Abstract
The significance of KRAS in advanced colorectal cancer (CRC) treated with bevacizumab (B) is not well understood. We conducted a systematic review and pooled analysis of published trials with the aim to assess the predictive and prognostic role of KRAS status in patients treated with B. We performed a systematic search of PubMed, EMBASE, Web of Science, and Cochrane Register of Controlled Trials. The primary endpoints included objective response rate (RR), progression-free survival (PFS), and overall survival (OS). The odds ratio (OR) for RR and hazard ratios (HRs) were calculated or extracted by published data either using a fixed effect model or a random effect model. A total of 12 studies were included. A total of 2,266 patients were analysed (54 % were KRAS wt). The pooled RRs for KRAS wild-type (wt) versus mutated (mut) patients were 54.8 and 48.3 %, respectively (OR 1.42, P = 0.02). Median PFS was significantly longer in KRAS wt patients compared with that in KRAS mut patients (HR = 0.85; 95 % confidence interval (CI) 0.74–0.98; P = 0.02). Similarly, median OS was significantly better in wt KRAS patients compared with that in mut KRAS patients (HR = 0.65; 95 % CI 0.46–0.92; P = 0.01). This pooled analysis of 12 published studies shows that KRAS wt status is a good prognostic factor for B-based chemotherapy. Also, KRAS wt CRC is associated with a better RR with B plus chemotherapy than mut counterpart.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Clinical data have indicated that KRAS mutation is a negative prognostic marker because it was associated with a poorer outcome in advanced colorectal cancer (CRC) [1]. This finding is not consistent in all treatment settings. In fact, in patients treated with standard cytotoxic chemotherapies, KRAS is not a predictive marker for benefit or lack of benefit [2–6]. Conversely, a significantly better outcome is associated with KRAS wild-type (wt) compared with mutant (mut) status in patients with CRC treated with anti-epidermal growth factor receptor (EGFR) antibodies [7]. This means that KRAS status is a prognostic factor for these subjects because wt patients live longer compared with mut population. Also, KRAS wt condition is a good predictive factor because it is associated with better activity and outcome in patients treated with chemotherapy + cetuximab or panitumumab compared with chemotherapy alone in the metastatic stage. This is well exploited by CRYSTAL and OPUS pooled analysis that showed a better response rate (RR), progression-free survival (PFS), and overall survival (OS) for chemotherapy + cetuximab versus chemotherapy alone in KRAS wt-only patients [8].
Bevacizumab (B) is a recombinant humanized monoclonal antibody targeting the isoform A of vascular endothelial growth factor (VEGF-A). Therefore, it inhibits tumour angiogenesis, starving the tumour of blood and nutrients. It is indicated as first- or second-line therapy of advanced CRC, in combination with 5-fluorouracil-based chemotherapy, extending both PFS and OS compared with chemotherapy alone. Up until today, some biomarkers have been evaluated as predictive factors of B activity. Some of these are single nucleotide polymorphisms in the VEGF, circulating endothelial cells, hypertension, and microvessel density, but the results were inconclusive [9–15].
The predictive and prognostic value of KRAS in patients treated with the anti-angiogenetic agent B is apparently less strong. In fact, in the pivotal trial led by Hurwitz [16, 17], B added to irinotecan + fluorouracil and folinic acid (IFL) chemotherapy conferred a significant benefit in both RR and OS only in KRAS wt patients compared to mut ones; however, the magnitude of benefit was similar, even if not significant, to the mut population. Nevertheless, KRAS wt patients treated with IFL + B do not have a significantly better survival that their mut counterparts, so its prognostic significance is frail in this setting. Only in KRAS wt/BRAF wt, condition was OS better (HR = 0.51) than KRAS mut/BRAF mut patients when these subjects were treated with IFL + B [16]. The significance of this data is that not only KRAS but other drivers are crucial in the biology of this disease.
Overall, KRAS status appears to be a significant predictive and prognostic biomarker in patients treated with chemotherapy and anti-EGFR monoclonal antibodies, which are in fact approved only in KRAS wt patients, but, apparently, is not a strong predictor of activity nor a clear prognostic factor for survival in patients treated with chemotherapy + B.
