Abstract
In mature mammals, optic nerve injury results in apoptosis of retinal ganglion cells. The literature confirms that lens injury enhances retinal ganglion cells survival, but the mechanism is not very clear. Using silver staining method and computer image analysis techniques, the effect of α-crystallin, a major component of the lens in the survival of retinal ganglion cell axons, was investigated in vivo after intravitreal injections. The results showed that enhanced survival of axotomized axons was observed beyond the crush site after a single intravitreal administration of α-crystallin at the time of axotomy. Axonal density of the retinal ganglion cell was significantly greater than in the untreated controls until 2 weeks after injection. This effect declined by 4 weeks after injection but survival of axons remained greater than controls. These findings indicate that α-crystallin plays a key role in protecting axons after optic nerve injury.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Axonal injury in the central nervous system of adult mammals often results in neuronal death. In the optic nerve, as in other central nervous system pathways, injured axons have shown a transient local sprouting reaction but no long-range growth (Hadani et al. 1984; Schwartz et al. 1985). In rats, about 90% of the retinal ganglion cells were lost within 2 weeks of optic nerve transection near the eyeball (Mey and Thanos 1993; Berkelaar et al. 1994). Neurons were presumed to die because they were deprived of the trophic support normally provided by the distant targets and the non-neuronal cells surrounding their axons. However, both cell death and regenerative failure could be altered by manipulation of extracellular conditions. Intravitreal injections of brain-derived neurotrophic factor (BDNF), neurotrophin (NT)-4/5, ciliary neurotrophic factor (CNTF), glial-derived neurotrophic factor (GDNF), and other polypeptide growth factors have enhanced transient retinal ganglion cell survival after nerve injury (Carmignoto et al. 1989; Mey and Thanos 1993; Cohen et al. 1994; Mansour-Robaey et al. 1994; Rabacchi et al. 1994; Sawai et al. 1996; Ge et al. 1998; Cui and Harvey 2000).
Several lines of evidence have suggested that a small puncture wound to the lens enhances retinal ganglion cell survival and enables these cells to regenerate their axons into the normally inhibitory environment of the optic nerve (Fischer et al. 2000, 2001; Heiduschka et al. 2005). Retinal ganglion cell axons may form growth cones at the site of injury in the optic nerve and terminate within the retinoreceptive layers of the superior colliculus 5 weeks after lesion (Fischer et al. 2001). Combining nerve injury with lens puncture has led to an eightfold increase in retinal ganglion cell survival and a 100-fold increase in the number of axons regenerating beyond the crush site (Leon et al. 2000). For the first time, these findings suggested that lentogenic stimulation of retinal ganglion cells was sufficient to induce regrowth of axons that could override inhibitors at the site of injury, grow through the white matter of the optic nerve, pass through the optic chiasm, and make synaptic connections within the brain. Various mechanisms associated with this enhancement have been proposed, including macrophage recruitment, activated retinal astrocytes cells, and stimulatory factors from the lens epithelial cells (Yin et al. 2003; Stupp et al. 2005; Liu et al. 2006; Wong et al. 2006; Yin et al. 2006). In vitro, co-culture of retinal ganglion cells from intact mice with macrophage-rich lesioned lenses led to increased axon lengths compared with co-culture with macrophage-free intact lenses, suggesting that lens-derived neurotrophic factor after interaction with macrophages may be helpful in the regeneration of optic nerve axons (Lorber et al. 2005). However, the role of specific lens components in optic nerve survival and/or regeneration has yet to be elucidated.
