Abstract
Functional polymorphisms in the thiopurine methyl transferase (TPMT) gene have been associated with varying levels of enzyme activity and the occurrence of toxicity related to thiopurines. A total of 98 patients (66 pediatric and 32 adults) with precursor B acute lymphoblastic leukemia (Pre-B ALL) were evaluated for TPMT gene polymorphisms. The inability to tolerate 6-mercaptopurine (6-MP) at conventional doses was considered as a surrogate marker of hematologic toxicity. The allele frequency of TPMT*2, *3A, *3B and *3C in the study population was 0.5, 0, 0 and 2.6%, respectively, similar to the frequency observed in other Asian populations. Five patients were heterozygous for TPMT*3C variant allele, and one of these patient’s was compound heterozygous with TPMT*2 variant as the other allele. The impact of TPMT polymorphisms on the toxicity and treatment outcome was assessed in 66 pediatric patients only, as there was no variant TPMT detected in the adult patients. Three of the 5 patients (60%) heterozygous for TPMT*2 or TPMT*3C polymorphisms and 12/61 patients (20%) with wild type TPMT genotype had more than 10% of reduction of 6-MP dose (P = 0.07). The presence of TPMT polymorphisms did not seem to completely explain the variation in 6-MP toxicity in this small group of patients. Other novel variants in TPMT or variations in the genes involved in transport and biotransformation of 6-MP need to be evaluated in the Indian population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
6-Mercaptopurine (6-MP) is one of the main drugs used for maintenance therapy in ALL, but it is associated with significant cytopenia in a subset of patients [1, 2]. TPMT is involved in the methylation reactions of 6-MP and azathioprine, its pro-drug. The activity of TPMT is influenced by the genetic polymorphisms, which can alter the rate of 6-MP metabolism by TPMT. The enzyme activity of TPMT varies among patients; 86.6% of the Caucasian population has high TPMT activity, 11.1% has intermediate activity, and 0.3% is deficient in TPMT [3, 4]. Three of these alleles (TPMT*2, *3A and *3C (G460A) account for 80–95% of intermediate- or low-enzyme activity cases [4–7]. The TPMT genotype correlates well with in vivo enzyme activity within erythrocytes and leukaemic blast cells and is clearly associated with risk of toxicity [8, 9]. The cumulative incidence of 6-MP dose reduction due to toxicity was highest among patients who were homozygous mutant for TPMT, intermediate among heterozygous patients and lowest among wild-type patients. Dose reduction in patients with inactive TPMT is associated with lower 6-TG concentrations and thus a higher risk of relapse [10–12]. In addition, there is emerging data that the TPMT genotype may influence the risk of secondary malignancies, including brain tumors and AML [8, 13].
To the best of our knowledge, there is no report from India on the incidence of common TPMT allelic variants and the influence of these alleles on hematologic toxicity in patients’with ALL. This retrospective analysis was undertaken to determine the prevalence of genetic polymorphisms in the TPMT gene in Indian patients with acute lymphoblastic leukemia and to study the impact of TPMT genotype on toxicity and treatment outcome. The inability to tolerate 6-MP at conventional doses was considered as a surrogate marker of hematologic toxicity.
Patients and methods
Patients
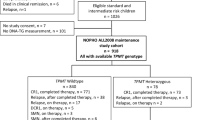
A total of 98 patients with Pre-B ALL, treated at our centre between 1999 till 2003 for whom, genomic DNA sample was available at diagnosis were included in this study. DNA was extracted by standard phenol–chloroform method from available bone marrow or peripheral blood sample at diagnosis that was sent for molecular diagnosis of leukemia-specific fusion transcripts. All patients received treatment as per institutional protocols. Impact of TPMT polymorphisms on treatment outcome and 6-MP intolerance was studied only in the pediatric patients as none of the adult patients had TPMT allelic variations.
Treatment protocol
Children were treated with a modified BFM protocol with a 6-drug induction consisting of vincristine, daunorubicin, l-asparaginase, cyclophosphamide, cytosine and prednisolone [14, 15]. CNS directed therapy consisted of intrathecal methotrexate and CNS radiation. Interim maintenance with 6-MP and methotrexate was followed by reinduction and then with maintenance therapy for 2 years with daily 6-MP (50 mg/m2) and weekly oral methotrexate (20 mg/m2). In addition, some patients received monthly vincristine and steroids during maintenance. Adults (≥15 years) were treated with a modified GMALL protocol wherein induction was followed by consolidation consisting of 2 courses of cytarabine and etoposide [15]. Patients further received reinduction followed by maintenance therapy with daily 6-MP, weekly methotrexate and monthly pulses of vincristine and prednisolone.
