Abstract
Indirubin-3-oxime (I3O), a synthetic derivative of indirubin, was originally designed as potent inhibitors of cyclin-dependent kinases (CDKs) and glycogen synthase kinase 3β (GSK3β) for leukemia therapy. In the current study, we have shown, for the first time, that I3O prevented 6-hydroxydopamine (6OHDA)-induced neuronal apoptosis and intracellular reactive oxygen species accumulation in PC12 cells in a concentration-dependent manner. GSK3β inhibitors but not CDK5 inhibitors reduced the neurotoxicity induced by 6OHDA. Moreover, the activation of GSK3β was observed after 6OHDA treatment. Furthermore, 6OHDA substantially decreased the transcriptional activity of myocyte enhancer factor 2D (MEF2D), a transcription factor that plays an important role in dopaminergic neuron survival, and reduced nuclear localized MEF2D expression. Interestingly, indirubin-3-oxime and GSK3β inhibitors prevented 6OHDA-induced dysregulation of MEF2D. In addition, short hairpin RNA-mediated decrease of MEF2D expression significantly abolished the neuroprotective effects of indirubin-3-oxime. Collectively, our results strongly suggested that indirubin-3-oxime prevented 6OHDA-induced neurotoxicity via activating MEF2D, possibly through the inhibition of GSK3β. In view of the capability of indirubin-3-oxime to cross the blood–brain barrier, our findings further indicated that indirubin-3-oxime might be a novel drug candidate for neurodegenerative disorders, including Parkinson’s disease in particular.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parkinson’s disease (PD) is the second most common neurodegenerative disorder among elderly and characterized by the progressive loss of dopaminergic neurons in the substantial nigra (Obeso et al. 2010). Although the detailed molecular mechanisms underlying dopaminergic neuronal loss in PD are still unclear, neuronal apoptosis induced by excessive oxidative stress has emerged as an important factor in PD pathogenesis (Barnham et al. 2004). 6-hydroxydopamine (6OHDA) has been most commonly used as a selective catecholaminergic neurotoxin to generate experimental cell models of PD (Kupershmidt et al. 2007; Dong et al. 2014). 6OHDA could be absorbed by dopamine transporter and generate excessive reactive oxygen species (ROS) via the inhibition of mitochondrial electron transport chain complexes I and IV (Bove et al. 2005). Excessive ROS induced by 6OHDA further leads to neuronal apoptosis via the dysregulation of signaling molecules, including GSK3β and CDK5 (Chen et al. 2004; Camins et al. 2009).
Transcription factor myocyte enhancer factor 2D (MEF2D) has been demonstrated to play important roles in neuronal survival in several experimental paradigms associated with PD (Mao et al. 1999). Activation of MEF2D, e.g., by bis(3)-cognitin, a novel dimer developed by our team, has been proved to produce substantial neuroprotections against PD-related pathology in vitro and in vivo (Yang et al. 2009; Yao et al. 2012), strongly suggesting that MEF2D is a novel and effective therapeutic target in treating PD. More recent studies reveal that a variety of pathological factors associated with PD including GSK3β and CDK5 converge their regulatory activities on MEF2D (Smith et al. 2006; Wang et al. 2009; Yang and Mao 2010), indicative of the potential intervention of the inhibitors of these proteins in PD.
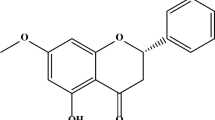
Indirubin-3-oxime (I3O) is a synthetic derivative of indirubin, an active constituent of the traditional Chinese medicine recipe Danggui Longhui Wan used against chronic myelocytic leukemia (Smith et al. 2006). Previous studies have shown that I3O potently inhibits cyclin-dependent kinases (CDKs) and glycogen synthase kinase 3β (GSK3β) via occupying their ATP binding sites, resulting in cancer cell growth inhibition and cell cycle arrest (Leclerc et al. 2001; Chebel et al. 2009; Liao and Leung 2013). More importantly, a recent pharmacokinetics study has demonstrated that intravenous injection of I3O could easily cross the blood–brain barrier and reach the central nervous system (CNS), suggesting that I3O might also be used to treat CNS disorders (Xu et al.).
Previous studies have shown that I3O could inhibit neuronal apoptosis induced by β-amyloid or potassium deprivation in vitro and prevent behavioral abnormity induced by β-amyloid or 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP) in vivo (Xie et al. 2004; Wang et al. 2007; Zhang et al. 2009; Ding et al. 2010). However, the molecular mechanisms underlying these neuroprotective effects of I3O are largely unknown. In this study, we have shown, for the first time, that I3O prevented 6OHDA-induced neuronal apoptosis and oxidative stress in PC12 cells. Furthermore, it was demonstrated that I3O produced its neuroprotective effects via activating MEF2D, possibly through the inhibition of GSK3β.