So to verify this information comprehensively, we have performed a systematic review and pooled analysis of studies that report the outcome and efficacy of B-treated patients according to KRAS status, to obtain a more precise estimation of prognostic value of KRAS in patients treated with B as first-line treatment for metastatic CRC.
Materials and methods
Literature search
Systematic computerised searches of the PubMed, EMBASE, Web of Science, and The Cochrane Central Register of Controlled Trials (up to 30th March 2013) were performed. The following search terms were used: ‘colorectal cancer’ or ‘colorectal carcinoma’ or ‘colon cancer’ or ‘colon carcinoma’, and ‘KRAS’ and ‘bevacizumab’. The search was limited to human studies in the English language. Eligible studies that reported RR and/or PFS and/or OS stratified by KRAS mutation status in (at least 20) patients treated with chemotherapy + B as first-line chemotherapy were retrieved, and their bibliographies were checked for other relevant publications. When the same patient population was used in several publications, only the most recent, largest, or complete study was included in the meta-analysis. Studies were excluded if they included associated treatment with other targeted therapies or radiotherapy. So only B + chemotherapy alone arms were considered.
Data extraction
Information was carefully extracted from all eligible studies. The following data were collected from each study: first author’s name, year of publication, study designs, line of therapy, number of patients with KRAS mutation status available, study treatment, RR stratified by KRAS mutation status, and median PFS and OS stratified by KRAS mutation status and hazard ratio (HR) with 95 % confidence intervals (CIs) for PFS or OS.
Data extraction was done independently by two of the authors (AC and FP). Any disagreement was resolved by consensus. If these two authors could not reach a consensus, another author (SB) was consulted to resolve the dispute and a final decision was made by consensus.
The co-primary endpoints were RR, PFS, and OS in wt vs mut populations. The RR was defined as the sum of CR and PR. The correlation between KRAS mutations and RR was expressed as odds ratio (OR) for RR of wt KRAS patients versus mut KRAS patients. Thus, an OR >1 indicates a better RR for KRAS wt patients with B treatment, and an OR <1 corresponds to a worse RR for KRAS wt patients. The other endpoints were PFS and OS. The correlation between KRAS mutations and these endpoints was expressed as an HR of wt KRAS patients over mut KRAS patients. HRs and 95 % CIs were estimated directly or indirectly from the reported data. When HR and 95 % CI were not reported in a publication, they were computed from other available data, as previously described [18–20]. Thus, an HR more than 1 indicates that KRAS wt is associated with shorter PFS and OS, and a HR less than 1 indicates that KRAS wt is associated with longer PFS and OS. The correlation between KRAS mutations and efficacy of B therapy was measured by OR and HR with 95 % CI.
A fixed effects or random effects (weighted with inverse variance) model and the Mantel–Haenszel’s (M–H) method were utilized to combine and weight the individual studies. The Cochran Q test, with a predefined significance threshold of 0.1, was used to assess statistical heterogeneity among studies. The assumption of homogeneity was considered invalid for P values <0.1; in this case, summary estimates were reported from the random effect models. To establish the effect of clinical heterogeneity among studies on meta-analyses conclusions, subgroup analyses were conducted by study designs (phase III vs others) and type of drug (oxaliplatin vs irinotecan-based). Begg’s funnel plots and Egger’s test were used to assess publication bias. Funnel plot asymmetry was assessed by the method of Egger’s linear regression test, a linear regression approach to measure funnel plot asymmetry on the natural logarithm scale of the OR. The significance of the intercept was determined by the t test as suggested by Egger (P < 0.05 was considered representative of statistically significant publication bias). If publication bias existed, the Duval and Tweedie nonparametric ‘trim and fill’ method was used to adjust it.
All statistical analyses were performed with Review Manager 5.1 (Review Manager (RevMan) [computer program] version 5.1; Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2008) and Comprehensive Meta-Analysis software (version 2.2.064; July 27, 2011).
