Abstract
Obstructive sleep apnea syndrome (OSAS) is considered a sleep-related respiratory disorder, characterized by repetitive episodes of complete (apnea) or partial (hypopnea) obstruction of airflow in the upper airway (UA) during sleep. The pathophysiology of upper airway obstruction in OSAS is multifactorial, leading to a chronic recurrent state of intermittent hypoxemia and reoxygenation during sleep, maintaining a state of oxidative stress, which seems to be the key to the pathophysiological manifestations of OSAS, and is associated with the development of a number of high morbidity–mortality systematic complications, such as obesity, type 2 diabetes, metabolic syndrome, and cardiovascular and neuropsychological diseases. This study is an open, cross-sectional, and comparative clinical trial, whose general objective was to assess the correlation between OSAS severity, oxidative stress markers, and the presence of affective symptoms (depressive and anxious) in OSAS patients. We studied 38 adult males, who had been diagnosed with OSAS by overnight polysomnography, between 18 and 60 years of age, divided into three groups: group 1—10 individuals with mild OSAS (AHI between 5 and 14.9/h), group 2—13 individuals with moderate OSAS (AHI between 15 and 30/h), and group 3—15 individuals with severe OSAS (AHI >30/h). All individuals were evaluated for level of subjective sleepiness using the Epworth Sleepiness Scale, for depressive and anxiety symptoms by the Hamilton Depression (HAM-D) and Anxiety (HAM-A) Scales, and for parameters of the oxidative stress state, measuring superoxide radical and serum nitrates and nitrites levels. There was a progressive and significant increase in the state of oxidative stress (p < 0.05), in the total score of depressive symptoms (p = 0.001) and in the overall score of anxiety symptoms (p = 0.004) directly proportional to the severity of apnea when comparing the mild group to the severe group. Positive correlations were identified between superoxide production and the apnea–hypopnea index (AHI) (r = 0.48), Epworth sleepiness score (r = 0.36), and Hamilton depression score (HAM-D) (r = 0.40); between serum nitrates and nitrites levels and SO2 min (r = 0.44); and between the AHI and the HAM-D (r = 0.51) score and HAM-A (r = 0.40) score. Negative correlations were observed between the AHI and serum nitrates and nitrites levels (r = −0.42), between superoxide production and SO2 min (r = −0.31), between serum nitrates and nitrites levels and HAM-D (r = −0.50) and HAM-A (−0.42) scores, and between SO2 min and HAM-D (r = −0.48) and HAM-A (r = −0.40) scores. According to the results of this study, we can conclude that (1) individuals with OSAS show an increase in the production of superoxide radical and a decrease in serum nitrates and nitrites levels, which are objective signs of a state of oxidative stress. (2) The more severe the OSAS, the more fragmented the sleep and the greater the nocturnal hypoxemia, the more severe is the oxidative stress state and the greater is the incidence of daytime symptoms, especially sleepiness and depressive and anxiety symptoms. Future studies might explore the investigation of oxidative stress parameters as an alternative approach to anticipate symptoms, measure prognosis, and monitor OSAS progression or treatment response.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea syndrome (OSAS) is considered a sleep-related breathing disorder, according to the latest International Classification of Sleep Disorders 2005. This syndrome is characterized by repetitive episodes of complete (apnea) or partial (hypopnea) upper airway obstruction during sleep, partially or totally impairing the passage of nasal airflow and oral, and lasted for 10 s or more, in the presence of respiratory effort (ASDA 1992; AASM 1999; CIDS 2005).
The severity of OSAS is determined by the total number of apnea or hypopnea per hour of sleep. It is considered abnormal apnea/hypopnea index (AHI) greater than or equal to five respiratory events per hour of sleep at level of oxygen desaturation measured by nocturnal polysomnography, and the degree of daytime sleepiness associated (ASDA 1992; AASM 1999; CIDS 2005).
In adults, the prevalence is around 2 % of women and 4 % of men, while the overall prevalence ranges from 0.3 % to 5 % (Lindberg and Gislason 2000; Young et al. 2002; Stradling and Davies 2004).
Multiple mechanisms appear to be involved in the pathophysiology that correlates OSAS (Lindberg and Gislason 2000; Fogel et al. 2004): obesity and metabolic syndrome, including structural and mechanical changes such as narrowing of the level of the upper airway by fat deposition in soft tissues; systemic inflammatory and metabolic disorders, such as resistance to insulin and development of type 2 diabetes; increased serum triglycerides and cholesterol; leptin resistance and hyperleptinemia; and increased ghrelin and cytokines (interleukins and tumor necrosis factor—TNF), among others, associated with visceral fat metabolically active, causing depression of the mechanisms of ventilatory control during sleep (Fogel et al. 2004; Shimura et al. 2005; Vgontzas et al. 2005; Trakada et al. 2007).
As daytime symptoms associated with OSAS, we might find variable degrees of drowsiness, fatigue, and daytime sleepiness. These and other daytime symptoms tend to express themselves as intellectuals and mood disorders, and may bring a negative impact on quality of life of patients with OSAS, impairing its ability to maintain employment, with low-income household chores or work requiring memory, trial, concentration, attention and skill, and personality changes, aggression, irritability, anxiety, and depression (Pape 1995; Redline and Tishler 2000; Sforza et al. 2002; Al-Barak et al. 2003; Stradling and Davies 2004; Ryan and Bradley 2005; Shimura et al. 2005; Vgontzas et al. 2005; Mccall et al. 2006; Peterson and Benca 2006; Marin and Carrizo 2007).
