Abstract
Objective
Thiopurine drugs are commonly used in pediatric patients for the treatment of acute leukemia, organ transplantation and inflammatory diseases. They are catabolized by the cytosolic thiopurine methyltransferase (TPMT), which is subject to a genetic polymorphism. In children, enzyme activities are immature at birth and developmental patterns vary widely from one enzyme to another. The present study was undertaken to evaluate erythrocyte TPMT activity and the correlation between genotype and phenotype in different age groups from birth to adolescence and adulthood.
Methods
The study included 304 healthy adult blood donors, 147 children and 18 neonates (cord bloods). TPMT activity was measured by liquid chromatography, and genotype was determined using a polymerase chain reaction reverse dot-blot analysis identifying the predominant TPMT mutant alleles (TPMT*3A, TPMT*3B, TPMT*3C, TPMT*2).
Results
There was no significant difference in TPMT activity between cord bloods (n=18) and children (n=147) (17.48±4.04 versus 18.62±4.14 respectively, P=0.424). However, TPMT was significantly lower in children than in adults (19.34±4.09) (P=0.033). In the whole population, there were 91.9% homozygous wild type, 7.9% heterozygous mutants and 0.2% homozygous mutants. The frequency of mutant alleles was 3.0% for TPMT*3A, 0.7% for TPMT*2 and 0.4% for TPMT*3C.
Conclusion
No impact of child development on TPMT activity could be evidenced, suggesting that TPMT activity is already mature at birth. The difference between children and adults was low with reduced clinical impact expected. When individual TPMT activity was compared with genotype, there was an overlapping region where subjects (4.5%, 12 adults, 9 children) were either homozygous wild type or heterozygous, with a TPMT activity below the antimode value. This result highlighted the importance of measuring TPMT activity to detect all patients at risk of thiopurine toxicity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thiopurine methyltransferase (TPMT, EC 2.1.1.67) is a cytosolic enzyme which catalyses the S-methylation of thiopurine drugs such as 6-mercaptopurine (6-MP) and 6-thioguanine (6-TG) [1, 2]. It is present in various organs (liver, kidneys) and cells (erythrocytes, leukocytes). Its physiological role remains unknown and there is no endogenous substrate identified [3].
TPMT activity can be measured in red blood cells using a radiochemical method [4, 5] or a high-performance liquid chromatography (HPLC) assay [6]. It is highly variable and under genetic control. The distribution of TPMT activity in adult volunteers appears trimodal in initial reports: approximately 89% of Caucasians are homozygous for the high activity allele, 11% are heterozygous and 1 subject in 300 inherits TPMT deficiency as an autosomal recessive trait [7]. The gene (34 Kb) is located on chromosome 6 (6 p22.3) and has 10 exons and 9 introns [8, 9]. To date, 13 mutant alleles have been associated with deficient TPMT activity [10] but 3 mutated alleles (TPMT*2, TPMT*3A, TPMT*3C) account for 80–95% of intermediate or low activity cases [11, 12]: TPMT*2 carries a single nucleotide transversion (G238C) in the open reading frame (exon 5) leading to an amino acid substitution at codon 80 (Ala→Pro) [13], TPMT*3A contains two nucleotide transition mutations [G460A (exon 7) and A719G (exon 10)], leading to amino acid substitutions respectively at codon 154 (Ala→Thr) and codon 240 (Tyr→Cys) [14] and TPMT*3C carries the single transition A719G (exon 10). Most genotyping studies use allele-specific polymerase chain reaction (PCR) or PCR-restriction fragment length polymorphism (RFLP) in order to detect these three single nucleotide polymorphisms (SNPs) [11, 12]. The SNP prevalence varies according to the ethnic origin [15]. Heterologous expression in yeast established an enhanced rate of proteolysis of mutant TPMT encoded by TPMT*2 and TPMT*3A alleles, with degradation half-lives of approximately 15 min for both mutant proteins compared with 18 h for the wild-type protein [16]. This rapid degradation is performed in part through a ubiquitin-proteasome-mediated process [16]. Chaperone proteins seems also to be involved in targeting TPMT for degradation [17].
TPMT catabolizes the thiopurine drugs 6-MP and thioguanine for treatment of adults and children with leukemia [15, 18] or chronic inflammatory diseases [19]. Patients with a deficient TPMT activity are at high risk of hematopoietic toxicity [20, 21]. Moreover, some authors describe a possible risk of secondary myelodysplasia or acute myeloid leukemia [22] or secondary brain tumors after cranial radiotherapy [23].
The impact of age has been demonstrated for many drug-metabolizing enzymes [24]. Thus, we studied the impact of age on TPMT activity by comparing TPMT activity in healthy young Caucasians from birth (by the use of cord blood) to adolescence with adult Caucasians. TPMT phenotype and genotype were determined and their correlation within the different age groups was examined.
