending the treatment. The observation end point is OS.
Statistical analysis
The SUVmax of the primary tumor was compared with the descriptive statistics, and the correlations between pairs of variables were evaluated by using Spearman’s rank correlation coefficient. The ROC curve was generated to assess the primary tumor SUVmax for lymph nodal metastases. The SUVmax values were divided into two groups using the threshold of primary tumor SUVmax chosen by the receiver operating characteristic (ROC) curve. The OS and PFS values were compared between the two groups using the Kaplan–Meier curve. The comparison of SUVmax with patients’ characteristics before treatment was evaluated by T test. To assess the effect of the patients’ characteristics and other prognostic factors on the outcome, we estimated the correlation between the SUVmax in the FDG-PET of the primary tumor, other prognostic factors (age, PS, UICC stage, histologic differentiation, and pathology), and OS and PFS using univariate and multivariate Cox regression analyses. The OS, PFS, and OS of patients with UICC stages I–IV were calculated by the Kaplan–Meier method from the date of initiation of treatment. All analyses were carried out using the SPSS 11.0. Statistical significance was defined as P < 0.05.
Results
The relations between SUVmax and other prognostic factors (age, tumor length, pathology, T stage, N stage, UICC stage, histologic differentiation) were shown in Table 2 and the correlation coefficients were obtained. Positive correlations were found between SUVmax and N stage (r = 0.855, P < 0.001), SUVmax and histologic differentiation (r = 0.435, P < 0.05), SUVmax and UICC stage (r = 0.345, P < 0.05) before treatment. For the primary tumors, no significant correlations were observed between SUVmax and age (r = 0.314, P = 0.24), SUVmax and tumor length (r = 0.298, P = 0.012), SUVmax and pathology (r = 0.173, P = 0.229), SUVmax and T stage (r = 0.105, P = 0.469).
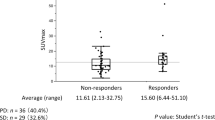
The median SUVmax in the FDG-PET images of the primary tumors was 9.82. The comparison of SUVmax with various patient characteristics before treatment was shown in Table 3. There was a significant difference between SUVmax of the primary tumor and N stage, UICC stage, and histologic differentiation (P = 0.000, 0.000, 0.003). We then divided the 50 patients into two groups according to ROC analysis of their SUVmax values: <5.45 (low-SUV) and ≥5.45 (high-SUV). The description of patient characteristics in the two groups (SUVmax <5.45 and ≥5.45) was distributed in Table 4. In the low- and high-SUV groups, N0 patients were 15 and 2; N1-3 patients were 1 and 32; UICC stages I–II patients were 10 and 3; UICC stages III–IV patients were 6 and 31; patients with high and moderate histologic differentiation were 16 and 9; patients with poor histologic differentiation were 0 and 25. The OS and PFS of the two groups were shown in Fig. 1. Significant differences between the two groups (stages I–II and stages III–IV) were found in SUVmax (P = 0.000). The OS, PFS, and the comparison in stages I, II, III, and IV in OS were shown, respectively in Fig. 2.
The results of the univariate analysis were shown in Table 5: significant differences were revealed between the low- and high-SUV groups in OS and PFS (P = 0.001, 0.0005). The SUVmax, ZPS, histologic differentiation, and UICC stage were significantly associated with OS and PFS. The results of the multivariate analysis were shown in Table 6: SUVmax was significantly associated with OS (OR = 4.21, P = 0.001) and PFS (OR = 3.80, P = 0.001). Other characteristics were less associated with OS and PFS than SUVmax.
Discussion
In our study, the SUVmax of the primary tumor was significantly correlated with tumor length, N stage, and UICC stage before treatment. And our study showed that there was a significant relationship between the SUVmax of the primary tumor and the pathologic N stage of NSCLC. Our results are consistent with those of Meng [7]. The mechanism may be interpreted as that FDG is avidly mainly taken up by tumor cells because cancer tissue consumes a large amount of glucose as an energy source [8], and the malignant cells have an altered metabolic activity with increased uptake of FDG. Tumor FDG uptake could be affected by cell differentiation, proliferative rate potential, microvessel density, and hypoxia, which are all consistent with the biological behavior of malignant cells [9, 10]. The higher the malignancy is, the greater the probability of lymph node metastasis will be, which leads to worse prognosis. A multicenter study concluded that higher SUVmax was associated with higher tumor invasion and lymph node metastasis where patients whose lung cancer showed high 18F-FDG uptake which had a 4.46- to 7.43-fold higher risk of intratumoral lymphatic vessel invasion and lymph node metastases after multivariate adjustment than those whose lung cancer showed low to moderate 18F-FDG uptake [11].
