Abstract
The relationship between plasma levels of total phospholipids (PL) and/or PL fractions and neoplastic diseases are not fully understood. Therefore, the aim of this study was to analyze concentrations and distribution of plasma phospholipids in patients with prostate cancer (PCa) related to the Gleason score, clinical stage and pathologic grade of prostate cancer. We analyzed plasma phospholipids in 57 newly diagnosed, untreated PCa patients and in 43 age-matched healthy male subjects. Significantly lower (P < 0.01) levels of total plasma PL and all PL classes were found in PCa patients when compared with healthy subjects. The relative concentrations of PL fractions were also changed. Further decrease of total PL and PL fractions was found related to an increase of clinical stadium, pathologic grade, and Gleason score, with phosphatidylethanolamine as the most sensitive plasma PL, the level of which significantly decreased even at the first stage of PCa. Our results showed an altered plasma PL profile in PCa patients, which may contribute to monitoring of the disease progression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Phospholipids (PL) are major structural components of cellular membranes which are involved in a diverse array of functions such as signal transduction and execution of both cellular proliferation and death programs [1, 2]. PL are well known for their amphiphilic nature and are surface active. Alterations in membrane lipid composition have an impact on a broad range of cellular functions from fluidity, which in turn affects permeability of membranes, then transport systems, activity of membrane-bound enzymes to cell growth, proliferation, and viability [3, 4].
Changes in the distribution and concentration of lipid molecules can serve as potential biomarkers for various diseases, including cancer [5]. Because of this potential, lipidomics research is of interest to determine the relative changes in composition and concentration of lipids in cells and also in biological fluids [6]. Quantifying the PL levels in normal and cancerous tissues and studying their interfacial properties may be of benefit in understanding changes in membrane properties and modulating these properties for therapeutic benefits. Various studies have shown that the individual PL and their degradation product levels in normal and tumor tissues are different and adversely affect the fluidity of the cell membranes thus leading to change in membrane penetration properties [7]. Many investigations have also demonstrated the strong influence of tumor tissue on systemic changes in lipids of blood plasma, but in spite of this fact, the data on plasma PL levels and distribution in cancer patients are rather poor. We have recently reported significantly lower levels of cholesterol, HDL cholesterol, and total phospholipids in serum of patients with non-Hodgkin lymphoma and in prostate cancer patients than in healthy subjects [8]. Sullentrop et al. found that plasma PL concentrations in renal cancer cell patients depended on tumor stage and metastatic spread [9]. A decreased concentration of plasma PL has been detected in certain hematological cancers and thyroid carcinoma as well [10–12].
Prostate cancer (PCa) is first in incidence and the second leading cause of cancer-related mortality in the human male population with few new and effective therapies [13, 14]. Early detection of prostate cancer is crucial factor in the prognosis of this disease, and prostate specific antigen (PSA) level in serum plays one of key roles in diagnosis and monitoring of PCa [15]. A diagnosis of PCa is usually confirmed by transrectal ultrasonography (TRUS) biopsy, and the biopsy result includes the Gleason score (GS) and indicates the tumor pathologic grade (PG). The Gleason score, which is a combination of PSA, prostate size, and clinical stage, represents the aggressiveness of the prostate cancer and is considered together with PG and stage of the disease when making decisions about treating PCa and its prognosis [16]. Regarding our previous results on a decreased level of plasma PL in prostate cancer patients as a potential nonspecific prognostic biomarker, the aim of this study was to determine the concentrations and distribution of plasma PL fractions in patients with PCa and in matched healthy subjects, depending on clinical stadium, pathologic grade and Gleason score.
Patients and methods
Eligibility of patients with prostate cancer
The total of 57 adult patients with newly diagnosed prostate carcinoma (CaP), median age 74 years (range 53–94 years of age) entered the study. All of these patients had no other malignant disease or a serious chronic disease and did not receive any therapy at the time of approach. Serum PSA level (ng/ml) [15, 17] and Gleason score (GS) [18] were used as important prognostic parameters. Sex-and age-matched control group was established from 43 apparently healthy male individuals aged 53–86 years (median age 72 years). None of the subjects in this study had any indications of cachexia.