α-Crystallin belongs to the family of small heat shock proteins (sHSPs), including Hsp25 and Hsp27 (Derham and Harding 1999), which comprise of as much as 40% of the cytoplasmic proteins in lens cells of the eye and are thought to play an essential role in maintaining its transparency. Many studies on α-crystallins deal with their abundant expression and role in the lens and multiple tissues of the body (Srinivasan et al. 1992). The two forms of α-crystallin, A and B, share an amino acid sequence homology of about 57% and have been found in heterogeneous aggregates of the two proteins (Horwitz 1992). Retinal pigment epithelium cells over-expressing α-crystallin have shown resistance to apoptosis, suggesting that α-crystallin might play a beneficial role in preventing stress-induced cell death (Alge et al. 2002). α-Crystallin has also been found to have antiapoptotic activity and is a potent negative regulator in several inflammatory pathways for both the immune system and central nervous system (Masilamoni et al. 2006). In vivo α-crystallin expression has been protected against cell death during mitosis in the lens epithelium (Bai et al. 2004; Andley 2007). These results suggest that α-crystallin might provide crucial physiological protection in tissues (Kamradt et al. 2001).
In this work, we studied the effects of early intravitreal administration of α-crystallin on the survival of retinal ganglion cell axons in adult rats.
Materials and Methods
Surgical Procedures
All surgical procedures, including intraocular injections, were performed in the Long–Evans rats (250–270 g) under general anesthesia (10% chloral hydrate; 40 mg per g of body weight, i.p.), with the approval of the animal ethical committee of the Southwest Hospital, Chongqing, China. All animals had bilateral intraorbital optic nerve crush. A 1-cm incision was made in the conjunctiva at the temporal side of each eye. The optic nerve was exposed under an operating microscope, and its dura was opened longitudinally. Using blood vessel forceps, the optic nerve was crushed 2 mm behind the nerve head for 5 s, avoiding injury to the ophthalmic artery. Nerve injury was verified by the appearance of a clearing at the crush site, and the vascular integrity of the retina was verified by funduscopic examination. α-Crystallin (10−4 g/l; 2 μl) was injected into vitreous space by posterior approach in the right eyes, which served as the experimental eyes, taking care not to damage the lens. The same volume of saline was injected in left eyes, which also had optic nerve crushes and served as control. Topical anti-inflammatory eyedrops were administrated for 3 days after operation. Another group of normal animals without nerve crushes was also maintained. Food and water were provided ad libitum postoperatively.
The rats were perfused through the heart with cold saline plus heparin followed by 4% paraformaldehyde at 1, 2, and 4 weeks after optic nerve crush injury. Both the right and left optic nerve segments up to the optic chiasm were dissected free and embedded with wax.
Silver Staining
Serial cross-sections (5-μm thick) of the optic nerve were cut. Sections were collected at the crush injury site at 0.5, 2, 5 mm distal to the site. Silver staining was performed and sections were examined under a light microscope.
Computer Image Analysis
All morphometric parameters were counted by light microscopy using image analyzing computer program MetaMorph Imaging System version 3.5 (MDS Inc., Ontario, Canada). The cross-sectional profile of each optic nerve under a magnification of ×200 and 15 random fields under a ×100 oil-immersion objective in each sample were photographed with SPOT cooled color digital camera (Diagnostic Instruments Inc., Michigan, USA) and a microscope Zeiss Axiophot 2 (Carl Zeiss, Inc., Germany).
The number of the optic nerve axons was counted in the photographs taken, and the density (expressed as number/μm2) was calculated.
Statistical Analysis
Quantitative data were analyzed using paired t tests between the experimental and control groups. Data were presented as mean ± standard deviation. P values < 0.05 were considered significant.
Results
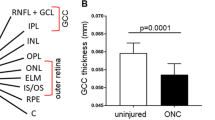
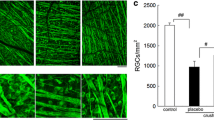
A total of 21 histological samples (three in normal group, nine in experiment group, and nine in control group) and 315 fields of the optic nerve were selected for morphometric analysis. The appearance of axons was depicted in Figs. 1 and 2a,b before and after crushing, and in the normal. In the normal optic nerves, there were 0.100214 ± 0.0148 axons per μm2 (mean ± SD).
