Abstract
The transforming growth factor β (TGF-β) pathway plays a key role in oncogenesis of advanced cancers, involving the non-Smad and Smad pathways. Meanwhile, nucleolin on the cell surface has been also reported to affect activation of signaling pathways. However, the effect of cell surface nucleolin on TGF-β pathway in glioblastoma is not still understood. Here, using antibodies of nucleolin and TGF-β receptor I (TβR-I), we observed blocking of either nucleolin or TβR-I inhibited the phosphorylation of CrkL, Erk1/2, and Smad2. Using nucleolin siRNA, nucleolin knockdown was also identified to suppress the expression of p-CrkL, p-Erk1/2, and p-Smad2. Furthermore, immunoprecipitation revealed the interaction between cell surface nucleolin and TβR-I on the U87 cell membrane. In addition, U87 cell wound-healing, soft-agar and MTT assay also showed si-nucleolin could obviously impair wound closure (p < 0.001), colony formation (p < 0.001) and cell growth (p < 0.001). In conclusion, nucleolin promotes and regulates the TGF-β pathway by interacting with TβR-I and is required for initiation and activation of TGF-β signaling. Thus, nucleolin could be a key factor in glioblastoma pathogenesis and considered a therapeutic target, which may also mediate more signaling pathways.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glioblastoma is the most common and deadly one of human brain tumors (Vehlow and Cordes 2013; Wen and Kesari 2008), whose underlying molecular mechanism was not fully unraveled. To date, TGF-β pathway has been focused on and considered a therapeutic target, due to its involvement in cell proliferation (Pickup et al. 2013) and epithelial-mesenchanyal transition (Katsuno et al. 2013).
TGF-β activates a heterodimeric complex comprising TβR-I and TβR-II, and initiates a signaling cascade through phosphorylation of the specific receptor-regulated Smad2/3 (Weiss and Attisano 2013; Shi and Massague 2003). Similarly, the non-Smad independent signaling mediated by TGF-β is also believed to be crucial in tumor progression (Davies et al. 2005; Drabsch and ten Dijke 2012).
Nucleolin, a major component of nucleolar proteins, is located widely in the nucleolus and cytoplasm (Ginisty et al. 1999), and over-expressed in human cancers, such as colon cancer (Reyes-Reyes and Akiyama 2008) and breast cancer (Litchfield et al. 2012). Intriguingly, nucleolin is also identified on the cell surface and suggested as a receptor of laminin-1 (Turck et al. 2006) and P-selectin, or as a collaborative receptor that is responsible for tyrosine phosphatase-sigma ectodomain in skeletal muscle (Alete et al. 2006). Besides, nucleolin had the anti-angiogenic effect through mediating endocytosis and translocation of endostatin (Song et al. 2012). Notably, Chandra et al. reported that in transformed breast cancer cells, TβR-I translocated to the nucleus depending on nuclear proteins upon activation by TGF-β (Chandra et al. 2012). So we hypothesized that nucleolin may be implicated in TGF-β pathway.
However, the role of cell surface nucleolin in TGF-β signaling pathway was not elucidated in glioblastoma. In the present study, small interfering RNA or antibodies was used to repress or antagonize cell surface nucleolin of U87 cells, and then CrkL, Erk1/2, and Smad2 was immunoblotted. Most importantly, immunoprecipitation was also applied to investigate the association between nucleolin and TβR-I.
Materials and Methods
Cell Culture and Reagents
The human glioblastoma cell lines U87 was purchased from American Type Culture Collection (ATCC, Manassas, Va.), and was cultured in DMEM (Gibco) supplemented with 10 % fetal bovine serum (FBS; Hyclone) and 100 U/mL penicillin/streptomycin (Gibco) and were maintained in a humidified atmosphere with 5 % CO2 at 37 °C. TGF-β1 was purchased from R&D Systems.
