Abstract
Transient receptor potential (TRP) ion channels, such as TRP vanilloid 1 and ankyrin repeat domain 1 (TRPV1 and TRPA1), are expressed on primary sensory neurons. Lutein, a natural tetraterpene carotenoid, can be incorporated into membranes and might modulate TRP channels. Therefore, the effects of the water-soluble randomly methylated-β-cyclodextrin (RAMEB) complex of lutein were investigated on TRPV1 and TRPA1 activation. RAMEB–lutein (100 μM) significantly diminished Ca2+ influx to cultured rat trigeminal neurons induced by TRPA1 activation with mustard oil, but not by TRPV1 stimulation with capsaicin, as determined with microfluorimetry. Calcitonin gene-related peptide release from afferents of isolated tracheae evoked by mustard oil, but not by capsaicin, was inhibited by RAMEB–lutein. Mustard oil-induced neurogenic mouse ear swelling was also significantly decreased by 100 μg/ml s.c. RAMEB–lutein pretreatment, while capsaicin-evoked edema was not altered. Myeloperoxidase activity indicating non-neurogenic granulocyte accumulation in the ear was not influenced by RAMEB–lutein in either case. It is concluded that lutein inhibits TRPA1, but not TRPV1 stimulation-induced responses on cell bodies and peripheral terminals of sensory neurons in vitro and in vivo. Based on these distinct actions and the carotenoid structure, the ability of lutein to modulate lipid rafts in the membrane around TRP channels can be suggested.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
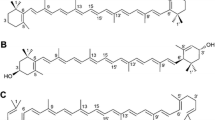
Carotenoids are isoprenoids which are important dietary nutrients with antioxidant potential (Britton et al. 1995; Krinsky 1989; Pfander 1992). They are lipophilic substances derived from the same basic C40 skeleton by different chemical modifications. Due to the large number of double bonds, there are extensive possibilities for geometrical (E/Z or trans/cis) isomerization in solutions. For pharmacological purposes, it is important to purify these substances and screen their biological activity. The majority of previous studies focused on β-carotene, but other carotenoids have also recently begun to draw attention (Molnár et al. 2005). The protective effects of natural carotenoids against severe degenerative, ischaemic, inflammatory, autoimmune and malignant diseases have been extensively investigated (Britton et al. 1995, 2008; Canfield et al. 1999; Krinsky 1998, 2005; Nishino et al. 2009; Pashkow et al. 2008; Schiedt and Liaaen-Jensen 1995; Tapiero et al. 2004).
Studies with polyunsaturated fatty acid-enriched model membranes revealed that interactions of carotenoids with lipid and protein structures can modify their chemical and physical properties, and therefore membrane stability. Data concerning the actions of carotenoids on oxidative processes are contradictory and seem to depend on the concentrations/doses and model systems. Divergent effects on lipid peroxidation rates were partially attributed to their orientation and location in membranes, as determined by small angle X-ray diffraction. Although the majority of papers describe their antioxidant and protective roles, there are also data on their harmful effects under certain conditions (McNulty et al. 2007, 2008).
Several experimental data and human reports indicate the role of carotenoids in inflammation and pain (Johnson and Krinsky 2009; Mayne et al. 2009; Palozza et al. 2009; Rock 2009). Although their anti-inflammatory effects are well established (Bhatt 2008; Hänninen et al. 2000; Quasim et al. 2003; Yaping et al. 2003), the mechanism of action is unknown. The importance of neuroimmune interactions has been emphasized in chronic inflammatory diseases and related pain (Cevikbas et al. 2007; Geppetti et al. 2008). Pro-inflammatory neuropeptides released from capsaicin-sensitive sensory nerves in response to the activation of transient receptor potential (TRP) ion channels, such as ankyrin repeat 1 (TRPA1) and vanilloid 1 (TRPV1) ionotropic receptors, induce neurogenic inflammation in the innervated area (Helyes et al. 2003; 2009; Szolcsányi 2004). TRPA1 receptors are activated by a variety of endogenous and exogenous ligands, e.g. mustard oil, formalin and cinnamaldehyde (Garcia-Anoveros and Nagata 2007), and TRPV1 channels are stimulated by capsaicin, noxious heat, protons and lipoxygenase products. Furthermore, both channels are sensitized by several inflammatory mediators, e.g. bradykinin and prostaglandins; therefore, they play an important role in inflammatory processes and related pain (Nilius, 2007; Schumacher, 2010).
Sensory neuropeptides, such as tachykinins (substance P: SP, neurokinin A and B), and calcitonin gene-related peptide (CGRP) released from capsaicin-sensitive afferents evoke consequent vasodilatation and plasma protein extravasation which play an important role in the pathophysiological mechanisms of a variety of chronic inflammatory diseases. These include ulcerative colitis, rheumatoid arthritis, allergic dermatitis, as well as neuropathic pain, which affect a large population (Geppetti et al. 2006) and cannot be satisfactorily treated by the conventional anti-inflammatory and analgesic drugs. Therefore there is a great need to precisely understand the mechanisms and to identify novel targets for drug development. Lipid rafts are microdomains rich in cholesterol, sphingomyelin and gangliosides. They have an important regulatory role on the function of receptors, such as the TRP channels (Szőke et al. 2010), and voltage-gated ion channels (Simons and Toomre 2000; Sjögren and Svenningsson 2007). Since carotenoids can incorporate into lipid rafts, they might influence the activation of TRP channels and consequently neurogenic inflammatory processes.