Results
Based on our search criteria, 12 studies were identified from a total of n = 263 screened (Fig. 1) [16, 17, 21–31]. A total of 2,266 patients were used in the pooled analyses. Table 1 lists the studies identified and their main characteristics. Of the 12 studies, sample sizes of the analysed KRAS population ranged from 45 to 425. Two of these studies were retrospective case series, while 10 of them were prospective studies (6 were phase III trials, 1 randomized phase II and 3 single arm phase II studies). The patients of 5 studies received oxaliplatin-based chemotherapy only; of 1 study, irinotecan-based chemotherapy; of 3 studies, oxaliplatin or irinotecan regimens; of 2 studies, triplets combinations; and of 1 study, capecitabine ± mytomicin C regimens. The rate of KRAS wt status was 54 %. In the trial of Bruera et al., the only comparison was between KRAS wt and KRAS with c.35 G>A mutation. Data include PFS and OS derived from n = 103 (wt + mut) patients treated in capecitabine alone arm in AGITG MAX trial, because these patients were included in the prognostic analysis according to KRAS status.
Overall response rate
The pooled RR of patients with mut KRAS was 48.3 %, whereas the RR of patients with wt KRAS was 54.8 % (n = 9 trials with data available). When the wt KRAS patients were compared with the mut KRAS patients, the OR was 1.42, (95 % CI 1.05–1.92, P = 0.02; P for heterogeneity 0.06, I 2 = 46 %, random effect model; Fig. 2). In the subgroup analysis by phase III or other designs, the pooled OR was 1.29 (95 % CI 0.91–1.84; P = 0.16) and 2.74 (95 % CI 1.5–4.99; P = 0.001), respectively. In the subgroup analysis by oxaliplatin versus irinotecan-based treatment, the pooled OR was 1.34 (95 % CI 0.83–2.17; P = 0.23) and 1.74 (95 % CI 1.01–3.02; P = 0.05).
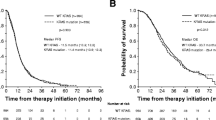
Progression-free survival
Data for KRAS mutations and PFS were reported in all studies. However, only seven studies provided data to extract or calculate HRs with 95 % CI for PFS. The median of PFS in KRAS wt and mut patients was 11.8 and 9.42 months, respectively. KRAS wt status is associated with a better PFS (HR = 0.85; 95 % CI 0.74–0.98; P = 0.02; Fig. 3) than KRAS mut CRCs, with low heterogeneity between studies (P = 0.31; I 2 = 16 %; fixed effect model). In phase III trial only (n = 5 trials), HR was 0.87 (P = 0.05), while in a phase II trial, HR was 0.5 (P = 0.038); in oxaliplatin trials (n = 4), HR was 0.85 (P not significant). In one irinotecan-based trial, HR for PFS was not significant.
Overall survival
Data for KRAS mutations and OS were reported in nine studies (in one trial, median OS was not reached in B arm, so this comparison was not included). However, only six studies provided data to extract or calculate HRs with 95 % CI for OS. The median of OS in KRAS mut or wt patients was 20.2 and 24.5 months, respectively. KRAS wt status is associated with a better OS (HR = 0.65; 95 % CI 0.46–0.92; P = 0.01; Fig. 4) than KRAS mut CRCs, with high heterogeneity between studies (P = 0.008; I 2 = 68 %; random effect model). In phase III trials only (n = 4 trials), HR was 0.76 (P = 0.001), while in a phase II trial, HR was 0.26 (P = 0.0001); in oxaliplatin trials (n = 3), HR was 0.63 (P not significant). In one irinotecan-based trial, HR for OS was not significant.
Publication bias
Begg’s funnel plot for OR of RR is reported in Fig. 5. Begg’s and Mazumadar’s test (P = 0.72) and Egger’s test (P = 0.30) confirmed the funnel plot symmetry in the comparison of the OR of RR in mut KRAS patients versus the wt KRAS patients in overall studies. Publication biases were not found for KRAS status and PFS by both Begg’s and Egger’s tests. The same is true for OS analysis.
Analyses with and without the ‘trim and fill’ method did not draw remarkably different conclusions. Using trim and fill, the imputed point estimate is 1.28183 for OR of RR (95 % CI 0.96–1.69). Conversely, for PFS and OS analyses, the results remained unchanged after trim and fill analysis.
