Abstract
Colon cancer with DNA mismatch repair (MMR) defects reveals distinct clinical and pathologic features, including a better prognosis but reduced response to 5-fluorouracil (5-FU)-based chemotherapy. A current standard treatment for recurrent or metastatic colon cancer uses capecitabine plus oxaliplatin (CAPOX), or continuous-infusion fluorouracil plus oxaliplatin (FOLFOX). This study investigated the effect of MMR status on the treatment outcomes for CAPOX and FOLFOX as first-line combination chemotherapy in recurrent or metastatic colon cancer. We analyzed 171 patients who had been treated with CAPOX or FOLFOX as first-line combination chemotherapy in recurrent or metastatic colon adenocarcinoma between February 2004 and July 2008. Tumor expression of the MMR proteins, MLH1 and MSH2, was detected by immunohistochemistry (IHC) in surgically resected tumor specimens. The microsatellite instability (MSI) was analyzed by polymerase chain reaction (PCR) amplification, using fluorescent dye-labeled primers specific to microsatellite loci. Tumors with MMR defect were defined as those demonstrating a loss of MMR protein expression (MMR-D) and/or a microsatellite instability-high (MSI-H) genotype. In all, 75 patients (44%) received FOLFOX, and 96 patients (56%) received CAPOX as first-line combination chemotherapy. The incidence of colon cancer with MMR defect was 10/171 (6%). Colon cancers with MMR defect (MSI-H and/or MMR-D) are more commonly located in proximal to the splenic flexure (p = 0.03). The MMR status did not significantly influence the overall response (p = 0.95) to first-line CAPOX or FOLFOX treatment in patients with recurrent or metastatic colon cancer. According to the MMR status, there was no significant difference for PFS (p = 0.50) and OS (p = 0.47) in patients with recurrent or metastatic colon cancer treated with first-line CAPOX or FOLFOX. In colon cancers with MMR defect, there was no significant difference for PFS (p = 0.48) and OS (p = 0.56) between CAPOX and FOLFOX as first-line combination chemotherapy. However, in MMR intact, there was significant difference for OS between CAPOX and FOLFOX (p = 0.04). OS was significantly better in patients treated with CAPOX when compared to patients with FOLFOX. The MMR status does not predict the effect of oxaliplatin-based combination chemotherapy as 1st line in recurrent or metastatic colon cancers. CAPOX in the first-line treatment of recurrent or metastatic colon cancer with MMR intacts showed a superior OS compared with FOLFOX unlike colon cancer with MMR defects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) develops either sporadically (85%), as part of a hereditary cancer syndrome (less than 10%), or against a background of inflammatory bowel disease. It is believed that the adenoma–carcinoma sequence underlies the development of colorectal cancer in most patients, and two distinct pathways have been identified as the microsatellite instability (MSI) and chromosomal instability (CIN) pathways [1–4]. The microsatellite instability (MSI) pathway, which involves failure of the nucleotide mismatch recognition and repair system, is one form of genomic instability [5, 6]. Deficient DNA mismatch repair (MMR defect) occurs in approximately 10–15% of all sporadic colorectal cancer [7]). Instability in microsatellite sequences in sporadic colorectal cancer exhibiting MSI, often due to the loss of expression of a mismatch repair gene (most commonly MLH1 and MSH2), is caused by epigenetic silencing [8–10]. High levels of MSI (MSI-H) colorectal cancers are more frequent in women and more commonly located proximal to the splenic flexure [6, 11–13]. The MSI-H colorectal cancers are known to bear many features that are generally associated with poor prognosis, including deep tumor invasion and poor histologic differentiation. However, patients with MSI-H tumors revealed longer overall and cancer-specific survival than stage-matched patients with tumors exhibiting CIN [14, 15], implicating that the pronounced genetic instability of tumor cells with MSI may increase the susceptibility to apoptosis.