Material and Methods
Materials
Unless otherwise noted, all media and supplements used for cell cultures were purchased from Invitrogen (Carlsbad, CA, USA). I3O and 3-amino-1 H-pyrazolo[3,4-b]quinoxaline were obtained from Tocris Biosciences (Bristol, UK). Indirubin, SB415286, roscovitine, Hoechst 33,342, LiCl, and 6OHDA were obtained from Sigma Chemicals (St Louis, MO, USA). Antibodies against phospho-Ser9 GSK3β, total GSK3β, and Histone-H3 were obtained from Cell Signaling Technology (Beverly, MA, USA). Antibody against β-actin was obtained from Santa Cruz Biotechnology (Santa Cruz, CA, USA). Antibody against MEF2D was purchased from BD Biosciences (Franklin Lakes, NJ, USA). I3O and indirubin were dissolved in dimethyl sulfoxide (DMSO) at a concentration of 50 mM and further diluted with Milli-Q water before use. Other chemicals were prepared in Milli-Q water.
PC12 Cell Culture
The rat pheochromocytoma PC12 cells were purchased from the American Type Culture Collection (ATCC, Manassas, VA, USA). PC12 cells were maintained in Dulbecco’s modified Eagle’s medium (DMEM) supplemented with 10 % fetal bovine serum (FBS), 100 U/ml penicillin, and 100 μg/ml streptomycin in a 37 °C, 5 % CO2 incubator. For the experiments with 6OHDA, PC12 cells (1 × 105 cells/ml) in DMEM with low serum content (1 % FBS) were seed in 6-well or 96-well plates. All experiments were carried out 24 h after the cells were seeded.
Measurement of Neurotoxicity
Cell viability was determined by the activity of mitochondrial dehydrogenases with 3(4,5-dimethylthiazol-2-yl)-2.5-diphenyltetrazolium bromide (MTT) assay as we previously described (Cui et al. 2013; Cui et al. 2014). Briefly, after treatment, 10 μl of 5 mg/ml MTT solution was added to each well. The plates were incubated at 37 °C for 4 h in a humidified incubator. One hundred microliters of the solvating solution (0.01 N HCl in 10 % SDS solution) was then added to each well for 16–20 h. The absorbance of the samples was measured at a wavelength of 570 nm with 655 nm as a reference wavelength. Unless otherwise indicated, the extent of MTT conversion in PC12 cells without treatment is expressed as a percentage of the control.
Hoechst Staining
Chromatin condensation was detected by staining the cell nucleus with Hoechst 33,342 as we previously described (Cui et al. 2012; Hu et al. 2014). After treatment, cells grown in 6-well plates were washed with ice-cold phosphate buffered saline (PBS), fixed with 4 % formaldehyde in PBS for 15 min, membrane-permeabilized in 0.1 % Triton X-100 for 15 min and blocked in 1 % bovine serum albumin. Cells were then stained with Hoechst 33,342 (5 μg/ml) at 4 °C for 5 min. Images were acquired using a fluorescence microscope (Nikon Instruments Inc. Melville, NY) at ×100 magnification. Ultraviolet excitation and emission wavelengths were used to obtain images of nuclei labeled with Hoechst-33,342. To quantify the percentage of apoptotic nuclei in each group, photos of each well were taken at five random fields and the number of pyknotic nuclei and total nuclei were counted, and the percentage of pyknotic nuclei was averaged.
Measurement of Intracellular ROS
The level of intracellular ROS was measured by the fluorescent dye 2′7′-dichlorodihydrofluorescein diacetate (DCFH-DA, Molecular Probes, Eugene, OR, USA), a nonpolar compound that is converted by cellular esterases to polar and membrane impermeable derivative DCFH [22]. DCFH is nonfluorescent. In the presence of intracellular ROS, DCFH is oxidized to highly fluorescent 2′,7′-dichlorofluorescein (DCF). Cells were pre-treated with drugs for 2 h and then were treated with 6OHDA. The treated cells were washed once with ice-cold PBS and incubated with 10 μM DCFH-DA at 37 °C for 30 min. The dye was removed, and cells were washed once with ice-cold PBS and scanned with a plate reader (Wallac, PerkinElmer, Waltham, MA, USA) at 485 nm excitation and 520 nm emission. Images were acquired using a fluorescence microscope (Nikon Instruments Inc. Melville, NY) at ×100 magnification. Unless otherwise indicated, the fluorescence intensity in PC12 cells without treatment is expressed as a percentage of the control.
MEF2 Luciferase Reporter Gene Assay
MEF2 luciferase reporter assay was performed as we previously described (Yao et al. 2012). Briefly, PC12 cells were transfected with a MEF2 luciferase reporter gene (MEF2 binding site: TCGACGGGCTATTTTTAGGGCC) by pGreenFire1™ reporter lentivector (System Biosciences, Mountain View, CA, USA). Cellular extracts were assayed for luciferase activities by luciferase assay system (Promega, Fitchburg, WI, USA).
Purification of Nuclear Proteins
Proteins in the nucleus of PC12 cells were purified by nuclear/cytosol fractionation kit (Biovision, Milpitas, CA, USA) according to the manufacturer’s instruction. Briefly, the cells were washed twice with ice-cold PBS, scrapped in cold cytosol extraction buffer A with protease inhibitor cocktail, and incubated on ice for 10 min. The supernatant that contains cytosolic proteins was collected by centrifugation at 16,000g for 5 min at 4 °C. A pellet-containing nuclear fraction was re-suspended in nuclear extraction buffer A with a protease inhibitor cocktail and incubated on ice for 40 min. Thereafter, the supernatant that contains nuclear proteins was collected by centrifugation at 16,000g for 10 min at 4 °C.