Discussion
In the era of personalised medicine, tailored therapies have been even more developed in oncology. Such examples are crizotinib in ALK + and erlotinib or gefitinib in EGFR mut lung cancers; and cetuximab and panitumumab in KRAS wt CRCs and trastuzumab in HER2 + breast cancers. In these cases, in fact, the presence of a specific molecular driver is considered a positive predictive factor of response to some approved targeted therapies. Other clinical or pathological biomarkers are considered, conversely, prognostic of outcome (OS) of disease, independently of the treatment performed. Among these in CRC are locoregional extent of disease; conversely, KRAS and other molecular markers are category III prognostic factors that are those not yet sufficiently validated to determine their prognostic value.
The monoclonal antibody B induces disruption of abnormal microvasculature and thus potentially permits regression of neoplastic disease in solid tumours, when coupled with cytotoxics drugs, offering a benefit in RR and OS in several diseases, such as CRC, breast cancer, and lung cancer. As for now, in advanced CRC, no subgroup of patients has been considered more or less sensitive to treatment with B, even if several clinical or molecular biomarkers have been extensively investigated [9–15, 32, 33].
We have demonstrated, for the first time, that KRAS wt status is associated with better response to B-based chemotherapy and represents a positive prognostic factor for patients with advanced CRC treated in the first-line setting.
In fact, RR is higher, and the risk of death is 35 % reduced in KRAS wt than in mut patients with B as first-line therapy for advanced CRC. The information is useful for both the clinician and the patients. First, we are aware that prognosis of KRAS mut CRC is fairly poor compared with wt ones, even with the addition of B; and second, in wt patients, the higher RR obtained with chemotherapy + B could be useful in some circumstances as during an attempt to de-bulk distant metastases. In this case, in fact, an RR of about 55 % is very similar to that obtained in wt patients with chemotherapy + cetuximab, that is now considered one the standard conversion therapies for potentially operable liver metastases [8]. The reason why KRAS wt patients have an improved survival and obtain relatively better objective responses when treated with B is relatively inexplicable. The hypothesis most often contemplated is that mutations in KRAS, but also BRAF and TP53, have been shown to result in an increased VEGF signalling as well as in reduced sensitivity to anti-angiogenic drugs in pre-clinical models [34–36]. In CRC, it is also well known that OS is especially driven by post-progression survival, that is, the time elapsed from the end of first-line therapy to death. In this case, a wt KRAS status could have permitted the use of anti-EGFR agents in later lines of therapy and so a better final outcome [37].
Up to today, the current literature tells us that no candidate for first-line chemotherapy can be excluded from or selected for B on the basis of clinical or molecular biomarkers. In fact, no predictive factors have been clearly demonstrated associated with a better efficacy with B. Recently, Hurwitz et al. [15] demonstrated that in six phase III studies, early increase of blood pressure was neither predictive of clinical benefit from B nor prognostic for the course of the disease. Conversely, in the study AVF2107 g, an early increase of blood pressure was associated with a longer PFS and OS in B group, so it was a potential prognostic but not predictive factor. Scartozzi et al. [32] come to similar conclusions. Among molecular biomarkers, BRAF is now considered more prognostic than predictive as analysis of MAX trial shows [24]. Other data indicate a predictive value for some circulating factors, such as an increase in VEGF, a decrease in VEGF receptor-2 or circulating endothelial cells, some tissue biomarkers such microvessel density, or certain polymorphisms affecting the VEGF pathway. However, data are still partially inconclusive [9–15].
This study level meta-analysis has some limitations but also some strengths. First, this is a pooled analysis that aggregates data derived from published papers, and so, with the lack of individual patient information, any adjustment for clinical and pathological variables was not possible. Second, analysis of mutation has not taken into account other molecular biomarkers such as BRAF (or PI3KCA) for example. In this case, however, BRAS wt status could have ameliorated the OS analysis more than the RR as MAX trial analysis showed [24]. Third, only half trials permitted to extrapolate or calculate the HRs with 95 % CI for PFS and OS, but the results showed low-to-moderate heterogeneity and no evident biases, and remained unchanged after inclusion of larger phase III trials only. However, our analysis derives from analysis of 12 trials, of which half were phase III, for a total of more than 2,000 patients with known KRAS status, and it is the largest analysis ever performed to assess the prognostic value of KRAS in patients treated with B for advanced CRC. In these patients, in fact, wt KRAS status seems associated with a better RR (about 6–7 % higher) and leads to an improved survival of about 4 months, compared to their mut counterparts.
