Abstract
Despite considerable research, the mechanisms of neuropathic pain induced by excessive oxidative stress production and overload calcium ion (Ca2+) entry in dorsal root ganglion (DRG) remain substantially unidentified. The transient receptor potential melastatin 2 (TRPM2) and vanilloid 1 (TRPV1) channels are activated with different stimuli including oxidative stress. TRPM2 and TRPV1 have been shown to be involved in induction of neuropathic pain. However, the activation mechanisms of TRPM2 and TRPV1 via NADPH oxidase and protein kinase C (PKC) pathways are poorly understood. In this study, I investigated the roles of NADPH oxidase and PKC on Ca2+ entry through TRPM2 and TRPV1 channels in in vitro DRG neurons of rats. Rat DRG neurons were used in whole-cell patch clamp experiments. The H2O2-induced TRPM2 current densities were decreased by N-(p-amylcinnamoyl)anthranilic acid (ACA), and dose-dependent capsaicin (CAP) and H2O2-induced TRPV1 currents were inhibited by capsazepine (CPZ). The TRPV1 channel is activated in the DRG neurons by 0.01 mM capsaicin but not 0.001 mM or 0.05 mM capsaicin. TRPM2 and TRPV1 currents were increased by the PKC activator, phorbol myristate acetate (PMA), although the currents were decreased by ACA, CPZ, and the PKC inhibitor, bisindolylmaleimide I (BIM). Both channel currents were further increased by PMA + H2O2 as compared to H2O2 only. In the combined presence of PMA + BIM, no TRPM2 or TRPV1 currents were observed. The CAP and H2O2-induced TRPM2 current densities were also decreased by the NADPH oxidase inhibitors apocynin and N-Acetylcysteine. In conclusion, these results demonstrate a protective role for NADPH oxidase and PKC inhibitors on Ca2+ entry through TRPM2 and TRPV1 channels in DRG neurons. Since excessive oxidative stress production and Ca2+ entry are implicated in the pathophysiology of neuropathic pain, the findings may be relevant to the etiology and treatment of neuropathology in DRG neurons.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Worldwide, there is high incidence of neuropathic pain among pain types and 2–7% of adults currently suffer from chronic neuropathic pain (Callaghan et al. 2015). The pain rate also increases as a result of disease or certain disease treatments. For example, approximately 20% of people with cancer have cancer-related neuropathic pain due to the cancer itself, or due to the chemotherapy (Kallenborn-Gerhardt et al. 2013; Callaghan et al. 2015). Neuropathic pain is induced by lesions of the nervous system and sensitization of the nociceptive system resulting in allodynia and hyperalgesia, both of which are increased by the lesions (Kallenborn-Gerhardt et al. 2012; Nazıroğlu et al. 2012). Oxidative stress stimuli activate cation channels including transient receptor potential (TRP) melastatin 2 (TRPM2) and vanilloid 1 (TRPV1), both of which are highly expressed in the nerve terminals of dorsal root ganglion (DRG) neurons (Caterina et al. 1997; Fonfria et al. 2006; Özgül and Nazıroğlu 2012). Accumulating evidence suggests that excessive production of reactive oxygen species (ROS) including hydrogen peroxide (H2O2), as well as the hot chili pepper component, capsaicin, contributes to the sensitization in persistent pain of DRG neurons (Kallenborn-Gerhardt et al. 2012; Övey and Nazıroğlu 2015; Özdemir et al. 2016). Therefore, neuropathic pain associated with diabetes and mechanical injury, resulting from excessive ROS production and overload of Ca2+ entry, has been treated in animal models by administration of antioxidants (Sözbir and Nazıroğlu 2016; Özdemir et al. 2016; Kahya et al. 2017). However, the sources of ROS production and how ROS contribute to pain sensitization remain poorly understood. With respect to the relevant enzymatic sources of these ROS, the NADPH oxidase enzyme has received considerable attention (Kallenborn-Gerhardt et al. 2012).
The ROS-generating effects of NADPH oxidase in cells are well known. NADPH oxidases may be the primary source of ROS, initiating oxidative stress and converting other enzymes into an ROS-producing state (Wind et al. 2010) to eventually induce pain pathophysiology (Kallenborn-Gerhardt et al. 2013). However, there are some concerns about the specificity of compounds currently used as NADPH oxidase inhibitors. For example, one of the most frequently applied compounds, apocynin, which is a naturally occurring compound isolated from Picrorhiza kurroa, also demonstrates NADPH oxidase inhibitory (Kallenborn-Gerhardt et al. 2013) and antioxidant properties (Heumüller et al. 2008). Accumulating evidence indicates that interactions between NADPH oxidase enzymes and TRP channels are important sources of ROS contributing to peripheral pain sensitization. For example, NADPH oxidase activation was reported as a primary source of ROS production in the pain process (Ibi et al. 2008). Protein kinase C (PKC)-mediated phosphorylation of serine residues in TRPV1 resulted in increased sensitivity to hyperalgesia (Chung et al. 2015). Serine protein phosphorylation through modulation of PKC was markedly decreased in the human glioblastoma cell line by glutathione (GSH) (Lo et al. 2004). Cytosolic GSH depletion-induced oxidative stress activates TRPM2 and TRPV1 channels in DRG neurons (Özgül and Nazıroğlu 2012; Övey and Nazıroğlu 2015), although in both cases channel activation was blocked by N-acetylcysteine (NAC) and GSH treatments (Nazıroğlu et al. 2011; Nazıroğlu et al. 2013; Sözbir and Nazıroğlu 2016). PKC is a family of enzymes involved in numerous important cellular events in neurons, including pain modulation (Hackel et al. 2013) and oxidative stress. PKC induces over-production of ROS through different molecular pathways such as stimulation of NADPH oxidase. Bisindolylmaleimide I (BIM) is a PKC inhibitor, while phorbol myristate acetate (PMA) is an activator of PKC. In pulmonary smooth muscle cells, both PKC and NADPH oxidase pathways were reported to activate L-type voltage-gated Ca2+ channels (Chakraborti et al. 2009). Hence, BIM may modulate activation of TRPM2 and TRPV1 channels resulting from PMA-induced oxidative stress due to its PKC modulator effects.