The loss of DNA mismatch repair (MMR) proteins that had DNA damage sensor function leads to a lack of appropriate signals for apoptosis induction [16, 17] and a resistance to specific chemotherapy drugs [18–20]. In studies for adjuvant chemotherapy in stage II or III colon cancer, patients with MSI-H demonstrated no benefit with a regimen containing fluorouracil (FU), unlike patients whose tumors demonstrate CIN [21–23].
A current treatment of reference for recurrent or metastatic colon cancer is capecitabine plus oxaliplatin (CAPOX), or continuous-infusion fluorouracil plus oxaliplatin (FOLFOX) [24]. In addition, targeted therapies with monoclonal antibodies against the vascular endothelial growth factor and the epidermal growth factor receptor have also become available [25, 26]. This increase in the availability of effective drugs offers a choice among various therapeutic options. However, a reliable prediction of tumor response and prognosis for each therapy scheme for individual patients has not been defined. Recently, some studies have investigated the relationship between the MMR status and chemotherapy efficacy in metastatic CRC [27–31]. Des Guetz et al. (2007) reported the prognostic value of MSI-H in patients treated with palliative first-line combination chemotherapy with FOLFOX (in 44 patients with metastatic CRC). They did not find a significant difference for chemotherapy efficacy between MSI-H and microsatellite stable (MSS or MSI-S) cases. One example of meta-analysis also showed that chemotherapy was not associated with a significantly improved outcome in patients with metastatic CRC among MSI-H, compared with MSI-S [28]. However, Muller et al. reported that MSI-H may be correlated with a poor response to a 5-FU/oxaliplatin treatment, and Jensen et al. found that patients with the higher gene expression of MSH-2 in advanced CRC treated with capecitabine showed a better response [27, 32]. In addition to these cases, the relationship between MMR status and outcomes for chemotherapy differed among studies. According to the MMR status, there has as yet been no consensus as to the choices among various effective therapeutic options in advanced CRC.
This study investigated the effect of MMR status on the outcomes for CAPOX and FOLFOX as first-line combination chemotherapy in recurrent or metastatic colon cancer.
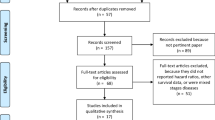
Patients and methods
Patients
Between February 2004 and July 2007, 171 patients were treated with CAPOX or FOLFOX as first-line combination chemotherapy in recurrent or metastatic colorectal adenocarcinoma at Samsung Medical Center, Seoul, Korea. Sixty-six of the 171 patients experienced recurrent disease after the complete resection. All 171 patients had been assessed for the status of the MMR protein or MSI genotype. The following clinical data were collected from medical records for each patient: surgical and pathologic reports, imaging, treatment modalities, the status of the MMR protein and MSI genotype, and expression of p53. Staging of the disease was classified according to the sixth edition of guidelines of the American Joint Committee on Cancer (AJCC).
Treatment
In all, 75 patients received FOLFOX. This consisted of oxaliplatin (85 mg/m2 over 2 h, day 1), followed by leucovorin (200 mg/m2 over 2 h, day 1), followed by 5-FU (400 mg/m2 bolus, day 1 and then 2,400 mg/m2 over 48 h, days 1 and 2) of intravenous infusion. Cycles were repeated every 2 weeks. Ninety-six patients received CAPOX, consisting of oxaliplatin (130 mg/m2 over 2 h, day 1) intravenous infusion and capecitabine (1,000 mg/m2, twice per day, consecutively for 2 weeks) per oral route. Cycles were repeated every 3 weeks. Tumor response was assessed at baseline and every 2 cycles according to RECIST. All patients were scheduled to receive chemotherapy until disease progression, intolerable adverse events, or the patients’ refusal to continue treatment. FOLFOX and CAPOX were both available as first-line combination chemotherapy in recurrent or metastatic colorectal adenocarcinoma in this center, and the decision of choosing the each regimen was entirely based on the physician’s discretion and patient’s request.