Nucleolin siRNA Transfection
Cell lines were seeded in a 6-cm dish at density of 5 × 105 cells/dish and incubated overnight. U87 cells were prepared for transfection of si-nucleolin (a generous gift from Dr. Lee). One milligram of si-nucleolin was added to Opti-MEM with Lipofectamine 2000 (Invitrogen) for transfection, according to the manufacturer’s instructions. Twelve hours following incubation, medium was changed into fresh DMEM containing 10 % FBS. Cells were harvested at 72 h following transfection of si-nucleolin. Then cells were subjected to western blot, wound healing assay, agar assay and MTT.
Western Blotting
Total protein from cultured cells was extracted in cell lysis buffer (PIERCE, Rockford, IL) and quantified using the BSA method. A 10 % SDS-PAGE was performed, and 30 μg of protein of each sample were analyzed. Proteins in the SDS gels were transferred to a polyvinylidene difluoride membrane by an electroblot apparatus. Membranes were incubated with primary antibodies: anti-p-CrkL, anti-CrkL, anti-p-Erk1/2, anti-Erk1/2, anti-p-Smad2, and anti-Smad2 (Santa Cruz Biotech) anti-β-actin (Santa Cruz Biotech). Antibody recognition was detected with either anti-mouse IgG or anti-rabbit IgG antibody linked to horseradish peroxidase (Sigma). Immunocomplexes were visualized by ECL (Amersham Pharmacia Biotech).
Immunoprecipitation
Cells were homogenized, and the supernatant and pellet fractions were obtained by centrifugation (100,000 × g, 40 min). Pellet fractions were incubated under gentle shaking at 4 °C overnight with a mixture of anti-nucleolin antibodies and protein A agarose in 300 ml of immunoprecipitation buffer (20 mM HEPES, pH 7.9, 420 mM NaCl, 1.5 mM MgCl2 and 25 % glycerol (v/v), 0.5 mM phenylmethylsulfonyl fluoride, 1 mM orthovanadate, 2 mg/ml pepstatin A and 2 mg/ml leupeptin). Beads were pelleted at 7,500 g for 2 min and washed three times with RIPA buffer (50 mM Tris–HCl, pH 7.5, 1 % IGEPAL CA-630 (v/v), 150 mM NaCl, and 0.5 % sodium deoxycholate). Protein was removed from the beads by boiling in sample buffer (120 mM Tris–HCl, pH 6.8, 10 % glycerol, 3 % SDS, 20 mM DTT, and 0.4 % bromophenol blue) for 5 min and subjected to 10 % SDS-PAGE. Western blot was carried out as described above.
Wound-Healing Assay
For analysis of cell motility, cells were seeded onto 10-cm diameter plates in DMEM with 10 % FBS overnight. The injury line was created in confluent cells by cell scraping using a pipette tip and was washed with medium to remove free-floating cells and debris. Wound healing within the scrape line was recorded every day.
Soft Agar Assay and MTT
Cell invasiveness was examined using a soft agar colony formation assay. Cells were plated at 4 × 104 in 60-mm culture wells in 3 ml of DMEM containing 0.36 % agar on a layer containing 5 ml of the same medium and 0.7 % agar. Three weeks following plating, cell colonies were stained with 3-(4,5-dimethylthiazol-2-yl)-2, 5-diphenyl tetrazolium bromide (MTT) (Sigma) and photographed. Cells were plated onto 96-well plates. Additionally, at various time points indicated, MTT was added to cells for 2 h, and then solutions were removed, DMSO was used to dissolve the MTT salt, and OD values were measured at 590 nm.
Statistical Analysis
An unpaired Student’s t-test was used to calculate differences between means. Differences were considered significant as p < 0.01. All data presented with mean ± SD.
Results
TGF-β signaling activation was suppressed by either nucleolin or TβR-I antibody.