Emerging evidence points to TRPM2 and TRPV1 channels as major pain transducers (Nazıroğlu 2007; Nazıroğlu et al. 2012). Due to their permeability to Ca2+, they exert a crucial regulatory function, most notably in pain modulation in DRG neurons (Nazıroğlu and Özgül 2013). TRPM2 has a special NUDT9 homology domain and enzymatic activity (adenosine 5′-diphosphoribose (ADPR) pyrophosphatase enzyme) located at the C-terminus of the channel. If the domain is activated by ADPR in the presence of extracellular H2O2, the channel is gated (Hara et al. 2002; Nazıroğlu and Lückhoff 2008). TRPV1 channels are activated by different stimuli including H2O2 and capsaicin while they were inhibited by capsazepine (CPZ) (Caterina et al. 1997; Nazıroğlu et al. 2013; Ogawa et al. 2016). It was reported that NADPH oxidase pathways are the major sources of TRPM2- and TRPV1-induced Ca2+ entry and superoxide production in cell lines (Hackel et al. 2013; Chen et al. 2013). TRPV1 channels were activated in DRG by oxidative stress induced by NADPH oxidase and the enzyme has also been identified as a source of oxidative stress in DRG (Ibi et al. 2008), but there is no report about the regulation of the TRPM2 channel and oxidative stress through NADPH oxidase and PKC pathways in DRG neurons.
The present study was aimed at elucidating the role of PKC and NADPH oxidase pathways in modulating the effects of TRPM2 and TRPV1 channels in DRG neurons.
Material and Methods
Chemicals
Roswell Park Memorial Institute (RPMI)-1640 medium, NAC, capsaicin (CAP), CPZ, penicillin–streptomycin, H2O2, dimethyl sulfoxide (DMSO), PMA, apocynin, BIM, and N-(p-amylcinnamoyl)anthranilic acid (ACA) were obtained from Sigma Chemical Co. (St. Louis, MO, USA). Collegenase type IV was purchased from Worthington Biochemical Corporation (NJ, USA). Cell culture flasks (50 ml and 25 cm2) were purchased from CELLSTAR (Greiner Bio-One Inc., Istanbul, Turkey). Remaining chemicals and plastic materials were purchased from Santa Cruz Inc. (Istanbul, Turkey).
Animals
Twelve male Wistar albino rats (12 weeks old) were housed in the Experimental Animal Research Center of Süleyman Demirel University (SDU). They were kept under controlled light (12 h day/night cycle) and humidity (60-70%) with free access to water (except in the fasting period) and commercial feed.
Study Groups
DRG neurons of each animal were divided into eight groups as follows:
-
1.
Control group. Neuron in the group was not stimulated by H2O2 and capsaicin (CAP). The neurons in the control group were incubated (37 °C and 5% CO2) in the incubator for 2 h with normal medium (DMEM with 5% bovine serum albumin and 1% penicillin–streptomycin).
-
2.
ACA-treated group. The DRG neurons were immediately treated with ACA (0.025 mM) in a patch chamber before H2O2 stimulation (Nazıroğlu et al. 2013).
-
3.
CPZ-treated group. The DRG neurons were immediately treated with CPZ (0.1 mM) in a patch chamber before H2O2 stimulation (Nazıroğlu et al. 2013; Övey and Nazıroğlu 2015).
-
4.
Apocynin-treated group. The DRG neurons were incubated with apocynin (0.25 mM) for 60 min in the incubator before H2O2 (10 mM) and capsaicin (0.01 mM) stimulations (Wind et al. 2010).
-
5.
NAC-treated group. The DRG neurons were incubated with NAC (10 mM) before H2O2 (10 mM) and capsaicin (0.01 mM) stimulations (Özgül and Nazıroğlu 2012; Nazıroğlu et al. 2013). NAC was added to the cell culture flasks for a 2-h incubation before capsaicin and H2O2 stimulations because transfer of the antioxidant into the cell is slow (Nazıroğlu et al. 2013).
-
6.
BIM-treated group. The DRG neurons were incubated with BIM (0.01 mM) for 30 min in the incubator before H2O2 (10 mM) and capsaicin (0.01 mM) stimulations (Miyano et al. 2010).
-
7.
PMA-treated group. The DRG neurons were incubated with PMA (0.001 mM) in the incubator for 30 min before H2O2 (10 mM) and capsaicin (0.01 mM) stimulations (Nazıroğlu and Özgül 2013). The TRPM2 and TRPV1 channels were inhibited by ACA (0.025 mM) and CPZ (0.1 mM), respectively.
-
8.
PMA plus BIM-treated group. The DRG neurons were incubated with PMA (0.001 mM) for 30 min in the incubator, and then they were incubated with BIM (0.01 mM) for 30 min before H2O2 (10 mM) and capsaicin (0.01 mM) stimulations.
At the end of the treatments and incubations, the DRG samples were immediately used for the patch clamp analyses.
Preparation of DRG Neurons
For preparing DRG neurons, rats were decapitated by cervical dislocation as described previously (Sözbir and Nazıroğlu 2016; Kahya et al. 2017). After decapitation, the skin on the back of the rats is split with fine forceps, and the spinal cord is exposed. Serial sections of the entire L4–L5 DRG neurons from the rats were cut (16 μm), and three sections, at least 100 μm apart, were taken. The DRG neurons are removed and placed into a 15-ml conical tube with a 5-ml cold Dulbecco’s modified Eagle’s medium (DMEM, Gibco, Istanbul, Turkey) and centrifuged for 5 min at 600×g. After centrifugation, the supernatant is discarded, and the pellet is re-suspended in 5 ml Hank’s buffered salt solution (Ca2+- and Mg2+-free, HBSS) containing 5 mg collagenase D, type IV (0.1%), and 5 mg trypsin, type 1 (0.1%). DRGs are digested for 45 min in a 37 °C water bath with rotation at 1000 g. After digestion, the samples are centrifuged at 500×g for 5 min. The supernatant is discarded, and the pellet is re-suspended in an 8-ml neurobasal medium (NBM) supplemented with B-27, a serum-free supplement (2 mM), l-glutamine (10 μl/ml), and penicillin–streptomycin (Invitrogen). Then, the DRG neurons were transferred to patch chambers for analyses.