Analysis of MSI
Primary tissue specimens were obtained during surgery or biopsy. Laboratory analysis was conducted at Samsung Medical Center. The MSI was analyzed by polymerase chain reaction (PCR) amplification using fluorescent dye-labeled primers for the Bethesda markers (BAT-26, BAT-25, D5S346, D2S123, and D17S250) specific to microsatellite loci, as recommended by the National Cancer Institute Workshop on MSI [33]. MSI was defined as a band shift in either of the two alleles or as the appearance of a differently sized band in the tumor sample. Tumors were classified by MSI-H if instability was found at ≥50% of the loci screened, and MSI-low (MSI-L) if at least one but ≤50% of the loci showed instability, and microsatellite stable (MSS or MSI-S) if all loci were stable. Immunohistochemistry (IHC) detected the presence of MLH1 and MSH2 proteins in resected tumor specimens. Two MMR proteins (MLH1 and MSH2) were lost most commonly in sporadic colon cancer. For each antibody, a known positive normal colonic mucosa served as a positive control. Tumors known to lack MLH1 or MSH2 served as a negative control. All cases were scored as positive (defined as ≥10% of tumor cells staining) or negative (<10% tumor cells staining). The loss of MMR protein (MLH1 and/or MSH2) expression was defined as MMR deficient (MMR-D), distinguishable from the mismatch repair intact (MMR-I). Tumors with MMR defect were those demonstrating loss of MMR protein expression (MMR-D) and/or microsatellite instability-high (MSI-H) genotype. Tumors with MMR intact were defined as MMR-I and/or MSI-L/S.
Immunohistochemistry and immunostaining
Formalin-fixed, paraffin-embedded tissues including both tumors and nontumorous liver tissues were sectioned at 4 μm. Immunohistochemical studies were performed using the streptavidin–biotin complex method and a TechMate™ 1000 automated staining system (DakoChemmate, Glostrup, Denmark). Primary monoclonal antibody against p53 (clone Bp53-12) was purchased from Zymed Laboratories Inc. (San Francisco, CA, USA) and used at 1:400 dilution. Deparaffinized sections were treated with 3% hydrogen peroxide in methanol for 10 min to block endogenous peroxidase. Sections were processed in 0.05 mol citrate buffer (pH 6.0) and heated in a microwave oven for 10 min for antigen retrieval. Sections were then incubated with the primary antibody for 30 min at room temperature. Secondary antibody (Dako, REAL™, EnVision™) was purchased from Zymed Laboratories Inc. (San Francisco, CA, USA). DAB (3,3’-diaminobenzidine tetrahydrochloride) was used as a chromogen, and Meyer’s hematoxylin counterstain was applied.
Expression patterns of p53 were determined in a semiquantitative manner using light microscopy. Immunoreactivity for p53 (nuclear staining) was categorized in accordance with the percentage of tumor cells stained as described previously: immunonegative, ≤5%; immunopositive, >5% staining. Brown nuclear stain was regarded as positive.
Statistical analysis
We intended to investigate whether the tumor MMR status influenced on the tumor response, progression-free survival (PFS), and overall survival (OS) to treatment with CAPOX or FOLFOX as first-line combination chemotherapy in recurrent or metastatic colon cancer. The MMR status was based on genotyping (MSI-H vs. MSI-L/S) and IHC (MMR-D vs. MMR-I). Moreover, we evaluated the significance of p53 expression as a prognostic marker in recurrent or metastatic colon cancer. Primary statistical outcomes included overall survival and progression-free survival (OS/PFS) measured from the start date of the first-line combination chemotherapy; PFS and OS were estimated by Kaplan–Meier curves and compared by means of the log-rank test. Relationships between tumor MMR status, p53 expression, and clinicopathologic factors were studied using the χ2 test. The proportional hazards model was used to make survival comparisons, controlling for treatment, and other clinicopathologic factors. Statistical significance was defined as a two-sided p < 0.05.