We have recently investigated the effects of three natural carotenoids with different structures (β-carotene, lutein and lycopene) on neurogenic inflammation of the mouse ear induced by topical application of the TRPA1 agonist mustard oil. Pretreatment with the oil injections of lutein and β-carotene containing α- and β-ionon rings significantly reduced mustard oil-induced ear edema, but lycopene composed of a linear structure had no anti-inflammatory effect (Horváth et al., submitted elsewhere). These data raised the possibility that lutein might negatively modulate lipid raft functions around the TRPA1 channels, which can be involved in its inhibitory effect on acute neurogenic inflammation (Horváth et al. 2009; 2010; Kemény et al. 2010a, b). The aim of the present experimental series was to systematically analyse the actions of lutein on the activation of TRPA1 and TRPV1 ion channels localized on sensory neurons and peripheral nerve terminals in vitro and in vivo.
Materials and Methods
Preparation of the Randomly Methylated-β-Cyclodextrin–Lutein Solutions
The randomly methylated-β-cyclodextrin (RAMEB)–lutein complex contains 1% lutein and was prepared by Cyclolab Ltd., a Hungarian cyclodextrin company (Budapest, Hungary; Iványi et al. 2008). Lutein packed in this complex was isolated from natural source (from Canadian goldenrod, Solidago canadensis L.; Horváth et al. 2010). The purity was >96%, as determined with liquid chromatography. Solutions of RAMEB–lutein were prepared freshly every day with cell culture medium, Krebs solution or sterile distilled water (Aqua ad injectabilia, Hungarian Pharmacopoea VIII.) in the different in vitro and in vivo experiments, respectively. The amount of lutein/RAMEB in 1 ml solution was 1 mg/100 mg. The administered concentrations and doses of RAMEB–lutein were calculated for the lutein content. The RAMEB vehicles used in the control experiments were also prepared the same way with the appropriate solvents and they had equal RAMEB concentrations to the respective RAMEB–lutein solutions. Solutions for the injections were stored in a dark bottle to avoid photo-degradation during the 24-h pretreatment period.
Ratiometric [Ca2+]i Measurement with the Fluorescent Indicator Fura-2 AM in Primary Cultures of Trigeminal Ganglion Neurons
Cultures were made from Wistar rat pups of 1–4 days old. The ganglia were dissected in ice cold phosphate-buffered solution (PBS), incubated for 35 min at 37°C in PBS-containing collagenase (Type XI, 1 mg/ml) and then in PBS with deoxyribonuclease I (1,000 units/ml) for 8 min. The ganglia were then rinsed with Ca2+- and Mg2+-free PBS and dissociated by trituration. Trigeminal ganglion cells were plated on poly-d-lysin-coated glass coverslips and grown in a nutrient-supplemented medium. The nutrient-supplemented cell culture medium contained 180 ml Dulbecco’s modified Eagle medium, 20 ml horse serum, 20 ml bovine albumin, 2 ml insulin–transferrin–selenium-S, 3.2 ml putrescin dihydrochloride (100 μg/ml), 20 μl triiodothyronine (0.2 mg/ml), 1.24 ml progesterone (0.5 mg/ml), 100 μl penicillin and 100 μl streptomycin. The coverslips were maintained at 37°C in a humid atmosphere with 5% CO2. Nerve growth factor (200 ng/ml) was added every other day, as described earlier (Szőke et al. 2000). All materials for cell culture were from Sigma Aldrich Ltd. (Hungary).
Cell cultures of 2–4 days old were stained for 30 min at 37°C in a solution containing (in mM): NaCl, 122; KCl, 3.3; CaCl2, 1.3; MgSO4, 0.4; KH2PO4 1.2; HEPES, 25; glucose, 10; pH 7.3 and 1 μM of fluorescent Ca2+ indicator dye, fura-2-AM (Invitrogen, California, USA). Dye loading was followed by at least a 5-min wash in extracellular solution (ECS) at room temperature. The ECS solution contained (in mM): NaCl, 160; KCl, 2.5; CaCl2, 1; MgCl2, 2; HEPES, 10; glucose, 10 and pH 7.3. Calcium transients of TRG neurons to chemicals were examined with a fluorescence microscope (Olympus BX50WI, Japan) placed on a vibration-free table (Supertech, Hungary; Szőke et al. 2000). ECS was gravity fed to the cells using a triple outlet tube of about 50 μm diameter from close vicinity. Test solutions arrived to the outlet via separate tubes, and the rapid changing of solutions was controlled by a fast step perfusion system (VC-77SP, Warner Instrument Corporation, Harvard Apparatus GmbH, Germany). Fluorescence images were taken with an Olympus LUMPLAN FI/×20 0.5 W water immersion objective and a digital camera (CCD, SensiCam PCO, Germany) connected to a Pentium II. This picture served as the reference for the later ones. Up to 12 dye-loaded cells were selected in each plate to monitor their fluorescence individually. Cells were illuminated alternately at 340 and 380 nm wavelength lights (for 50 to 400 ms each) generated by a monochromator (Polychrome II., Till Photonics, Germany) under the control of Axon Imaging Workbench 2.1 (AIW, Axon Instruments, CA). Emitted light >510 nm was measured. Data from points on the cell-free area of the plate were used for background substraction. The R = F340/F380 was monitored (rate 1 Hz) continuously for up to 5 min, while a few sample images were also recorded. The R values were not converted to intracellular free Ca2+ concentrations in this study. The R values generated by the AIW software were then processed by the Origin software version 7.0 (Originlab Corp. Northampton, USA). The baseline fluorescence was read from the period of recordings taken before exposing the cells to any drug. In the next step, the baseline was adjusted to R = 0 and the peak magnitude of ratiometric responses was calculated. Pre-incubation in the presence of 100 μM RAMEB–lutein or the respective RAMEB vehicle was performed for 60 min under these conditions directly before the measurement.