Electrophysiology
The neurons were transferred to extracellular buffer [as mM: 40 NaCl, 1.2 MgCl2, 1.2 CaCl2, 5 KCl, 10 HEPES, pH 7.4 (KOH)] in a temperature-controlled (22–24 °C) recording chamber (Luigs & Neumann, Ratingen, Germany). In some experiments, Na+ was replaced by 150 mM N-methyl-d-glucamine (NMDG+) and the titration was performed with HCl. Channel activity in DRG neuron was studied with the patch clamp technique in the whole-cell mode, using an EPC 10 equipped with a personal computer with Patchmaster software (HEKA, Lamprecht, Germany) (Özdemir et al. 2016; Kahya et al. 2017). Control records were taken on each experimental day using the same animals as those used for studying TRPM2 and TRPV1. The neurons were held at a potential of −60 mV, and current–voltage (I–V) relationships were obtained from voltage ramps from −90 to +60 mV applied over 200 ms. Bridge balance and access resistance were monitored during recordings, and experiments with >20% changes were discarded. Whole-cell mode of patch clamp experiments was used in all experiments, using an EPC 10 equipped with a personal computer with Patchmaster software (HEKA, Lamprecht, Germany). The TRPM2 agonist (H2O2), TRPV1 agonists (capsaicin and H2O2), TRPM2 antagonist (ACA), and TRPV1 antagonist (CPZ) solutions were daily prepared and added to the extracellular buffer in the patch chamber. The inhibition with ACA and CPZ was performed by adding bath solution directly to the bath chamber during measurement. Open tip resistance of borosilicate patch pipettes was between 4 and 7 MΩ. Intracellular solution contained (in mM) 145 cesium glutamate, 8 NaCl, 10 EGTA, 2 MgCl2, and 10 HEPES (pH 7.2) (adjusted with CsOH). It was reported that TRPM2 gating in neurons is greatly facilitated by elevated concentrations of high intracellular free Ca2+ ([Ca2+]i) concentration (McHugh et al. 2003). Hence, the [Ca2+]i in TRPM2 experiments was set to 1 μM (0.886 mM Ca2+, 1 mM Cs-EGTA) instead of the physiologic intracellular Ca2+concentration. The Ca2+ concentrations of the intracellular and extracellular solutions were calculated as described previously by using a specific computer program (Özdemir et al. 2016; Kahya et al. 2017).
Preparation of Agonists and Antagonists
Stock solutions (1 mM) of PMA, apocynin, BIM, ACA, capsaicin, and CPZ were dissolved in DMSO and stored at −85 °C. H2O2 was freshly prepared each day. Before the experiment, PMA (0.001 mM), apocynin (0.25 mM), BIM (0.01 mM), ACA (0.025 mM), capsaicin (0.001–0.01 mM), and CPZ (0.1 mM) in extracellular bath solutions were diluted to reach the final concentrations. After addition of NAC, PMA, CAP, ACA, and CPZ to standard extracellular bath solution, the pH values of these solutions were adjusted with KOH and to 7.4.
Statistical Analyses
The channel capacitances were compared by one-way ANOVA followed by Tukey’s post hoc test. Differences were considered statistically significant when the p value was 0.05. All statistical analyses were performed by SPSS Statistical program (17.0, SPSS Inc., Chicago, Illinois, USA). All the results were expressed as means ± standard deviation (SD).
Results
Effects of the TRPM2 Antagonist (ACA) on H2O2-Induced TRPM2 Currents in DRG Neurons
TRP channels can be indirectly blocked by various chemicals. However, for most TRP channels including TRPM2, the range of pharmacological modulators is limited. ACA as 0.025–0.040 mM was reported as a potent inhibitor of TRPM2 (Kraft et al. 2006), although reports on the effects of ACA in different cell types are conflicting (Nazıroğlu et al. 2012). Hence, we wanted to further clarify the effects of the channel blocker on TRPM2 channel currents in DRG neurons.
The mean value for the current density (pA/pF) in the control group was 2.21 (n = 8) (Fig. 1a), and there was little or no current in control records in the absence of H2O2. In DRG neurons, H2O2-induced currents of TRPM2 channels are reported between 0.52 and 1.2 nA (Özgül and Nazıroğlu 2012; Nazıroğlu et al. 2013; Sözbir and Nazıroğlu 2016; Yazğan and Nazıroğlu 2017). In the current study, we observed 0.62 nA current in the DRG neurons through superfusion of H2O2 (10 mM). These currents were blocked by ACA, as well as by substituting NMDG+ for Na+ (see Fig. 1b). The mean values of the current densities in the H2O2 and H2O2 + ACA groups as pA/pF were 87.13 (n = 8) and 13.00 (n = 8), respectively (Fig. 2). The current densities were high in the H2O2 and H2O2 + ACA groups as compared to the control (p < 0.001) although the densities were significantly lower (p < 0.001) in the H2O2 + ACA group (Figs. 2, 4, and 5). The data with H2O2 indicated that H2O2 acts by initiating a metabolic cascade resulting in the increase of a cytosolic oxidative stress factor and that this is responsible for the activation of the C-terminal Nudix domain ADPR pyrophosphate enzyme of the TRPM2 channel. H2O2-induced activation of the TRPM2 channels was inhibited by the TRPM2 channel blocker, ACA.