The crush injury of the optic nerve caused marked decreases in the numbers of axon in the control eyes at 1 week after injury. The axonal density was 0.060468 ± 0.0062 per μm2 (60.3% of the normal) in the left control eyes, compared with the right experimental eyes that had 0.073332 ± 0.0039 per μm2 (73.2% of the normal) at 0.5 mm distal to the injury site. At 2 mm distal to the site, the axonal number was 0.067742 ± 0.0053 per μm2 (67.6% of the normal) in the left control compared with 0.084054 ± 0.0053 per μm2 (83.9% of the normal) in the right experimental eyes. At 5 mm distal to the injury site, axonal density in the left control eyes was 0.084544 ± 0.0071 per μm2 (84.4% of the normal) versus 0.091681 ± 0.0052 per μm2 (91.5% of the normal) in the right experimental eyes. It was evident that degeneration was more apparent near the site of the lesion.
Two weeks after optic nerve injury, more axons were lost in both eyes. In the left control eyes, axonal number at 0.5 mm distal to the injury site was 0.012355 ± 0.0024 per μm2 (12.3% of the normal). After injections of α-crystallin, axonal density was 0.016045 ± 0.0023 per μm2 (16.0% of the normal) in the right experimental eyes. At 2 mm distal to the site, axonal density was 0.011282 ± 0.0025 per μm2 (11.3% of the normal) in the left control eye compared with the right experimental eye of 0.020708 ± 0.0043 per μm2 (20.7% of the normal). At 5 mm distal to the injury site, axonal density was 0.017218 ± 0.0035 per μm2 (17.2% of the normal) in the left control versus 0.028186 ± 0.0055 per μm2 (28.1% of the normal) in right eyes.
By 4 weeks after optic nerve injury, the numbers of axons decreased for all groups, but the values for the α-crystallin-treated right eyes remained significantly greater than the left control. At 0.5 mm distal to the injury site, axonal density declined to 12.7% of the normal (0.012684 ± 0.0020 per μm2) in right eyes compared with 6.37% of the normal in left eyes (0.006385 ± 0.0012 per μm2). At 2 mm distal to the site, the number of axons fell to 11.9% of the normal (0.011928 ± 0.0024 per μm2) for α-crystallin-treated group and to 6.12% of the normal (0.006129 ± 0.0015 per μm2) for the control. At 5 mm distal to the injury site, axonal density in the left eyes was 0.005786 ± 0.0032 per μm2 (5.77% of the normal) versus 0.008443 ± 0.0017 per μm2 (8.42% of the normal) in right eyes. The data are summarized in Figs. 3, 4, and 5.
Discussion
In mature mammals, retinal ganglion cells are unable to regrow injured axons and soon undergo apoptotic death. However, as shown in this study, the greater survival of axotomized axons observed after intravitreal administration of α-crystallin was consistent with the hypothesis that molecules derived from the lens (e.g., α-crystallin) are an important survival factor for these neurons (Lorber et al. 2005). In this case, α-crystallin assisted the survival of nearly 40% more of the axotomized axons 1 week after crush injury. This study, on the other hand, did not assess the possibility of collateral sprouting in the optic nerve.
α-Crystallin is a member of the mammalian sHsp superfamily that function as cytoprotective molecular chaperones, preventing stress-induced aggregation of denaturing proteins, as well as keeping aggregation-prone proteins in reservoirs of non-native refoldable intermediates by holding proteins within large, soluble, multimeric structures (Ghosh et al. 2005, 2006; Parcellier et al. 2005; Ohto-Fujita et al. 2007). In the human body, α-crystallin was expressed at much lower levels in other body tissues than in the lens (Bhat et al. 1991; Srinivasan et al. 1992). α-Crystallin shares a close homology with another sHsp termed Hsp27; both of these proteins were activated in response to stress such as radiation, heat shock, hyper- or hypo-oxidation (Mehlen et al. 1996; Andley et al. 1998; Regini et al. 2004). Moreover, both proteins have been shown to have antiapoptotic functions by interfering with the activity of various apoptotic proteins (Clark and Muchowski 2000; Parcellier et al. 2005; Sun and MacRae 2005). It has also been found that the absence of α-crystallin increased cell death during the mitotic phase (Xi et al. 2003). Recent studies have addressed the link between crystallin expression and progression of retinal diseases. The level of αB-crystallin in rd1 mouse retina increased significantly at 15 days postnatal, which correlated with the stage of maximal rod degeneration in this model (Jones et al. 1998; Cavusoglu et al. 2003). Furthermore, an increase of αB-crystallin was also found in various retinal degenerations that varied according to the severity, type, and onset of the degeneration (Organisciak et al. 2006). Oxidative stress could cause alterations in crystallin content as had been observed in the brains afflicted with Alzheimer’s disease (Rogalla et al. 1999; Stege et al. 1999).