Obstructive Sleep Apnea and Oxidative Stress
The condition of chronic intermittent hypoxia (CIH) and reoxygenation in OSAS promotes the status of oxidative stress by generation of oxygen free radicals, particularly superoxide (O −2 ), and highly reactive nitrogen with potential toxic effects on the vessel walls and body's cells. These reactive oxygen species (ROS) react with nucleic acids, lipids, and proteins, and reduce levels of anti-oxidants and nitric oxide (NO), a powerful vasodilator, causing endothelial damage and vasoconstriction, increasing the risk of developing atherosclerosis, and heart and vascular diseases (Pape 1995). The state of oxidative stress can be evaluated scientifically in several ways, including the analysis of superoxide production (RAS) and nitric oxide (NO), this through the dosage of serum nitrite and nitrate. Besides its important role as systemic vasodilator, NO is closely related to various systems of neurotransmission and neuromodulation involved in regulating many physiological functions such as the inflammatory response, circadian rhythms, sleep–wake cycle, memory processing, synaptic plasticity, and gastrointestinal motility. As mentioned before, the situation of CIH generating the oxidative stress status will lead to increased ROS and therefore the superoxide (RAS), and the reduction of nitric oxide (NO), which can be considered markers of clinical status (Pape 1995; McCord 2000; Shamsuzzaman et al. 2003; Ozkan et al. 2008).
Obstructive Sleep Apnea and Neuropsychological Disorders
Cognitive deterioration and depressive or anxious symptoms may be early symptoms and are often not valued in the statement of investigation for OSAS. In humans with OSAS, CIH and fragmentation of sleep architecture associated with impairments in several domains of neuropsychological functions were more commonly observed abnormalities in executive functions and attention, as well as depression, anxiety, irritability, aggressiveness, hyperactivity, and changes in personality (Bardwell et al. 2007; Sforza et al. 2002; (Ohayon 2003); Mccall et al. 2006; Peterson and Benca 2006; Shen et al. 2006).
It seems difficult to assess how depression is a consequence of primary OSAS or secondary symptoms of OSAS themselves or due to comorbidities associated with OSAS such as obesity, diabetes, and hypertension (Bardwell et al. 2001; Sforza et al. 2002; Ohayon 2003; Mccall et al. 2006; Peterson and Benca 2006; Shen et al. 2006).
The study of symptoms associated with mood disorder may indicate the clinical suspicion for a specific disease, in the case of OSAS, depressive symptoms that are associated with difficulties in sleep, fatigue, and daytime sleepiness, suggesting the diagnosis. One must be careful in the evaluation method to avoid confusing the effects of poor sleep quality and daytime sleepiness with changes in mood. The correlation between depression and OSAS has been described in previous studies that showed improvement in depressive symptoms with treatment of OSAS using continuous positive airway pressure (CPAP) (Bardwell et al. 2001; Deldin et al. 2006; Shen et al. 2006).
We believe that effective diagnosis and treatment of OSAS aims to improve objective and subjective quality of life, and accident prevention and the emergence of serious comorbidities. Thus, the sleep study and the investigation of symptoms often hidden or neglected, as usually the mood disorders, can be of great benefit to the affected individuals.
Our present goal was to investigate the correlation between the severity of OSAS, oxidative stress, and depressive symptoms and anxiety in patients with OSAS.
Methods
Sample and Inclusion Criteria
Thirty-eight male adults were enrolled with age range between 18 and 60 years old. They were divided into three groups according to the severity of OSAS:
-
(a)
Group 1: 10 subjects with mild OSAS (AHI between 5 and 14.9/h)
-
(b)
Group 2: 13 subjects with moderate OSAS (AHI between 15 and 30/h)
-
(c)
Group 3: 15 individuals with severe OSAS (AHI >30/h)
Exclusion Criteria
To prevent other medical conditions that increase oxidative stress, inflammatory status, and risk of mood disorders, causing interference and potential error, we excluded from the study the following subjects:
-
Diagnosed with type I or II diabetes, cardiovascular disease, inflammatory disease or acute or chronic infections (in the last 4 weeks before performing the evaluations in this study), central sleep apnea or Cheyne–Stokes respiration, chronic obstructive pulmonary disease or asthma, smoking, thyroid disease, chronic kidney disease, autoimmune diseases, neurological or genetic;
-
Use of corticosteroids or anti-inflammatory drugs, antibiotics, and β-agonists or blockers, or having been treated for OSAS.
-
Females, to avoid subjects with higher chance to present mood swings due to cyclic hormonal changes.
Anthropometric Measurements
Weight (kg) and height (m) were measured in all volunteers in order to also calculate body mass index (BMI).
Laboratory Study of Sleep: Polysomnography
The measured parameters were as follows: EEG with monopolar central and occipital derivations (C3, C4, O1, O2), electro-oculogram of left and right eye, electrocardiogram (ECG), electromyogram of pretibial and submandibular muscles, thoracic and abdominal respiratory effort (plethysmography), peripheral oxygen saturation (SpO2) by pulse oximetry, digital transcutaneous airflow, and nasal/oral thermistor recorded by, besides the recording of snoring (microphone).
The analysis of sleep stages was performed manually at intervals of 30 s according to the criteria of Rechtschaffen and Kales (1968). Apneas and hypopneas were considered with a minimum duration of 10 s. Apnea/hypopnea index (AHI) is obtained by dividing the total number of respiratory events by the total sleep time (events per hour), being used as diagnostic criteria of OSAS (AHI >5), and to stratify their severity: AHI >5/h considered as diagnostic of OSAS. As to the severity: mild if AHI >5–15/h, moderate if between AHI >15 and 30/h, and severe OSAS or severe degree if AHI >30/h. Oxygen desaturation during sleep was defined as a drop of basal saturation >3 %. The arousals were defined as abrupt change in EEG frequency greater than 3 s and the index of arousals considered the number of arousals per hour of sleep.