Western Blot Analysis
Western blot assay was performed as we previously described (Hu et al. 2013). Protein was separated on SDS–polyacrylamide gel and transferred onto polyvinyldifluoride membranes. After membrane blocking, proteins were detected using primary antibodies. After incubation at 4 °C overnight, signals were obtained after binding to chemiluminescent secondary antibodies (Santa Cruz Biotechnology, Santa Cruz, CA, USA). Blots were developed using an enhanced chemiluminescence plus kit (Amersham Bioscience, Aylesbury, UK) and exposed to autoradiographic films.
Short Hairpin RNA Design
The short hairpin RNA (shRNA) against MEF2D was designed based on a previous report and targeted the sequence 5′-GTAGCTCTCTGGTCACTCC-3′ (Flavell et al. 2006). Sense and antisense oligonucleotides were annealed and cloned into pG418-GFP vector to express shRNA directed against MEF2D under the control of the U6 promoter (GenePharma, Shanghai, China). A negative control shRNA (ShNC) with the same nucleotide composition but lacked significant sequence homology to the genome was also used in the experiments.
Cell Transfection
Cells of 2 × 105 were transfected with 3 μg indicated plasmids by using Lipofectamine 2000 (Invitrogen, Carlsbad, CA, USA) according to the manufacturer’s instructions and our previous studies (Cui et al. 2012; Cui et al. 2014). Selection media that contained 100 μg/ml G418 (Sigma Chemicals, St. Louis, MO, USA) were added to the cells 24 h after transfection. Experiments were carried out 48 h after the cells were transfected.
Data Analysis and Statistics
Data, representative of at least three independent experiments, were expressed as the means ± SEM. Statistical significance was determined by analysis of variance with Dunnett’s test in the case of multiple comparisons with control or Tukey’s test. Differences were accepted as significant at p < 0.05.
Results
I3O but not Indirubin Prevents 6OHDA-Induced Apoptosis and Oxidative Stress in PC12 Cells
We have previously reported that the treatment of 300 μM 6OHDA for 6 h could induce typical apoptosis in PC12 cells (Zhang et al. 2011). Therefore, we used this model to investigate the neuroprotective effects of I3O. PC12 cells were pre-treated with gradually increased concentrations of I3O (1–10 μM) or indirubin (1–30 μM) for 2 h and then treated with 300 μM 6OHDA for another 6 h. Cell viability was measured using the MTT assay. It was found that I3O prevented 6OHDA-induced neuronal death in a concentration-dependent manner (Fig. 1a). However, indirubin failed to block 6OHDA-induced cell death. Treatments with 10 μM I3O or 30 μM indirubin alone for 8 h did not show any cell proliferative or cytotoxic effects. However, I3O at a higher concentration (20 μM) showed toxicity to PC12 cells (data not shown).
I3O, but not indirubin, prevents 6OHDA-induced neuronal apoptosis in PC12 cells. a I3O, but not indirubin, prevents 6OHDA-induced neuronal death in PC12 cells in a concentration-dependent manner. PC12 cells were pre-treated with I3O or indirubin at the indicated concentrations for 2 h, and then exposed to 300 μM 6OHDA. Cell viability was measured by the MTT assay at 6 h after 6OHDA challenge. b I3O significantly prevents 6OHDA-induced neuronal apoptosis in PC12 cells. PC12 cells were pre-treated with 10 μM I3O for 2 h, and then exposed to 300 μM 6OHDA. After 6 h of 6OHDA challenge, PC12 cells were assayed with Hoechst staining. The number of pyknotic nuclei with condensed chromatin were counted from representative Hoechst staining photomicrographs and represented as a percentage of the total number of nuclei counted. * p < 0.05 and ** p < 0.01 versus 6OHDA group
To further characterize the neuroprotective effects of I3O against 6OHDA-induced apoptosis, we used Hoechst staining. PC12 cells were pre-treated with 10 μM I3O for 2 h and then treated with 300 μM 6OHDA for 6 h. According to the number of pyknotic bodies stained by Hoechst 33,342, I3O significantly prevented apoptosis induced by 6OHDA in PC12 cells (Fig. 1b).
The intracellular level of ROS is an important biomarker for oxidative stress and increased ROS level generally indicates increased oxidative stress. The intracellular ROS level in PC12 cells was measured by using DCFH-DA in this study. It was found that 300 μM 6OHDA induced an increase in intracellular ROS level in a time-dependent manner (Fig. 2a). Pre-treatment of PC12 cells with 10 μM I3O for 2 h significantly reduced the increase in intracellular ROS levels induced by 6OHDA, suggesting that I3O could attenuate 6OHDA-induced oxidative stress in PC12 cells (Fig. 2b).