PKC and NADPH oxidase-dependent activation of the TRPM2 channel in DRG neurons. a Original recordings from control neurons at holding potential (−60 mV). b TRPM2 currents in DRG neurons were stimulated by H2O2 (10 mM) in the bath (chamber), and they were inhibited by ACA (0.025 mM) in the patch chamber. c TRPM2 currents in DRG neurons were stimulated by H2O2 in the bath (chamber), and they were inhibited by CPZ (0.1 mM) in the patch chamber. d–h The DRG neurons in the d–h groups were incubated with extracellular apocynin (0.25 mM for 1 h), NAC (10 mM for 2 h), BIM (0.01 mM for 30 min), PMA (0.001 mM for 1 h), and PMA + BIM (0.01 mM for 1 h and 0.001 mM for 30 min) before H2O2 stimulation, respectively. b, c, g Current voltage relationships of NMDG+ and H2O2 through the TRPM2 channel in the presence of various extracellular cations (same experiments as in panels b, c). W.C. is used abbreviation of whole cell
Effects of TRPM2 (ACA and 0.025 mM) and TRPV1 (CPZ and 0.1 mM) blockers on H2O2-induced TRPM2 channel activation in DRG neurons. For each of the four applications studied in the cells, the initial current density (divided by the cell capacitance, a measure of cell size) was determined as well as the maximal current density after administration of H2O2. The numbers in parentheses indicate n numbers of the groups. Significant (a p < 0.001 versus controls. b p < 0.001 versus H2O2 groups. c p < 0.05 versus H2O2 + ACA group) (mean ± SD)
Effects of TRPV1 Antagonist (CPZ) on H2O2-Induced TRPV1 Currents in DRG Neurons
The TRPV1 channels are activated by different stimuli including capsaicin and nitric oxide. Recently, activation of the TRPV1 channel by H2O2 was reported in different cell lines (Ogawa et al. 2016). Activation of TRPV1 channels with different stimuli changes in different cell types (Nazıroğlu et al. 2012). To our knowledge, there is no report on H2O2-dependent activation of TRPV1 channels in DRG neurons. Hence, I wanted to clarify the effects of H2O2 on TRPV1 channel currents in DRG neurons.
There was little or no current in control records (Figs. 1a) in the absence of H2O2, and the mean value for the current density in control DRG neurons was 3.02 pA/pF (n = 7). However, addition of H2O2 to the patch chamber activated TRPV1 channels to well above 0.62 nA. These currents were reversibly and partially blocked by CPZ, as well as by substituting NMDG+ for Na+ (see Figs. 1c and 3c, f). The mean values of the current densities in the H2O2 and H2O2 + CPZ groups as pA/pF were 90.67 (n = 4) and 20.84 (n = 4), respectively. The current densities were high in the H2O2 and H2O2 + ACA groups as compared to the control (p < 0.001), and the densities were comparatively lower (p < 0.001) in the H2O2 + CPZ group. The current densities were also markedly (p < 0.05) lower in the H2O2 + CPZ group than in the H2O2 + ACA group (Fig. 2). Cysteine residues are main targets of H2O2, and a recent report indicated the presence of cysteine groups in the TRPV1 channel structure (Ogawa et al. 2016). It is possible that cysteines in TRPV1 channels might be the targets of H2O2 exposure.
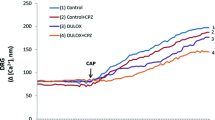
PKC and NADPH oxidase-dependent activation of the TRPV1 channel in DRG neurons. a Original whole cell (W.C.) recordings from control neurons (holding potential was −60 mV). b TRPV1 currents in DRG neurons were stimulated by 0.01 mM capsaicin (CAP) but not 0.001 and 0.005 mM CAP in the bath (chamber), and they were inhibited by capsazepine (CPZ and 0.1 mM) in the patch chamber. c–g The DRG neurons in the c–g groups were incubated with extracellular apocynin (0.25 mM for 1 h), NAC (10 mM for 2 h), BIM (0.01 mM for 30 min), PMA (0.001 mM for 1 h), and PMA + BIM (0.01 mM for 1 h and 0.001 mM for 30 min) before CAP (0.01 mM) stimulation, respectively. Current voltage relationships of NMDG+ and H2O2 through the TRPV1 channel in the presence of various extracellular cations (same experiments as in panels b, c, f)
H2O2 was reported as an activator of TRPA1 channels in vagal lung C-fibers (Ruan et al. 2014), although the channel is inhibited by AP18 (Yazğan and Nazıroğlu 2017). I tested TRPA1 and TRPM2 currents in response to H2O2 in the DRG neuron (data are not shown). The neurons were pre-incubated by addition of ACA (0.025 mM) and AP18 (0.02 mM) combination into the patch chamber before activation of the TRPV1 channel via H2O2 (10 mM). The TRPV1 currents were even activated in the presence of AP18 and ACA combination by H2O2. Hence, I decided that the current belongs to the TRPV1 channel.
Effects of TRPV1 Antagonist (CPZ) on Capsaicin-Induced TRPV1 Currents in DRG Neurons
Capsaicin activates TRPV1 channels. Activation of TRPV1 channels with different doses of capsaicin changes in different cell types. For example, dose-dependent (600 nM–0.002 mM) activation of the TRPV1 channel in the intestinal afferent nerve was reported (Miranda-Morales et al. 2010). Hence, I wanted to clarify the dose-dependent effects of capsaicin on TRPV1 channel currents in DRG neurons.
In whole cell chamber bath experiments, superfusion of three doses of capsaicin (0.001, 0.005, and 0.010 mM) evoked a dose-dependent activation of rat DRG neurons (Fig. 3b) as described previously (Miranda-Morales et al. 2010; Deba and Bessac 2015; Yazğan and Nazıroğlu 2017). In DRG neurons, TRPV1 channel activation doses of capsaicin were reported between 0.001 and 0.015 mM (Deba and Bessac 2015; Yazğan and Nazıroğlu 2017). The TRPV1 currents in the DRG neurons were activated by treatment of 0.01 mM capsaicin but not 0.001 and 0.005 mM capsaicin and reached amplitudes of well above 0.83 nA (Fig. 3b). These currents were reversibly and partially blocked by CPZ (0.1 mM) (Fig. 3b, e, f). There was little or no current (mean value as pA/pF was 3.71) in control records (n = 6) in the absence of capsaicin (Fig. 3a). The mean values of the current densities in the capsaicin and capsaicin + CPZ groups as pA/pF were 106.51 (n = 6) and 6.97 (n = 6), respectively (Figs. 6 and 7). The current densities were significantly greater (p < 0.001) in the capsaicin group as compared to the control, and the densities were significantly lower (p < 0.001) in the capsaicin + CPZ group than in the capsaicin group (Fig. 7).