All patients were diagnosed with prostate cancer by transrectal ultrasonography (TRUS) biopsy after abnormal digital rectal examination findings. The number of biopsy cores taken ranged from 10 to 12, and biopsy slides were deciphered by a pathologist to confirm the diagnosis of prostate cancer and Gleason score. Biopsy results included the number and length of cores taken, Gleason score of positive cores, location and tumor length in positive cores. The 2002 TNM staging system of the American Joint Committee on Cancer (AJCC) was used for clinical staging [19], and the patients were divided into 4 groups: clinical stage (CS) I (n = 8 patients), CS II (n = 21), CS III (n = 14) and CS IV (n = 14). In addition, pathologic grade of tumor in all patients was also determined and patients were grouped into four groups depending on the PG. There were 14 patients with PG 1, 23 patients with PG 2, 17 patients had PG 3, and only 3 patients were classified as PG 4. Furthermore, according to the Gleason score, patients were divided into 2 groups: 25 patients with GS <7 and 32 patients with GS ≥7.
All patients and control subjects had body mass index between 20 and 30 kg/m2. All study participants provided written informed consent, which was approved by the Ethical Review Boards of the participating institutions in accordance with the principles of the Declaration of Helsinki.
Analytical methods
Concentration of serum prostate specific antigen was determined using a commercial kit IRMA-PSA (INEP, Zemun, Serbia) [20]. The total PL concentration in plasma was determined by the Zilversmit method [21]. Plasma lipids were extracted with chloroform–methanol mixture (2:1v/v) as we previously described [4]. The PL fraction was isolated from the extracted lipids by one-dimensional thin-layer chromatography (TLC) in a neutral solvent system (petrol ether-diethyl ether-acetic acid; 87:12:1v/v) on Silica Gel GF plates (Merck, Darmstadt, Germany). Four fractions of PL were identified in plasma: lysophosphatidylcholine (LPC), sphingomyelin (SM), phosphatidylcholine (PC) and phosphatidylethanolamine (PE). The other classes of PL which are also present in plasma were not detected by TLC and were not examined in this paper; thus, the relative concentrations of PL classes were expressed as percentages of total PL identified in this study, as described previously [22, 23].
Statistical analysis
All the results are expressed as the mean ± SD. Normality was tested using the Kolmogorov–Smirnov test. Since all variables showed normal distribution, one-way ANOVA, followed by the Tukey post hoc test, and the Student t-test for the comparisons between two groups (Tables 1, 4) were used. The differences were considered significant at P ≤ 0.05.
Results
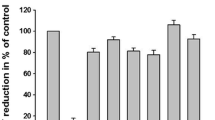
The levels of total PL and PL classes, as well as relative concentrations of PL classes in plasma of prostate cancer patients and healthy subjects are presented in Table 1. Patients with PCa had significantly lower absolute concentration of total PL and all PL fractions. Furthermore, the distribution of PL classes was different between the patient and control groups. Thus, the relative concentrations of LPC and PE were significantly lower (P < 0.001), while percentage of phosphatidylcholine was significantly higher in plasma of PCa patients as compared with healthy persons.
When we divided patients according to clinical stadium into 4 groups (CS I-CS IV), we found a decrease in level of total PL and in all PL fractions from CS I to CS IV, which was significant in CS III and CS IV when compared with CS I and II. Although there were no significant difference neither between CS I and CS II, nor between CS III and IV in any fractions of PL, the lower clinical stadiums I and II significantly differed from CS III and IV. However, when we compared the distribution of PL classes according to CS, we did not find any statistically significant differences (Table 2).
The similar distribution of PL fractions was found when we grouped patients according to pathologic grade into 4 groups, with no significant difference among percentages of PL classes. The level of total PL and PL fractions also showed a decreasing trend, even though we found slightly higher values of total PL, LPC, PC, and PE fractions in plasma of patients with PG 4 than in group with PG 3 (P > 0.05). The levels of all PL were significantly different in PG1 as compared with the other three PG, with an exception of PE, which was similar in all groups. In addition, we found significantly higher concentrations of SM and PC in PG2 group than in PG3, while SM was also higher in PG2 than in PG 4 group (Table 3).
Furthermore, our patients with GS ≥7 had significantly reduced levels of total PL and all PL fractions than patients with GS <7 (Table 4), while the GS did not affected the distribution of PL fractions.