The ROC curve, used to determine the optimal cutoff value of SUVmax, was generated to assess the relationship between SUVmax and lymph node metastases (with 5.45 as the threshold), which showed a quite high sensitivity (93.9 %) and high specificity (82.4 %). In other studies, various cutoff SUV values have been used, ranging from 2.5 to 7 [12–22]. It is difficult to define an arbitrary cutoff value due to differences in patient characteristics, use of different protocols, and many other factors such as described above.
Statistical recordings of OS and PFS witnessed significant differences between the group exceeding 5.45 and the one below 5.45. When the SUVmax of the primary tumor exceeds 5.45, the OS and PFS decrease. This result is similar to our finding with regard to relationship between SUV value and N stage, UICC stage and differentiation. Analysis of Table 3 indicates that in the group with SUV values below 5.4, those patients with tumor diameter less than 5 mm accounted for 93.75 %, those at stages I and II 68.75 %, and those without lymphatic metastasis 93.75 % (including patients at stages I and II). For the group with SUV values above 5.4, those patients with maximum tumor diameter higher than 5 mm covered 97.05 % of the presence of higher T stage, N stage, and UICC stage but with mainly lower differentiated degrees.
Many studies have indicated the usefulness of FDG-PET to predict the prognosis for NSCLC patients. An European meta-analysis suggested that SUV in primary tumor before therapy had prognostic value for NSCLC [3, 23]; Higashi et al. investigated relationship between SUV and postoperative recurrence for 57 patients with resectable NSCLC through univariate analysis, reporting that patients with SUV values <5.0 outdid those with SUV values >5.0 in disease-free survival which was especially true for stage I patients (patients with SUV values <5.0 at this stage had 88 % of expected 5-year survival rate while those with SUV values >5.0 at the same stage only had 17 % of 5-year survival rate). Multivariate analyses confirmed that SUV was the most important independent prognostic factor for disease-free survival in the postoperation period [24].
Through univariate and multivariate analyses, our study found that SUVmax of the primary tumor showed statistical significance, suggesting that the FDG uptake in the primary tumor was an independent predictor for NSCLC patients (with the highest OR in SUVmax, OR = 5.13 in univariate survival analyses and OR = 4.21 in multivariate survival analyses: both are higher than those of other factors), which can be used to reflect patients’ prognosis and OS. We also found the same pattern in the PFS. The mechanism underlying this phenomenon may be explained as below: FDG-PET imaging relies on the Warburg effect, namely that cancer cells have the fundamental property of switching to anaerobic glycolysis despite of the presence of adequate oxygenation, an effect mediated in part by a hypoxia-inducible transcription factor (HIF-1) [25, 26]. HIF-1 can upregulate not only GLUT-1 and hexokinase to increase FDG uptake, but also other biological processes to promote increased tumor aggression and treatment resistance [27]. On the basis of our findings that the SUV for primary tumor predicted both local tumor control and distant metastasis, we hypothesize that tumor glucose metabolism is related to the metastatic potential of the tumor. Several investigators have also speculated that SUV is correlated with cellular proliferation or biological factors such as Ki-67, proliferating cell nuclear antigen, Glut-1, and hexokinase [28, 29].
To sum up, SUVmax may be related to tumor size, differentiation, pathological pattern, or even lymph node or distant metastasis related tumor cell proliferation and multiplication and other biological factors. Use of SUVmax for NSCLC patients have following strengths: on the one hand, SUVmax can substantially reflect malignancy degree of the tumor at molecular metastasis level by identifying individual differences of NSCLC in glycometabolism; on the other hand, SUVmax can make an objective evaluation of staging and prognosis for each NSCLC patient, provide reliable clinical basis for personalized treatment, and act as a predictive index for disease control and survival. However, it should be noted that some researches have reported results different from ours, showing that tumor size and histologic differentiation have no significant difference on multivariate analysis.