Effects of NADPH Oxidase Modulators (Apocynin and NAC) on H2O2, Capsaicin, and PMA-Induced TRPM2 and TRPV1 Channel Activations
Recently, we observed a modulator role of sulfhydryl protective agents such as GSH and NAC on TRPM2 and TRPV1 channel activation in DRG neurons (Özgül and Nazıroğlu 2012; Nazıroğlu et al. 2013; Sözbir and Nazıroğlu 2016). Reports on the effects of antioxidants on the PMA-induced TRPM2 channel activation are conflicting. For example, it was reported that the PMA-induced TRPM2 channel activation was blocked in DRG neurons by vitamin E treatment but not vitamin C or catalase (Nazıroğlu and Özgül 2013). However, there is no report on the effects of apocynin and NAC on TRPM2 and TRPV1 currents in H2O2- and capsaicin-treated DRG neurons. Hence, I examined the potential protective roles of NAC and apocynin on H2O2-induced TRPM2 and capsaicin-induced TRPV1 activations in DRG neurons. Exposure of isolated DRG neurons isolated to H2O2 and capsaicin significantly (p < 0.001) increased the activation of TRPM2 (Figs. 1b and 2) and TRPV1 channels, respectively (Figs. 3b, f and 6). In contrast, H2O2- and capsaicin-induced NADPH oxidase (H2O2) activation of TRPM2 (Figs. 1d, e and 4) and TRPV1 (Figs. 3c–e and 7) was substantially (p < 0.001) reduced in DRG neurons by apocynin and NAC treatments.
Protective effects of NADPH oxidase inhibitors (apocynin, 0.25 mM for a 1-h incubation, and NAC, 10 mM for a 2-h incubation) on H2O2-induced TRPM2 channel activation in DRG neurons (mean ± SD). The values were expressed as current densities after administration of H2O2. The numbers in parentheses indicate n numbers of the groups. (a p < 0.001 versus control. b p < 0.001 versus the H2O2 group. c p < 0.001 versus H2O2 + ACA. d p < 0.001 versus PMA + H2O2. e p < 0.001 versus PMA + H2O2 + ACA)
Effects of PKC Stimulator (PMA) and Inhibitor (BIM) on TRPM2 and TRPV1 Channel Activations
NADPH oxidase-induced TRPV1 activation is dependent on the PKC pathway (Ibi et al. 2008). Recently, we observed a TRPM2 activator role of PMA via excessive production of ROS in DRG neurons, and this activation was inhibited by vitamin E treatment (Nazıroğlu and Özgül 2013). To clarify the role of NADPH oxidase in the PKC-dependent activation of TRPM2 and TRPV1 channels, I next tested the effects of the PKC inhibitor, BIM, in DRG neurons. During the oxidative burst stimulated by PMA in DRG neurons, TRPM2 and TRPV1 channel activities were determined by measuring the current density of the channels (Fig. 5). The H2O2- and CAP-induced TRPM2 (Figs. 1g and 5) and TRPV1 (Figs. 6f and 7) current densities were markedly (p < 0.001) higher in the PMA group than in the control. Both currents were further increased in the PMA group as compared to the H2O2-alone group (p < 0.001) (Figs. 5 and 7). The TRPM2 and TRPV1 currents in the PMA group were decreased by ACA and CPZ treatments, respectively (p < 0.001) (Figs. 1e, 3d, 5, and 7). The TRPM2 and TRPV1 current densities were significantly (p < 0.001) lower in the BIM + H2O2 and BIM + capsaicin groups than in the H2O2 and PMA + H2O2, capsaicin, and PMA + capsaicin groups (Figs. 1f, 3e, 5, and 7). As compared to the H2O2 and capsaicin groups, the TRPM2 and TRPV1 current densities were further increased by H2O2 + PMA and capsaicin + PMA exposures. However, the PMA-induced TRPM2 and TRPV1 current densities were totally (p < 0.001) inhibited in the PMA + BIM + H2O2 and PMA + BIM + capsaicin groups by post-incubation of BIM (Figs. 1h, 3g, 5, and 7) and there were little or no TRPM2 and TRPV1 currents in the PMA + BIM group after H2O2 and capsaicin treatments (Figs. 5 and 7).