Discussion
We quantified the plasma phospholipids in patients with prostate cancer and in healthy subjects and established significant alterations in systemic PL metabolism in patients with PCa. Our phospholipid quantification revealed lower levels of all PL fractions in patients group, with PC as the major PL in plasma of both groups, but the proportion of PC in total PL was higher in PCa patients than in healthy subjects. It should be noticed that results expressed as concentrations and those calculated on a percentage weight may lead to different conclusions [24], and that concentrations are more accurate reflections of changes than are percentage calculations [25]. However, distribution of PL fractions is often altered in diseases, and many functional disturbances may be related to changes in PL distribution [22].
The alterations in PL profile can be assumed to be a result of tumor metabolism and systemic tumor effects. Tumor growth is associated with phospholipid/tumor membrane metabolism and can lead to systemic changes in the systemic PL distribution [11]. The precise mechanisms underlying the alteration in PL metabolism after malignant transformation are yet to be delineated. One of the possible explanations assumes that the metabolic changes associated with cancer might be caused by an increased rate of PL metabolism and by the faster cell replication of cancer cells in comparison with normal tissue, which lead to a higher demand for PL than that needed for normal growth [12]. However, Ackerstaff et al. showed that this explanation was at least plausible by experiments on cell culture, suggesting that the mechanisms should be further investigated [26]. Our results are consistent with previously published results of other studies showing an altered lipid metabolism in patients with hematological cancer [27–29] and other malignant diseases [9, 11, 12]. All authors reported significantly reduced concentrations of total PL in cancer patients than in healthy persons. Moreover, Murphy et al. [30] demonstrated that low plasma level of PL had been associated with approximately twofold shorter survival in cancer patients, giving this parameter a prognostic significance.
Furthermore, we examined the levels of PL fractions in control group and in patients in relation to the most important clinical factors that are associated with the aggressiveness, treatment, and prognosis of prostate cancer: the Gleason score, clinical stage, and PG. Thus, we divided our patients according to these parameters and we found a decrease in concentrations of all PL classes from lower to higher stages. The only exception is PG 4 with PL levels slightly higher than PG 3, but it could be explained with very small number of patients (only 3 patients). Additionally, we did not find any significant difference between CS I and II, as well as between CS III and IV, while plasma PL levels in patients with PG 1 significantly differed not only from PG 3 and 4, but also from PG 2.
In order to examine the potential of PL fractions as nonspecific biomarkers, we compared PL fractions in patients at the beginning of the disease (CS I and PG 1) with the control group, and only the concentration of PE was significantly lower in patients with CS I and PG 1 than in healthy subjects (data not shown). These results suggest that the level of decrease in the PL concentrations is linked not only to the occurrence of cancer in the prostate, but also to the stage of the disease. Although PE was present in plasma PL measured in this study in the lowest concentration, it was the only PL whose concentration significantly differed between patients with CS I (and/or PG 1) and healthy subjects, so it seems to be the most sensitive plasma PL related to development of prostate cancer. The study in rat hepatoma cells culture has shown that PE (but not other PL classes) synthesis had been affected by testosterone [31], but several studies have reported similar testosterone levels in prostate cancer patients and in healthy men [32, 33]. Thus, it can be assumed that decreased concentration of PE in PCa patients is rather a consequence of disease than an altered hormonal status, although mechanism underlying these changes requires further investigations. At the moment we are not able to compare these results with the data reported on other malignancies, since the other authors presented the sum of PE and SM (PE + SM) because of using another technique [9, 11, 12, 27], but our preliminary results demonstrated similar trend in hematological cancers, supporting our hypothesis on the effect of cancer on PE synthesis. Plasma concentrations of SM and PC in our patients were also decreased when compared with control group, but this decrease was non-significant at early stages of PCa, and similar trend was found for LPC. This is in line with the study by Taylor et al. on patients with different tumors, who found that LPC plasma level correlated with weight loss and inflammatory parameters and, therefore, might be a general indicator of severity of malignant disease [10]. On the contrary, Kuliszkiewicz-Janus and Baczynski found significantly reduced plasma LPC, unlikely the other PL fractions, in patients with early stages of different cancers than in controls [27], while Zhao et al. found low plasma LPC as a useful biomarker for early stages of colorectal cancer [34].
The relative concentrations of PL showed an altered distribution of PL classes toward elevation of PC proportion, and reduction of PE and LPC percentages, when compared with healthy persons. On the other hand, the relative concentrations of PL fractions did not depend on CS, PG, and GS, suggesting that occurrence of PCa, rather than the stage of disease, affects the alterations in distribution of PL fractions. In addition, the influence of other PL classes, which were not examined in this study, cannot be ruled out.