Measurement of Calcitonin Gene-Related Peptide Release from Isolated Rat Tracheae in Response to Chemical Activation
The trachea is densely innervated by capsaicin-sensitive peptidergic fibres and their terminals are close to the surface, which can be easily activated by different chemical stimuli. Therefore this has proven to be an excellent model system to study the effects of agents acting at the level of peripheral nerve terminals to modulate sensory neuropeptide release (Helyes et al. 2001). The whole rat tracheae were removed, cleaned of fat and adhering connective tissues and placed into an organ bath. They were perfused with controlled oxygenized Krebs solution for 60 min (equilibration period) at 37°C temperature, then incubated in the presence of RAMEB–lutein (100 μM and 1 mM) or RAMEB by itself (corresponding concentrations with the applied RAMEB–lutein) for 30 min. After discontinuation of the flow, the solution was changed three times for 8–8 min to produce pre-stimulated, stimulated and post-stimulated fractions. Chemical activation was performed in the second 8-min period with the selective TRPV1 agonist capsaicin (10−6 M) or the TRPA1 agonist mustard oil (10−4 M) to elicit CGRP release. CGRP concentrations were determined from 200 μl samples of the incubation medium of the trachea preparations by means of specific and sensitive radioimmunoassay methods developed in our laboratories (Helyes et al. 2006). At the end of the experiments, the trachea samples were weighed; CGRP release was calculated as fmol/mg wet tissue. The absolute peptide outflow in response to the chemical stimulations were calculated by adding CGRP release measured in the stimulated and post-stimulated fractions after taking off the basal release measured in the pre-stimulated 8-min fraction. In each group, six experiments were performed to provide n = 6 data per group (12 tracheae per group; two tracheae in each organ bath chamber).
Investigation of Mustard Oil- and Capsaicin-Induced Acute Neurogenic Inflammation of the Mouse Ear
Experiments were performed on 12-week-old CD1 mice of both sexes (25–35 g) bred and kept in the Laboratory Animal House of the Department of Pharmacology and Pharmacotherapy of the University of Pécs at 24–25°C and provided with standard rat chow and water ad libitum. All experimental procedures were carried out according to the 1998/XXVIII Act of the Hungarian Parliament on Animal Protection and Consideration Decree of Scientific Procedures of Animal Experiments (243/1988) and complied with the recommendations of the International Association for the Study of Pain and the Helsinki Declaration. The studies were approved by the Ethics Committee on Animal Research of Pécs University according to the Ethical Codex of Animal Experiments, and the licence was given (licence no.: BA 02/2000-11-2006).
Animals were pretreated s.c. with the 100 mg/kg dose of RAMEB–lutein (10 mg/ml, 0.1 ml/10 g) three times (0, 8 and 24 h) throughout a 24-h pretreatment period, and the inflammatory agents were applied topically. In the control group, the same volume of the respective RAMEB vehicle was administered. This dose was chosen on the basis of previous studies where dose–response relationship was investigated in this model (data not shown, submitted elsewhere). One hour after the last pretreatment, mice were anaesthesized with ketamine (100 mg/kg, i.p.) and xylazine (10 mg/kg, i.m.). In one series of experiments, ear inflammation was induced by the selective TRPA1 agonist mustard oil (5% dissolved in paraffin oil) applied topically on both surfaces (15–15 μl) of the ears at the beginning of the experiment and at the 3-h timepoint. In another series, the TRPV1 agonist capsaicin (2.5% dissolved in 96% ethanol) was administered the same way every hour during the 6-h period.
Ear diameter was measured with an engineer’s micrometer, and swelling was expressed as percentage compared to the initial control values. Dissected ears were fixed in 4% buffered formaldehyde. Cross sections (4 μm) were cut at the base of the ears after paraffin embedding and stained with haematoxylin–eosin. Ear diameters were also measured on the histological sections. Myeloperoxidase (MPO) activity correlating with the number of accumulated granulocytes was also measured from the ear homogenates by spectrophotometry 6 h after the induction of the inflammation (Kemény et al. 2010a, b).