Effects of the PKC inhibitor (BIM, 0.01 mM for a 30-min incubation) and stimulator (PMA, 0.01 mM for a 30-min incubation) on H2O2-induced TRPM2 channel activation in DRG neurons (mean ± SD). The values were expressed as current densities after administration of H2O2. The numbers in parentheses indicate n numbers of the groups. (a p < 0.001 versus control. b p < 0.001 versus the H2O2 group. c p < 0.001 versus H2O2 + ACA. d p < 0.001 versus PMA + H2O2. e p < 0.001 versus PMA + H2O2 + ACA)
Protective effects of NADPH oxidase inhibitors (apocynin and NAC) on capsaicin (0.01 mM)-induced TRPV1 channel activation in DRG neurons (mean ± SD). The DRG neurons were incubated with apocynin (0.25 mM) and NAC (10 mM) for 60 min before capsaicin (CAP, 0.01 mM) stimulation, respectively. The values were expressed as current densities after administration of CAP. The numbers in parentheses indicate n numbers of the groups. (a p < 0.001 versus control. b p < 0.001 versus the CAP group)
Effects of PKC inhibitor (BIM) and stimulator (PMA) on capsaicin-induced TRPV1 channel activation in DRG neurons (mean ± SD and n = 3). The DRG neurons PMA and BIM groups were incubated with PMA (0.001 mM) and BIM (0.01 mM) for 30 min before capsaicin (CAP, 0.01 mM) stimulation, respectively. In the PMA + BIM group, the neurons were pre-incubated with PMA for 30 min and then they were further incubated with BIM for 30 min before CAP (0.01 mM) stimulation. The values were expressed as current densities after administration of CAP (a p < 0.001 versus control. b p < 0.001 versus the CAP group. c p < 0.001 versus the PMA + CAP group)
Discussion
Changes in DRG Ca2+ signaling in diabetes contribute to the development of neuropathic pain (Nazıroğlu et al. 2012). Overload Ca2+ entry through activation of TRPM2 and TRPV1 channels in the DRG is increased by excessive production of oxidative stress (Nazıroğlu et al. 2011b). PKC and NADPH oxidase pathways are activated by excessive intracellular free Ca2+ entry via TRPM2 and TRPV1 channels (Ibi et al. 2008; Nazıroğlu and Özgül 2013). In experimental models, pain was blocked by inhibition of these pathways (Kallenborn-Gerhardt et al. 2012; Kallenborn-Gerhardt et al. 2013). The TRPM2 and TRPV1 channels are mainly expressed in DRG neurons (Caterina et al. 1997; Fonfria et al. 2006; Özgül and Nazıroğlu 2012). Therefore, inhibition of NADPH oxidase and PKC pathway-induced excessive oxidative stress and overload Ca2+ entry via inhibition of TRPM2 and TRPV1 channels in DRG neurons may represent important therapeutic targets in the treatment of peripheral neuropathic pain. I observed that Ca2+ entry via TRPM2 and TRPV1 channels was increased in DRG neurons in response to PMA, H2O2, and dose-dependent capsaicin. Furthermore, PMA-, H2O2-, and capsaicin-induced Ca2+ entry through the TRPM2 and TRPV1 channels was decreased to control levels by NADPH oxidase inhibitors (apocynin and NAC) and the PKC inhibitor, BIM. To the best of my knowledge (Ibi et al. 2008; Nazıroğlu and Özgül 2013), this study represents the first examination of the effects of apocynin and BIM on PKC and NADPH oxidase-dependent gating of TRPM2 and TRPV1 channels in DRG neurons. Therefore, as a result of the findings in this study, I believe that inhibitors of PKC and NADPH oxidase have the potential to serve as TRPM2 and TRPV1 channel modulators in diseases involving DRG neurons.
The C-terminal domain of TRPM2 contains the enzyme ADPR pyrophosphatase, and this enzyme is sensitive to ROS and reactive nitrogen species (Nazıroğlu 2007). TRPM2 channels are gated by extracellular and intracellular ROS, possibly by interacting with the ADPR pyrophosphatase enzyme in the tail of the C domain of the protein (Fonfria et al. 2006; Nazıroğlu and Lückhoff 2008; Nazıroğlu and Özgül 2013). It is well known that excessive ROS production results in excessive production of H2O2 and thereby contributes to sensitization in persistent pain of DRG neurons (Kallenborn-Gerhardt et al. 2012; Özdemir et al. 2016). In the current study, increased current densities and sensitization in TRPM2 channel activation via stimulation of H2O2, NADPH oxidase, and PKC productions were observed in the DRG neurons. The data with H2O2 support the previous reports (Hara et al. 2002; Nazıroğlu and Lückhoff 2008) that H2O2 acts by initiating a metabolic cascade resulting in the increase of NADPH oxidase and PKC enzymes, and those H2O2 production pathways are responsible for the activation of ADPR pyrophosphatase in the C domain of the TRPM2 channel.
The activation threshold and sensitivity of TRPV1 channels are changed by different mechanisms such as mechanical injury and high temperature. The sensitivity of TRPV1 is reduced by PKC-mediated phosphorylation of serine residues (Chung et al. 2015). An obligate role of cysteine residues in the pore region of TRPM2 and TRPV1 channels has been reported (Mei et al. 2006). If oxidation of cysteine residues of TRPM2 and TRPV1 occurs, the channel structure may be modified such that overload Ca2+ entry will occur through over-activation of TRPM2 and TRPV1 channels. High amounts of intracellular free Ca2+ might then induce excessive reactive oxygen species (ROS) production via mitochondrial membrane depolarization, resulting in even further activation of the channels by mitochondrial ROS production (Özdemir et al. 2016; Kahya et al. 2017). NAC is a sulfhydryl group containing antioxidant and is an important member of the glutathione redox cycle. NAC has an important role in scavenging ROS production in mitochondria (Nazıroğlu et al. 2013). For this reason, NAC is believed to play critical roles in protecting cells from hazardous mitochondrial ROS. In the current study, I observed a modulator role of apocynin and NAC in TRPM2 and TRPV1 channels likely due to interaction with cysteine residues and protection against excessive ROS production.
NADPH oxidase activation is regulated by Ca2+ and diacylglycerol (DAG) signaling pathways. In addition to oxidative stress, PKC isoenzymes are also activated by Ca2+ and DAG signaling pathways. Recent studies suggest that NADPH oxidase pathways in the DRG and neuroblastoma SH-SY5Y cell lines may be more important than ADPR as the major sources of TRPM2-induced Ca2+ entry and superoxide production (Hackel et al. 2013; Chen et al. 2013). NADPH oxidase activation was reported as a primary source of ROS production in DRG neurons (Ibi et al. 2008). Both TRPM2 and TRPV1 channels are activated in hippocampal and DRG neurons by cytosolic glutathione depletion-induced oxidative stress (Özgül and Nazıroğlu 2012; Övey and Nazıroğlu 2015). Recently, we also observed a modulator role of sulfhydryl antioxidant agents such as GSH and NAC on TRPM2 and TRPV1 channel activation in DRG neurons (Nazıroğlu et al. 2011; Nazıroğlu et al. 2013; Sözbir and Nazıroğlu 2016). Vitamin E treatment reduced the PMA-induced TRPM2 channel activation in DRG neurons. However, there is no report on PMA-induced TRPM2 and TRPV1 activations in NAC-treated DRG neurons. In the current study, treatment of isolated DRG neurons with PMA and H2O2 significantly (p < 0.001) increased the activation of TRPM2 and TRPV1 channels and the TRPM2 and TRPV1 activations were decreased in DRG neurons by NAC treatment. Similarly, Ibi et al. (2008) reported an increase of PMA-induced PKC isoforms in DRG neurons by NAC pre-treatment. These findings suggest that the activation of TRPM2 and TRPV1 channels by ROS derived from NADPH oxidase is decreased in DRG neurons by pre-treatment with NAC and subsequent inhibition of PKC.