To figure out the effect of nucleolin on TGF-β signaling activation, we used the nucleolin antibody to block U87 cells, with TβR-I antibody as comparison. Precious work has shown that CrkL and Erk1/2 was a key indicator in the non-Smad pathway, as Smad2 in the Smad pathway, so CrkL, Erk1/2, and Smad2 were detected. We observed that compared with control, blocking TβR-I markedly decreased the phosphorylation ratio of CrkL, Erk1/2 (Fig. 1a) and Smad2 (Fig. 1b). That is, the TGF-β signaling pathway was not nearly activated (non-Smad and Smad pathways). Subsequently, antagonizing cell surface nucleolin with nucleolin antibody also obviously reduced the expression of p-CrkL, p-Erk1/2, and p-Smad2 (Fig. 2). All of these suggested that nucleolin suppressed the activation and initiation of TGF-β signaling pathway.
The effect of TβR-I antibody on TGF-β signaling in U87 cells. U87 cells were serum-starved for 24 h and then treated by anti-TβR-I or IgG antibodies (control). Subsequently, U87 was exposed to TGF-β (100 ng/ml) or not for 60 min. Western blot was conducted for CrkL, Erk1/2 (a) and Smad2 (b), with β-actin as an internal control. Data from three independent experiments was expressed as the mean ± SD. The proportion of phosph-/total- represents the phosphorylation ratio. *p < 0.01, anti-nucleolin (TGF-β+) versus control (TGF-β+)
The effect of nucleolin antibody on TGF-β signaling in U87 cells. U87 cells were serum-starved for 24 h and then treated by anti-TβR-I or IgG antibodies (control). Subsequently, U87 was exposed to TGF-β1 (100 ng/ml) or not for 60 min. Western blot was conducted for CrkL, Erk1/2 (a) and Smad2 (b), with β-actin as a internal control. Data from three independent experiments was expressed as the mean ± SD. The proportion of phosph-/total- represented the phosphorylation ratio. *p < 0.01, anti-nucleolin (TGF-β+) versus control (TGF-β+)
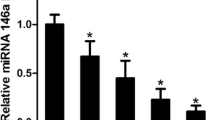
Nucleolin Knockdown Inhibited the Initiation of TGF-β Signaling
To further determine the impact of nucleolin on TGF-β pathway, we conducted endogenous nucleolin knockdown with si-nucleolin. Following nucleolin knockdown, we examined the activation status of TGF signaling. For this purpose, U87 cells were subjected to western blot. Our results revealed that in non-Smad pathway, p-CrkL and p-Erk1/2 downregulated significantly (p < 0.000, versus control; Fig.3a); in the Smad pathways, p-Smad2 level also greatly decreased (p < 0.000, versus control; Fig. 3b). Conversely, in U87 cells without si-nucleolin, p-CrkL p-Erk1/2, and p-Smad2 showed unaffected, indicating that nucleolin knockdown indeed inhibited TGF-β signaling. These results suggested that cell surface nucleolin exhibited the same active effect with TβR-I, inferring nucleolin can be required for the interaction of TGF-β and TβR-I.
The effect of si-nucleolin on TGF-β signaling in U87 cells. U87 cells were transfected with si-control or si-nucleolin for 72 h and then treated with TGF-β1 (100 ng/ml). CrkL, Erk1/2 (a) and Smad2 (b) were subjected to immunoblot analysis, with β-actin as an internal control. Data from three independent experiments was expressed as the mean ± SD. *p < 0.01, versus control (TGF-β+)
Nucleolin Interacted with TβR-I
Based on the precious hypothesis that cell surface nucleolin interacted with TβR-I, we conducted immunoprecipitation. Lysates of U87 cells were separated into supernatant and pellet, and then pellet was precipitated with anti-nucleolin antibody and blotted with anti-TβR-I antibody. As shown in Fig. 4, 30 min following TGF-β treatment, TβR-I was immunoprecipitated by nucleolin antibody in the group without si-nucleolin, whereas in the group with si-nucleolin, TβR-I was not examined in immunoprecipitates. Differences were significant (p < 0.001). Our data testified that once U87 was stimulated by TGF-β, cell surface nucleolin wound bind to TβR-I on plasma membrane and then prompted TGF/TβR-I interaction. Taken together, nucleolin indeed acted as a key component of TGF-β pathway.