Methods
The study was approved by the ethics committee of the two participating centers. A written informed consent was obtained from all adult subjects and from all the children’s parents.
Subjects
A questionnaire was filled for all the patients. The data age, sex and ethnicity were collected and only Caucasians were included. Patients with a past history of acute, chronic or genetic diseases and/or receiving medications were not included.
Adults were 304 blood donors, 229 men and 75 women, aged 40.9±10.0 years (mean±SD). Children (n=147) were hospitalized for day-care surgery: they were 97 boys and 50 girls, aged 5.7±4.2 years. For one child, blood could not be available for genotype. Eighteen umbilical cord bloods were obtained after normal pregnancy. They were 11 girls and 7 boys, with an Apgar score over 9 at 5 min. Birth weight was 3401±354 g and term was 40±1.2 week’s gestation.
Blood samples were collected in 3-ml tubes containing ethylene diamine tetraacetic acid (EDTA) for genotype and 3-ml tubes containing lithium heparin for phenotype determination. The volume of blood was reduced (1–2 ml) for the youngest children.
HPLC assay for red-cell TPMT activity determination
Erythrocyte lysate preparation and incubation conditions were similar to those previously described by Jacqz-Aigrain et al. [6]. Erythrocyte lysates were kept at −80°C until analysis. After slow thawing, magnesium chelation was performed by addition of Chelex 100 resin. During incubation, phosphate buffer replaced cofactors solution (S-adenosyl-l-methionine, dithiotreitol, allopurinol) in the blank tubes. The enzymatic reaction was stopped after 60 min at 37°C by addition of 50 μl perchloric acid (70–72%). After vortex stirring and centrifugation (10 min at 4°C), the amount of 6-methylmercaptopurine formed during incubation was measured by liquid chromatography: 75 μl supernatant was injected into the chromatographic system. The chromatographic conditions were reported elsewhere [25]. Briefly, the mobile phase consisted of water-acetonitrile-triethylamine (91.7:8:0.03, v/v) with dithiotreitol 0.65 mM, adjusted to pH 3.2 with o-phosphoric acid. The flow rate was 1 ml min−1, the detection wavelength 290 nm and 75 μl acetonitrile was injected between two samples. TPMT activities were determined in the two different sites, after blinded assessment of 20 samples showing a significant correlation between the two HPLC methods measuring TPMT activity (y=1.059x+0.019; r2=0.682; P<0.001).
The calibration curve was linear over the range of 5–150 ng ml−1 6-methylmercaptopurine. The precision was studied by adding 6-methylmercaptopurine to erythrocyte lysate at three different concentrations (25, 75, 125 ng ml−1). The intra-day and inter-days coefficients of variation were 1.7–4.3% (n=6) and 0.8–6.0% (n=6) for both laboratories. The limit of detection was 5 ng ml−1 and the limit of quantification 10 ng ml−1. Quality controls (TPMT activity measured in adult volunteers) showed inter-assay variations of 5.8% (n=20) and 5.2% (n=5) for a mean TPMT activity of 19.4 nmol h−1 ml−1 and 17.6 nmol h−1 ml−1 packed red blood cells (PRBC) (U/ml PRBC) for two different erythrocyte lysates analyzed, respectively, in each laboratory.
Determination of TPMT genotype by PCR-reverse dot blot
DNA was extracted using an erythrocyte differential lysis with ammonium carbonate buffer, followed by a leukocyte lysis obtained using proteinase K and tensioactive agents (Tween 20). DNA fragments were amplified by means of PCR. We searched SNPs on exons 5, 7 and 10 to detect variant alleles TPMT *2, *3A, *3B and *3C. The following 5′ biotinylated oligonucleotide forward primers (FP) and reverse primers (RP) were used: exon 5-FP: 5′-GCTTACTCTAATATAACCCTCTA-3′; exon 5-RP: 5′-CTTTTGTGGGGATATGGATACA-3′; exon 7-FP: 5′-CGATTGTTGAAGTACCAGCAT-3′; exon 7-RP: 5′-CTAGAACCCAGAAAAAGTATAGT-3′; exon 10-FP: 5′B-AATCCCTGATGTCATTCTTCATA-3′; exon 10-RP: 5′B-TTCAATTCCTCAAAAACATGTCA-3′.