Our volunteers completed a questionnaire, which we call "sleep questionnaire”, to investigate signs and symptoms related to sleep, including filing the Epworth Sleepiness Scale (ESS)—ANNEX 1 in order to determine the degree of subjective sleepiness. The scale scores range from 0 to 3 points for each situation (0 = never, 1 = slight chance, 2 = moderate chance, 3 = high chance). The total score ranges from 0 to 24, scores 8–11 = mild sleepiness, 12–15 = moderate sleepiness, and from 16 = severe drowsiness.
Parameters to Evaluate the Oxidative Stress
Peripheral venous blood samples were obtained by venipuncture in fasting in the morning hours. As the half life of nitrites and nitrates (NO derivatives) is 4–7 h, the measurement of those elements upon awakening reflects NO production during the night, during which the apneic patients have recurrent episodes of hypoxia/reoxygenation. The assessment of oxidative stress was performed by measuring superoxide radical (RAS) with spectrophotometric methods, and estimating the production of serum nitric oxide (NO) measured indirectly by determination of serum nitrite and nitrate, using a quantitative colorimetric assay based on the Griess reaction (Ding et al. 1988).
In the present study, triplicate 50-μl aliquots of cell culture supernatants were incubated with 50 μl of freshly prepared Griess reagent (1 % sulfanilamide, 0.1 % naphthylethylene diamide dihydrochloride, and 5 % o-phosphoric acid) at room temperature for 10 min. The absorbance of the azochromophore was measured at 550 nm (Bel Photonics 1105; Tecnal, Piracicaba/SP, Brazil). The NO concentration was determined using sodium nitrite as a standard (0–100 μM). All samples were assayed against a blank comprising complete RPMI-1640 incubated for 24 h in the same plates as the samples, but in the absence of cells. All reagents were purchased from Sigma-Aldrich. The results were expressed in micromoles of NO per 5 × 105 cells.
Assessment of Anxious and Depressive Symptoms
Depressive symptoms and/or anxiety were assessed using the Hamilton Rating Scale for Depression (HAM-D) and Anxiety (HAM-A)—APPENDIX 3 and 4. The assessment was based on interviews and information from other sources such as family members. Hamilton scale for anxiety is known as HAM-A (Hamilton Anxiety Scale) and HARS (Hamilton Anxiety Rating Scale).
The HAM-A is widely used and studies have shown its reliability by the capacity of assessment of anxiety symptoms rather consistently, and similarly that for the HAM-D.
Statistical Analysis
For verification of inter- and intra-group quantitative variables, we used the parametric ANOVA test for variance analysis and Tukey's post-test analysis of the differences between the categories, with confidence interval of 95 %. To evaluate the non-parametric data qualitative non-normal distribution, the Kruskal–Wallis (KW) test was first used followed by multiple comparison procedure by Dunn's paired test (bilateral). The results were presented as mean, standard deviation, and maximum and minimum values. The p value <0.05 was considered statistically significant and the correlation’s degree was measured using Pearson correlation coefficient, represented by r in values between −1 and 1.
Results
Results of General Data and Anthropometric Study of Sleep
Table 1 shows characteristics of the patients analyzed. There were no significant differences among the three groups of mild, moderate, and severe apnea, according to age and body mass index, which confirms the homogeneity of the sample. The apnea–hypopnea index was used to classify patients into three groups according to the latest CIDS-2005: mild, moderate, and severe apnea. We noticed a trend of progressive correlation in between weight, body mass index (BMI), and neck circumference when comparing the groups regarding the degree of apnea (AHI).
Variables were studied in the sleep questionnaire completed by volunteers on the night of PSG with questions relating to sleep or symptoms daytime members: the most frequently reported clinical claim for the realization examination in the three groups was snoring, occurring in 77 % to 90 % of cases. With regard to sleep architecture, these variables were increased latencies of NREM and REM for all groups, although no significant difference between groups, and sleep fragmentation in all groups, with the arousal index (ARI) showing higher mean proportional to the severity of OSAS with a statistically significant difference (p = 0.0001)—mild OSAS = 8/h, moderate = 24/h, and serious OSAS and mean IMD = 47/h.
Results of the Assessment of Depressive and Anxiety Symptoms
In a study of the percentages (Table 2), there was a progressive increase in cases with scores compatible with mild depressive syndrome (HAM-D between 7 and 17 points) for all groups of OSAS and depressive syndrome with moderate (HAM-D between 18 and 24 points) for moderate and severe OSAS groups. None of the three apneic groups had scores consistent with severe depression (HAM-D total score over 25 points).
Table 3 presents the percentages of patients with anxiety symptoms according to severity by the total score of HAM-A scale in the three apneic groups classified according to the severity of OSAS. In all apneic groups, we detected the presence of anxiety symptoms in a different percentage of patients, with progressive increase in the severity of anxiety symptoms proportional to the severity of OSAS. In the group with mild apnea, only 3 % of the total score was consistent with mild anxiety (HAM-A total score of 7–17 points). In the groups with moderate and severe apnea, scores were detected to be compatible with moderate anxiety in 15 % and 33 %, and severe anxiety in 8 % and 13 %, respectively.