Results
Microsatellite stability status and p53 status
In total, 147 tumor specimens were genotyped, and 144 specimens were tested by IHC. Genotyping results demonstrated that seven (4.7%) patients were MSI-H, and 140 (95.3%) were MSI-L/S. By IHC, nine (6.3%) patients were MMR-D, and 135 (93.7%) were MMR-I. According to the definition of MMR status, the incidence of colon cancer with MMR defect was 10/171 (5.8%), and 161/171 (94.2%) were MMR intact. As well, 125 patients were assessed for p53 expression by immunostaining. Colon cancers with MMR defect (MSI-H and/or MMR-D) are more commonly located proximal to the splenic flexure (p = 0.03). The median age of the patients was 61.8 (range, 24.5–85.6), and 56.1% of the patients were male. There were 66 (38.6%) patients with recurrent disease, 105 (61.4%) with metastatic disease.
Correlation between tumor MMR status and clinical characteristics
There were no significant differences in sex, age, ECOG performance status, histologic differentiation, p53 status, or types of first-line combination chemotherapy according to tumor MMR status (MMR defect vs. MMR intact) (Table 1). Patients with MMR-intact tumors had significantly more primary tumors of the left side (χ2, p = 0.03).
Correlation between tumor MMR status and treatment response
Among ten MMR-defect patients, two complete responses and five partial responses were observed (overall response rates, 70%). Stable disease was observed in one patient (10%) and progressive disease in two patients (20%) (Table 2). The disease control rate was 80%. Among 161 MMR-intact patients, 14 complete responses and 97 partial responses were observed (overall response rates, 69%). Stable disease was observed in 34 patients (21%) and progressive disease in 16 patients (10%). The disease control rate was 90%. The overall response rates and disease control rates of MMR-defect and MMR-intact groups were 70 versus 69% (p = 0.95) and 80 versus 90% (p = 0.28), respectively. The MMR status did not significantly influence the overall response (p = 0.95) to first-line CAPOX or FOLFOX treatment in patients with recurrent or metastatic colon cancer.
Correlation between tumor MMR status and PFS and OS
The overall survival (OS) rate for all 171 patients was 29.6 months, and the progression-free survival (PFS) rate was 9.5 months (95% C.I. 7.96–11.04) (Table 3). There was no significant difference in PFS according to MMR status, sex, tumor site, p53 status, or chemotherapy regimens. Histologic differentiation (G1-2 vs. G3-4) was the only factor that made a difference to PFS (p < 0.01). For OS, there was no significant difference according to MMR status, sex, p53 status, or chemotherapy regimens. There was a significant difference in OS according to tumor site (right vs. left) and histologic differentiation (G1-2 vs. G3-4) (p = 0.03 and p = 0.01), respectively. According to the MMR status, there was no significant difference for PFS (p = 0.50) and OS (p = 0.47) in patients with recurrent or metastatic colon cancer treated with first-line CAPOX or FOLFOX.
In each MMR status, PFS and OS were evaluated according to clinical characteristics. There was no significant difference in PFS and OS according to tumor site, histologic differentiation, p53 status, or chemotherapy regimens in patients with MMR-defect tumors (Table 4). In colon cancers with MMR defect, there was no significant difference for PFS (p = 0.48) and OS (p = 0.56) between CAPOX and FOLFOX as a first-line combination chemotherapy (Fig. 1). PFS and OS were significantly better in female patients when compared to male patients.
In MMR-intact tumors, there was a significant difference for PFS (p = 0.04) according to histologic differentiation, and for OS according to tumor site (p = 0.03), histologic differentiation (p = 0.01) and chemotherapy regimens (p = 0.04) (Table 5). In colon cancers with MMR-intact tumors, there was a significant difference for OS between CAPOX and FOLFOX (p = 0.04, Fig. 2). As indicated, the OS was significantly better in patients treated with CAPOX when compared to patients treated with FOLFOX.