The amplified fragment size were 253 bp (exon 5), 242 bp (exon 7), 219 bp (exon 10). The amplification reaction was carried out in a total volume of 50 μl in the presence of 100 ng DNA, 0.01 mM TrisHCl pH 7.5, 0.05 mM KCl, 2.5 mM MgCl2, 0.025 μl Tween 20, 0.1 mM each dNTP, 0.2 μM each primer, and 0.08 U Taq DNA polymerase. The amplification profile of the thermocycler (Applied Biosystems 9700, Les Ulis, France) consisted of an initial denaturation step of 95°C for 5 min, a hybridization step for 2 min at 55°C followed by 30 cycles of denaturation at 95°C for 30 s, annealing at 55°C for 30 s, extension at 72°C for 30 s and a final extension at 72°C for 2 min. Mutations were identified by a reverse dot-blot assay performed on amplified DNA. This technique used allele specific oligonucleotides (ASO) linked to a membrane. The amino-linked oligonucleotide sequences for normal alleles (wt) and alleles with SNP were:
- Exon 5-wt:
-
5′NH2-TATGCAGGTTTGCAGACC-3′
- Exon 5-SNP:
-
5′NH2-GGTCTGGAAACCTGCATA-3′
- Exon 7-wt:
-
5′NH2-ACTAATGCTCCTCTATCC-3′
- Exon 7-SNP:
-
5′NH2-GATAGAGGAACATTAGTTG-3′
- Exon 10-wt:
-
5′NH2-GAAAAGTTATATCTACTTACA-3′
- Exon 10-SNP:
-
5′NH2-GTAAGTAGACATAACTTTTCA-3′
After a DNA denaturation step, hybridization with ASO was realized at specific temperatures (46°C for G238C, 42°C for G460A and A719G). After a washing step, the streptavidine-peroxydase conjugate added bound with biotine of amplified DNA. After other washing steps, the addition of 3,3′, 5,5′-tetramethylbenzidine (chromogene substrate of streptavidine-peroxydase) gives a blue spot on the membrane in presence of hydrogen peroxide. Blanks and controls (known homozygote wild-type DNA, heterozygote DNA, homozygote mutant DNA except G238C/G238C) were included into each batch and always gave expected results.
Data analysis
Statistical analysis was performed using Systat 9.0 for Windows (SPSS Inc, Chicago, Ill). Results are expressed as mean±standard deviation. According to the central limit theorem for big-size groups (n>30), t-tests were used to compare TPMT activity between two groups and ANOVA for more than two groups. ANOVA was used to test simultaneously the effect of age and gender on children’s TPMT activity. Correlations were studied using the Pearson coefficient for quantitative variables and Spearman coefficient for quantitative non-continued variables. Non-parametric tests were used for the analysis of TPMT in cord blood. A P value less than 0.05 was considered as significant. Confidence intervals (CI) are presented at 95%.
Results
TPMT phenotype and genotype were determined in a population of 469 healthy Caucasian subjects (except one genotype for a child): there were 304 adults, 147 children and 18 neonates (cord blood).
Adults
TPMT activity (n=304) ranged from 0.43 nmol h−1 ml−1 to 30.38 nmol h−1 ml−1 PRBC. The frequency distribution histogram appeared optically trimodal (Fig. 1a). On the probit plot (not shown), we could see three groups of results: one individual had a very low TPMT activity of 0.43 U/ml PRBC, intermediate activities were between 7.14 nmol h−1 ml−1 and 12.01 nmol h−1 ml−1 PRBC and high activities were between 13.27 nmol h−1 ml−1 and 30.38 nmol h−1 ml−1 PRBC. Mean TPMT activity was 19.34±4.09 nmol h−1 ml−1 PRBC with no significant difference between men and women (19.55±4.25 nmol h−1 ml−1 versus 18.61±3.59 nmol h−1 ml−1 PRBC, respectively, P=0.057).
Genotype results are presented in Table 1. The frequency of homozygous wild type is 92.1%. One adult individual had a homozygous mutated genotype *3A/*3A. Twenty-three (7.6%) individuals were heterozygous. The mutant allele TPMT*3A (n=18) was predominant, while TPMT*2 (n=3) and TPMT *3C (n=2) were less frequent.
The correlation between individual phenotype and genotype was analyzed. The homozygous deficient individual (*3A/*3A) had the lowest TPMT activity of 0.43 nmol h−1 ml−1 PRBC. TPMT activity ranged from 7.14 U/ml to 13.34 U/ml PRBC in heterozygous individuals and from 10.82 nmol h−1 ml−1 to 30.38 nmol h−1 ml−1 PRBC in homozygous wild-type individuals. Twelve subjects had a TPMT activity between 10.82 nmol h−1 ml−1 and 13.34 nmol h−1 ml−1 PRBC, within an overlapping region between heterozygous or homozygous wild-type individuals.