Results of the Evaluation of Markers for Oxidative Stress
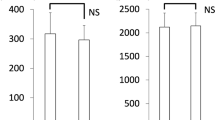
There was a progressive increase of the average levels of RAS directly proportional to the severity of OSAS, while the mean levels of NO were decreasing in inverse proportion to the severity of OSAS. These findings were statistically significant (p < 0.05) and differences in values were significant between the groups of mild compared to apneic groups of moderate or severe apnea. Graphical representations of these variations in the levels of nitrites and nitrates serum (NO) and superoxide production (RAS) of the three groups with voluntary apnea are shown in figures below.
In Fig. 1, we found levels of nitrite and nitrate (NO) in three experimental groups and observed an increasingly smaller with increasing severity OSAS (p = 0.002).
In Fig. 2, we observed the production of RAS in the three experimental groups and observed a progressive increase in the levels of RAS compared groups in relation to OSAS severity (p = 0.00001), with significant difference values between groups mild and moderate or severe.
Study of Correlations
Correlations study using Pearson’s coefficient is presented in Table 4.
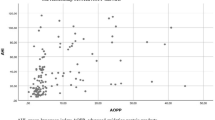
A moderate negative correlation was found, revealing that a higher severity of OSAS is associated with lower levels of nitric oxide (NO) (Fig. 3).
A moderate positive correlation was detected, revealing higher severity of OSAS associated with higher levels of superoxide radical, indicating oxidative stress (Fig. 4). A similar correlation was found between a higher severity of OSAS and higher scores of depression and anxiety (Figs. 5 and 6).
Discussion
Studying the variables of the PSG, in all groups (mild, moderate, and severe) there was compromise of parameters that highlight the quality of sleep. Sleep is usually fragmented and inefficient, with reduction in total sleep time, besides the increase in NREM and REM latency, and increase of the average of arousals. Moreover, sleep architecture was impaired in all groups, with an imbalance in the percentage distribution of sleep stages, with increasing time in shallow sleep and reduced delta time in deep sleep and REM sleep.
Also, the study of nocturnal oximetry in these patients showed average levels of O2 saturation inversely proportional to the degree of apnea, which was statistically significant.
Some of these changes described in the polysomnographic OSAS, such as an increase in wakefulness time and number of awakenings, time reduction in delta sleep, and total sleep time abnormalities, are shared by individuals with depression (Deldin et al. 2006).
Our results regarding the evaluation of depressive and anxiety symptoms in apneic groups showed increasing average values of total scores for the HAM-D directly proportional to the severity of OSAS, the difference being statistically significant when comparing the groups with mild apnea and groups moderate or severe. The mean HAM-D scores for moderate and severe OSAS groups characterize mild depressive syndrome, with higher expression of the sub-items: depressed mood, psychic anxiety, and initial insomnia.
There was a growing percentage directly proportional to the severity of apnea in HAM-D scores consistent with mild depressive syndrome for the three apnea groups, and cases of HAM-D scores consistent with moderate depressive syndrome only in groups moderate and severe apnea.
As for the study of anxiety symptoms, the mean HAM-A were directly proportional to increasing severity of apnea, with significant difference between groups of mild and severe OSAS. For all three groups were the highest averages for the sub-items of psychological symptoms such as anxiety psychic insomnia, anxious mood, tension, and intellectual difficulty.
Somatic symptoms scored with lower averages than the psychological symptoms, and the most relevant symptoms were muscle pains and the SNA. But the sub-items that showed significant differences between groups just too mild and severe OSAS were psychological symptoms (anxious mood and tension) and somatic symptoms (gastrointestinal, genitourinary, and SNA). As for the HAM-D study, the percentages of HAM-A score were compatible with mild, moderate, or severe anxiety, and were increasing in direct proportion to the degree of apnea, especially when compared to mild OSAS group and moderate or severe, with no cases of anxiety scores consistent with moderate or severe to mild apnea group. We found no correlation between age and HAM-D scores and HAM-A.
We found a weak positive correlation between depressive and anxiety symptoms and BMI, between levels of RAS and anxious symptoms, as well as weak negative correlation between the levels of RAS and SpO2 min, and between the scores of Epworth Sleepiness and NO levels.
Correlations of greater significance, of moderate value, were positive for RAS levels versus AHI levels, RAS versus HAM-D score, AHI scores versus HAM-D and HAM-A, scores of Epworth versus RAS levels, and NO levels versus SpO2 min. There were negative correlations between NO levels versus AHI, SpO2 min versus HAM-A scores and HAM-D scores, and between levels of NO versus HAM-D scores and HAM-A scores.
These results suggest the correlation between the greater degree of apnea, higher blood oxygen desaturation, and the severity of oxidative stress status as well as increased daytime sleepiness and a higher presence of depressive or anxiety symptoms.
Depressive and anxiety symptoms have been described as more frequent in OSAS patients than in the general population, focusing on depression in 7 % to 56 % of apneic patients (Sforza et al. 2002; Al-Barak et al. 2003). For some authors, the depression scores were higher in more severe cases on the AHI and nocturnal hypoxemia (Bardwell et al. 2007). Other authors found no direct correlation between this severity of apnea and hypoxemia night as a potential risk factor for depression, mood disorders, or personality disorders (Bardwell et al. 2001; McMahon et al. 2003; Deldin et al. 2006; Shen et al. 2006).
Thus, it is difficult to determine how these psychopathological symptoms are due to the severity of OSAS or specific symptoms such as drowsiness and decreased alertness or daytime fatigue, lack of energy or sleepiness, the primary psychiatric disorder or due to association of various clinical conditions comorbid with OSAS, such as obesity, diabetes and hypertension, leading to situations of disability and loss of overall health and diminished quality of life, or even due to chronic use of psychotropic drugs (Sforza et al. 2002; Hagen and Black 2008).