Until now, the importance of α-crystallin in optic nerve injury and regeneration has been vaguely attributed only to its antiapoptotic functions. In this study, we have shown that injections of α-crystallin helped to maintain the survival of retinal ganglion cell axons. These findings could indicate that conditions created by administration of α-crystallin or by release of this protein within the eye itself might be instrumental for preventing the loss of significant numbers of injured retinal ganglion cell axons. Furthermore, our data show that the effect of α-crystallin declined by 4 weeks after optic nerve injury. It could be that more axons might continue to survive with multiple applications of α-crystallin. Further study is needed to determine safe methods for sustained intraocular delivery of α-crystallin and other critical molecules, and to develop an understanding of the conditions that prevent disintegration of retinal ganglion cell axons after injury.
References
Alge, C. S., Priglinger, S. G., Neubauer, A. S., et al. (2002). Retinal pigment epithelium is protected against apoptosis by alphaB-crystallin. Investigative Ophthalmology and Visual Science, 43, 3575–3582.
Andley, U. P. (2007). Crystallins in the eye: Function and pathology. Progress in Retinal and Eye Research, 26, 78–98.
Andley, U. P., Song, Z., Wawrousek, E. F., & Bassnett, S. (1998). The molecular chaperone alphaA-crystallin enhances lens epithelial cell growth and resistance to UVA stress. Journal of Biological Chemistry, 273, 31252–31261.
Bai, F., Xi, J., Higashikubo, R., & Andley, U. P. (2004). Cell kinetic status of mouse lens epithelial cells lacking alphaA- and alphaB-crystallin. Molecular and Cellular Biochemistry, 265, 115–122.
Berkelaar, M., Clarke, D. B., Wang, Y. C., Bray, G. M., & Aguayo, A. J. (1994). Axotomy results in delayed death and apoptosis of retinal ganglion cells in adult rats. Journal of Neuroscience, 14, 4368–4374.
Bhat, S. P., Horwitz, J., Srinivasan, A., & Ding, L. (1991). Alpha B-crystallin exists as an independent protein in the heart and in the lens. European Journal of Biochemistry, 202, 775–781.
Carmignoto, G., Maffei, L., Candeo, P., Canella, R., & Comelli, C. (1989). Effect of NGF on the survival of rat retinal ganglion cells following optic nerve section. Journal of Neuroscience, 9, 1263–1272.
Cavusoglu, N., Thierse, D., Mohand-Said, S., et al. (2003). Differential proteomic analysis of the mouse retina: The induction of crystallin proteins by retinal degeneration in the rd1 mouse. Molecular & Cellular Proteomics, 2, 494–505.
Clark, J. I., & Muchowski, P. J. (2000). Small heat-shock proteins and their potential role in human disease. Current Opinion in Structural Biology, 10, 52–59.
Cohen, A., Bray, G. M., & Aguayo, A. J. (1994). Neurotrophin-4/5 (NT-4/5) increases adult rat retinal ganglion cell survival and neurite outgrowth in vitro. Journal of Neurobiology, 25, 953–959.
Cui, Q., & Harvey, A. R. (2000). CNTF promotes the regrowth of retinal ganglion cell axons into murine peripheral nerve grafts. Neuroreport, 11, 3999–4002.
Derham, B. K., & Harding, J. J. (1999). Alpha-crystallin as a molecular chaperone. Progress in Retinal and Eye Research, 18, 463–509.
Fischer, D., Heiduschka, P., & Thanos, S. (2001). Lens-injury-stimulated axonal regeneration throughout the optic pathway of adult rats. Experimental Neurology, 172, 257–272.