Hematological toxicity. Detailed information on the doses tolerated and the reductions in 6-MP doses required were obtained from hospital records. More than 2 episodes of neutropenia (ANC < 0.5 × 109/l) requiring temporary discontinuation of therapy or greater than 2 episodes of febrile neutropenia within a period of 3 months was considered as an indication to reduce the 6-MP doses. A reduction in 6-MP doses of 10% or more was considered significant. Blood tests were done every 2 weeks during maintenance to monitor hematologic toxicity. Dosage alterations were allowed to maintain an optimal white cell count of about 3 × 109/l, minimize time of therapy omission and hospital admissions from febrile neutropenia. Dosing and outcome data was available for both pediatric and adult patients.
TPMT polymorphism analysis. Four common functional variants of TPMT gene TPMT*2 and TPMT*3 (*3A, *3B and *3C) were screened in all the ALL samples using previously published methods [5, 16]. All the amplification was done in a 25-μl reaction containing approximately 250 ng of DNA in a PCR master mix (Eppendorf, Hamburg, Germany). Briefly, for G238C mutation (TPMT*2), an allele specific PCR was performed using the forward wild type and mutant primers and a common reverse primers, and the 254-bp PCR product was resolved in 3% agarose. For G460A and A719G mutation (TPMT*3B and *3C), PCR–RFLP was performed using the primers described by Yates et al. [5], and the 365 and 293-bp products PCR products were digested with a restriction enzyme MwoI and AccI (New England Bio labs, Beverly, MA, USA) and kept in water bath for 2 h at 60°C and resolved in 3% agarose.
Statistical analysis
The Chi-square or Fisher’s exact test was used to test the difference in the genotype and allele frequencies within the groups, and also with respect to age, sex, and treatment outcome such as dose reduction and toxicity.
Results
Four common functional variants of the TPMT gene, TPTM*2, TPMT*3A, TPMT*3B and TPMT*3C were evaluated in 98 patients diagnosed with Pre-B ALL. There were 66 children and 32 adults with a median age of 5 and 24 respectively. None of these 4 variant alleles was present in any of the adult patients who underwent this therapy, but 4 of the pediatric patients were heterozygous carriers of TPMT*3C allele and one was compound heterozygous for TPMT*2 and TPMT*3C. The allele frequency of TPMT*2, TPMT*3A, TPMT*3B and TPMT*3C alleles in the present study was 0.5, 0, 0 and 2.6% respectively.
Fifteen of the 66 patients had 6-MP dose reduction; however, the TPMT variant alleles were present only in 3/15 patients. Two patients with TPMT*3C heterozygous genotype did not require dose reduction. There was no significant difference between patients who were wild type or heterozygous for the TPMT alleles with respect to age (P = 0.308), sex (P = 1.00) and treatment outcome (P = 0.389), but there was a trend to significant increase in the incidence of hematologic toxicity (P = 0.07) in patients with variant TPMT allele (Table 1). Although 9 out of 32 adult patients (27%) had significant dose reduction, none of the samples had the common variant TPMT alleles.
Discussion
To the best of our knowledge, there is no report on the prevalence of the common TPMT allelic variants in the Indian population. The frequencies of four common allelic variants of the TPMT gene, namely TPMT*2, TPMT*3A, TPMT*3B and TPMT*3C exhibit ethnic differences. The overall TPMT heterozygous carrier allele frequency in our study population was 3.1%, which is much lower than reported for Caucasian population (7–14%) but similar to earlier Asian studies in Han Chinese (2.5%) and a multiracial study from Singapore (4.6%) [17]. TPMT*3C is more prevalent in Ghanaians (14.8%), while TPMT*3A was the common variant (10.1%) in British subjects [18]. In our study, the most commonly reported polymorphic allele was TPMT*3C (2.6%). Earlier studies in samples of Indian origin from UK and Singapore have noted presence of TPMT*3A and TPMT*3C variants at low frequencies of 0.5 and 0.8% respectively [17, 19] (Table 2). Studies have suggested that the A719G (TPMT*3C) mutation may be the ancestral TPMT mutant allele from which other rare mutant allele originate as it was present in both Caucasian, African, Chinese and Indian populations [20].