Discussion
In our study, there was no difference in the overall response rates, PFS, or OS between patients with MMR-defect and MMR-intact advanced colon cancer, implying that the MMR status did not seem to be a viable predictive marker to evaluate chemosensitivity in a recurrent or metastatic setting. This finding is consistent with previous studies [28–30]. In a recent meta-analysis, Des Guetz et al. reported that MSI status did not predict the effects of chemotherapy in metastatic colorectal tumors [28–30]. These findings may be caused by using oxaliplatin-based combination chemotherapy. The MMR system is not largely involved in the recognition of oxaliplatin adducts in DNA [20], and MMR-defect cells are not resistant to oxaliplatin [20, 34]. Experimental evidence has identified links between MMR-defect cells and cytotoxic drug resistance for alkylating agents [10, 35, 36]. Selection for cisplatin resistance in several human cancer cell lines resulted in a loss of expression of the MMR proteins MLH1 and MSH2 in most (90%) cell lines, implicating the MMR system in cisplatin resistance [35]. Cisplatin-sensitive cell lines and human biopsies are hypermethylations of the promoters of only one MLH1 allele, whereas resistant cell lines all exhibit hypermethylation of the promoters of both MLH1 alleles [37, 38]. Treatment of cisplatin-resistant cell lines with 5-azacytidine, a methylation inhibitor, resulted in re-expression of MLH1 and consequently increased sensitivity to cisplatin. Whereas MMR is clearly involved in cisplatin activity, in vitro and preclinical experiments have shown that MLH1-, MSH2-, and MSH6-deficient cells, which are resistant to cisplatin, are nonetheless susceptible to oxaliplatin; defects in MMR are associated with a modest to moderate level of resistance to cisplatin, but not to oxaliplatin [20, 39].
Interestingly, our results suggested that advanced colon cancer might have a different chemosensitivity according to MMR status. In colon cancers with MMR defect, there was no significant difference for PFS (p = 0.48) and OS (p = 0.56) between CAPOX and FOLFOX as a first-line combination chemotherapy. However, with only 10 MMR-defect patients, it would be very unlikely to show a significant difference between treatments. With a larger study with more MMR-defect patients, a difference between treatment arms may be demonstrated. In colon cancers with MMR intact, there was a significant difference for OS (p = 0.04) between CAPOX and FOLFOX. Thus, OS was significantly better in patients treated with CAPOX when compared to patients treated with FOLFOX. This finding of our study is similar to that of Jensen [32]. Jensen et al. reported that the higher gene expression of MSH2 in responders, and the trend for predicting overall survival, indicated a predictive value of this marker in the treatment of advanced CRC with capecitabine [32].
In this study, 125 patients were assessed for p53 expression by immunostaining. About 69% (86/125) of patients tested positive for the p53 protein expression. The p53 expression is known to occur more often in well/moderated-differentiated tumors [40–42]. The largest study on p53 overexpression in early stage colorectal cancer demonstrated no significant prognostic value of p53 protein overexpression in 465 colon cancer samples [43]. However, in advanced colon cancer, there has been no consensus for the p53 as a prognostic marker. In this study, the status of p53 expression did not have a significant impact on DFS and OS in patients with recurrent or metastatic colon cancer treated with CAPOX or FOLFOX as a first-line combination chemotherapy. According to the p53 status, there was no significant difference for response rate, PFS, and OS between CAPOX and FOLFOX. Thus, p53 expression status may not be an indicator of prognosis in colon cancer.
In our study, OS seems more favorable than those reported in previous studies; one of the plausible explanations for such observation may owe to high proportion of patients with complete metastatectomy (54/171 (32%)).
To conclude, MMR status and p53 status did not seem to be viable predictive markers in evaluating outcomes in recurrent or metastatic colon cancer cases treated with CAPOX or FOLFOX, as we did not find a significant difference in clinical outcomes according to MMR and p53 status. However, we found that advanced colon cancer might have a different chemosensitivity, according to the MMR status. Future studies for treatment in recurrent or metastatic colon cancer must include various tailored chemotherapy strategies according to the status of potential prognostic markers, such as MMR status, p53, SMAD4, thymidylate synthetases, and K-ras.
References
Gervaz P, Bucher P, Morel P. Two colons-two cancers: paradigm shift and clinical implications. J Surg Oncol. 2004;88:261–6.
Gervaz P, et al. Comparison of microsatellite instability and chromosomal instability in predicting survival of patients with T3N0 colorectal cancer. Surgery. 2002;131:190–7.