Various efforts have been made to try to clarify the origin of fatigue and daytime sleepiness in depressed patients with sleep disorders such as OSAS, but the results are conflicting, although there is suggestion that fatigue is more related to depression than to severity of OSAS, as has been observed in the improvement in fatigue with treatment of depression regardless of the treatment of OSAS (Bardwell et al. 2001). The ideal would be to optimize the treatment of both comorbid conditions, improving the symptoms in a reciprocal manner (Brunello et al. 1999; Kawahara et al. 2005).
Assuming that the loss of life in the daytime activities is crucial to the emergence of psychopathology, some hypotheses can explain that daytime sleepiness affects the psychological profile of patients with OSAS. Daytime symptoms of OSAS such as excessive daytime sleepiness is one of the most common daytime symptoms of OSAS, and decreased alertness, fatigue, or lack of energy can be severe enough to incapacitate the individual in their executive functioning in work and social activities, and compromise their perception of functional and emotional well-being, leading to mood and personality disorders (Sforza et al. 2002; Glebocka et al. 2006).
Anyway, it is very important to investigate and treat symptoms, and some authors have suggested that fatigue, chronic inability to initiate and maintain sleep, and insomnia increase the risk of suicide (Mccall et al. 2006; Chelappa and Araujo 2007). Patients with symptoms related to mood disorders that initially presented to the sleep specialist should be evaluated for possible diagnosis of depression/anxiety, or not associated with sleep disorders, and the risk of suicide so they can be treated appropriately.
In our study, the production of NO and RAS in subjects with OSAS showed moderate correlation, negative and positive, respectively, with the AHI, strengthening the role of the events of hypoxia reoxygenation on oxidative stress, directly linking the severity of both OSAS and oxidative stress.
There is a negative correlation between AHI and NO production in individuals with OSAS, a relationship which remained even after adjustments were made in relation to BMI, which confirms that OSAS causes changes in the synthesis of nitric oxide, independent of obesity (Ip et al. 2000; Mehra and Redline 2008). The increased synthesis of RAS in OSAS correlated with the reduction in NO levels and with possible changes in the homeostasis of vasomotor tone with consequent endothelial injury (Khalid and Ashraf 1993).
Our study showed moderate correlations of direct correlation between the severity of OSAS, depression, and anxiety scores and the severity of oxidative stress, and between oxidative stress and severity of subjective sleepiness, psychological distress, and O2 desaturation. Therefore, we believe there is evidence, although our sample is small, that there is a cycle of interactions and feedback between the OSAS, the state of oxidative stress, and the onset of psychopathological symptoms of depression and anxiety in these individuals.
In our sample, the average pattern of oxidative stress in moderate OSAS is very similar to severe OSAS, and both are far different from mild OSAS. This encourages us to propose that there is a threshold in the triggering of oxidative stress metabolism and symptoms, and it seems to be the frontier between mild and moderate OSAS, with moderate and severe OSAS being part of the same process of consolidated oxidative stress.
Thus, although we respect the formal classification of OSAS based on the number of apnea/hypopnea per hour, we may also state another classification in two groups (mild and severe) of severity based on the oxidative stress profile. So, patients with AHI >15 would be considered moderate OSAS in the former classification but severe OSAS considering the oxidative profile.
However, the interaction between OSAS and mood seems to be reciprocal and complex, with probable common neurobiological mechanisms in the development of these clinical states. Studies have shown that sleep deprivation and chronic intermittent hypoxia lead to prejudice in the functions of the prefrontal cortex, in hippocampal neurogenesis, and neuronal injury, probably mediated by cellular oxidative stress and HPA axis activation, participating in the pathophysiology of memory disorders, attention, and mood in humans (Khalid and Ashraf 1993; Nester et al. 2002; Buckley and Schatzberg 2005; Peterson and Benca 2006; Mehra and Redline 2008). Similarly, functional neuroimaging studies by MRI or PET (positron emission tomography) scan in patients with OSA and patients with major depression showed abnormalities in the activation of the prefrontal cortex (Jones and Harrison 2001; Germain et al. 2004; Verstraeten and Cluydts 2004).
Neuroendocrine dysregulation, in particular the hyperactivation of the HPA axis associated with elevations of corticotropin-releasing hormone (CRH) and cortisol, has been recognized as having an important role in the genesis of mood disorders and is also closely involved in the pathophysiology of chronic oxidative stress resulting in OSAS (Jones and Harrison 2001; Tafet et al. 2001; Yee et al. 2004; Peterson and Benca 2006; Tsao et al. 2006; Trakada et al. 2007). Also, the chronic inflammatory condition occurring in OSAS, with the elevation of cytokines such as interleukin 6 (IL-6) and tumor necrosis factor alpha (TNF-α), has been associated with excessive daytime sleepiness and fatigue levels plasma and correlated positively with the degree of apnea and nocturnal hypoxemia independent of the occurrence of obesity (O’Brien et al. 2004; Vgontzas et al. 2005; Kasasbeh et al. 2006; Trakada et al. 2007; Mehra and Redline 2008).
Studies correlate inflammatory cytokines and mood disorders, especially major depression, showing increased serum levels of TNF-α and / or interleukins IL-1β, IL-6, IL-8 in depressed patients. Increased serum IL-6 leads to reduction of plasma tryptophan, and promotes the activation of the HPA, with increased cortisol, reflecting both the reduction of central neurotransmission of serotonin, a neurotransmitter important in regulating sleep and mood disorders predisposing to these spheres (Maes 1993; Song et al. 1998; Wichers and Maes 2002; O’Brien et al. 2004; Krystal 2006; Tsao et al. 2006).