Statistical Analysis
Results are shown as means ± S.E.M of ten mice per group. Statistical analysis was performed by ANOVA followed by Bonferroni’s modified t test; in all cases, p < 0.05 was considered statistically significant. Percent of responsive and non-responsive cells were statistically analysed by Fisher’s exact test.
Results
Effect of RAMEB–Lutein on Mustard Oil- and Capsaicin-Evoked Ca2+ Influx in Cultured TRG Neurons
In the first series of experiments, the percentage of neurons responding with Ca2+ influx to 200 μM mustard oil or 330 nM capsaicin was determined in control plates (Fig. 1). Response to mustard oil had a longer duration and developed after a longer latency (20–30 s). Response to capsaicin had a short latency (1–2 s), and it was either transient or had a biphasic waveform with an initial peak followed by a prolonged plateau. The percentage of mustard oil- and capsaicin-responsive cells was 25.6% (21 out of 82) and 62.2% (33 out of 53), respectively. In the second series of experiments, the effect of 100 μM RAMEB–lutein treatment was investigated on the ratio of trigeminal neurons, which responded to mustard oil or capsaicin administration compared to RAMEB vehicle. Significant decrease in the percent of mustard oil-sensitive cells was observed after RAMEB–lutein treatment, 6.5% of the cells responded with Ca2+ influx (eight out of 123) to mustard oil. In contrast RAMEB–lutein had no effect on the percent of capsaicin-sensitive cells, 65% of the neurons responded to capsaicin exposure (34 out of 52). RAMEB alone did not influence the proportion of mustard oil- and capsaicin-responsive neurons, the values were 29.5% (31 out of 105) and 51% (38 out of 74), respectively.
Effect of RAMEB–lutein on TRPA1 and TRPV1 activation-induced Ca2+ influx in cultured trigeminal ganglion neurons. Columns show the percentage of neurons responding to the TRPA1 activating agent mustard oil (200 μM) or the TRPV1 agonist capsaicin (330 nM) in untreated control, RAMEB-solvent-treated and 100 μM RAMEB–lutein-treated cell cultures. n = 53–123 cells per group. Percent of responsive and non-responsive cells were statistically analysed by Fisher’s exact test
Effect of RAMEB–Lutein on Mustard Oil- and Capsaicin-Evoked CGRP Release
Capsaicin (10−7 M) evoked an almost double CGRP release than mustard oil (10−4 M) from the peptidergic afferents of isolated rat tracheae in the presence of RAMEB vehicle. Interestingly, in case of the ten times higher concentration of RAMEB itself CGRP release decreased for both chemical stimulants. Peptide release in the presence of 100 μM and 1 mM RAMEB–lutein was compared to the corresponding concentrations of the RAMEB vehicle. RAMEB–lutein incubation inhibited the mustard oil-evoked release of CGRP in a concentration-dependent manner: 100 μM RAMEB–lutein induced a non-significant, 25% decrease (0.75 ± 0.24 vs. 0.57 ± 0.12 fmol/mg), but the 1 mM concentration produced a significant, 70% inhibition compared to respective control (0.37 ± 0.11 vs. 0.11 ± 0.05 fmol/mg; Fig. 2a). In contrast, neither concentrations of RAMEB–lutein inhibited significantly the capsaicin-evoked CGRP outflow in comparison with the respective RAMEB-treated controls (Fig. 2b).
Effect of RAMEB–lutein on TRPA1 and TRPV1 activation-induced calcitonin gene-related peptide (CGRP) release from capsaicin-sensitive afferents. Columns represent the means ± S.E.M. of a 10−4 M mustard oil- and b 10−7 M capsaicin-induced CGRP released from the peripheral terminals of sensory nerves of isolated rat tracheae in the presence of 100 μM or 1 mM lutein–RAMEB compared to the respective concentration of the RAMEB vehicle; n = 5 experiments/group (*p < 0.05 compared to the respective RAMEB-vehicle-pretreated group; ANOVA + Bonferroni’s modified t test)
Effect of RAMEB–Lutein on Mustard Oil- and Capsaicin-Induced Acute Neurogenic Ear Swelling
Stimulation of the TRPA1 channels on sensory nerve endings of the mouse ear with 5% mustard oil-induced ear swelling reaching its maximum, 35%, at the 5-h timepoint (Fig. 3a). Meanwhile, the activation of the TRPV1 receptors with 2.5% capsaicin resulted in a 50% neurogenic edema formation 1 h after its topical application, which gradually decreased during the 6-h experiment to about 15% in the 100 mg/kg RAMEB-vehicle-treated group (Fig. 3b). The mustard oil-induced neurogenic edema was significantly decreased by 3 × 100 mg/kg s.c. RAMEB–lutein pretreatment after the third hour, but the capsaicin-evoked swelling was not altered (Fig. 3). The areas under the ear swelling curves (AUC) were 151.4 ± 17.1 and 54.0 ± 10.5 for the RAMEB–lutein and the RAMEB-vehicle-pretreated groups in case of mustard oil stimulation (***p < 0.001). The corresponding values were 169.3 ± 8.5 and 158.4 ± 14.6 for capsaicin activation (NS).