I3O significantly prevents 6OHDA-induced ROS accumulation in PC12 cells. a I3O prevents 6OHDA-induced ROS accumulation in PC12 cells in a time-dependent manner. PC12 cells were pre-treated with or without 10 μM I3O for 2 h, and then exposed to 300 μM 6OHDA for various durations as indicated. The intracellular ROS level was measured using DCFH-DA after the 6OHDA challenge. b I3O effectively prevents 6OHDA-induced ROS accumulation in PC12 cells at 4 h after 6OHDA challenge. PC12 cells were pre-treated with or without 10 μM I3O for 2 h, and then exposed to 300 μM 6OHDA. Intracellular ROS level was measured at 4 h after 6OHDA challenge. ** p < 0.01 versus 6OHDA group
6OHDA Increases the Activity of GSK3β in PC12 Cells
It was reported that I3O is a potent inhibitor of GSK3β and CDK5 with IC50 values of 22 and 100 nM, respectively (Leclerc et al. 2001). To determine whether the activation of GSK3β and/or CDK5 is involved in 6OHDA-induced cell death, we used GSK3β inhibitors, LiCl (IC50 2 mM) and SB415286 (IC50 77 nM), and CDK5 inhibitors, 3-amino-1H-pyrazolo[3,4-b]quinoxaline (IC50 400 nM) and roscovitine (IC50 160 nM). The inhibitors were pre-treated for 2 h before 6OHDA challenge. It was found that LiCl (3–10 mM) and SB415286 (3–10 μM) significantly protected PC12 cells against 6OHDA-induced cell death (Fig. 3a). However, neither 3-amino-1H-pyrazolo[3,4-b]quinoxaline (1–30 μM) nor roscovitine (1–30 μM) could prevent 6OHDA-induced cell death at the same condition (Fig. 3b). We have also determined the level of phospho-Ser9 GSK3β by using Western blotting analysis. As shown in Fig. 3c, 6OHDA at 300 μM time-dependently decreased the level of phospho-Ser9 GSK3β, suggesting that 6OHDA increased the activity of GSK3β. Collectively, our findings suggested that the activation of GSK3β is involved in 6OHDA-induced cell death in PC12 cells, and I3O, a potent GSK3β inhibitor, might prevent 6OHDA-induced cell death via inhibiting GSK3β.
The activation of GSK3β contributes to 6OHDA-induced neuronal death in PC12 cells. a GSK3β inhibitors efficiently prevent 6OHDA-induced neuronal death in a concentration-dependent manner. PC12 cells were pre-treated with LiCl or SB415286 at the indicated concentrations for 2 h, and then exposed to 300 μM 6OHDA. Cell viability was measured by the MTT assay at 6 h after 6OHDA challenge. b CDK5 inhibitors could not prevent 6OHDA-induced neuronal death. PC12 cells were pre-treated with 3-amino-1H-pyrazolo[3,4-b]quinoxaline or roscovitine at the indicated concentrations for 2 h, and then exposed to 300 μM 6OHDA. Cell viability was measured by the MTT assay at 6 h after 6OHDA challenge. * p < 0.05 and ** p < 0.01 versus 6OHDA group. c 6OHDA decreases the level of phospho-Ser9 GSK3β in PC12 cells in a time-dependent manner. PC12 cells were incubated with 300 μM 6OHDA for various durations as indicated. The total proteins were extracted for Western blotting analysis with specific antibodies. ** p < 0.01 versus control group
I3O Prevents 6OHDA-Induced MEF2D Dysregulation in PC12 Cells
It is reported that the inhibition of GSK3β could enhance MEF2 transcriptional activity (Leclerc et al. 2001). Therefore, we tested if I3O increased MEF2D activity in our model. We transfected PC12 cells with MEF2-dependent luciferase reporter construct. In transfected cells, exposure of 6OHDA led to a significant decrease in MEF2 transcriptional activity. At the same condition, I3O significantly enhanced MEF2 transcriptional activity in 6OHDA-treated cells (Fig. 4a). Moreover, 6OHDA-induced decrease of MEF2 transcriptional activity could be greatly attenuated by GSK3β inhibitors, suggesting that I3O might enhance MEF2 transcriptional activity via directly inhibiting GSK3β.
I3O markedly prevents 6OHDA-induced MEF2D dysregulation in PC12 cells. a I3O and GSK3β inhibitors significantly prevent 6OHDA-induced decrease of MEF2 transcriptional activity. PC12 cells transfected with a MEF2 luciferase reporter gene were pre-treated with I3O, LiCl, or SB415286 at the indicated concentrations for 2 h, and then exposed to 300 μM 6OHDA. The luciferase activity was determined at 6 h after 6OHDA challenge. ** p < 0.01 versus 6OHDA group. b I3O and LiCl significantly prevent 6OHDA-induced decrease of nuclear localized MEF2D expression. PC12 cells were pre-treated with 10 μM I3O or 10 mM LiCl for 2 h, and then exposed to 300 μM 6OHDA for 6 h. Lysates of nuclei and cytoplasm extracts from these PC12 cells were probed for MEF2D, Histone-H3 (nuclei loading control), and α-tubulin (cytoplasm loading control). ** p < 0.01 versus control group, and ## p < 0.01 versus 6OHDA group
MEF2D has been shown to act as a transcriptional factor in the nuclei of cells (Yang and Mao 2010). Therefore, we further investigated the effects of I3O on nuclear localized MEF2D expression. 6OHDA greatly reduced nuclear localized MEF2D expression in PC12 cells, whereas I3O significantly prevented the decrease of nuclear localized MEF2D expression induced by 6OHDA (Fig.4b). At the same condition, 6OHDA-induced decrease of nuclear localized MEF2D expression could be prevented by LiCl, suggesting that I3O might prevent 6OHDA-induced MEF2D dysregulation via inhibiting GSK3β.