Other biomarkers will probably be entered in clinical trials in the future but will need necessarily a prospective validation. Some of these, such as LDH, are now being considered an ideal candidate for further prospective development [34].
In the meantime, wt KRAS status can be considered a good predictive factor for response and outcome in patients treated with chemotherapy + B in clinical practice.
References
Ren J, Li G, Ge J, Li X, Zhao Y. Is K-ras gene mutation a prognostic factor for colorectal cancer: a systematic review and meta-analysis. Dis Colon Rectum. 2012;55(8):913–23.
Esteller M, González S, Risques RA, et al. K-ras and p16 aberrations confer poor prognosis in human colorectal cancer. J Clin Oncol. 2001;19:299–304.
Cerottini JP, Caplin S, Saraga E, Givel JC, Benhattar J. The type of K-ras mutation determines prognosis in colorectal cancer. Am J Surg. 1998;175(3):198–202.
Samowitz WS, Curtin K, Schaffer D, Robertson M, Leppert M, Slattery ML. Relationship of Ki-ras mutations in colon cancers to tumor location, stage, and survival: a population-based study. Cancer Epidemiol Biomarkers Prev. 2000;9(11):1193–7.
Andreyev HJ, Norman AR, Cunningham D, et al. Kirsten ras mutations in patients with colorectal cancer: the ‘RASCAL II’ study. Br J Cancer. 2001;85:692–6.
Ahnen DJ, Feigl P, Quan G, et al. Ki-ras mutation and p53 overexpression predict the clinical behavior of colorectal cancer: a Southwest Oncology Group study. Cancer Res. 1998;58:1149–58.
Qiu LX, Mao C, Zhang J, Zhu XD, Liao RY, Xue K, Li J, Chen Q. Predictive and prognostic value of KRAS mutations in metastatic colorectal cancer patients treated with cetuximab: a meta-analysis of 22 studies. Eur J Cancer. 2010;46(15):2781–7.
Bokemeyer C, Van Cutsem E, Rougier P, Ciardiello F, Heeger S, Schlichting M, Celik I, Köhne CH. Addition of cetuximab to chemotherapy as first-line treatment for KRAS wild-type metastatic colorectal cancer: pooled analysis of the CRYSTAL and OPUS randomised clinical trials. Eur J Cancer. 2012;48(10):1466–75.
Hansen TF, Christensen Rd, Andersen RF, Garm Spindler KL, Johnsson A, Jakobsen A. The predictive value of single nucleotide polymorphisms in the VEGF system to the efficacy of first-line treatment with bevacizumab plus chemotherapy in patients with metastatic colorectal cancer: results from the Nordic ACT trial. Int J Colorectal Dis. 2012;27(6):715–20.
Pohl M, Werner N, Munding J, Tannapfel A, Graeven U, Nickenig G, Schmiegel W, Reinacher-Schick A. Biomarkers of anti-angiogenic therapy in metastatic colorectal cancer (mCRC): original data and review of the literature. Z Gastroenterol. 2011;49(10):1398–406.
Jubb AM, Hurwitz HI, Bai W, Holmgren EB, Tobin P, Guerrero AS, Kabbinavar F, Holden SN, Novotny WF, Frantz GD, Hillan KJ, Koeppen H. Impact of vascular endothelial growth factor-A expression, thrombospondin-2 expression, and microvessel density on the treatment effect of bevacizumab in metastatic colorectal cancer. J Clin Oncol. 2006;24(2):217–27.
Malka D, Boige V, Jacques N, Vimond N, Adenis A, Boucher E, Pierga JY, Conroy T, Chauffert B, François E, Guichard P, Galais MP, Cvitkovic F, Ducreux M, Farace F. Clinical value of circulating endothelial cell levels in metastatic colorectal cancer patients treated with first-line chemotherapy and bevacizumab. Ann Oncol. 2012;23(4):919–27.