Effect of RΑΜΕΒ–lutein on TRPA1 and TRPV1 activation-induced mouse ear edema. Ear swelling induced by topical application of a 5% mustard and b 2.5% capsaicin on the mouse ear in RAMEB–lutein-pretreated mice (3 × 100 mg/kg s.c. during a 24-h pretreatment period completed 1 h before the induction of the inflammation). RAMEB pretreatment according to the same protocol served as control. Results are expressed as percentage swelling compared to the initial control values; data are means ± S.E.M. of n = 10 animals/group (**p < 0.01 compared to the RAMEB-vehicle-pretreated group; ANOVA + Bonferroni’s modified t test)
Effect of RAMEB–Lutein on Mustard Oil- and Capsaicin-Induced MPO Activity in the Ear
Both mustard oil and capsaicin induced a similar, tenfold increase of the MPO activity in the ear homogenates 6 h after the induction of the inflammation, which is a quantitative biochemical marker of neutrophil and macrophage accumulation. Pretreatments with 3 × 100 mg/kg s.c. RAMEB–lutein did not influence MPO increase in response to either TRPV1 or TRPA1 stimulation (Fig. 4a, b).
Effect of RΑΜΕΒ–lutein on TRPA1 and TRPV1 activation-induced myeloperoxidase (MPO) activity in the ear homogenates. Ear samples were excised 6 h after topical application of a 5% mustard oil and b 2.5% capsaicin. RAMEB and RAMEB–lutein were injected s.c. in 3 × 100 mg/kg dose during a 24-h pretreatment period, intact samples refer to untreated mice. Columns show the means ± S.E.M. of n = 10 mice/group (ANOVA + Bonferroni’s modified t test)
Effect of RAMEB–Lutein on Mustard Oil- and Capsaicin-Induced Histopathological Changes
Microscopical examinations and measurements confirmed edema formation of the mouse ear in response to mustard oil smearing (intact: 240.2 ± 36.3 μm; RAMEB-vehicle-pretreated mustard oil-treated control: 417.3 ± 35.7 μm). Furthermore, a remarkable influx of inflammatory cells, particularly neutrophils, also occurred 6 h after mustard oil administration compared to the non-inflamed ears (Fig. 5a, b). Mustard oil-evoked edema was significantly diminished by this RAMEB–lutein pre-administration (Fig. 5c, d). In contrast, remarkable difference was not observed in the influx of inflammatory cells after RAMEB–lutein injections, which is supported by the MPO results. In accordance with the in vivo measurements, capsaicin-induced ear swelling was only minimal at the 6-h timepoint as determined on the histological slides, and there was no significant difference in the RAMEB–lutein-pretreated group (data not shown).
Effect of RΑΜΕΒ–lutein on TRPA1 activation-induced histopathological alterations in the mouse ear. a, b, c The representative light micrographs of the mouse ear cross sections: a intact, untreated mouse ear; b 5% mustard oil-smeared ear of a RAMEB-vehicle-pretreated mouse (RAMEB + MO) and c 5% mustard oil-smeared ear of a 3 × 100-mg/kg s.c. RAMEB–lutein-pretreated mouse (RAMEB–lutein + MO) taken 6 h after the induction of the inflammation. Haematoxylin–eosin staining, ×100 magnification. d The means ± S.E.M. of ear diameter values measured on the histological slides; n = 10 samples/group (++ p < 0.01 vs. intact; *p < 0.05 vs. RAMEB; ANOVA + Bonferroni’s modified t test)
Discussion
The results of these studies provide complex, integrative experimental evidence for the ability of RAMEB–lutein to inhibit TRPA1-induced responses on the cell bodies, as well as peripheral terminals of capsaicin-sensitive primary sensory neurons both in vitro and in vivo. RAMEB–lutein significantly decreases neurogenic ear swelling in response to TRPA1 receptor activation by 5% mustard oil. It has been previously shown that mustard oil in this concentration selectively activates capsaicin-sensitive sensory nerves, evokes the release of pro-inflammatory sensory neuropeptides, such as SP and CGRP, and induces acute vasodilatation and plasma protein extravasation exclusively this neurogenic mechanism (Bánvölgyi et al. 2004; Szolcsányi 2004). The ability of RAMEB–lutein to attenuate mustard oil-induced CGRP release was also evidenced in our in vitro system, which explains the in vivo results. Similarly to these functional data obtained at the level of the peripheral nerve terminals, RAMEB–lutein also inhibits mustard oil-evoked Ca2+ influx in TRG neurons.