MEF2D Reduction Significantly Abolishes the Neuroprotective Effects of I3O in PC12 Cells
To further determine whether the neuroprotective effects of I3O were through the activation of MEF2D, ShRNA was performed. MEF2D ShRNA (ShMEF2D) caused a significant reduction in MEF2D protein level, whereas the negative control ShRNA (ShNC) and vector had no effect on MEF2D protein level (Fig. 5a). The reduction of MEF2D by ShRNA significantly abolished the neuroprotective effects of I3O against 6OHDA-induced cell death (Fig. 5b), suggesting that the neuroprotective effects of I3O were mainly through the activation of MEF2D. And notably, in our PC12 cell model, knockdown of MEF2D by ShRNA had no overt effect on cell viability, which is consistent with that reported in the previous study (She et al., 2011). It has been well documented that 6OHDA induced neurotoxicity via acting multiple targets or pathways, particularly including N-Methyl-D-aspartate receptors (Fiorentini et al., 2006; Michel et al., 2014), mitochondria (Tobon-Velasco et al., 2013), mitogen-activated protein kinases (Gomez-Lazaro et al., 2008), and MEF2D (Gao et al., 2014). This explained why 6OHDA and ShRNA-mediated silencing of MEF2D did not result in a significant decrease in cell viability synergistically. As such, I3O effectively and partially, but not completely, prevented 6OHDA-induced neurotoxicity via activating MEF2D in our cell model.
MEF2D reduction significantly abolishes the neuroprotective effects of indirubin-3-oxiime against 6OHDA-induced neuronal death in PC12 cells. a PC12 cells were transfected with pG418-GFP plasmid (vector), pG418-GFP plasmid encoding MEF2D ShRNA (ShMEF2D) and pG418-GFP plasmid encoding negative control ShRNA (ShNC). The extracted proteins were subjected to Western blot analysis using anti-MEF2D and β-actin antibodies. b Cells were pre-treated with or without 10 μM I3O for 2 h, and then exposed to 300 μM 6OHDA. Cell viability was measured at 6 h after 6OHDA challenge by MTT assays. ** p < 0.01 versus 6OHDA group; ## p < 0.01 versus I3O and 6OHDA in ShMEF2D group
Discussion
In this study, we have demonstrated, for the first time, that I3O protected against 6OHDA-induced neurotoxicity in PC12 cells. Our study further revealed that the neuroprotective effects of I3O were mediated through the activation of MEF2D, possibly via the direct inhibition of GSK3β.
We have previously reported that 6 h treatment of 300 μM 6OHDA resulted in the decrease of cell viability, the increased number of cells with apoptotic bodies, and the reduction of mitochondrial membrane potential in PC12 cells, suggesting that 6OHDA mainly induces cell apoptosis in our model (Zhang et al. 2011). Moreover, in our experiments with 6OHDA, cells were treated in a low serum (1 % FBS) medium for a relative short period (6 h) in order to decrease cell proliferation. Therefore, in this study, I3O prevented 6OHDA-induced decrease of cell viability mainly via protecting against cell death but not increasing cell proliferation. This finding was further confirmed by Hoechst staining which showed that the number of pyknotic bodies increased by 6OHDA was significantly decreased by the pre-treatment of I3O. Furthermore, we have demonstrated that I3O suppressed the increase of intracellular ROS induced by 6OHDA. These findings are consistent with a previous report that pre-treatment with I3O substantially decreased lipopolysaccharide-induced ROS production in primary microglia cultures (Jung et al. 2010). Collectively, our results showed that I3O significantly prevented 6OHDA-induced neurotoxicity.
How I3O produced neuroprotective effects against 6OHDA-induced neurotoxicity? I3O is a potent inhibitor of GSK3β and CDK5 (Leclerc et al. 2001). Previous studies have shown that both GSK3β and CDK5 cascades play important roles in PD neurotoxin-induced neuronal death (Chen et al. 2004; Zhang et al. 2012a). Therefore, we examined if the inhibition of GSK3β and/or CDK5 is involved in the neuroprotective effects of I3O. We found that (1) GSK3β inhibitors but not CDK5 inhibitors significantly produced neuroprotective effects; and (2) 6OHDA substantially increased GSK3β activity, suggesting that I3O might produce its neuroprotective effects via the inhibition of GSK3β. These findings are consistent with a previous study that I3O prevented MPTP-induced dopaminergic neuronal loss and behavioral abnormity through inhibiting GSK3β in rats (Wang et al. 2007).