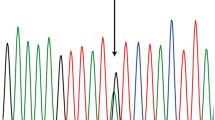
Children
TPMT activity was 18.62±4.14 nmol h−1 ml−1 PRBC (range 8.25–30.0; n=147) and it was 17.48±4.04 nmol h−1 ml−1 PRBC (range 9.24–22.79) in cord bloods (n=18). There was no significant difference in TPMT activity between the two groups (P=0.424). Therefore, the data obtained in children and in cord blood were pooled in a unique group (n=165) with a TPMT activity of 18.49±4.13. The corresponding frequency distribution histogram appeared bimodal (Fig. 1b). We did not observe any influence of gender and age on TPMT activity (P=0.310). Mean TPMT activity for boys and girls was, respectively, 18.34±4.21 and 18.87±3.98. When children were separated into five age groups (Table 2) and heterozygous children were withdrawn to remove the influence of the genetic factor, TPMT activity was not significantly different between the five groups (P=0.492). In addition, there was no significant correlation between TPMT activity and individual erythrocyte counts (P=0.976) or reticulocyte counts (P=0.145). In addition, there was no significant correlation between TPMT activity in cord blood and fetal hemoglobin (P=0.88) or term at birth (P=0.95).
Of the children, 150 (91.5%) had a homozygous wild-type genotype and 14 (8.5%) were heterozygous. The mutant allele TPMT*3A was predominant followed by TPMT*2 and TPMT*3C (Table 1).
The correlation between individual phenotype and genotype showed a TPMT activity ranging from 8.25 nmol h−1 ml−1 to 13.05 nmol h−1 ml−1 PRBC in heterozygous children and from 9.95 nmol h−1 ml−1 to 30.00 nmol h−1 ml−1 PRBC in homozygous children, with 9 children having a TPMT activity within an overlapping region of 9.95 nmol h−1 ml−1 to 13.05 nmol h−1 ml−1 PRBC.
Comparison adult/children
TPMT activity was significantly lower in children than in adults (P=0.033).
When the whole group of individuals (n=468) was considered, 91.9% (CI 88.2–94.5) were homozygous wild type, 7.9% (CI 5.2–11.3) were heterozygous mutants and one individual (0.2%, CI 0.0–1.4) was a homozygous mutant. The frequency of mutant alleles was 3.0% (CI 1.8–4.7) (n=28) for TPMT*3A, 0.7% (CI 0.2–1.8) (n=7) for TPMT*2 and 0.4% (CI 0.1–1.3) (n=4) for TPMT*3C.
The overlapping regions comprised 12 adults (TPMT activity 10.82–13.34) and 9 children (TPMT activity 9.95–13.05)—(Fig. 2) or 21 subjects (4.5%) for the entire group. Among these subjects, 18 (3.8%) were heterozygous and 3 (0.6%) were homozygous. If the higher limit of TPMT activity in the heterozygous group is selected, 3 individuals (1 adult and 2 children) would have been classified as heterozygous but were homozygous wild type at the genotype level.
The correlation between phenotype and genotype showed that the antimode between intermediate and high activity had a value close to 13.5, because all subjects (adults and children) with a TPMT activity above 13.5 had a wild-type genotype, and the majority of the individuals below 13.5 was heterozygous.
Discussion
Most drug-metabolizing enzymes are immature during fetal life and at birth and reach adult activities after a few months [26] or years [27, 28, 29]. Therefore, in addition to genetic factors, the impact of ontogeny should be analyzed in pediatric populations [24, 30]. In the present study, we investigated the developmental pharmacogenetics of TPMT activity. We compared TPMT activity in large groups of adults and children and showed that there was no major impact of child development on TPMT activity. However, we evidenced a slightly lower TPMT activity in children than adults. The phenotype was correlated with genotype in both age groups in almost all subjects.
Thiopurine drugs are widely administered both in adult and pediatric patients. Major indications include leukemia occurring primarily during childhood [18, 31], chronic inflammatory bowel diseases [32], organ transplantations [33], and rheumatoid [34] and dermatological diseases [35]. These drugs are highly metabolized through three competing pathways, TPMT being a catabolic pathway under genetic control [7].
In order to investigate the impact of age on TPMT activity, we first studied an adult population of 304 healthy volunteers. The frequency distribution histogram appeared trimodal, in agreement with the reference data initially published by Weinshilboum and Sladek [7]. In our population, there was no gender difference as in previous studies [6, 7, 36, 37].