TPMT*2 appears to be a more recent allele, and seen in compound heterozygous form in one patient with TPMT*3C. TPMT*2 allele is very rare, which has been detected in British Caucasians (0.5%) [20], German Caucasians (0.2%) [21], French Caucasians (0.7%) [22], Brazilian (2.2%) [23], but not in British Ghanaian population [18]. Even the studies done in cord blood samples from the multiracial Asian populations including Indians found no TPMT*2 variant allele. None of the patients had variant TPMT*3A or TPMT*3B in our study cohort, although TPMT*3A has been reported to occur in an Indian population at a lower frequency (0.5%) [22]. It is possible that TPMT*2 and TPMT*3B alleles were likely to be generated from the ancestral one (TPMT*3C) as the latter is prevalent in all studied populations. In spite of small numbers and a select patient population, our study reveals an interesting trend in TPMT genotypes in the Indian population. Nevertheless, a large population-based study would be required to confirm this finding.
Patients inheriting TPMT deficiency develop severe and life threatening hematopoietic toxicity on treatment with conventional doses of 6-MP. Patients heterozygous for TPMT variant allele are also at higher risk [10]. Lowering doses of 6-MP in TPMT heterozygotes and in deficient patients allowed administration of full protocol doses of other chemotherapy while maintaining high thioguanine nucleotide concentrations [10]. Evans et al. [24] noted a significant (>sixfold) overrepresentation of TPMT deficiency or heterozygosity among patients developing dose-limiting hematopoietic toxicity from therapy containing thiopurines. Conversely no increased hematological toxicity was noted in patients heterozygous for TPMT polymorphisms by McLeod et al. [25]. In our pediatric population, there was a dose reduction for 15 patients (15/66), but among them only three were carriers for TPMT*3C allele out of which one patient exhibiting compound heterozygosity had a significant dose reduction. However, in the adult group, 9 out of 32 patients had a dose reduction, but none had TPMT variant alleles. This implies that apart from commonly studied polymorphisms, various other rare polymorphic alleles in the TPMT gene might have an effect on this toxicity. Other novel variants in TPMT or variations in the genes involved in transport and biotransformation of 6-MP need to be evaluated in the Indian population.
References
Weinshilboum RM, Sladek SL. Mercaptopurine pharmacogenetics: monogenic inheritance of erythrocyte thiopurine methyltransferase activity. Am J Hum Genet. 1980;32(5):651–62.
Krynetski EY, Tai HL, Yates CR, et al. Genetic polymorphism of thiopurine S-methyltransferase: clinical importance and molecular mechanisms. Pharmacogenetics. 1996;6(4):279–90.
McLeod HL, Pritchard SC, Githang’a J, et al. Ethnic differences in thiopurine methyltransferase pharmacogenetics: evidence for allele specificity in Caucasian and Kenyan individuals. Pharmacogenetics. 1999;9(6):773–6.
Tai HL, Krynetski EY, Yates CR, et al. Thiopurine S-methyltransferase deficiency: two nucleotide transitions define the most prevalent mutant allele associated with loss of catalytic activity in Caucasians. Am J Hum Genet. 1996;58(4):694–702.
Yates CR, Krynetski EY, Loennechen T, et al. Molecular diagnosis of thiopurine S-methyltransferase deficiency: genetic basis for azathioprine and mercaptopurine intolerance. Ann Intern Med. 1997;126(8):608–14.
Otterness DM, Szumlanski CL, Wood TC, Weinshilboum RM. Human thiopurine methyltransferase pharmacogenetics. Kindred with a terminal exon splice junction mutation that results in loss of activity. J Clin Invest. 1998;101(5):1036–44.
Otterness D, Szumlanski C, Lennard L, et al. Human thiopurine methyltransferase pharmacogenetics: gene sequence polymorphisms. Clin Pharmacol Ther. 1997;62(1):60–73.
McLeod HL, Krynetski EY, Relling MV, Evans WE. Genetic polymorphism of thiopurine methyltransferase and its clinical relevance for childhood acute lymphoblastic leukemia. Leukemia. 2000;14(4):567–72.
Corominas H, Baiget M. Clinical utility of thiopurine S-methyltransferase genotyping. Am J Pharmacogenomics. 2004;4(1):1–8.
Relling MV, Hancock ML, Rivera GK, et al. Mercaptopurine therapy intolerance and heterozygosity at the thiopurine S-methyltransferase gene locus. J Natl Cancer Inst. 1999;91(23):2001–8.
McLeod HL, Relling MV, Liu Q, et al. Polymorphic thiopurine methyltransferase in erythrocytes is indicative of activity in leukemic blasts from children with acute lymphoblastic leukemia. Blood. 1995;85(7):1897–902.