In contrast to the inhibitory actions seen on TRPA1 activation, RAMEB–lutein does not influence TRPV1-evoked actions in any systems. Based on the finding that lutein inhibits the activation of TRPA1, but not that of TRPV1 channels, and its ability to be incorporated in membranes, its selective modulatory action on lipid raft functions around the TRPA1 receptors can be proposed. Lipid rafts, which are microdomains rich in cholesterol, sphingolipids and phospholipids, have been evidenced to exert crucial functional significance around glycoprotein structures of ligand-gated ion channels, such as the nicotinic receptor (Corbin et al. 1998; Simons and Toomre 2000; Sjögren and Svenningsson 2007). These lipid rafts are able to regulate channel functions in different ways: sphingolipids and cholesterol can directly interact with the receptor protein and lipid components, as well as affect the physical features of the lipid bilayer (Dart, 2010).
The concept suggesting potential lipid raft modulation by lutein is supported by the fact that the polar carotenoid lutein containing hydroxylated α- and β- ionon rings can be perfectly incorporated into membrane bilayers due to its rod-like structure, polar end groups and the molecular dimensions matching the thickness of the bilayer. Furthermore, it has a specific position of one double bond in one of its rings and it has one membrane-spanning segment and one oriented horizontally (Britton et al. 2008). Lutein was shown to be segregated out from saturated lipid regions of the membrane and accumulate in segments which are rich in unsaturated phospholipids (Wiśniewska et al. 2003, 2006).
We have shown that the depletion of cholesterol by methyl-β-cyclodextrin results in an inhibition of TRPV1 activation (Szőke et al. 2010), which is supported by earlier electrophysiological data (Liu et al. 2006). We showed different effects of cholesterol depletion on Ca2+ responses induced by resiniferatoxin or capsaicin, two TRPV1 agonists activating the receptor through distinct binding sites (Szolcsányi 2002, 2008). Methyl-β-cyclodextrin inhibited the effect of capsaicin, but not that of resiniferatoxin on TRPV1-expressing CHO cells. Decomposition of lipid rafts surrounding the ligand-gated ion channel influenced only one of the two binding sites. Consequently, the microenvironments of receptor proteins in the lipid rafts might have a significant importance in receptor activation (Szőke et al. 2010). It is worth mentioning that in the present experiments the RAMEB vehicle, which is a similar molecule to methyl-β-cyclodextrin, by itself exerted a clear concentration-dependent inhibition on CGRP release, as compared to earlier control experiments using only Krebs solution (Helyes et al. 2006; Börzsei et al. 2008). However, the significant CGRP release inhibiting action of RAMEB–lutein versus the corresponding RAMEB vehicle control is remarkable in case of the 1 mM concentration. Similarly, in the in vivo studies the RAMEB vehicle also decreased ear swelling in response to both stimulants compared to saline used in previous experiments (Bánvölgyi et al. 2004), but the effect of RAMEB–lutein was remarkable on the mustard oil-evoked edema formation compared to RAMEB by itself.
Despite the acute neurogenic edema, RAMEB–lutein does not inhibit mustard oil-evoked MPO activity elevation in tissue homogenates reflecting to the accumulation of neutrophils and macrophages in the subcutaneous tissue. We have demonstrated earlier that neurogenic inflammatory components and sensory nerves are not involved in this later, non-neurogenic inflammatory process (Bánvölgyi et al. 2004).
In conclusion, the present results provide two important messages. On one hand, they help to understand the activation mechanisms of TRP channels and the significance of potential lipid raft modulation in their function. On the other hand, they also add significant novel information in elucidating the processes involved in the inhibitory actions of lutein on neural activation with special emphasis on the neurogenic inflammatory components and TRPA1 functions. A possible important role of hydrophobic interactions of agonists or antagonists both to the TRPA1 protein and to the surrounding lipid raft might give further clues for drug development. This research direction can open interesting new perspectives for the development of novel anti-inflammatory and analgesic therapies.