Ronzoni M, Manzoni M, Mariucci S, Loupakis F, Brugnatelli S, Bencardino K, Rovati B, Tinelli C, Falcone A, Villa E, Danova M. Circulating endothelial cells and endothelial progenitors as predictive markers of clinical response to bevacizumab-based first-line treatment in advanced colorectal cancer patients. Ann Oncol. 2010;21(12):2382–9.
Österlund P, Soveri LM, Isoniemi H, Poussa T, Alanko T, Bono P. Hypertension and overall survival in metastatic colorectal cancer patients treated with bevacizumab-containing chemotherapy. Br J Cancer. 2011;104(4):599–604.
Hurwitz HI, Douglas PS, Middleton JP, Sledge GW, Johnson DH, Reardon DA, Chen D, Rosen O. Analysis of early hypertension and clinical outcome with bevacizumab: results from seven phase III studies. Oncologist. 2013;18(3):273–80.
Ince WL, Jubb AM, Holden SN, Holmgren EB, Tobin P, Sridhar M, Hurwitz HI, Kabbinavar F, Novotny WF, Hillan KJ, Koeppen H. Association of k-ras, b-raf, and p53 status with the treatment effect of bevacizumab. J Natl Cancer Inst. 2005;97(13):981–9.
Hurwitz HI, Yi J, Ince W, Novotny WF, Rosen O. The clinical benefit of bevacizumab in metastatic colorectal cancer is independent of K-ras mutation status: analysis of a phase III study of bevacizumab with chemotherapy in previously untreated metastatic colorectal cancer. Oncologist. 2009;14(1):22–8.
Parmar MK, Torri V, Stewart L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat Med. 1998;17:2815–34.
Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials. 2007;8:16.
Williamson P, Tudur Smith C, Hutton JL, Marson AG. Aggregate data meta-analysis with time-to-event outcomes. Stat Med. 2002;21:3337–51.
Bruera G, Cannita K, Di Giacomo D, Lamy A, Troncone G, Dal Mas A, Coletti G, Frébourg T, Sabourin JC, Tosi M, Ficorella C, Ricevuto E. Prognostic value of KRAS genotype in metastatic colorectal cancer (MCRC) patients treated with intensive triplet chemotherapy plus bevacizumab (FIr-B/FOx) according to extension of metastatic disease. BMC Med. 2012;10:135.
Stremitzer S, Stift J, Gruenberger B, Tamandl D, Aschacher T, Wolf B, Wrba F, Gruenberger T. KRAS status and outcome of liver resection after neoadjuvant chemotherapy including bevacizumab. Br J Surg. 2012;99(11):1575–82.
Saltz L, Badarinath S, Dakhil S, Bienvenu B, Harker WG, Birchfield G, Tokaz LK, Barrera D, Conkling PR, O’Rourke MA, Richards DA, Reidy D, Solit D, Vakiani E, Capanu M, Scales A, Zhan F, Boehm KA, Asmar L, Cohn A. Phase III trial of cetuximab, bevacizumab, and 5-fluorouracil/leucovorin vs. FOLFOX-bevacizumab in colorectal cancer. Clin Colorectal Cancer. 2012;11(2):101–11.
Price TJ, Hardingham JE, Lee CK, Weickhardt A, Townsend AR, Wrin JW, Chua A, Shivasami A, Cummins MM, Murone C, Tebbutt NC. Impact of KRAS and BRAF gene mutation status on outcomes from the phase III AGITG MAX trial of capecitabine alone or in combination with bevacizumab and mitomycin in advanced colorectal cancer. J Clin Oncol. 2011;29(19):2675–82.
Tol J, Koopman M, Cats A, Rodenburg CJ, Creemers GJ, Schrama JG, Erdkamp FL, Vos AH, van Groeningen CJ, Sinnige HA, Richel DJ, Voest EE, Dijkstra JR, Vink-Börger ME, Antonini NF, Mol L, van Krieken JH, Dalesio O, Punt CJ. Chemotherapy, bevacizumab, and cetuximab in metastatic colorectal cancer. N Engl J Med. 2009;360(6):563–72. doi:10.1056/NEJMoa0808268. Erratum in: N Engl J Med. 2010 Dec 23;363(26):2573.