Fischer, D., Pavlidis, M., & Thanos, S. (2000). Cataractogenic lens injury prevents traumatic ganglion cell death and promotes axonal regeneration both in vivo and in culture. Investigative Ophthalmology and Visual Science, 41, 3943–3954.
Ge, J., Li, Y., Zhuo, Y., & Guo, Y. (1998). Peripheral nerve and transgene cells transplantation in the treatment of experimental neuropathy of SD rats. Yan Ke Xue Bao., 14, 121–125.
Ghosh, J. G., Estrada, M. R., & Clark, J. I. (2005). Interactive domains for chaperone activity in the small heat shock protein, human alphaB crystallin. Biochemistry, 44, 14854–14869.
Ghosh, J. G., Shenoy, A. K., & Clark, J. I. (2006). N- and C-Terminal motifs in human alphaB crystallin play an important role in the recognition, selection, and solubilization of substrates. Biochemistry, 45, 13847–13854.
Hadani, M., Harel, A., Solomon, A., Belkin, M., Lavie, V., & Schwartz, M. (1984). Substances originating from the optic nerve of neonatal rabbit induce regeneration-associated response in the injured optic nerve of adult rabbit. Proceedings of the National Academy of Sciences of the United States of America, 81, 7965–7969.
Heiduschka, P., Fischer, D., & Thanos, S. (2005). Recovery of visual evoked potentials after regeneration of cut retinal ganglion cell axons within the ascending visual pathway in adult rats. Restorative Neurology and Neuroscience, 23, 303–312.
Horwitz, J. (1992). Alpha-crystallin can function as a molecular chaperone. Proceedings of the National Academy of Sciences of the United States of America, 89, 10449–10453.
Jones, S. E., Jomary, C., Grist, J., Thomas, M. R., & Neal, M. J. (1998). Expression of alphaB-crystallin in a mouse model of inherited retinal degeneration. Neuroreport, 9, 4161–4165.
Kamradt, M. C., Chen, F., & Cryns, V. L. (2001). The small heat shock protein alpha B-crystallin negatively regulates cytochrome c- and caspase-8-dependent activation of caspase-3 by inhibiting its autoproteolytic maturation. Journal of Biological Chemistry, 276, 16059–16063.
Leon, S., Yin, Y., Nguyen, J., Irwin, N., & Benowitz, L. I. (2000). Lens injury stimulates axon regeneration in the mature rat optic nerve. Journal of Neuroscience, 20, 4615–4626.
Liu, X., Hawkes, E., Ishimaru, T., Tran, T., & Sretavan, D. W. (2006). EphB3: an endogenous mediator of adult axonal plasticity and regrowth after CNS injury. Journal of Neuroscience, 26, 3087–3101.
Lorber, B., Berry, M., & Logan, A. (2005). Lens injury stimulates adult mouse retinal ganglion cell axon regeneration via both macrophage- and lens-derived factors. European Journal of Neuroscience, 21, 2029–2034.
Mansour-Robaey, S., Clarke, D. B., Wang, Y. C., Bray, G. M., & Aguayo, A. J. (1994). Effects of ocular injury and administration of brain-derived neurotrophic factor on survival and regrowth of axotomized retinal ganglion cells. Proceedings of the National Academy of Sciences of the United States of America, 91, 1632–1636.
Masilamoni, J. G., Jesudason, E. P., Baben, B., Jebaraj, C. E., Dhandayuthapani, S., & Jayakumar, R. (2006). Molecular chaperone alpha-crystallin prevents detrimental effects of neuroinflammation. Biochimica Et Biophysica Acta, 1762, 284–293.
Mehlen, P., Kretz-Remy, C., Préville, X., & Arrigo, A. P. (1996). Human hsp27, Drosophila hsp27 and human alphaB-crystallin expression-mediated increase in glutathione is essential for the protective activity of these proteins against TNFalpha-induced cell death. EMBO Journal, 15, 2695–2706.