References
Bánvölgyi Á, Pozsgai G, Brain SD et al (2004) Mustard oil induces a transient receptor potential vanilloid 1 receptor-independent neurogenic inflammation and a non-neurogenic cellular inflammatory component in mice. Neuroscience 125:449–459
Bhatt DL (2008) Anti-inflammatory agents and antioxidants as a possible “Third Great Wave” in cardiovascular secondary prevention. Am J Cardiol 101:4D–13D
Börzsei R, Pozsgai G, Bagoly T et al (2008) Inhibitory action of endomorphin-1 on sensory neuropeptide release and neurogenic inflammation in rats and mice. Neuroscience 152(1):82–88
Britton G, Liaaen-Jensen S, Pfander H (1995) Carotenoids today and challenges for the future. In: Britton G, Liaaen-Jensen S, Pfander H (eds) Carotenoids, vol 1A. Birkhäuser, Basel, Boston, Berlin, pp 13–26
Britton G, Liaaen-Jensen S, Pfander H (2008) Special molecules, special properties. In: Britton G, Liaaen-Jensen S, Pfander H (eds) Carotenoids, vol 4. Birkhäuser, Basel, Boston, Berlin, pp 1–6
Canfield LM, Hu X, White KM, Jacobsen NE, Mangelsdorf DJ (1999) β-Carotene oxidation products inhibit growth and cholesterol synthesis in breast cancer cells. 12th International Carotenoid Symposium, Cairns, Australia. Abstract 6A-4:191
Cevikbas F, Steinhoff A, Homey B, Steinhoff M (2007) Neuroimmune interactions in allergic skin diseases. Curr Opin Allergy Clin Immunol 7(5):365–373
Corbin J, Méthot N, Wang HH, Baenziger JE, Blanton MP (1998) Secondary structure analysis of individual transmembrane segments of the nicotinic acetylcholine receptor by circular dichroism and Fourier transform infrared spectroscopy. J Biol Chem 273(2):771–777
Dart C (2010) Lipid microdomains and the regulation of ion channel function. J Physiol 588:3169–3178
Geppetti P, Materazzi S, Nicoletti P (2006) The transient receptor potential vanilloid 1: role in airway inflammation and disease. Eur J Pharmacol 533(1–3):207–214
Geppetti P, Nassini R, Materazzi S, Benemei S (2008) The concept of neurogenic inflammation. BJU Int 101(Suppl 3):2–6
Garcia-Anoveros J, Nagata K (2007) Trpa1. Handb Exp Pharmacol 179:347–362
Hänninen O, Kaartinen K, Rauma AL et al (2000) Antioxidants in vegan diet and rheumatic disorders. Toxicology 155:45–53
Helyes Z, Pintér E, Németh J et al (2001) Anti-inflammatory effect of synthetic somatostatin analogs in the rat. Br J Pharmacol 134:1571–1579
Helyes Z, Pintér E, Németh J, Szolcsányi J (2003) Pharmacological targets for the inhibition of neurogenic inflammation. Curr Med Chem 2:191–218
Helyes Z, Pintér E, Németh J et al (2006) Effects of the somatostatin receptor subtype 4 selective agonist J-2156 on sensory neuropeptide release and inflammatory reactions in rodents. Br J Pharmacol 149:405–415
Helyes Z, Pintér E, Szolcsányi J (2009) In: Kovács M, Merchenthaler I (eds) Regulatory role of sensory neuropeptides in inflammation, in neuropeptides and peptide analogs, vol 7. Research Signpost, Kerala, India, pp 111–141
Horváth Gy, Molnár P, Deli J et al (2009) Karotinoidok hatásának vizsgálata neurogén gyulladásos folyamatokra in vivo egérmodellekben. Congressus Pharmaceuticus Hungaricus XIV. Budapest, Abstract (P-26). Gyógyszerészet Supplementum 11(Supl. I):S83
Horvárth Gy, Molnár P, Farkas Á, Szabó LGy, Turcsi E, Deli J (2010) Separation and identification of carotenoids in flowers of Chelidonium majus L. and inflorescenses of Solidago canadensis L. Chromatographia Supplement 71:103–108
Iványi R, Németh K, Visy J, Szeman J, Szente L, Simonyi M (2008) Water soluble carotenoid/CD complexes: preparation, characterization. The 14th International Cyclodextrins Symposium—Kyoto, Japan, Abstract book no. P1-29
Johnson EJ, Krinsky NI (2009) Carotenoids and coronary heart disease. In: Britton G, Liaaen-Jensen S, Pfander H (eds) Carotenoids, vol 1A. Birkhäuser, Basel, Boston, Berlin, pp 287–300
Kemény Á, Horváth Gy, Molnár P et al (2010a) Effects of carotenoids on skin inflammation in in vivo mice models. IBRO International Workshop, Pécs. Abstract P4–16:26
Kemény Á, Reglődi D, Cseharovszky R et al (2010b) Pituitary adenylate cyclase-activating polypeptide deficiency enhances oxazolone-induced allergic contact dermatitis in mice. J Mol Neurosci 42:443–449
Krinsky NI (1989) Carotenoids in medicine. In: Krinsky NI, Mathews-Roth MM, Taylor RF (eds) Carotenoids: chemistry and biology, I. Plenum, New York, pp 279–291
Krinsky NI (1998) The antioxidant and biological properties of the carotenoids. Annu NY Acad Sci 854:443–447
Krinsky NI, Johnson EJ (2005) Carotenoid actions and their relation to health and disease. Mol Aspects Med 26:459–516
Liu M, Huang W, Wu D, Priestley JV (2006) TRPV1, but not P2X, requires cholesterol for its function and membrane expression in rat nociceptors. Eur J Neurosci 24(1):1–6
Mayne ST, Wright ME, Cartmel B (2009) Epidemiology and intervention trials. In: Britton G, Liaaen-Jensen S, Pfander H (eds) Carotenoids, vol 5. Birkhäuser, Basel, Boston, Berlin, pp 191–210