Hecht JR, Mitchell E, Chidiac T, Scroggin C, Hagenstad C, Spigel D, Marshall J, Cohn A, McCollum D, Stella P, Deeter R, Shahin S, Amado RG. A randomized phase IIIB trial of chemotherapy, bevacizumab, and panitumumab compared with chemotherapy and bevacizumab alone for metastatic colorectal cancer. J Clin Oncol. 2009;27(5):672–80.
Díaz-Rubio E, Gómez-España A, Massutí B, Sastre J, Reboredo M, Manzano JL, Rivera F, Safont MJ, Montagut C, González E, Benavides M, Marcuello E, Cervantes A, Martínez de Prado P, Fernández-Martos C, Arrivi A, Bando I, Aranda E, Spanish Cooperative Group for the Treatment of Digestive Tumors (TTD). Role of Kras status in patients with metastatic colorectal cancer receiving first-line chemotherapy plus bevacizumab: a TTD group cooperative study. PLoS One. 2012;7(10):e47345.
Salvatore L, Loupakis F, Fontanini G, et al. KRAS and BRAF mutational analyses in a phase II trial of first-line FOLFOXIRI plus bevacizumab (BV) in metastatic colorectal cancer (mCRC) patients (pts). Eur J Cancer. 2009;2(suppl 7):339.
Reinacher-Schick AC, Arnold D, Kubicka S, et al. Impact of kras status on survival in patients (pts.) with metastatic colorectal cancer (mcrc) undergoing bevacizumab (bev) containing chemotherapy regimen-analysis of the aio colorectal cancer study group. Ann Oncol. 2010;21(suppl 8):190.
Cartwright T, Yim YM, Yu E, et al. Clinical outcomes of bevacizumab used in community oncology metastatic colorectal cancer (mcrc) patients with confirmed kras-status. Ann Oncol. 2012;23(suppl 4):99.
El-Khoueiry AB, Pohl A, Danenberg K, et al. Wt Kras and gene expression levels of VEGFR2, EGFR, and ERCC-1 associated with progression-free survival (PFS) in patients (pts) with metastatic colorectal cancer (mCRC) treated with first-line 5-FU or capecitabine with oxaliplatin and bevacizumab (FOLFOX/BV or XELOX/BV). J Clin Oncol. 2009;15(suppl 5):abstr 4056.
Scartozzi M, Galizia E, Chiorrini S, Giampieri R, Berardi R, Pierantoni C, Cascinu S. Arterial hypertension correlates with clinical outcome in colorectal cancer patients treated with first-line bevacizumab. Ann Oncol. 2009;20(2):227–30.
Scartozzi M, Giampieri R, Maccaroni E, Del Prete M, Faloppi L, Bianconi M, Galizia E, Loretelli C, Belvederesi L, Bittoni A, Cascinu S. Pre-treatment lactate dehydrogenase levels as predictor of efficacy of first-line bevacizumab-based therapy in metastatic colorectal cancer patients. Br J Cancer. 2012;106(5):799–804.
Chin L, Tam A, Pomerantz J, Wong M, Holash J, Bardeesy N, et al. Essential role for oncogenic Ras in tumour maintenance. Nature. 1999;400:468–72.
Watnick RS, Cheng Y-N, Rangarajan A, Ince TA, Weinberg RA. Ras modulates Myc activity to repress thrombospondin-1 expression and increase tumor angiogenesis. Cancer Cell. 2003;3:219–31.
Yu JL, Rak JW, Coomber BL, Hicklin DJ, Kerbel RS. Effect of p53 status on tumor response to antiangiogenic therapy. Science. 2002;295:1526–8.
Petrelli F, Barni S. Correlation of progression-free and post-progression survival with overall survival in advanced colorectal cancer. Ann Oncol. 2013;24(1):186–92.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Petrelli, F., Coinu, A., Cabiddu, M. et al. KRAS as prognostic biomarker in metastatic colorectal cancer patients treated with bevacizumab: a pooled analysis of 12 published trials. Med Oncol 30, 650 (2013). https://doi.org/10.1007/s12032-013-0650-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-013-0650-4