Thus, activation of the HPA system, with elevated serum cortisol and corticotropin, and the inflammatory system, with elevated serum IL-6 and TNF-alpha, among other substances, in the presence of a state of oxidative stress, chronic inflammation, are closely interconnected and possibly involved in the neurobiological link between OSAS and symptoms of depression and anxiety.
There may be individual variability in response to fragmentation/chronic sleep deprivation determining the predominant phenotype of excessive sleepiness and/or daytime fatigue, depression, carelessness, and more or less predisposed to mood disorders, but OSAS may contribute to exacerbate the condition predisposed to a particular individual (Shen et al. 2006). Psychiatric symptoms of depression and anxiety in patients with OSAS lead to lower tolerance to CPAP and were predictors of poor adherence to this treatment, impacting negatively on treatment outcome (McMahon et al. 2003; Kawahara et al. 2005). Moreover, treatment of OSAS may improve or prevent symptoms of depression and anxiety (Derderian et al. 1998; Engleman et al. 2005; Deldin et al. 2006).
Thus, it seems elementary to diagnose and treat depressive and anxiety states in patients with OSAS, contributing positively in the therapeutic results of both clinical conditions.
Several great studies have already displayed evidence of increased oxidative stress in OSAS in plasma (Barceló et al. 2000; Christou et al. 2003; Lavie et al. 2004), urine (Yamauchi et al. 2005), and exhaled air (Carpagnano et al. 2003; Petrosyan et al. 2008). Moreover, treatment with nCPAP has already been shown to attenuate oxidative stress (Barceló et al. 2000; Carpagnano et al. 2003; Lavie et al. 2004; Itzhaki et al. 2007).
Additional reports referred to the association of depression and anxiety to OSAS (Guglielmi et al. 2011), and the idea that nCPAP might improve mood alterations is already known (Saunamäki and Jehkonen 2007). However, we think that the main contribution of our work is to link and combine the three parts (OSAS, oxidative stress, and neuropsychiatric symptoms, such as depression and anxiety). There are not many studies with a similar approach as far as we know.
We need to be cautious about our findings, and no causality link can be determined now. Additional studies with nCPAP intervention must be performed to address this question. We also cannot exclude the possibility of limitations in our study due to methodological bias. The use of questionnaires and scales can introduce bias in the estimation of subjective symptoms, but objective data from polysomnography and examination of the laboratory study served to support and consider our argument.
We must state that there are many parameters in daily life which can interfere with the account for depression and anxiety. Just to enumerate, we can say that food quality, sports practicing, family status, occupational status, and health status, of course, may directly or indirectly change the evaluation of such neuropsychiatric symptoms. In this specific study, we could have added to the article profile the application of the Pittsburgh Sleep Quality Index (Buysse et al. 1989) or other scores in order to also consider the quality of sleep.
Nevertheless, the Epworth score is also a reliable and worldwide applied tool with success in the characterization of patients with sleep disorders. Besides, although the specific conclusion of Epworth score translates the daily sleepiness, it is a confident proof of sleep quality.
Another point raised is that the duration of OSAS could account for some of the correlations evaluated in this work (Petrosyan et al. 2008). The definition of OSAS depends on an apneic episode of at least 10 s. Surely, the oxidative stress markers and organic consequences are dependent on time of exposure to hypoxic states. The whole time can be achieved by prolonged episodes of apnea or by the sum of shorter periods of apnea with a higher frequency. The usual classification uses as standard parameter the frequency of apneic/hypopneic periods in an hour. However, less episodes with larger time of apnea would also count. That is a valid concept which we did not apply in our work due to limits of valid protocols. Doubtlessly, it is worthy to stratify these patients not only by frequency but by duration of each apnea, and it will be the target for future discussions.
Conclusion
OSAS patients complain of daytime symptoms, with predominance of sleepiness, and nocturnal symptoms, with prevalence of snoring, nightmares, and insomnia. They showed increased superoxide production and decreased levels of serum nitrite and nitrate, objective signs of a state of oxidative stress. The greater the severity of OSAS, the more serious was the state of oxidative stress and the higher the incidence of daytime symptoms, particularly sleepiness, and depressive and anxiety symptoms.
With increasing global prevalence of obesity and other risk factors for OSAS in the general population, investigating and treating OSAS and possible mutual interaction of comorbidities such as depression and anxiety disorders is an attitude of great clinical value. This allows preventing the perpetuation of the vicious cycle of feedback and choice of these clinical situations aware of therapeutic measures that can benefit and not harm the development of both pictures.
Future studies might explore the investigation of oxidative stress parameters as an alternative approach to anticipate symptoms, measure prognosis, and monitor OSAS progression or treatment response.