In summary, determination of PL concentration in plasma, as well as PL fractions, can be of interest in diagnosis and monitoring of prostate cancer. In particular, level of PE decreases at an early stage of PCa, even though the serum concentration of PSA in these patients is often lower than 10 ng/ml; thus, phosphatidyl-ethanolamine may represent potential biomarker for PCa. Based on the findings of this study, we think that PL status of prostate cancer patients at the moment of diagnosis and during follow-up may contribute to monitoring of the disease progression. Further studies on a larger number of patients are needed to establish the possible clinical role of measurement of plasma PL classes in patients with prostate cancer.
References
Wright MM, Howe AG, Zaremberg V. Cell membranes and apoptosis: role of cardiolipin, phosphatidylcholine, and anticancer lipid analogues. Biochem Cell Biol. 2004;82(1):18–26.
Wolf C, Quinn PJ. Lipidomics: practical aspects and applications. Prog Lipid Res. 2008;47(1):15–36.
Spector AA, Yorek MA. Membrane lipid composition and cellular function. J Lipid Res. 1985;26:1015–35.
Tepsic J, Vucic V, Arsic A, Blazencic-Mladenovic V, Mazic S, Glibetic M. Plasma and erythrocyte phospholipid fatty acid profile in professional basketball and football players. Eur J Appl Physiol. 2009;107(3):359–65.
Kim H, Min HK, Kong G, Moon MH. Quantitative analysis of phosphatidylcholines and phosphatidylethanolamines in urine of patients with breast cancer by nanoflow liquid chromatography/tandem mass spectrometry. Anal Bioanal Chem. 2009;393(6–7):1649–56.
Min HK, Kong G, Moon MH. Quantitative analysis of urinary phospholipids found in patients with breast cancer by nanoflow liquid chromatography-tandem mass spectrometry: II. Negative ion mode analysis of four phospholipid classes. Anal Bioanal Chem. 2010;396(3):1273–80.
Preetha A, Banerjee R, Huilgol N. Surface activity, lipid profiles and their implications in cervical cancer. J Cancer Res Ther. 2005;1(3):180–6.
Cvetkovic Z, Cvetkovic B, Petrovic M, et al. Lipid profile as a prognostic factor in cancer patients. J BUON. 2009;14(3):501–6.
Sullentrop F, Moka D, Neubauer S, et al. 31P NMR spectroscopy of blood plasma: determination and quantification of phospholipid classes in patients with renal cell carcinoma. NMR Biomed. 2002;15(1):60–8.
Taylor LA, Arends J, Hodina AK, Unger C, Massing U. Plasma lyso-phosphatidylcholine concentration is decreased in cancer patients with weight loss and activated inflammatory status. Lipids Health Dis. 2007;6:17.
Kuliszkiewicz-Janus M, Janus W, Baczynski S. Application of 31P NMR spectroscopy in clinical analysis of changes of serum phospholipids in leukemia, lymphoma and some other non-haematological cancers. Anticancer Res. 1996;161(3B):1587–94.
Raffelt K, Moka D, Sullentrop F, Dietlein M, Hahn J, Schicha H. Systemic alterations in phospholipid concentrations of blood plasma in patients with thyroid carcinoma: an in vitro (31)P high-resolution NMR study. NMR Biomed. 2000;13(1):8–13.
Grubb RL 3rd, Kibel AS. Prostate cancer: screening, diagnosis and management in 2007. Mo Med. 2007;104(5):408–13. quiz 413–414.
Vucic V, Niciforovic A, Adzic M, Radojcic MB, Ruzdijic S. The combination of gamma ionizing radiation and 8-Cl-cAMP induces synergistic cell growth inhibition and induction of apoptosis in human prostate cancer cells. Invest New Drugs. 2008;26(4):309–17.
Tosoian J, Loeb S. PSA and beyond: the past, present, and future of investigative biomarkers for prostate cancer. ScientificWorldJournal. 2010;10:1919–31.
Rubin MA, Bismar TA, Curtis S, Montie JE. Prostate needle biopsy reporting: how are the surgical members of the Society of Urologic Oncology using pathology reports to guide treatment of prostate cancer patients? Am J Surg Pathol. 2004;28(7):946–52.