Nucleolin suppressed U87 cellular biology induced by TGF-β
As a consequence of the involvement of nucleolin in the initiation of TGF-β, we decided to address the effect of nucleolin on U87 cellular biology. In our study, wound-healing assay and soft agar assay were introduced. As was shown in Fig. 5a, in wound-healing assay, nucleolin knockdown efficiently decreased wound-healing velocity of U87 cells (p < 0.001, versus control and TGF-β-). In comparison with control, the ability of wound closure was decreased by about 40 %, suggesting U87 cell migration capacity was significantly injured by si-nucleolin. By MTT assay (Fig. 5b), si-nucleolin also lowered TGF-β mediated cell growth with significant differences (p < 0.001, versus control). In addition, the soft agar assay also revealed that si-nucleolin effectively reduced the invasiveness by average 55% (p < 0.001, versus control, data and figures not shown). All of the above indicated that nucleolin was essential to prompt U87 cell proliferation, migration, and invasiveness.
The effect of nucleolin on proliferation, migration, and invasiveness of U87 cells. a Wound-healing assay was performed as mentioned above. The wound line was created in confluent U87 cells using a pipette tip. Wound healing within the scrape line was recorded every day. Representative scrape lines are shown at the first 24 h; dashed line indicates the margin of the scratch. The average initial wound width was measured and defined as 100 %. b Cells were transfected with si-control or si-nucleolin for 72 h prior to exposure with TGF-β1 (100 ng/ml) or not. Then cell growth curve and the results of the inhibitory rates of cell growth were applied to absorbance at 590 nm. Data from three independent experiments was expressed as the mean ± SD. *p < 0.001, versus control and TGF-β (−)
Discussion
In recent years, TGF-β has been reported to prompt tumor progression and invasion by TGF-β signaling pathway in high-grade gliomas (Kjellman et al. 2000). Additionally, cell surface nucleolin is also abundant in proliferative cancer cells, and mediating multiple biological effects. Up to now, the role of nucleolin in TGF-β signaling has been not well clarified, especially in glioblastoma. Since the activated TGF-β signaling leads to the activation of CrkL and Erk1/2 of non-Smad pathway as well as Smad2 of Smad pathway (Lv et al. 2013; Sun et al. 2014), by which we examined the status of TGF-β signaling to throw light on the potential effects of nucleolin.
In our study, we identified nucleolin as an essential component for TGF signaling initiation. In non-Smad pathway, despite that TβR-I was not affected, either nucleolin antibody or si-nucleolin wreaked havoc on activation of CrkL and Erk1/2. Nucleolin may exert the collaborative effects on recognition of TGF-β and TβR-I. Given that CrkL and Erk1/2 have been implicated in induction of cell migration and invasion (Tague et al. 2004), we further investigated the impact of nucleolin on biological effects of U87 cells and observed that nucleolin knockdown interfered with wound closure and colony formation, indicating cell proliferation, migration, and invasiveness, was affected. Therefore, cell surface nucleolin plays an active role in TGF-β signaling.
On the other hand, in the Smad pathway, Smad2 also showed no sign of activation due to antibody blocking and si-nucleolin. The Smad proteins, such as Smad2 and Smad3, are directly phosphorylated on two serine residues at their extreme C-terminal motif by TβR-I, and then form complexes with the Smad4 (Matsuura et al. 2004). The activated Smad complexes translocate into the nucleus to regulate transcription of target genes, such as p15 and c-myc (Li et al. 2004; Hill 2009; Massague et al. 2005). Therefore, nucleolin can depend on Smad pathway to promote glioblastoma development.
It should be noted that both nucleolin and TβR-I were required for TGF signaling, so we hypothesized that nucleolin may interact with TβR-I to trigger TGF-β/TβR-I complex formation. As expected, immunoprecipitation demonstrated that nucleolin indeed interacted with TβR-I, which accounted for requirement of nucleolin for TGF-β signaling initiation. Consistent with our results, Farin et al. confirmed that nucleolin affected ErbB dimerization and activation leading to enhanced cell growth. Moreover, when the C-terminal 212 amino acids region of nucleolin was expressed with ErbB1, it can enhance anchorage independent cell growth (Farin et al. 2009). Thus, nucleolin more likely acted as a key component in more receptors signaling pathways.