Mey, J., & Thanos, S. (1993). Intravitreal injections of neurotrophic factors support the survival of axotomized retinal ganglion cells in adult rats in vivo. Brain Research, 602, 304–317.
Ohto-Fujita, E., Fujita, Y., & Atomi, Y. (2007). Analysis of the alphaB-crystallin domain responsible for inhibiting tubulin aggregation. Cell Stress and Chaperones, 12, 163–171.
Organisciak, D., Darrow, R., Gu, X., Barsalou, L., & Crabb, J. W. (2006). Genetic, age and light mediated effects on crystallin protein expression in the retina. Photochem Photobiol, 82, 1088–1096.
Parcellier, A., Schmitt, E., Brunet, M., Hammann, A., Solary, E., & Garrido, C. (2005). Small heat shock proteins HSP27 and alphaB-crystallin: Cytoprotective and oncogenic functions. Antioxidants & Redox Signalling, 7, 404–413.
Rabacchi, S. A., Ensini, M., Bonfanti, L., Gravina, A., & Maffei, L. (1994). Nerve growth factor reduces apoptosis of axotomized retinal ganglion cells in the neonatal rat. Neuroscience, 63, 969–973.
Regini, J. W., Grossmann, J. G., Burgio, M. R., et al. (2004). Structural changes in alpha-crystallin and whole eye lens during heating, observed by low-angle X-ray diffraction. Journal of Molecular Biology, 336, 1185–1194.
Rogalla, T., Ehrnsperger, M., Preville, X., et al. (1999). Regulation of Hsp27 oligomerization, chaperone function, and protective activity against oxidative stress/tumor necrosis factor alpha by phosphorylation. Journal of Biological Chemistry, 274, 18947–18956.
Sawai, H., Clarke, D. B., Kittlerova, P., Bray, G. M., & Aguayo, A. J. (1996). Brain-derived neurotrophic factor and neurotrophin-4/5 stimulate growth of axonal branches from regenerating retinal ganglion cells. Journal of Neuroscience, 16, 3887–3894.
Schwartz, M., Belkin, M., & Harel, A. (1985). Regenerating fish optic nerves and a regeneration-like response in injured optic nerves of adult rabbits. Science, 228, 600–603.
Srinivasan, A. N., Nagineni, C. N., & Bhat, S. P. (1992). alpha A-crystallin is expressed in non-ocular tissues. Journal of Biological Chemistry, 267, 23337–23341.
Stege, G. J., Renkawek, K., Overkamp, P. S., et al. (1999). The molecular chaperone alphaB-crystallin enhances amyloid beta neurotoxicity. Biochemical and Biophysical Research Communications, 262, 152–156.
Stupp, T., Pavlidis, M., Busse, H., & Thanos, S. (2005). Lens epithelium supports axonal regeneration of retinal ganglion cells in a coculture model in vitro. Experimental Eye Research, 81, 530–538.
Sun, Y., & MacRae, T. H. (2005). The small heat shock proteins and their role in human disease. FEBS Journal, 272, 2613–2627.
Wong, W. K., Cheung, A. W., & Cho, E. Y. (2006). Lens epithelial cells promote regrowth of retinal ganglion cells in culture and in vivo. Neuroreport, 17, 699–704.
Xi, J. H., Bai, F., & Andley, U. P. (2003). Reduced survival of lens epithelial cells in the alphaA-crystallin-knockout mouse. Journal of Cell Science, 116, 1073–1085.
Yin, Y., Cui, Q., Li, Y., et al. (2003). Macrophage-derived factors stimulate optic nerve regeneration. Journal of Neuroscience, 23, 2284–2293.
Yin, Y., Henzl, M. T., Lorber, B., et al. (2006). Oncomodulin is a macrophage-derived signal for axon regeneration in retinal ganglion cells. Nature Neuroscience, 9, 715–717.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Ying, X., Zhang, J., Wang, Y. et al. α-Crystallin Protected Axons from Optic Nerve Degeneration After Crushing in Rats. J Mol Neurosci 35, 253–258 (2008). https://doi.org/10.1007/s12031-007-9010-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12031-007-9010-1