Some data studying the developmental aspects of TPMT activity have already been published. Pacifici et al. [38] showed that TPMT activity was three times lower in the human fetal liver at midgestation than in the adult liver. The data by Ferroni et al. [36] and McLeod et al. [3] reported that TPMT activity was higher in cord and peripheral blood at birth than in adults, while TPMT activity was similar in children aged 4–23 years and in adults [18]. In contrast, we did not evidence differences in TPMT activity between neonates at birth, infants and children. Our data did not show a gender difference for children, in agreement with other studies in children [39, 40]. Differences among studies, particularly in the determination of TPMT activity at birth, may be related to analytical differences. High TPMT activities in cord blood were measured by radiochemical method [3, 36] and 6-methylmercaptopurine may have been overestimated while we used a HPLC method that specifically measured 6-methylmercaptopurine. In the whole children population, TPMT activity was lower than in adults. Nevertheless, the difference was low and the clinical impact is expected to be reduced. In a Norwegian control population, Petterson et al. [41] found a significantly higher TPMT activity in children (n=71) than adults (n=219). The difference with our study may be due to a higher TPMT activity in Norwegian children than in French Caucasian children. In our study, we concluded that no impact of development could be detected in children from birth to adolescence. Consequently, TPMT appears functional in infants and children and dosage adjustment should not be required in the youngest patients treated with thiopurines.
We determined TPMT genotypes in a large group of Caucasians (n=468), including both adults and children. As expected, the homozygous TPMT wild-type patients were predominant and the frequency of heterozygous subjects (7.9%) was very close to the frequencies reported in other Caucasian populations already studied ranging from 7.4% to 9.6% [12, 42, 43]. The TPMT*3A variant allele was predominant in these three studies with frequencies ranging from 3.2% to 5.7% as in our study (3.0%). The TPMT*3C and TPMT*2 mutant alleles were detected at lower frequencies, TPMT*2 being more frequent than TPMT*3C.
The correlation between phenotype and genotype was also studied in the whole group of adults and children. There was an overlap in TPMT activity between homozygous wild-type and heterozygous subjects but only 21 subjects (4.5%) (12 adults and 9 children) were concerned. This is in agreement with previous studies that showed a good correlation between phenotype and genotype in healthy non-treated patients [11, 12, 37]. The reasons for the overlap that we observed may be related to the measurement of TPMT activity (although all TPMT below 15.0 U/ml PRBC were assayed in triplicate), to the possible impact of environmental factors. The role of the polymorphic variable number of tandem repeats in the 5′ flanking region of the TPMT gene modulating gene expression [44] is controversially discussed [45]. In addition, other rare SNPs in the open reading frame of the TPMT gene [15] exist and were not tested here. A few new SNPs have been recently evidenced [10, 46]. These rare polymorphisms could be at the origin of a misidentified wild-type allele. Three subjects in the overlapping region had a low activity and were homozygous wild type. Such individuals have already been identified in previous studies [11, 47] where DNA was sequenced and no other polymorphism was detected inside the coding region. The correlation between phenotype and genotype showed that the antimode value of TPMT activity separating the majority of homozygous wild-type and heterozygous subjects was close to 13.5 both for adults and children. This enables classification of patients as either high or intermediate methylators before starting thiopurine treatment. The antimode values may be different according to the analytical method. For radiochemical technique [7], deficient TPMT activity is below 5.0, intermediate activity between 5.0 and 10.0, and high activity above 10.0 U/ml PRBC. The HPLC method using 6-TG instead of 6-MP has a cut-off value between intermediate and high activity of 23.5 nmol/g Hb/h [48], since TPMT activity was 34% lower with 6-MP substrate than with 6-TG [49].
What is essential, is to identify all patients at risk of hematotoxicity [20], secondary myelodysplasia or acute myeloid leukemia [22], secondary brain tumors after cranial radiotherapy [23]. Most of these patients have a deficient TPMT activity associated with a homozygous mutated or heterozygous genotype [21]. Others, more scarce, have a wild-type genotype with a TPMT activity either deficient or near but above the antimode value [21, 22]. This fact highlights the importance of measuring TPMT activity. Which analysis (genotype or phenotype) the physician requires depends on the clinical situation. First, at diagnosis of inflammatory bowel disease (adults and children), rheumatoid and dermatological disease, we can recommend TPMT phenotype, to be sure to detect rare patients with low TPMT activity associated with non-mutated genotype. Second, at diagnosis of children LAL, TPMT activity is significantly lower than in the reference children population, due, at least in part, to an excess of old erythrocytes with low TPMT activity [50]. Thus, the genotype will certainly give the most appropriate information. Genotype is also the single available test for patients who received donor erythrocyte transfusions within the past 2–3 months. Misinterpretation of the constitutive deficient TPMT phenotype due to previous erythrocyte transfusion led to serious hematotoxicity in a few clinical situations [51, 52]. Finally, when patients are already under treatment, TPMT activity is sometimes modified. Thiopurines induce TPMT activity [18] with a mean increase of 30–35%. The phenotype is a possible test, when raising the antimode value in the same proportion [21]. An alteration (decrease) of TPMT activity for patients with inflammatory bowel disease treated with 5-aminosalicylic acid (5-ASA) formulations is controversially discussed. However, an increased risk to develop leucopenia under co-medication with 6-MP or azathioprine needs to be taken into account [53]. For all these patients, the genotype is available and can be a choice to detect TPMT deficiency.