Additionally, Chandra et al. (Chandra et al. 2012) determined that TβR-I translocated to the nucleus with the help of nuclear proteins and selectively induced EGFR splicing isoform, once activation by TGF-β. According to our results, nucleolin maybe mediate endocytosis and translocation of TβR-I to enhance the EGFR expression, which might be a kind of tumor-causing mechanism. Furthermore, HB-19 pseudopeptide, a nucleolin antagonist that binds GAR domain, can efficiently antagonize cell surface nucleolin, which may be recommended as regimen of glioblastoma (Krust et al. 2011; Birmpas et al. 2012). Based on the above, nucleolin should be suggested as an efficient target for clinical treatment.
To conclude, our findings confirmed that nucleolin can interact with TβR-I to regulate and promote the activation of TGF-β signaling via the non-Smad and Smad pathways. At the same time, this study also highlights the importance of nucleolin as a therapeutic target. It is believed that more significant roles of nucleolin can be found and determined.
References
Alete DE, Weeks ME, Hovanession AG, Hawadle M, Stoker AW (2006) Cell surface nucleolin on developing muscle is a potential ligand for the axonal receptor protein tyrosine phosphatase-sigma. FEBS J 273:4668–4681
Birmpas C, Briand JP, Courty J, Katsoris P (2012) The pseudopeptide HB-19 binds to cell surface nucleolin and inhibits angiogenesis. Vasc Cell 4:21
Chandra M, Zang S, Li H, Zimmerman LJ, Champer J, Tsuyada A, Chow A, Zhou W, Yu Y, Gao H, Ren X, Lin RJ, Wang SE (2012) Nuclear translocation of type I transforming growth factor β receptor confers a novel function in RNA processing. Mol Cell Biol 32:2183–2195
Davies M, Robinson M, Smith E, Huntley S, Prime S, Paterson I (2005) Induction of an epithelial to mesenchymal transition in human immortal and malignant keratinocytes by TGF-beta1 involves MAPK, Smad and AP-1 signalling pathways. J Cell Biochem 95:918–931
Drabsch Y, ten Dijke P (2012) TGF-β signalling and its role in cancer progression and metastasis. Cancer Metastasis Rev 31:553–568
Farin K, Di Segni A, Mor A, Pinkas-Kramarski R (2009) Structure-function analysis of nucleolin and ErbB receptors interactions. PLoS ONE 4:e6128
Ginisty H, Sicard H, Roger B, Bouvet P (1999) Structure and functions of nucleolin. J Cell Sci 112:761–772
Hill CS (2009) Nucleocytoplasmic shuttling of Smad proteins. Cell Res 19:36–46
Katsuno Y, Lamouille S, Derynck R (2013) TGF-β signaling and epithelial-mesenchymal transition in cancer progression. Curr Opin Oncol 25:76–84
Kjellman C, Olofsson SP, Hansson O, Von Schantz T, Lindvall M, Nilsson I, Salford LG, Sjogren HO, Widegren B (2000) Expression of TGF-beta isoforms, TGF-beta receptors, and SMAD molecules at different stages of human glioma. Int J Cancer 89:251–258
Krust B, El Khoury D, Nondier I, Soundaramourty C, Hovanessian AG (2011) Targeting surface nucleolin with multivalent HB-19 and related Nucant pseudopeptides results in distinct inhibitory mechanisms depending on the malignant tumor cell type. BMC Cancer 11:333
Li AG, Wang D, Feng XH, Wang XJ (2004) Latent TGFβ1 overexpression in keratinocytes results in a severe psoriasis-like skin disorder. EMBO J 23:1770–1781
Litchfield LM, Riggs KA, Hockenberry AM, Oliver LD, Barnhart KG, Cai J, Pierce WM Jr, Ivanova MM, Bates PJ, Appana SN, Datta S, Kulesza P, McBryan J, Young LS, Klinge CM (2012) Identification and characterization of nucleolin as a COUP-TFII coactivator of retinoic acid receptor β transcription in breast cancer cells. PLoS ONE 7:e38278