In conclusion, the main finding of the current study is that NADPH oxidase blockers apocynin and NAC decreased the TRPM2 and TRPV1 channel-dependent Ca2+ influx in DRG neurons. I clearly observed that the channels are modulated by H2O2- and dose-dependent capsaicin-induced oxidative stress in the neurons by a PKC-dependent pathway. Hence, our results indicate that NADPH oxidase and PKC enzyme inhibition acts as a neuronal modulator against oxidative stress-induced Ca2+ mobilization through TRPM2 and TRPV1 channels in DRG neurons. This finding is of particular significance and may provide an explanation for the neuropathic and peripheral pain properties of NADPH oxidase and PKC enzymes, in keeping with the proposed role of excessive Ca2+ entry in the pathology of neuropathic pain.
Abbreviations
- [Ca2+]i :
-
Intracellular Ca2+
- ACA:
-
N-(p-Amylcinnamoyl)anthranilic acid
- ADPR:
-
Adenosine diphosphatase ribose
- BIM:
-
Bisindolylmaleimide I
- CAP:
-
Capsaicin
- CPZ:
-
Capsazepine
- DRG:
-
Dorsal root ganglion
- GSH:
-
Glutathione
- NAC:
-
N-Acetylcysteine
- NMDG:
-
N-Methyl-d-glucamine
- PKC:
-
Protein kinase C
- PMA:
-
Phorbol myristate acetate
- ROS:
-
Reactive oxygen species
- TRP:
-
Transient receptor potential
- TRPM2:
-
Melastatin-like transient receptor potential 2
- TRPV1:
-
Transient receptor potential vanilloid 1
- W.C.:
-
Whole cell
References
Callaghan BC, Price RS, Feldman EL (2015) Distal symmetric polyneuropathy: a review. JAMA 314:2172–2181
Caterina MJ, Schumacher MA, Tominaga M, Rosen TA, Levine JD, Julius D (1997) The capsaicin receptor: a heat-activated ion channel in the pain pathway. Nature 389:816–824
Chakraborti S, Chowdhury A, Kar P, Das P, Shaikh S, Roy S, Chakraborti T (2009) Role of protein kinase C in NADPH oxidase derived O2*(-)-mediated regulation of KV-LVOCC axis under U46619 induced increase in [Ca2+]i in pulmonary smooth muscle cells. Arch Biochem Biophys 487:123–130
Chen SJ, Zhang W, Tong Q, Conrad K, Hirschler-Laszkiewicz I, Bayerl M, Kim JK, Cheung JY, Miller BA (2013) Role of TRPM2 in cell proliferation and susceptibility to oxidative stress. Am J Physiol Cell Physiol. 304:C548–C560
Chung MK, Lee J, Joseph J, Saloman J, Ro JY (2015) Peripheral group I metabotropic glutamate receptor activation leads to muscle mechanical hyperalgesia through TRPV1 phosphorylation in the rat. J Pain 16:67–76
Deba F, Bessac BF (2015) Anoctamin-1 Cl(−) channels in nociception: activation by an N-aroylaminothiazole and capsaicin and inhibition by T16A[inh]-A01. Mol Pain 11:55
Fonfria E, Murdock PR, Cusdin FS, Benham CD, Kelsell RE, McNulty S (2006) Tissue distribution profiles of the human TRPM cation channel family. J Recept Signal Transduct Res 26:159–178
Hackel D, Pflücke D, Neumann A, Viebahn J, Mousa S, Wischmeyer E, Roewer N, Brack A, Rittner HL (2013) The connection of monocytes and reactive oxygen species in pain. PLoS One 8:e63564
Hara Y, Wakamori M, Ishii M, Maeno E, Nishida M, Yoshida T, Yamada H, Shimizu S, Mori E, Kudoh J, Shimizu N, Kurose H, Okada Y, Imoto K, Mori Y (2002) LTRPC2 Ca2+-permeable channel activated by changes in redox status confers susceptibility to cell death. Mol Cell 9:163–173
Heumüller S, Wind S, Barbosa-Sicard E, Schmidt HH, Busse R, Schröder K, Brandes RP (2008) Apocynin is not an inhibitor of vascular NADPH oxidases but an antioxidant. Hypertension 51:211–217
Ibi M, Matsuno K, Shiba D, Katsuyama M, Iwata K, Kakehi T, Nakagawa T, Sango K, Shirai Y, Yokoyama T, Kaneko S, Saito N, Yabe-Nishimura C (2008) Reactive oxygen species derived from NOX1/NADPH oxidase enhance inflammatory pain. J Neurosci 28:9486–9494
Kahya MC, Nazıroğlu M, Övey İS (2017) Modulation of diabetes-induced oxidative stress, apoptosis, and Ca2+ entry through TRPM2 and TRPV1 channels in dorsal root ganglion and hippocampus of diabetic rats by melatonin and selenium. Mol Neurobiol. doi:10.1007/s12035-016-9727-3
Kallenborn-Gerhardt W, Schröder K, Del Turco D, Lu R, Kynast K, Kosowski J, Niederberger E, Shah AM, Brandes RP, Geisslinger G, Schmidtko A (2012) NADPH oxidase-4 maintains neuropathic pain after peripheral nerve injury. J Neurosci 32:10136–10145
Kallenborn-Gerhardt W, Schröder K, Geisslinger G, Schmidtko A (2013) NOXious signaling in pain processing. Pharmacol Ther 137:309–317
Kraft R, Grimm C, Frenzel H, Harteneck C (2006) Inhibition of TRPM2 cation channels by N-(p-amylcinnamoyl)anthranilic acid. Br J Pharmacol 148:264–273
Lo HW, Antoun GR, Ali-Osman F (2004) The human glutathione S-transferase P1 protein is phosphorylated and its metabolic function enhanced by the Ser/Thr protein kinases, cAMP-dependent protein kinase and protein kinase C, in glioblastoma cells. Cancer Res 64:9131–9138