Brenner TL, Pui CH, Evan WE. Pharmacogenomics of childhood acute lymphoblastic leukemia. Curr Opin Mol Ther. 2001;3(6):567–78.
McLeod HL, Siva C. The thiopurine S-methyltransferase gene locus—implications for clinical pharmacogenomics. Pharmacogenomics. 2002;3(1):89–98.
Bajel A, George B, Mathews V, et al. Treatment of children with acute lymphoblastic leukemia in India using a BFM protocol. Pediatr Blood Cancer. 2008;51(5):621–5.
Bajel A, George B, Mathews V, et al. Adult ALL: treatment outcome and prognostic factors in an Indian population using a modified German ALL (GMALL) protocol. Leukemia. 2007;21(10):2230–3.
Stanulla M, Schaeffeler E, Moricke A, et al. Thiopurine methyltransferase genetics is not a major risk factor for secondary malignant neoplasms after treatment of childhood acute lymphoblastic leukemia on Berlin-Frankfurt-Munster protocols. Blood. 2009;114(7):1314–8.
Kham SK, Tan PL, Tay AH, et al. Thiopurine methyltransferase polymorphisms in a multiracial asian population and children with acute lymphoblastic leukemia. J Pediatr Hematol Oncol. 2002;24(5):353–9.
Ameyaw MM, Collie-Duguid ES, Powrie RH, et al. Thiopurine methyltransferase alleles in British and Ghanaian populations. Hum Mol Genet. 1999;8(2):367–70.
Kham SK, Soh CK, Liu TC, et al. Thiopurine S-methyltransferase activity in three major Asian populations: a population-based study in Singapore. Eur J Clin Pharmacol. 2008;64(4):373–9.
Collie-Duguid ES, Pritchard SC, Powrie RH, et al. The frequency and distribution of thiopurine methyltransferase alleles in Caucasian and Asian populations. Pharmacogenetics. 1999;9(1):37–42.
Schaeffeler E, Fischer C, Brockmeier D, et al. Comprehensive analysis of thiopurine S-methyltransferase phenotype-genotype correlation in a large population of German-Caucasians and identification of novel TPMT variants. Pharmacogenetics. 2004;14(7):407–17.
Ganiere-Monteil C, Medard Y, Lejus C, et al. Phenotype and genotype for thiopurine methyltransferase activity in the French Caucasian population: impact of age. Eur J Clin Pharmacol. 2004;60(2):89–96.
Boson WL, Romano-Silva MA, Correa H, et al. Thiopurine methyltransferase polymorphisms in a Brazilian population. Pharmacogenomics J. 2003;3(3):178–82.
Evans WE, Hon YY, Bomgaars L, et al. Preponderance of thiopurine S-methyltransferase deficiency and heterozygosity among patients intolerant to mercaptopurine or azathioprine. J Clin Oncol. 2001;19(8):2293–301.
McLeod HL, Coulthard S, Thomas AE, et al. Analysis of thiopurine methyltransferase variant alleles in childhood acute lymphoblastic leukaemia. Br J Haematol. 1999;105(3):696–700.
Spire-Vayron de la Moureyre C, Debuysere H, Mastain B, et al. Genotypic and phenotypic analysis of the polymorphic thiopurine S-methyltransferase gene (TPMT) in a European population. Br J Pharmacol. 1998;125(4):879–87.
Stanulla M, Schaeffeler E, Flohr T, et al. Thiopurine methyltransferase (TPMT) genotype and early treatment response to mercaptopurine in childhood acute lymphoblastic leukemia. Jama. 2005;293(12):1485–9.
Ma XL, Zhu P, Wu MY, et al. Relationship between single nucleotide polymorphisms in thiopurine methyltransferase gene and tolerance to thiopurines in acute leukemia. Zhonghua Er Ke Za Zhi. 2003;41(12):929–33.
Hongeng S, Sasanakul W, Chuansumrit A, et al. Frequency of thiopurine S-methyltransferase genetic variation in Thai children with acute leukemia. Med Pediatr Oncol. 2000;35(4):410–4.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Desire, S., Balasubramanian, P., Bajel, A. et al. Frequency of TPMT alleles in Indian patients with acute lymphatic leukemia and effect on the dose of 6-mercaptopurine. Med Oncol 27, 1046–1049 (2010). https://doi.org/10.1007/s12032-009-9331-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12032-009-9331-8