Lv S, Qin J, Yi R, Coreman M, Shi R, Kang H, Yao C (2013) CrkL efficiently mediates cell proliferation, migration, and invasion induced by TGF-β pathway in glioblastoma. J Mol Neurosci 51:1046–1051
Massague J, Seoane J, Wotton D (2005) Smad transcription factors. Genes Dev 19:2783–2810
Matsuura I, Denissova NG, Wang G, He D, Long J, Liu F (2004) Cyclin-dependent kinases regulate the antiproliferative function of Smads. Nature 430:226–231
Pickup M, Novitskiy S, Moses HL (2013) The roles of TGF-β in the tumour microenvironment. Nat Rev Cancer 13:788–799
Reyes-Reyes EM, Akiyama SK (2008) Cell-surface nucleolin is a signal transducing P-selectin binding protein for human colon carcinoma cells. Exp Cell Res 1314:2212–2223
Shi Y, Massague J (2003) Mechanisms of TGF-beta signaling from cell membrane to the nucleus. Cell 113:685–700
Song N, Ding Y, Zhuo W, He T, Fu Z, Chen Y, Song X, Fu Y, Luo Y (2012) The nuclear translocation of endostatin is mediated by its receptor nucleolin in endothelial cells. Angiogenesis 15:697–711
Sun J, Liu SZ, Lin Y, Cao XP, Liu JM (2014) TGF-β promotes glioma cell growth via activating Nodal expression through Smad and ERK1/2 pathways. Biochem Biophys Res Commun 443:1066–1072
Tague SE, Muralidharan V, Souza-Schorey CD (2004) ADP-ribosylation factor 6 regulates tumor cell invasion through the activation of the MEK/ERK signaling pathway. Proc Natl Acad Sci U S A 101:9671–9676
Turck N, Lefebvre O, Gross I, Gendry P, Kedinger M, Simon-Assmann P, Launay JF (2006) Effect of laminin-1 on intestinal cell differentiation involves inhibition of nuclear nucleolin. J Cell Physiol 206:545–555
Vehlow A, Cordes N (2013) Invasion as target for therapy of glioblastoma multiforme. Biochim Biophys Acta 1836:236–244
Weiss A, Attisano L (2013) The TGFbeta superfamily signaling pathway. Wiley Interdiscip Rev Dev Biol 2:47–63
Wen PY, Kesari S (2008) Malignant gliomas in adults. N Engl J Med 359:492–507
Acknowledgments
This study was supported by National Key Basic Research Program of China (No. 2013CB932502), and National Natural Science Foundation of China (No. 81171295). We greatly thank Shigang Zhao in Sandy lab for valuable suggestions and writing.
Conflict of Interest
The authors state that there are no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
Shunzeng Lv and Jie Zhang contributed equally to this work.
An erratum to this article is available at http://dx.doi.org/10.1007/s12031-017-0935-8.
This article has been retracted at the request of Dr Chengjun Yao, Dr. Dongxiao Zhuang, The Editor in Chief and the Publisher per the Committee on Publication Ethics guidelines for the following reasons:
– There is strong reason to believe that the peer review process was compromised
– The article shows evidence of irregularities in authorship during the submission process
– Dr. Chengjun Yao has confirmed that he was not involved in the submission process and does not support its publication
– Dr. Dongxiao Zhuang has confirmed that he was not involved in the research nor in the writing of this article
– The National Natural Science Foundation of China mentioned in this paper was not involved in the research reported in this article
About this article
Cite this article
Lv, S., Zhang, J., Han, M. et al. RETRACTED ARTICLE: Nucleolin Promotes TGF-β Signaling Initiation via TGF-β Receptor I in Glioblastoma. J Mol Neurosci 55, 1–6 (2015). https://doi.org/10.1007/s12031-014-0292-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12031-014-0292-9