Stamey TA, Kabalin JN, Ferrari M, Yang N. Prostate specific antigen in the diagnosis and treatment of adenocarcinoma of the prostate. IV. Anti-androgen treated patients. J Urol. 1989;141(5):1088–90.
Gleason DF, Mellinger GT. Prediction of prognosis for prostatic adenocarcinoma by combined histological grading and clinical staging. J Urol. 1974;111(1):58–64.
American Joint Committee on Cancer (AJCC), et al. Prostate. In: Greene FL, Pge DL, Fleming ID, Fritz AG, Balch CM, editors. AJCC cancer staging manual, vol. 6. New York (NY): Springer; 2002. p. 309–16.
Marinovic V, Nedic O, Stanojevic N, Baricevic I, Pavlica S. Investigation of the relationship between two major prostate tumour markers. Yugoslav Med Biochem. 2000;19(4):407–10.
Zilversmit DB, Davis AK. Microdetermination of plasma phospholipids by trichloroacetic acid precipitation. J Lab Clin Med. 1950;35(1):155–60.
Ristic V, Tepsic V, Ristic-Medic D, et al. Plasma and erythrocyte phospholipid fatty acids composition in Serbian hemodialyzed patients. Ren Fail. 2006;28(3):211–6.
Marinetti GV, Albrecht M, Ford T, Stotz E. Analysis of human plasma phosphatides by paper chromatography. Biochim Biophys Acta. 1959;36:4–13.
Khuu Thi-Dinh KL, Demarne Y, Nicolas C, Lhuillery C. Effect of dietary fat on phospholipid class distribution and fatty acid composition in rat fat cell plasma membrane. Lipids. 1990;25(5):278–83.
Zeghari N, Younsi M, Meyer L, Donner M, Drouin P, Ziegler O. Adipocyte and erythrocyte plasma membrane phospholipid composition and hyperinsulinemia: a study in nondiabetic and diabetic obese women. Int J Obes Relat Metab Disord. 2000;24(12):1600–7.
Ackerstaff E, Pflug BR, Nelson JB, Bhujwalla ZM. Detection of increased choline compounds with proton nuclear magnetic resonance spectroscopy subsequent to malignant transformation of human prostatic epithelial cells. Cancer Res. 2001;61(9):3599–603.
Kuliszkiewicz-Janus M, Baczynski S. Application of 31P NMR spectroscopy to monitor chemotherapy-associated changes of serum phospholipids in patients with malignant lymphomas. Magn Reson Med. 1996;35(4):449–56.
Kuliszkiewicz-Janus M, Baczynski S. Treatment-induced changes in 31P-MRS (magnetic resonance spectroscopy) spectra of sera from patients with acute leukemia. Biochim Biophys Acta. 1997;1360(1):71–83.
Cvetkovic Z, Vucic V, Cvetkovic B, et al. Abnormal fatty acid distribution of the serum phospholipids of patients with non-Hodgkin lymphoma. Ann Hematol. 2010;89(8):775–82.
Murphy RA, Wilke MS, Perrine M, et al. Loss of adipose tissue and plasma phospholipids: relationship to survival in advanced cancer patients. Clin Nutr. 2010;29(4):482–7.
Marra CA, de Alaniz MJ. Regulatory effect of various steroid hormones on the incorporation and metabolism of [14C]stearate in rat hepatoma cells in culture. Mol Cell Biochem. 1995;145(1):1–9.
Koo JM, Shim BS. Significance of Serum Testosterone for Prostate-Specific Antigen (PSA) Elevation and Prediction of Prostate Cancer in Patients with PSA Above 10 ng/ml. Korean J Urol. 2010;51(12):831–5.
Morote J, Planas J, Ramirez C, et al. Evaluation of the serum testosterone to prostate-specific antigen ratio as a predictor of prostate cancer risk. BJU Int. 2010;105(4):481–4.
Zhao Z, Xiao Y, Elson P, et al. Plasma lysophosphatidylcholine levels: potential biomarkers for colorectal cancer. J Clin Oncol. 2007;25(19):2696–701.
Acknowledgments
This work was supported by the Project 41030 financed by the Ministry of Science of the Republic of Serbia.
Conflict of interests
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cvetković, B., Vučić, V., Cvetković, Z. et al. Systemic alterations in concentrations and distribution of plasma phospholipids in prostate cancer patients. Med Oncol 29, 809–814 (2012). https://doi.org/10.1007/s12032-011-9914-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12032-011-9914-z