From the technical point of view, the genotype at the three major SNPs can be assayed in any laboratory realizing genetic analysis in routine with an identical response from one laboratory to another. In contrast, the measurement of TPMT activity with different methods (radiochemical or chromatographic) or using modified parameters (incubation with Chelex 100 resin or not, various SAM concentrations) can give different TPMT values. Therefore, each laboratory has to test a reference population (phenotype and genotype) to have its own reference and antimode values.
In conclusion, we determined TPMT phenotype and genotype in a French healthy Caucasian population including both adults and children. No impact of development on TPMT activity during childhood could be evidenced, suggesting that TPMT activity is already mature at birth. TPMT activity seems to be slightly lower in children than adults. Only one subject (0.2%) was homozygous mutant and the proportion of heterozygous subjects was 7.9% (CI 5.2–11.3), *3A being the preponderant mutant allele. In the whole population, the comparison between phenotype and genotype showed that a limited number of patients having a TPMT activity close to the antimode value could be either homozygous wild-type or heterozygous subjects. According to this data, different clinical situations were considered to evaluate whether genotype or phenotype is the most appropriate test to detect patients at risk of thiopurine toxicity.
References
Remy CN (1963) Metabolism of thiopyrimidines and thiopurines: S-methylation with S-adenosylmethionine transmethylase and catabolism in mammalian tissue. J Biol Chem 238:1078–1084
Woodson LC, Weinshilboum RM (1983) Human kidney thiopurine methyltransferase: purification and biochemical properties. Biochem Pharmacol 32:819–826
McLeod HL, Krynetski EY, Wilimas JA, Evans WE (1995) Higher activity of polymorphic thiopurine-S-methyltransferase in erythrocytes from neonates compared to adults. Pharmacogenetics 5:281–286
Weinshilboum RM, Raymond FA, Pazmino PA (1978) Human erythrocyte thiopurine methyltransferase: radiochemical microassay and biochemical properties. Clin Chim Acta 85:323–333
McLeod HL, Lin JS, Scott EP, Pui CH, Evans WE (1994) Thiopurine methyltransferase activity in American white subjects and black subjects. Clin Pharmacol Ther 55:15–20
Jacqz-Aigrain E, Bessa E, Medard Y, Mircheva Y, Vilmer E (1994) Thiopurine methyltransferase activity in a French population: HPLC assay conditions and effects of drugs and inhibitors. Br J Clin Pharmacol 38:1–8
Weinshilboum RM, Sladek SL (1980) Mercaptopurine pharmacogenetics: monogenic inheritance of erythrocyte thiopurine methyltransferase activity. Am J Hum Genet 32:651–662
Szumlanski C, Otterness D, Her C, Lee D, Brandriff B, Kelsell D et al (1996) Thiopurine methyltransferase pharmacogenetics: human gene cloning and characterization of a common polymorphism. DNA Cell Biol 15:17–30
Krynetski EY, Fessing MY, Yates CR, Sun D, Schuetz JD, Evans WE (1997) Promoter and intronic sequences of the human thiopurine-S-methyltransferase (TPMT) gene isolated from a human PACI genomic library. Pharm Res 14:1672–1678
Hamdan-Khalil R, Allorge D, Lo-Guidice JM, Cauffiez C, Chevalier D, Spire C et al (2003) In vitro characterization of four novel non-functional variants of the thiopurine S-methyltransferase. Biochem Biophys Res Commun 309:1005–1010
Otterness D, Szumlanski C, Lennard L, Klemetsdal B, Aarbakke J, Park-Hah JO et al (1997) Human thiopurine methyltransferase pharmacogenetics: gene sequence polymorphisms. Clin Pharmacol Ther 62:60–73
Yates CR, Krynetski EY, Loennechen T, Fessing MY, Tai HL, Pui CH et al (1997) Molecular diagnosis of thiopurine S-methyltransferase deficiency: genetic basis for azathioprine and mercaptopurine intolerance. Ann Intern Med 126:608–614
Krynetski EY, Schuetz JD, Galpin AJ, Pui CH, Relling MV, Evans WE (1995) A single point mutation leading to loss of catalytic activity in human thiopurine S-methyltransferase. Proc Natl Acad Sci U S A 92:949–953