McHugh D, Flemming R, Xu SZ, Perraud AL, Beech DJ (2003) Critical intracellular Ca2+ dependence of transient receptor potential melastatin 2 (TRPM2) cation channel activation. J Biol Chem 278:11002–11006
Mei ZZ, Mao HJ, Jiang LH (2006) Conserved cysteine residues in the pore region are obligatory for human TRPM2 channel function. Am J Physiol Cell Physiol 291:C1022–C1028
Miranda-Morales M, Ochoa-Cortes F, Stern E, Lomax AE, Vanner S (2010) Axon reflexes evoked by transient receptor potential vanilloid 1 activation are mediated by tetrodotoxin-resistant voltage-gated Na+ channels in intestinal afferent nerves. J Pharmacol Exp Ther 334:566–575
Miyano K, Morioka N, Sugimoto T, Shiraishi S, Uezono Y, Nakata Y (2010) Activation of the neurokinin-1 receptor in rat spinal astrocytes induces Ca2+ release from IP3-sensitive Ca2+ stores and extracellular Ca2+ influx through TRPC3. Neurochem Int 57:923–934
Nazıroğlu M (2007) New molecular mechanisms on the activation of TRPM2 channels by oxidative stress and ADP-ribose. Neurochem Res 32:1990–2001
Nazıroğlu M, Lückhoff A (2008) A calcium influx pathway regulated separately by oxidative stress and ADP-ribose in TRPM2 channels: single channel events. Neurochem Res 33:1256–1262
Nazıroğlu M, Özgül C (2013) Vitamin E modulates oxidative stress and protein kinase C activator (PMA)-induced TRPM2 channel gate in dorsal root ganglion of rats. J Bioenerg Biomembr 45:541–549
Nazıroğlu M, Özgül C, Çiğ B, Doğan S, Uğuz AC (2011) Glutathione modulates Ca(2+) influx and oxidative toxicity through TRPM2 channel in rat dorsal root ganglion neurons. J Membr Biol 242:109–118
Nazıroğlu M, Dikici DM, Dursun Ş (2012) Role of oxidative stress and Ca2+ signaling on molecular pathways of neuropathic pain in diabetes: focus on TRP channels. Neurochem Res 37:2065–2075
Nazıroğlu M, Ciğ B, Ozgül C (2013) Neuroprotection induced by N-acetylcysteine against cytosolic glutathione depletion-induced Ca2+ influx in dorsal root ganglion neurons of mice: role of TRPV1 channels. Neuroscience 242:151–160
Ogawa N, Kurokawa T, Fujiwara K, Polat OK, Badr H, Takahashi N, Mori Y (2016) Functional and structural divergence in human TRPV1 channel subunits by oxidative cysteine modification. J Biol Chem 291:4197–4210
Övey IS, Nazıroğlu M (2015) Homocysteine and cytosolic GSH depletion induce apoptosis and oxidative toxicity through cytosolic calcium overload in the hippocampus of aged mice: involvement of TRPM2 and TRPV1 channels. Neuroscience 284:225–233
Özdemir ÜS, Nazıroğlu M, Şenol N, Ghazizadeh V (2016) Hypericum perforatum attenuates spinal cord injury-induced oxidative stress and apoptosis in the dorsal root ganglion of rats: involvement of TRPM2 and TRPV1 channels. Mol Neurobiol 53:3540–3551
Özgül C, Nazıroğlu M (2012) TRPM2 channel protective properties of N-acetylcysteine on cytosolic glutathione depletion dependent oxidative stress and Ca2+ influx in rat dorsal root ganglion. Physiol Behav 106:122–128
Ruan T, Lin YJ, Hsu TH, Lu SH, Jow GM, Kou YR (2014) Sensitization by pulmonary reactive oxygen species of rat vagal lung C-fibers: the roles of the TRPV1, TRPA1, and P2X receptors. PLoS One 9:e91763
Sözbir E, Nazıroğlu M (2016) Diabetes enhances oxidative stress-induced TRPM2 channel activity and its control by N-acetylcysteine in rat dorsal root ganglion and brain. Metab Brain Dis 31:385–393
Wind S, Beuerlein K, Eucker T, Müller H, Scheurer P, Armitage ME, Ho H, Schmidt HH, Wingler K (2010) Comparative pharmacology of chemically distinct NADPH oxidase inhibitors. Br J Pharmacol 161:885–898
Yazğan Y, Nazıroğlu M (2017) Ovariectomy-induced mitochondrial oxidative stress, apoptosis, and calcium ion influx through TRPA1, TRPM2, and TRPV1 are prevented by 17β-estradiol, tamoxifen, and raloxifene in the hippocampus and dorsal root ganglion of rats. Mol Neurobiol. doi:10.1007/s12035-016-0232-5
Acknowledgements
The authors wish to thank Prof. Dr. James W. Putney (NIEHS, NC, USA) for helpful discussions on the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the Local Experimental Animal Ethical Committee of SDU (protocol number 2010-13).
Financial Disclosure
There is no financial disclosure and support for the current study.
Conflict of Interest
The author declares that he has no conflict of interest.
Rights and permissions
About this article
Cite this article
Nazıroğlu, M. Activation of TRPM2 and TRPV1 Channels in Dorsal Root Ganglion by NADPH Oxidase and Protein Kinase C Molecular Pathways: a Patch Clamp Study. J Mol Neurosci 61, 425–435 (2017). https://doi.org/10.1007/s12031-017-0882-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12031-017-0882-4