References
Al-Barak M, Shepertyeky MR, Kryger MH (2003) Morbidity and mortality in obstructive sleep apnea syndrome: effect of treatment on neuropsychiatric morbidity and quality of life. Sleep Biol Rhythms 1:65–74
American Academy of Sleep Medicine Task Force (1999) Sleep related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Sleep 22:667–689
American Sleep Disorders Association—Atlas Task Force (1992) EEG arousals: scoring rules and examples. Sleep 15:174–184
Barceló A, Miralles C, Barbé F, Vila M, Pons S, Agustí AG (2000) Abnormal lipid peroxidation in patients with sleep apnoea. Eur Respir J 16(4):644–647
Bardwell WA, Ancoli-Israel S, Berry CC, Dimsdale JE (2001) Neuropsychological effects for one-week continuous positive airway pressure treatment in patients with obstructive sleep apnea: a placebo-controlled study. Psychol Med 63:579–584
Bardwell WA, Ancoli-israel S, Dimsdale JE (2007) Comparison of the effects of depressive symptoms and apnea severity on fatigue in patients with obstructive sleep apnea: a replication study. J Affect Disord 97:181–186
Brunello N, Akiskal H, Bover P et al (1999) Dysthymia: clinical picture, extent of overlap with chronic fatigue syndrome, neuropharmacological considerations, and new therapeutic vistas. J Affect Disord 52:275–290
Buckley TM, Schatzberg AF (2005) On the interactions of the hypothalamic–pituitary–adrenal (HPA) axis and sleep: normal HPA axis activity and circadian rhythm, exemplary sleep disorders. J Clin Endocrinol Metab 90:3106–3114
Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28(2):193–213
Carpagnano GE, Kharitonov SA, Resta O, Foschino-Barbaro MP, Gramiccioni E, Barnes PJ (2003) 8-Isoprostane, a marker of oxidative stress, is increased in exhaled breath condensate of patients with obstructive sleep apnea after night and is reduced by continuous positive airway pressure therapy. Chest 124(4):1386–1392
Chelappa SL, Araujo JF (2007) Sleep disorders and suicidal ideation in patients with depressive disorder. Psychiatry Res 153(2):131–136
Christou K, Moulas AN, Pastaka C, Gourgoulianis KI (2003) Antioxidant capacity in obstructive sleep apnea patients. Sleep Med 4(3):225–228
CIDS—The International Classification of Sleep Disorders (2005) Diagnostic and coding manual, 2nd edition. American Academy of Sleep Medicine, Darien
Deldin PJ, Phillips LK, Thomas RJ (2006) A preliminary study of sleep-disordered breathing in major depressive disorder. Sleep Med 7:131–139
Derderian SS, Brindenbaugh RH, Rajagopal KR (1998) Neuropsychologic symptoms in obstructive sleep apnea improve after treatment with nasal continuous positive airway pressure. Chest 94:1023–1027
Ding AH, Nathan CF, Stuehr DJ (1988) Release of reactive nitrogen intermediates and reactive oxygen intermediates from mouse peritoneal macrophages. Comparison of activating cytokines and evidence for independent production. J Immunol 141:2407–2412
Engleman HM, Cheshire KE, Deary IJ, Douglas NJ (2005) Daytime sleepiness, cognitive performance and mood after continuous positive airway pressure for the sleep apnea/hypopnea syndrome. Thorax 48:187–197
Fogel RB, Malhotra A, White DP (2004) Sleep 2: pathophysiology of obstructive sleep apnea/hypopnea syndrome. Thorax 59:159–163
Germain A, Nofzinger EA, Kupfer DJ, Buysse DJ (2004) Neurobiology of non-REM sleep in depression: further evidence for hypofrontality and thalamic dysregulation. Am J Psychiatry 161:1856–1863
Glebocka A, Kossowska A, Bednarek M (2006) Obstructive sleep apnea and the quality of life. J Physiol Pharmacol 57(Suppl 4):111–117
Guglielmi O, Sánchez AI, Jurado-Gámez B, Buela-Casal G, Bardwell WA (2011) Obesity and sleep quality: the predictors of depression and anxiety in obstructive sleep apnea syndrome patients. Rev Neurol 52(9):515–521
Hagen CC, Black JE (2008) Sleepiness and fatigue in patients with psychiatric disorders. Sleep Med Clin 3:205–215
Ip MS, Lam B, Chan LY et al (2000) Circulating nitric oxide is suppressed in obstructive sleep apnea and is reversed by nasal continuous positive airway pressure. Am J Respir Crit Care Med 162:2166–2171
Itzhaki S, Dorchin H, Clark G, Lavie L, Lavie P, Pillar G (2007) The effects of 1-year treatment with a Herbst mandibular advancement splint on obstructive sleep apnea, oxidative stress, and endothelial function. Chest 131(3):740–749
Jones K, Harrison Y (2001) Frontal lobe function, sleep loss and fragmented sleep. Sleep Med Rev 5:463–475
Kasasbeh E, Chi DS, Krishnaswamy G (2006) Inflammatory aspects of sleep apnea and their cardiovascular consequences. South Med J 99:58–67
Kawahara S, Akashiba T, Akahoshi T, Nasal HT (2005) CPAP improves the quality of life and lessens the depressive symptoms in patients with obstructive sleep apnea syndrome. Int Med 44:422–427
Khalid MA, Ashraf M (1993) Direct detection of endogenous hydroxyl radical production in cultured adult cardiomyocyte during anoxia and reoxygenation: is the hydroxyl radical really the most damaging radical species? Circ Res 72:725–736
Krystal RAD (2006) Sleep and psychiatric disorders: future directions. Psychiatr Clin N Am 29:1115–1130
Lavie L, Vishnevsky A, Lavie P (2004) Evidence for lipid peroxidation in obstructive sleep apnea. Sleep 27(1):123–128