Dysfunction of survival factor MEF2D has been shown to underlie the loss of dopaminergic neurons in the substantial nigra pars compacta and the pathogenic process of PD (Wang et al. 2014), strongly suggesting MEF2D has emerged as a novel and effective therapeutic target in treating PD. Indeed, several lines of evidence have shown that enhancing MEF2D in vivo could protect dopaminergic neurons in an animal model of PD (Smith et al. 2006; She et al. 2011). However, those studies enhanced MEF2D using recombinant viral approach to enhance MEF2D, which clearly had its limits in clinical practice (Yang et al. 2009; She et al. 2011). It is, therefore, necessary to find small molecules which could enhance MEF2D transcriptional activity. We demonstrated that 6OHDA remarkably reduced MEF2 transcriptional activity and decreased nuclear localized MEF2D expression, which is consistent with a previous study that 6OHDA-induced apoptosis is mediated by MEF2D down-regulation in PC12 cells (Kim et al. 2011). We further explored if I3O could act on MEF2D to produce neuroprotective effects. We found that (1) I3O prevented 6OHDA-dysregulated MEF2D; and (2) genetic depletion of MEF2D significantly abolished the neuroprotective effects of I3O, clearly demonstrating that I3O produced neuroprotective effects via the activation of MEF2D. Moreover, LiCl, a GSK3β inhibitor, prevented 6OHDA-dysregulated MEF2D in our model, which is consistent with previous studies that GSK3β could inhibit MEF2D transcriptional activity in neurons (Leclerc et al. 2001; Wang et al. 2009). These findings further supported that I3O might prevent MEF2D dysregulation possibly via inhibiting GSK3β. I3O might, therefore, provide an effective as well as practical approach of enhancing MEF2D transcriptional activity and a promising anti-PD drug candidate.
Although I3O and other GSK3β inhibitors could fully prevent 6OHDA-induced decrease of MEF2 transcriptional activity and nuclear localized MEF2D expression, they could not completely protect against 6OHDA-induced cell death. We speculated that although GSK3β-mediated MEF2D dysregulation was implicated in the neurotoxicity, the contribution of MEF2D dysregulation to the neurotoxicity in our model may be partial. Other factors such as the dysregulation of mitogen-activated protein kinase signaling pathways, the inactivation of transcriptional factor Nrf2, and the activation of nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) pathway were also reported to be involved in 6OHDA-induced neurotoxicity (Tobon-Velasco et al. 2012; Zhang et al. 2012b). Therefore, the neuroprotective effects from inhibiting GSK3β may not be enough to completely block neuronal death.
In summary, our findings demonstrated that I3O protected against 6OHDA-induced neurotoxicity in PC12 cells. Moreover, we have shown that these neuroprotective effects of I3O were mediated through the activation of MEF2D, possibly via the inhibition of GSK3β. Given the importance of MEF2D in neuronal survival and the capability of I3O to cross the blood–brain barrier, our finding indicated that I3O might be a novel drug candidate for various neurodegenerative disorders, including PD in particular.
Abbreviations
- CDKs:
-
Cyclin-dependent kinases
- CNS:
-
Central nervous system
- DCF:
-
2′,7′-dichlorofluorescein
- DCFH-DA:
-
2′7′-dichlorodihydrofluorescein diacetate
- DMEM:
-
Dulbecco’s modified Eagle’s medium
- FBS:
-
Fetal bovine serum
- GSK3β:
-
Glycogen synthase kinase 3β
- MEF2:
-
Myocyte enhancer factor 2 indirubin-3-oxime I3O
- MPTP:
-
1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine
- MTT:
-
3(4,5-dimethylthiazol-2-yl)-2.5-diphenyltetrazolium bromide
- PBS:
-
Phosphate buffered saline
- PD:
-
Parkinson’s disease
- ROS:
-
reactive oxygen species
- ShRNA:
-
Short hairpin RNA
- 6OHDA:
-
6-hydroxydopamine
Reference
Barnham KJ, Masters CL, Bush AI (2004) Neurodegenerative diseases and oxidative stress. Nat Rev Drug Discov 3:205–214
Bove J, Prou D, Perier C, Przedborski S (2005) Toxin-induced models of Parkinson's disease. NeuroRx 2:484–494
Camins A, Verdaguer E, Junyent F, Yeste-Velasco M, Pelegri C, Vilaplana J, Pallas M (2009) Potential mechanisms involved in the prevention of neurodegenerative diseases by lithium. CNS Neurosci Ther 15:333–344
Chebel A, Kagialis-Girard S, Catallo R, Chien WW, Mialou V, Domenech C, Badiou C, Tigaud I, Ffrench M (2009) Indirubin derivatives inhibit malignant lymphoid cell proliferation. Leuk Lymphoma 50:2049–2060
Chen G, Bower KA, Ma C, Fang S, Thiele CJ, Luo J (2004) Glycogen synthase kinase 3beta (GSK3beta) mediates 6-hydroxydopamine-induced neuronal death. FASEB J 18:1162–1164
Cui W., Zhang Z., Li W., Mak S., Hu S., Zhang H., Yuan S., Rong J., Choi T. C., Lee S. M. and Han Y. (2012) Unexpected neuronal protection of SU5416 against 1-methyl-4-phenylpyridinium ion-induced toxicity via inhibiting neuronal nitric oxide synthase. PLoS One 7, e46253.