Tai HL, Krynetski EY, Yates CR, Loennechen T, Fessing MY, Krynetskaia NF et al (1996) Thiopurine-S-methyltransferase deficiency: two nucleotide transitions define the most prevalent mutant allele associated with loss of catalytic activity in Caucasians. Am J Hum Genet 58:694–702
McLeod HL, Krynetski EY, Relling MV, Evans WE (2000) Genetic polymorphism of thiopurine methyltransferase and its clinical relevance for childhood acute lymphoblastic leukemia. Leukemia 14:567–572
Tai HL, Krynetski EY, Schuetz EG, Yanishevsky Y, Evans WE (1997) Enhanced proteolysis of thiopurine-S-methyltransferase (TPMT) encoded by mutant alleles in humans (TPMT*3A, TPMT*2): mechanisms for the genetic polymorphism of TPMT activity. Proc Natl Acad Sci U S A 94:6444–6449
Wang L, Sullivan W, Toft D, Weinshilboum R (2003) Thiopurine S-methyltransferase pharmacogenetics: chaperone protein association and allozyme degradation. Pharmacogenetics 13:555–564
Lennard L, Lilleyman JS, Van Loon J, Weinshilboum RM (1990) Genetic variation in response to 6-mercaptopurine for childhood acute lymphoblastic leukaemia. Lancet 336:225–229
Colombel JF, Ferrari N, Debuysere H, Marteau P, Gendre JP, Bonaz B et al (2000) Genotypic analysis of thiopurine-S-methyltransferase in patients with Crohn’s disease and severe myelosuppression during azathioprine therapy. Gastroenterology 118:1025–1030
Lennard L, Rees CA, Lilleyman JS, Maddocks JL (1983) Childhood leukemia: a relationship between intracellular 6-mercaptopurine metabolism and neutropenia. Br J Clin Pharmacol 16:359–363
Evans WE, Hon YY, Bomgaars L, Coutre S, Holdsworth M, Janco R et al (2001) Preponderance of thiopurine S-methyltransferase deficiency and heterozygosity among patients intolerant to mercaptopurine or azathioprine. J Clin Oncol 19:2293–2301
Bo Thomsen J, Schroder H, Kristinsson J, Madsen B, Szumlanski C, Weinshilboum RM et al (1999) Possible carcinogenic effect of 6-mercaptopurine on bone marrow stem cells. Cancer 86:1080–1086
Relling MV, Rubnitz JE, Rivera GK, Boyett JM, Hancock ML, Felix CA et al (1999) High incidence of secondary brain tumours after radiotherapy and antimetabolites. Lancet 354:34–39
Kearns GL (1995) Pharmacogenetics and development: are infants and children at increased risk for adverse outcomes? Curr Opin Pediatr 7:220–233
Ganiere-Monteil C, Pineau A, Kergueris MF, Azoulay C, Bourin M (1999) Thiopurine methyl transferase activity: new extraction conditions for high performance liquid chromatographic assay. J Chromatogr B 727:235–239
Cazeneuve C, Pons G, Rey E, Treluyer JM, Cresteil T, Thiroux G et al (1994) Biotransformation of caffeine in human liver microsomes from foetuses, neonates, infants and adults. Br J Clin Pharmacol 37:405–412
Pariente-Khayat A, Pons G, Rey E, Richard MO, D’Athis P, Moran C et al (1991) Caffeine acetylator phenotyping during maturation in infants. Pediatr Res 29:492–495
Hadasova E, Brysova V, Kadlcakova E (1990) N-Acetylation in healthy and diseased children. Eur J Clin Pharmacol 39:43–47
Jacqz-Aigrain E, Cresteil T (1992) Cytochrome P450-dependent metabolism of dextromethorphan: fetal and adult studies. Dev Pharmacol Ther 18:161–168
Leeder JS, Kearns GL (1997) Pharmacogenetics in pediatrics. Implications for practice. Ped Clin North Am 44:55–77
Dervieux T, Medard Y, Verpillat P, Guigonis V, Duval M, Lescoeur B, Suciu S, Vilmer E, Jacqz-Aigrain E (2001) Possible implication of thiopurine S-methyltransferase in occurrence of infectious episodes during maintenance therapy for childhood lymphoblastic leukemia with mercaptopurine. Leukemia 15:1706–1712
Paerregaard A, Schmiegelow (2002) Monitoring azathioprine metabolite levels and thiopurine methyltransferase (TPMT) activity in children with inflammatory bowel disease. Scand J Gastroenterol 37:371–372
Smith L, Morris M, Wrong W (1997) Renal transplantation in children: the Auckland experience 1980–1996. N Z Med J 110:202–204
Corominas H, Domenech M, Laiz M, Gich I, Geli C, Diaz C et al (2003) Is thiopurine methyltransferase genetic polymorphism a major factor for withdrawal of azathioprine in rheumatoid arthritis patients? Rheumatology 42:40–45
Murphy LA, Atherton D (2002) A retrospective evaluation of azathioprine in severe childhood atopic eczema, using thiopurine methyltransferase levels to exclude patients at high risk of myelosuppression. Br J Dermatol 147:308–315