Haydon AM, Jass JR. Emerging pathways in colorectal-cancer development. Lancet Oncol. 2002;3:83–8.
Jass JR, Whitehall VL, Young J, Leggett BA. Emerging concepts in colorectal neoplasia. Gastroenterology. 2002;123:862–76.
Aaltonen LA, et al. Clues to the pathogenesis of familial colorectal cancer. Science. 1993;260:812–6.
Ionov Y, Peinado MA, Malkhosyan S, Shibata D, Perucho M. Ubiquitous somatic mutations in simple repeated sequences reveal a new mechanism for colonic carcinogenesis. Nature. 1993;363:558–61.
Soreide K, Janssen EA, Soiland H, Korner H, Baak JP. Microsatellite instability in colorectal cancer. Br J Surg. 2006;93:395–406.
Miyakura Y, et al. Extensive but hemiallelic methylation of the hMLH1 promoter region in early-onset sporadic colon cancers with microsatellite instability. Clin Gastroenterol Hepatol. 2004;2:147–56.
Herman JG, Baylin SB. Gene silencing in cancer in association with promoter hypermethylation. N Engl J Med. 2003;349:2042–54.
Herman JG, et al. Incidence and functional consequences of hMLH1 promoter hypermethylation in colorectal carcinoma. Proc Natl Acad Sci USA. 1998;95:6870–5.
Jass JR, et al. Morphology of sporadic colorectal cancer with DNA replication errors. Gut. 1998;42:673–9.
Thibodeau SN, Bren G, Schaid D. Microsatellite instability in cancer of the proximal colon. Science. 1993;260:816–9.
Lothe RA, et al. Genomic instability in colorectal cancer: relationship to clinicopathological variables and family history. Cancer Res. 1993;53:5849–52.
Gryfe R, et al. Tumor microsatellite instability and clinical outcome in young patients with colorectal cancer. N Engl J Med. 2000;342:69–77.
Popat S, Hubner R, Houlston RS. Systematic review of microsatellite instability and colorectal cancer prognosis. J Clin Oncol. 2005;23:609–18.
Anthoney DA, McIlwrath AJ, Gallagher WM, Edlin AR, Brown R. Microsatellite instability, apoptosis, and loss of p53 function in drug-resistant tumor cells. Cancer Res. 1996;56:1374–81.
Gradia S, Acharya S, Fishel R. The role of mismatched nucleotides in activating the hMSH2-hMSH6 molecular switch. J Biol Chem. 2000;275:3922–30.
Kat A, et al. An alkylation-tolerant, mutator human cell line is deficient in strand-specific mismatch repair. Proc Natl Acad Sci USA. 1993;90:6424–8.
Aebi S, et al. Loss of DNA mismatch repair in acquired resistance to cisplatin. Cancer Res. 1996;56:3087–90.
Fink D, et al. The role of DNA mismatch repair in platinum drug resistance. Cancer Res. 1996;56:4881–6.
Ribic CM, et al. Tumor microsatellite-instability status as a predictor of benefit from fluorouracil-based adjuvant chemotherapy for colon cancer. N Engl J Med. 2003;349:247–57.
Kim GP, et al. Prognostic and predictive roles of high-degree microsatellite instability in colon cancer: a national cancer institute-national surgical adjuvant breast and bowel project collaborative study. J Clin Oncol. 2007;25:767–72.
Barratt PL, et al. DNA markers predicting benefit from adjuvant fluorouracil in patients with colon cancer: a molecular study. Lancet. 2002;360:1381–91.
Diaz-Rubio E, et al. Phase III study of capecitabine plus oxaliplatin compared with continuous-infusion fluorouracil plus oxaliplatin as first-line therapy in metastatic colorectal cancer: final report of the Spanish Cooperative Group for the Treatment of Digestive Tumors Trial. J Clin Oncol. 2007;25:4224–30.
Kelly H, Goldberg RM. Systemic therapy for metastatic colorectal cancer: current options, current evidence. J Clin Oncol. 2005;23:4553–60.