Cui W, Zhang ZJ, Hu SQ, Mak SH, Xu DP, Choi CL, Wang YQ, Tsim WK, Lee MY, Rong JH, Han YF (2014) Sunitinib produces neuroprotective effect via inhibiting nitric oxide overproduction. CNS Neurosci Ther 20:244–252
Cui W, Zhang Z, Li W, Hu S, Mak S, Zhang H, Han R, Yuan S, Li S, Sa F, Xu D, Lin Z, Zuo Z, Rong J, Ma ED, Choi TC, Lee SM, Han Y (2013) The anti-cancer agent SU4312 unexpectedly protects against MPP(+)-induced neurotoxicity via selective and direct inhibition of neuronal NOS. Br J Pharmacol 168:1201–1214
Ding Y, Qiao A, Fan GH (2010) Indirubin-3′-monoxime rescues spatial memory deficits and attenuates beta-amyloid-associated neuropathology in a mouse model of Alzheimer’s disease. Neurobiol Dis 39:156–168
Flavell SW, Cowan CW, Kim TK, Greer PL, Lin Y, Paradis S, Griffith EC, Hu LS, Chen C, Greenberg ME (2006) Activity-dependent regulation of MEF2 transcription factors suppresses excitatory synapse number. Science 311:1008–1012
Fiorentini C, Rizzetti MC, Busi C, Bontempi S, Collo G, Spano P, Missale C (2006) Loss of synaptic D1 dopamine/N-methyl-D-aspartate glutamate receptor complexes in L-DOPA-induced dyskinesia in the rat. Mol Pharmacol 69:805–812
Gao L, She H, Li W, Zeng J, Zhu J, Jones DP, Mao Z, Gao G, Yang Q (2014) Oxidation of survival factor MEF2D in neuronal death and Parkinson’s disease. Antioxid Redox Signal 20:2936–2948
Gomez-Lazaro M, Galindo MF, Concannon CG, Segura MF, Fernandez-Gomez FJ, Llecha N, Comella JX, Prehn JH, Jordan J (2008) 6-hydroxydopamine activates the mitochondrial apoptosis pathway through p38 MAPK-mediated, p53-independent activation of Bax and PUMA. J Neurochem 104:1599–1612
Hu S, Wang R, Cui W, Zhang Z, Mak S, Xu D, Choi C, Tsim KW, Carlier PR, Lee M, Han Y (2014) Inhibiting beta-amyloid-associated Alzheimer’s pathogenesis in vitro and in vivo by a multifunctional dimeric bis(12)-hupyridone derived from its natural analogue. J Mol Neurosci 55:1014–1021
Hu SQ, Cui W, Xu DP, Mak SH, Tang J, Choi CL, Pang YP, Han YF (2013) Substantial neuroprotection against K+ deprivation-induced apoptosis in primary cerebellar granule neurons by novel dimer bis(propyl)-cognitin via the activation of VEGFR-2 signaling pathway. CNS Neurosci Ther 19:764–772
Jung HJ, Nam KN, Son MS, Kang H, Hong JW, Kim JW, Lee EH (2010) Indirubin-3′-oxime inhibits inflammatory activation of rat brain microglia. Neurosci Lett 487:139–143
Kim MK, Kim SC, Kang JI, Hyun JH, Boo HJ, Eun SY, Park DB, Yoo ES, Kang HK, Kang JH (2011) 6-hydroxydopamine-induced PC12 cell death is mediated by MEF2D down-regulation. Neurochem Res 36:223–231
Kupershmidt L, Amit T, Bar-Am O, Youdim MB, Blumenfeld Z (2007) The neuroprotective effect of activin A and B: implication for neurodegenerative diseases. J Neurochem 103:962–971
Leclerc S, Garnier M, Hoessel R, Marko D, Bibb JA, Snyder GL, Greengard P, Biernat J, Wu YZ, Mandelkow EM, Eisenbrand G, Meijer L (2001) Indirubins inhibit glycogen synthase kinase-3 beta and CDK5/p25, two protein kinases involved in abnormal tau phosphorylation in Alzheimer’s disease. A property common to most cyclin-dependent kinase inhibitors? J Biol Chem 276:251–260
Liao XM, Leung KN (2013) Indirubin-′-oxime induces mitochondrial dysfunction and triggers growth inhibition and cell cycle arrest in human neuroblastoma cells. Oncol Rep 29:371–379
Mao Z, Bonni A, Xia F, Nadal-Vicens M, Greenberg ME (1999) Neuronal activity-dependent cell survival mediated by transcription factor MEF2. Science 286:785–790
Michel A., Downey P., Nicolas J. M. and Scheller D. (2014) Unprecedented therapeutic potential with a combination of A2A/NR2B receptor antagonists as observed in the 6-OHDA lesioned rat model of Parkinson’s disease. PLoS One 9, e114086.