However, this prognostic value does not seem to be so clear in advanced stage lesions [30]. Hoang et al. [31] found that FDG uptake in the primary tumor of patients with advanced stage NSCLC had no prognostic value. Kieninger et al. [32] analyzed prognostic significance for early lung cancer and held that SUVmax was not an independent predictive index for OS, despite its relations with tumor staging, differentiation and other prognostic factors. Our study mainly involved stages III and IV patients (38 patients, 76 % of all patients) while stages II and III cases were in the majority, so all results and conclusions need to be further tested and verified in more experiments. Furthermore, as a semiquantitative parameter of glucose uptake, SUVmax is subject to various factors such as patient size, ROI definition, the partial-volume effect, image resolution, reconstruction methods, noise, interval time between tracer injection and imaging, attenuation correction, normalization factor, and plasma glucose level.
In conclusion, the results of our study suggest that the SUVmax from FDG-PET of primary tumors is significantly associated with OS and PFS of NSCLC. For OS and PFS, SUVmax is an independent prognostic variable. FDG uptake by the primary tumor may have prognostic value for NSCLC. For patients with higher SUV values, more aggressive adjuvant treatments should be considered. SUVmax is readily amenable to clinical use due to its non-invasive nature and convenience.
References
Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62:10–29.
Boellaard R, O’Doherty MJ, Weber WA, et al. FDG PET and PET/CT: EANM procedure guidelines for tumour PET imaging: version 1.0. Eur J Nuclear Med Mol Imaging. 2010;37:181–200. doi:10.1007/s00259-009-1297-4.
Paesmans M, Berghmans T, Dusart M, et al. Primary tumor standardized uptake value measured on fluorodeoxyglucose positron emission tomography is of prognostic value for survival in non-small cell lung cancer: update of a systematic review and meta-analysis by the European Lung Cancer Working Party for the International Association for the Study of Lung Cancer Staging Project. J Thorac Oncol. 2010;5:612–9.
Soussan M, Chouahnia K, Maisonobe JA, et al. Prognostic implications of volume-based measurements on FDG PET/CT in stage III non-small-cell lung cancer after induction chemotherapy. Eur J Nucl Med Mol Imaging. 2013;40:668–76.
Shankar LK, Hoffman JM, Bacharach S, et al. Consensus recommendations for the use of 18F-FDG PET as an indicator of therapeutic response in patients in National Cancer Institute Trials. J Nucl Med. 2006;47:1059–66.
Accorsi R, Adam LE, Werner ME, et al. Optimization of a fully 3D single scatter simulation algorithm for 3D PET. Phys Med Biol. 2004;49:2577–98.
Li M, Wu H, Zheng R, et al. Primary tumor PET/CT [18F] FDG uptake is an independent predictive factor for regional lymph node metastasis in patients with non-small cell lung cancer”. Cancer Imaging. 2012;12:566–72.
Strauss LG, Conti PS. The applications of PET in clinical oncology. J Nucl Med. 1991;32:623–48.
Bisdas S, Spicer K, Rumboldt Z. Whole-tumor perfusion CT parameters and glucose metabolism measurements in head and neck squamous cell carcinomas: a pilot study using combined positron-emission tomography/CT imaging. AJNR Am J Neuroradiol. 2008;29:1376–81.
Ganeshan B, Burnand K, Young R, et al. Dynamic contrast-enhanced texture analysis of the liver: initial assessment in colorectal cancer. Invest Radiol. 2011;46:160–8.
Higashi K, Ito K, Hiramatsu Y, et al. 18F-FDG uptake by primary tumor as a predictor of intratumoral lymphatic vessel invasion and lymph node involvement in non-small cell lung cancer: analysis of a multicenter study. J Nucl Med. 2005;46:267–77.
Sauter AW, Spira D, Schulze M, et al. Correlation between [18F]FDG PET/CT and volume perfusion CT in primary tumours and mediastinal lymph nodes of non-small-cell lung cancer. Eur J Nucl Med Mol Imaging. 2013;40:677–84.
Higashi K, Ueda Y, Arisaka Y, et al. 18F-FDG uptake as a biologic prognostic factor for recurrence in patients with surgically resected non-small cell lung cancer. J Nucl Med. 2002;43:39–45.
Jeong HJ, Min JJ, Park JM, et al. Determination of the prognostic value of [18F] fluorodeox yglucose uptake by using positron emission tomography in patients with non -small cell lung cancer. Nucl Med Commun. 2002;23:865–70.
Suzuki A, Xiao L, Hayashi Y, et al. Prognostic significance of baseline positron emission tomography and importance of clinical complete response in patients with esophageal or gastroesophageal junction cancer treated with definitive chemoradiotherapy. Cancer. 2011;117:4823–33.