Meyerhardt JA, Mayer RJ. Systemic therapy for colorectal cancer. N Engl J Med. 2005;352:476–87.
Muller CI, et al. Predictive and prognostic value of microsatellite instability in patients with advanced colorectal cancer treated with a fluoropyrimidine and oxaliplatin containing first-line chemotherapy. A report of the AIO colorectal study group. Int J Colorectal Dis. 2008;23:1033–9.
Des Guetz G, et al. Microsatellite instability does not predict the efficacy of chemotherapy in metastatic colorectal cancer. A systematic review and meta-analysis. Anticancer Res. 2009;29:1615–20.
Des Guetz G, Uzzan B, Nicolas P, Schischmanoff O, Morere JF. Microsatellite instability: a predictive marker in metastatic colorectal cancer? Target Oncol. 2009;4:57–62.
des Guetz G, et al. Microsatellite instability and sensitivity to FOLFOX treatment in metastatic colorectal cancer. Anticancer Res. 2007;27:2715–9.
Koopman M, et al. Deficient mismatch repair system in patients with sporadic advanced colorectal cancer. Br J Cancer. 2009;100:266–73.
Jensen LH, Danenberg KD, Danenberg PV, Jakobsen A. Predictive value of MSH2 gene expression in colorectal cancer treated with capecitabine. Clin Colorectal Cancer. 2007;6:433–5.
Choe WH, et al. High frequency of microsatellite instability in intestinal-type gastric cancer in Korean patients. Korean J Intern Med. 2005;20:116–22.
Vaisman A, et al. The role of hMLH1, hMSH3, and hMSH6 defects in cisplatin and oxaliplatin resistance: correlation with replicative bypass of platinum-DNA adducts. Cancer Res. 1998;58:3579–85.
Brown R, et al. hMLH1 expression and cellular responses of ovarian tumour cells to treatment with cytotoxic anticancer agents. Oncogene. 1997;15:45–52.
Plumb JA, Strathdee G, Sludden J, Kaye SB, Brown R. Reversal of drug resistance in human tumor xenografts by 2’-deoxy-5-azacytidine-induced demethylation of the hMLH1 gene promoter. Cancer Res. 2000;60:6039–44.
Strathdee G, MacKean MJ, Illand M, Brown R. A role for methylation of the hMLH1 promoter in loss of hMLH1 expression and drug resistance in ovarian cancer. Oncogene. 1999;18:2335–41.
Strathdee G, et al. Primary ovarian carcinomas display multiple methylator phenotypes involving known tumor suppressor genes. Am J Pathol. 2001;158:1121–7.
Fink D, et al. In vitro and in vivo resistance to cisplatin in cells that have lost DNA mismatch repair. Cancer Res. 1997;57:1841–5.
Schernhammer ES, Ogino S, Fuchs CS. Folate and vitamin B6 intake and risk of colon cancer in relation to p53 expression. Gastroenterology. 2008;135:770–80.
Munro AJ, Lain S, Lane DP. P53 abnormalities and outcomes in colorectal cancer: a systematic review. Br J Cancer. 2005;92:434–44.
Nehls O, et al. Studies on p53, BAX and Bcl-2 protein expression and microsatellite instability in stage III (UICC) colon cancer treated by adjuvant chemotherapy: major prognostic impact of proapoptotic BAX. Br J Cancer. 2007;96:1409–18.
Allegra CJ, et al. Investigation of the prognostic and predictive value of thymidylate synthase, p53, and Ki-67 in patients with locally advanced colon cancer. J Clin Oncol. 2002;20:1735–43.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by the Korea Health 21 R&D Project, Ministry of Health and Welfare, Republic of Korea (Grant No. 0412-CR01-0704-0001).
Rights and permissions
About this article
Cite this article
Kim, S.T., Lee, J., Park, S.H. et al. The effect of DNA mismatch repair (MMR) status on oxaliplatin-based first-line chemotherapy as in recurrent or metastatic colon cancer. Med Oncol 27, 1277–1285 (2010). https://doi.org/10.1007/s12032-009-9374-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12032-009-9374-x