Obeso JA, Rodriguez-Oroz MC, Goetz CG, Marin C, Kordower JH, Rodriguez M, Hirsch EC, Farrer M, Schapira AH, Halliday G (2010) Missing pieces in the Parkinson’s disease puzzle. Nat Med 16:653–661
She H, Yang Q, Shepherd K, Smith Y, Miller G, Testa C, Mao Z (2011) Direct regulation of complex I by mitochondrial MEF2D is disrupted in a mouse model of Parkinson disease and in human patients. J Clin Invest 121:930–940
Smith PD, Mount MP, Shree R, Callaghan S, Slack RS, Anisman H, Vincent I, Wang X, Mao Z, Park DS (2006) Calpain-regulated p35/cdk5 plays a central role in dopaminergic neuron death through modulation of the transcription factor myocyte enhancer factor 2. J Neurosci 26:440–447
Tobon-Velasco JC, Limon-Pacheco JH, Orozco-Ibarra M, Macias-Silva M, Vazquez-Victorio G, Cuevas E, Ali SF, Cuadrado A, Pedraza-Chaverri J, Santamaria A (2012) 6-OHDA-induced apoptosis and mitochondrial dysfunction are mediated by early modulation of intracellular signals and interaction of Nrf2 and NF-kappaB factors. Toxicology 304:109–119
Wang B, Cai Z, Lu F, Li C, Zhu X, Su L, Gao G, Yang Q (2014) Destabilization of survival factor MEF2D mRNA by neurotoxin in models of Parkinson’s disease. J Neurochem 130:720–728
Wang W, Yang Y, Ying C, Li W, Ruan H, Zhu X, You Y, Han Y, Chen R, Wang Y, Li M (2007) Inhibition of glycogen synthase kinase-3beta protects dopaminergic neurons from MPTP toxicity. Neuropharmacology 52:1678–1684
Wang X, She H, Mao Z (2009) Phosphorylation of neuronal survival factor MEF2D by glycogen synthase kinase 3beta in neuronal apoptosis. J Biol Chem 284:32619–32626
Xie Y, Liu Y, Ma C, Yuan Z, Wang W, Zhu Z, Gao G, Liu X, Yuan H, Chen R, Huang S, Wang X, Zhu X, Wang X, Mao Z, Li M (2004) Indirubin-3′-oxime inhibits c-Jun NH2-terminal kinase: anti-apoptotic effect in cerebellar granule neurons. Neurosci Lett 367:355–359
Xu H., Li Q., Yin Y., Lv C., Sun W., He B., Liu R., Chen X. and Bi K. Simultaneous determination of three alkaloids, four ginsenosides and limonin in the plasma of normal and headache rats after oral administration of Wu-Zhu-Yu decoction by a novel ultra fast liquid chromatography-tandem mass spectrometry method: application to a comparative pharmacokinetics and ethological study. J Mass Spectrom 48, 519–532.
Yang Q, Mao Z (2010) Dysregulation of autophagy and Parkinson’s disease: the MEF2D link. Apoptosis 15:1410–1414
Yang Q, She H, Gearing M, Colla E, Lee M, Shacka JJ, Mao Z (2009) Regulation of neuronal survival factor MEF2D by chaperone-mediated autophagy. Science 323:124–127
Yao L, Li W, She H, Dou J, Jia L, He Y, Yang Q, Zhu J, Capiro NL, Walker DI, Pennell KD, Pang Y, Liu Y, Han Y, Mao Z (2012) Activation of transcription factor MEF2D by bis(3)-cognitin protects dopaminergic neurons and ameliorates Parkinsonian motor defects. J Biol Chem 287:34246–34255
Zhang H, Mak S, Cui W, Li W, Han R, Hu S, Ye M, Pi R, Han Y (2011) Tacrine(2)-ferulic acid, a novel multifunctional dimer, attenuates 6-hydroxydopamine-induced apoptosis in PC12 cells by activating Akt pathway. Neurochem Int 59:981–988
Zhang L, Liu W, Szumlinski KK, Lew J (2012a) p10, the N-terminal domain of p35, protects against CDK5/p25-induced neurotoxicity. Proc Natl Acad Sci U S A 109:20041–20046
Zhang S, Zhang Y, Xu L, Lin X, Lu J, Di Q, Shi J, Xu J (2009) Indirubin-3′-monoxime inhibits beta-amyloid-induced neurotoxicity in neuroblastoma SH-SY5Y cells. Neurosci Lett 450:142–146
Zhang Z, Cui W, Li G, Yuan S, Xu D, Hoi MP, Lin Z, Dou J, Han Y, Lee SM (2012b) Baicalein protects against 6-OHDA-induced neurotoxicity through activation of Keap1/Nrf2/HO-1 and involving PKCalpha and PI3K/AKT signaling pathways. J Agric Food Chem 60:8171–8182
Acknowledgments
This work was supported by grants from the Research Grants Council of Hong Kong (561011, 15101014), the Hong Kong Polytechnic University (G-SB10 and G-UC15), China Postdoctoral Science Foundation Grant (2015 M570753), the National Natural Science Foundation of China (81202510), Ningbo International Science and Technology Cooperation Project (No. 2014D10019), the Science and Technology Development Fund of Macao SAR (Ref. No. 134/2014/A3), and the Research Committee, University of Macau (Ref. No. MYRG2015-00214-ICMS-QRCM3).
Author information
Authors and Affiliations
Corresponding author
Additional information
Shengquan Hu and Wei Cui contributed equally to this work.
Rights and permissions
About this article
Cite this article
Hu, S., Cui, W., Zhang, Z. et al. Indirubin-3-Oxime Effectively Prevents 6OHDA-Induced Neurotoxicity in PC12 Cells via Activating MEF2D Through the Inhibition of GSK3β. J Mol Neurosci 57, 561–570 (2015). https://doi.org/10.1007/s12031-015-0638-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12031-015-0638-y