Lindberg E, Gislason T (2000) Clinical review article: epidemiology of sleep-related obstructive breathing. Sleep Med Rev 4(5):411–433
Maes M (1993) A review on the acute phase response in major depression. Rev Neurosci 4:407–416
Marin JM, Carrizo SJ (2007) Mortality in obstructive sleep apnea. Sleep Med Clin 2:593–601
Mccall WV, Harding D, O’Donovan C (2006) Correlates of depressive symptoms in patients with obstructive sleep apnea. J Clin Sleep Med 2:424–426
McCord JM (2000) The evolution of free radicals and oxidative stress. Am J Med 108:652–659
McMahon JP, Foresman BH, Chisholm RC (2003) The influence of CPAP on the neurobehavioral performance of patients with obstructive sleep apnea hypopnea syndrome: a systematic review. WMJ 102:36–43
Mehra R, Redline S (2008) Sleep apnea: a proinflammatory disorder that coaggregates with obesity. J Allergy Clin Immunol 121(5):1096–1102
Nester EJ, Barrot M, DiLeone RJ, Eisch AJ, Gold SJ, Monteggia LM (2002) Neurobiology of depression. Neuron 34:13–25
O’Brien SM, Scott LV, Dinan TG (2004) Cytokines: abnormalities in major depression and implications for pharmacological treatment. Hum Psychopharmacol 19:397–403
Ohayon MM (2003) The effects of breathing-related sleep disorders on mood disturbances in the general population. J Clin Psychiatry 64:1195–1200
Ozkan Y, Firat H, Simsek B, Torun M, Yardim-Akaydin S (2008) Circulating nitric oxide (NO), asymmetric dimethylarginine (ADMA), homocysteine, and oxidative status in obstructive sleep apnea–hypopnea syndrome (OSAHS). Sleep Breath 12:149–154
Pape HC (1995) Nitric oxide: an adequate modulatory link between biological oscillators and control systems in the mammalian brain. Neurosciences 7:329–340
Peterson MJ, Benca RM (2006) Sleep in mood disorders. Psychiatr Clin N Am 29:1009–1032
Petrosyan M, Perraki E, Simoes D et al (2008) Exhaled breath markers in patients with obstructive sleep apnoea. Sleep Breath 12(3):207–215, Epub 2007 Dec 11
Rechtschaffen A, Kales A (eds) (1968) A manual of standardized terminology, techniques and scoring system of sleep stages in human subjects. Brain Information Service/Brain Research Institute, University of California, Los Angeles
Ryan CM, Bradley TD (2005) Pathogenesis of obstructive sleep apnea. J Appl Physiol 99(6):2440–2450
Redline S, Tishler P (2000) The genetics of sleep apnea. Review article. Sleep Med Rev 4(6):583–602
Saunamäki T, Jehkonen M (2007) Depression and anxiety in obstructive sleep apnea syndrome: a review. Acta Neurol Scand 116(5):277–288, Epub 2007 Sep 14
Sforza E, de Saint Hilaire Z, Pelissolo A, Rochat T, Ibanez V (2002) Personality, anxiety and mood traits in patients with sleep related breathing disorders: effect of reduced daytime alertness. Sleep Med 3:139–145
Shamsuzzaman ASM, Gersh BJ, Somers VK (2003) Obstructive sleep apnea. Implications for cardiac and vascular disease. JAMA 290:1906–1914
Shen J, Barbera J, Shapiro CM (2006) Distinguishing sleepiness and fatigue: focus on definition and measurement. Sleep Med Rev 10:63–76
Shimura R, Tatsumi K, Nakamura A et al (2005) Fat accumulation, leptin, and hypercapnia in obstructive sleep apnea–hypopnea syndrome. Chest 127:543–549
Song C, Lin A, Bonaccorso S et al (1998) The inflammatory response system and the availability of plasma tryptophan in patients with primary sleep disorders and major depression. J Affect Disord 49:211–219
Stradling JR, Davies RJO (2004) Sleep 1: obstructive sleep apnea/hypopnea syndrome: definitions, epidemiology, and natural history. Thorax 59:73–78
Tafet GE, Toister-Achituv M, Shinitzky M (2001) Enhancement of serotonin uptake by cortisol: a possible link between stress and depression. Cogn Affect Behav Neurosci 1:96–104
Trakada G, Chrousos GP, Pejovic S, Vgontzas ANV (2007) Sleep apnea and its association with the stress system, inflammation, inflammation, insulin resistance and visceral obesity. Sleep Med Clin 2:251–261
Tsao CW, Lin YS, Chen CC, Bai CH, Wu SR (2006) Cytokines and serotonin transporter in patients with major depression. Prog Neuropsychopharmacol Biol Psychiatry 30:899–905
Verstraeten E, Cluydts RM (2004) Executive control of attention in sleep apnea patients: theoretical concepts and methodological considerations. Sleep Med Rev 8:257–267
Vgontzas AN, Bixler EO, Chrousos GP (2005) Sleep apnea is a manifestation of the metabolic syndrome. Theoretical review. Sleep Med Rev 9:211–224
Wichers M, Maes M (2002) The psychoneuroimmuno-pathophysiology of cytokine-induced depression in humans. Int J Neuropsychopharmacol 5:375–388
Yamauchi M, Nakano H, Maekawa J et al (2005) Oxidative stress in obstructive sleep apnea. Chest 127(5):1674–1679
Yee B, Liu P, Phillips C, Grunstein R (2004) Neuroendocrine changes in sleep apnea. Curr Opin Pulm Med 10:475–481
Young T, Peppard P, Gottlieb D (2002) Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med 165:1217–1239
Conflicts of Interest
The authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Franco, C.M.R., Lima, A.M.J., Ataíde, L. et al. Obstructive Sleep Apnea Severity Correlates with Cellular and Plasma Oxidative Stress Parameters and Affective Symptoms. J Mol Neurosci 47, 300–310 (2012). https://doi.org/10.1007/s12031-012-9738-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12031-012-9738-0