McNulty H, Byun J, Lockwood SF, Jacob RF, Mason RP (2007) Differential effects of carotenoids on lipid peroxidation due to membrane interactions: X-ray diffraction analysis. Biochim Biophys Acta 1768:167–174
McNulty H, Jacob RF, Mason RP (2008) Biologic activity of carotenoids related to distinct membrane physicochemical interactions. Am J Cardiol 101:20D–29D
Molnár P, Kawase M, Motohashi N (2005) Isolation, crystallization and handling of carotenoids and (E/Z)-isomerization of carotenoids. In: Motohashi N (ed) Functional polyphenols and carotenoids with antioxidative action. RSFLASH, Kerala, pp 111–131, a review book series of Chem Pharm Sci
Nilius B (2007) Transient receptor potential (TRP) cation channels: rewarding unique proteins. Bull Mém Acad R Méd Belg 162(3–4):244–253
Nishino H, Murakoshi M, Tokuda H, Satomi Y (2009) Cancer prevention by carotenoids. Arch Biochem Biophys 483:165–168
Palozza P, Serini S, Ameruso M, Verdecchia S (2009) Modulation of intracellular signalling pathways by carotenoids. In: Britton G, Liaaen-Jensen S, Pfander H (eds) Carotenoids, vol 5. Birkhäuser, Basel, Boston, Berlin, pp 211–234
Pashkow FJ, Watumull DG, Campbell CL (2008) Astaxanthin: a novel potential treatment for oxidative stress and inflammation in cardiovascular disease. Am J Cardiol 101:58D–68D
Pfander H (1992) Carotenoids: an overview in methods in enzymology, vol 213. Academic, New York, pp 3–31
Quasim T, McMillan DC, Talwar D, Sattar N, O'Reilly J, Kinsella J (2003) Lower concentrations of carotenoids in the critically-ill patient are related to a systemic inflammatory response and increased lipid peroxidation. Clin Nutr 22(5):459–462
Rock CL (2009) Carotenoids and cancer. In: Britton G, Liaaen-Jensen S, Pfander H (eds) Carotenoids, vol 5. Birkhäuser, Basel, Boston, Berlin, pp 269–286
Schiedt K, Liaaen-Jensen S (1995) Isolation and analysis. In: Britton G, Liaaen-Jensen S, Pfander H (eds) Carotenoids, vol 1A. Birkhäuser, Basel, Boston, Berlin, pp 109–144
Schumacher MA (2010) Transient receptor potential channels in pain and inflammation: therapeutic opportunities. Pain Pract 10(3):185–200
Simons K, Toomre D (2000) Lipid rafts and signal transduction. Nat Rev Mol Cell Biol 1:31–39
Sjögren B, Svenningsson P (2007) Depletion of the lipid raft constituents, sphingomyelin and ganglioside, decreases serotonin binding at human 5-HT7(a) receptors in HeLa cells. Acta Physiol 190:47–53
Szolcsányi J (2002) Capsaicin receptor as target molecule on nociceptors for development of novel analgesic agents. In: Kéri G, Tóth I (eds) Molecular pathomechanisms and new trends in drug research. Taylor and Francis, London, pp 319–333
Szolcsányi J (2004) Forty years in capsaicin research for sensory pharmacology and physiology. Neuropeptides 38(6):377–384
Szolcsányi J (2008) Hot target on nociceptors: perspectives, caveats and unique features. Br J Pharmacol 155(8):1142–1144
Szőke É, Zs B, Csernoch L, Czéh G, Szolcsányi J (2000) Interacting effects of capsaicin and anandamide on intracellular calcium in sensory neurons. Neuroreport 11:1949–1952
Szőke É, Börzsei R, Tóth DM et al (2010) Effect of lipid raft disruption on TRPV1 receptor activation of trigeminal sensory neurons and transfected cell line. Eur J Pharmacol 628(1–3):67–74
Tapiero H, Townsend DM, Tew KD (2004) The role of carotenoids in the prevention of human pathologies. Biomed Pharmacother 58:100–110
Wiśniewska A, Draus J, Subczynski WK (2003) Is a fluid-mosaic model of biological membranes fully relevant? Studies on lipid organization in model and biological membranes. Cell Mol Biol Lett 8(1):147–159
Wisniewska A, Widomska J, Subczynski WK (2006) Carotenoid-membrane interactions in liposomes: effect of dipolar, monopolar, and nonpolar carotenoids. Acta Biochim Pol 53(3):475–484
Yaping Z, Wenli Y, Weile H, Ying Y (2003) Anti-inflammatory and anticoagulant activities of lycopene in mice. Nutr Res 23(11):1591–1595
Acknowledgements
The authors thank Anikó Hirné Perkecz for the preparation of the histological slides and Dániel Tóth for technical assistance. Attila Dévay, the Head of Institute of Pharmaceutical Technology and Biopharmacy, for technical support. Our work was supported by OTKA K60121, K76176 K73044, K78059, ETT 03-380/2009, ETT 04-364/2009 and the “Science, Please! Research Teams on Innovation” programme (SROP-4.2.2/08/1/2008-0011) and Developing Competitiveness of Universities in the South Transdanubian Region (SROP-4.2.1.B-10/2/KONV-2010-0002). Györgyi Horváth was supported by PTE ÁOK KA-34039-35/2009 grant.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Horváth, G., Szőke, É., Kemény, Á. et al. Lutein Inhibits the Function of the Transient Receptor Potential A1 Ion Channel in Different In Vitro and In Vivo Models. J Mol Neurosci 46, 1–9 (2012). https://doi.org/10.1007/s12031-011-9525-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12031-011-9525-3