Kato H, Nakajima M, Sohda M, et al. The clinical application of 18-F-fluorodeoxyglucose positron emission tomography to predict survival in patients with operable esophageal cancer. Cancer. 2009;115:3196–203.
Hong D, Lunagomez S, Kim EE, et al. Value of baseline positron emission tomography for predicting overall survival in patient with non metastatic esophageal or gastroesophageal junction carcinoma. Cancer. 2005;104:1620–6.
Swisher SG, Maish M, Erasmus JJ, et al. Utility of PET, CT, and EUS to identify pathologic responders in esophageal cancer. Ann Thorac Surg. 2004;78:1152–60.
Konski AA, Cheng JD, Goldberg M, et al. Correlation of molecular response as measured by 18-FDG positron emission tomography with outcome after chemoradiotherapy in patients with esophageal carcinoma. Int J Radiat Oncol Biol Phys. 2007;69:358–63.
Ishihara R, Yamamoto S, Iishi H, et al. Predicting the effects of chemoradiotherapy for squamous cell carcinoma of the esophagus by induction chemotherapy response assessed by positron emission tomography: toward PET-response-guided selection of chemoradiotherapy or esophagectomy. Int J Clin Oncol. 2012;17:225–32.
Yasuda T, Higuchi I, Yano M, et al. The impact of (18)F-fluorodeoxyglucose positron emission tomography positive lymph nodes on postoperative recurrence and survival in resectable thoracic esophageal squamous cell carcinoma. Ann Surg Oncol. 2012;19:652–60.
Wieder HA, Beer AJ, Lordick F, et al. Comparison of changes in tumor metabolic activity and tumor size during chemotherapy of adenocarcinomas of the esophagogastric junction. J Nucl Med. 2005;46:2029–34.
Berghmans T, Dusart M, Paesmans M, et al. Primary tumor standardized uptake value (SUVmax) measured on fluorodeoxyglucose positron emission tomography (FDG-PET) is of prognostic value for survival innon-sma ll cell lung cancer (NSCLC): a systematic review and meta-analysis (MA) by the European Lung Cancer Working Party for the IAS LC Lung Cancer Staging Project. J Thorac Oncol. 2008;3:6–12.
Higashi K, Ueda Y, Arisaka Y, et al. 18F-FDG uptake as a biologic prognostic factor for recurrence in patients with surgically resected non-small cell lung cancer. J Nucl Med. 2002;43:39–45.
Miles KA, Williams RE. Warburg revisited: imaging tumour blood flow and metabolism. Cancer Imaging. 2008;8:81–6.
Gillies RJ, Robey I, Gatenby RA. Causes and consequences of increased glucose metabolism of cancers. J Nucl Med. 2008;49(Suppl 2):24S–42S.
Vaupel P, Harrison L. Tumor hypoxia: causative factors, compensatory mechanisms, and cellular response. Oncologist. 2004;9(Suppl 5):4–9.
Vesselle H, Schmidt RA, Pugsley JM, et al. Lung cancer proliferation correlates with [F-18] fluorodeoxyglucose uptake by positron emission tomography. Clin Cancer Res. 2000;6:3837–44.
Bos R, van Der Hoeven JJ, van Der Wall E, et al. Biologic correlates of 18fluorode oxy glucose uptake in human breast cancer measured by positron emission tomography. J Clin Oncol. 2002;20:379–87.
Berghmans T, Paesmans M, Sculier JP. Prognostic factors in stage III non-small cell lung cancer: a review of conventional, metabolic and new biological variables. Ther Adv Med Oncol. 2011;3:127–38.
Hoang JK, Hoagland LF, Coleman RE, et al. Prognostic value of fluorine-18 fluorodeoxyglucose positron emission tomography imaging in patients with advanced stage non-small-cell lung carcinoma. J Clin Oncol. 2008;26:1459–64.
Kieninger AN, Welsh R, Bendick PJ, et al. Positron-emission tomography as a prognostic tool for early—stage lung cancer. Am J Surg. 2006;191:433–6.
Acknowledgments
This work was supported by China Postdoctoral Science Foundation (20080431411).
Conflict of interest
The authors have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
An-Na Tong and Shao-Rong Han have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Tong, AN., Han, SR., Yan, P. et al. Prognostic value of FDG uptake in primary inoperable non-small cell lung cancer. Med Oncol 31, 780 (2014). https://doi.org/10.1007/s12032-013-0780-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-013-0780-8