Ferroni MA, Marchi G, Sansone E, Romeo P, Giulianotti PC, Pietrabissa A et al (1996) Variability in the rate of 6-mercaptopurine methylation in the erythrocytes, liver and kidney in an Italian population. Eur J Clin Pharmacol 51:23–29
Coulthard SA, Rabello C, Robson J, Howell C, Minto L, Middleton PG et al (2000) A comparison of molecular and enzyme-based assays for the detection of thiopurine methyltransferase mutations. Br J Haematol 110:599–604
Pacifici GM, Romiti P, Giliani L, Rane A (1991) Thiopurine methyltransferase in humans: development and tissue distribution. Dev Pharmacol Ther 17:16–23
Keizer-Garritsen JJ, Brouwer C, Lamboy LH, Ter Riet P, Bokkerink JP, Trijbels FJ, De Abreu RA (2003) Measurement of thiopurine S-methyltransferase activity in human blood samples based on high-performance liquid chromatography: reference values in erythrocytes from children. Ann Clin Biochem 40:86–93
Lennard L, Singleton HJ (1994) High-performance liquid chromatographic assay of red blood cell thiopurine methyltransferase activity. J Chromatogr B 661:25–33
Petterson B, Almer S, Albertioni F, Söderhäll S, Peterson C (2002) Differences between children and adults in thiopurine methyltransferase activity and metabolite formation during thiopurine therapy: possible role of concomitant methotrexate. Ther Drug Monit 24:351–358
Alves S, Amorim A, Ferreira F, Prata MJ (2001) Influence of the variable number of tandem repeats located in the promoter region of the thiopurine methyltransferase gene on enzymatic activity. Clin Pharmacol Ther 70:165–174
Ameyaw MM, Collie-Duguid ES, Powrie RH, Ofori-Adjei D, McLeod HL (1999) Thiopurine methyltransferase alleles in British and Ghanaian populations. Hum Mol Genet 8:367–370
Spire-Vayron de la Moureyre C, Debuysere H, Fazio F, Sergent E, Bernard C, Sabbagh N et al (1999) Characterization of a variable number tandem repeat region in the thiopurine S-methyltransferase gene promoter. Pharmacogenetics 9:189–198
Marinaki AM, Arenas M, Khan ZH, Lewis CM, Shobowale-Bakre el-M, Escuredo E et al (2003) Genetic determinants of the thiopurine methyltransferase intermediate activity phenotype in British Asians and Caucasians. Pharmacogenetics 13:97–105
Schaeffeler E, Stanulla M, Greil J, Schrappe M, Eichelbaum M, Zanger UM et al (2003) A novel TPMT missense mutation associated with TPMT deficiency in a 5-year-old boy with ALL. Leukemia 17:1422–1424
Hon YY, Fessing MY, Pui CH, Relling MV, Krynetski EY, Evans WE (1999) Polymorphism of the thiopurine S-methyltransferase gene in African-Americans. Hum Mol Genet 8:371–376
Kröplin T, Weyer N, Gutsche S, Iven H (1998) Thiopurine S-methyltransferase activity in human erythrocytes: a new HPLC method using 6-thioguanine as substrate. Eur J Clin Pharmacol 54:265–271
Kröplin T, Iven H (2000) Methylation of 6-mercaptopurine and 6-thioguanine by thiopurine S-methyltransferase. Eur J Clin Pharmacol 56:343–345
Lennard L, Chew TS, Lilleyman JS (2001) Human thiopurine methyltransferase activity varies with red blood cell age. Br J Clin Pharmacol 52:539–546
Cheung ST, Allan RN (2003) Mistaken identity: misclassification of TPMT phenotype following blood transfusion. Eur J Gastroenterol Hepatol 15:1245–1247
Schwab M, Schaeffeler E, Marx C, Zanger U, Aulitzky W, Eichelbaum M (2001) Shortcoming in the diagnosis of TPMT deficiency in a patient with Crohn’s disease using phenotyping only. Gastroenterology 121:500–506
Lowry PW, Franklin CL, Weaver AL, Szumlanski CL, Mays DC, Loftus EV et al (2001) Leucopenia resulting from a drug interaction between azathioprine or 6-mercaptopurine and mesalamine, sulphasalazine, or balsazide. Gut 49:656–664
Acknowledgements
We thank A. Benoussaidh, N. Ripoll and V. De Burgat for their technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ganiere-Monteil, C., Medard, Y., Lejus, C. et al. Phenotype and genotype for thiopurine methyltransferase activity in the French Caucasian population: impact of age. Eur J Clin Pharmacol 60, 89–96 (2004). https://doi.org/10.1007/s00228-004-0732-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-004-0732-5