Abstract
Purpose
Primary leiomyosarcoma of the pancreas (PLMSP) is rare. The clinical features and outcomes are still unclear. The present study aims to identify the clinical features, outcomes, and racial differences of PLMSP.
Methods
PLMSP cases reported in Chinese, English, French, and Japanese journals were collected and reviewed. Data from these reports were summarized and analyzed statistically.
Results
In addition to a female patient presented to our department with PLMS, a total of 87 cases reported in the literature were included in the present study. An equal incidence in gender was observed. The mean age was 53.8 years. Common symptoms were abdominal pain and abdominal mass. At the time of diagnosis or after a period of follow-up, 37.5% of patients had distant metastasis and 31.8% of patients had regional organs/vessels invasion. The 5-year mortality rate was 77.8%. The presence of distant metastasis and the absence of radical surgery are significantly associated with poor outcomes. Regional invasion was significantly more common in East Asians.
Conclusion
PLMSP is an aggressive tumor with a poor prognosis. Radical resection can decrease the mortality of the patients. Early detection of such tumor is recommended.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pancreatic cancer is currently estimated as the seventh leading cause of cancer-related deaths in both sexes worldwide [1]. Primary pancreatic tumors are usually of epithelial origin, among which the ductal adenocarcinomas are the most common representing 90% of all pancreatic tumors. However, mesenchymal tumors are rare and account for 1–2% of all pancreatic tumors. They can be derived from the connective fibromuscular, lymphatic, vascular, and neuronal tissues of the pancreas [2,3,4].
Leiomyosarcoma is a mesenchymal malignant tumor composed of cells showing distinct smooth muscle features [5]. Primary pancreatic leiomyosarcoma (PLMSP) is extremely rare and has seldom been reported in the literature. According to the World Health Organization (WHO) classification of soft tumors, the most common location of soft tissue leiomyosarcoma is the retroperitoneum, including the pelvis [5]. However, pancreatic leiomyosarcoma is not mentioned in the WHO classification of tumors of the digestive system except for one sentence because of its uncommonness [2]. In 2014, Kim et al. published an article about their 16-year experience with pancreatic tumors and showed only 1 case of leiomyosarcoma out of 7129 pancreatic specimens [6]. Nevertheless, the first report of PLMSP was by Ross in 1951 [7].
In this article, we presented a case of leiomyosarcoma in a 65-year-old female and described the main clinical features along with the management protocol in this condition. In addition, we comprehensively reviewed all reported cases in literature since 1951 until now and statistically analyzed the available patient characteristics and clinical information related to this condition in order to reveal any significant association with the incidence and prognosis of this type of tumor.
Methods
Case Presentation
A 65-year-old female known to have type II diabetes mellitus and hypertension presented to the hospital with a discomfort and abdominal mass that was increasing in size over the past 4 months. She denied having abdominal pain, dysphagia, heartburn, nausea, vomiting, constipation, or bloody stool. She also declared neither loss of appetite nor noticeable weight loss. The patient was a non-smoker and did not have a family history of any kind of malignancies.
On examination, abdominal distention with a large mass appeared to occupy the left upper quadrant. The mass was irregular in shape, hard, immobile, and non-tender, with no overlying skin changes. The mass seemed to disappear when asking the patient to contract her abdominal muscles. There was no visible jaundice, and the per-rectal examination was free of any findings.
Laboratory investigations revealed an elevation in carcinoembryonic antigen to 4.2 ng/ml and an increased erythrocyte sedimentation rate of 37 mm/h. However, the liver function test, kidney function test, complete blood count, and urine analysis were within normal levels.
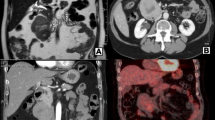
Ultrasound examination showed an irregular mass measuring 7 × 8 cm that was arising from the left colon flexure. The patient underwent colonoscopy that showed a normal mucosa with no masses arising from the colon. A CT with IV and oral contrast scan was performed and showed a large, lobulated, poorly enhancing mass that is inseparable from the body and tail of the pancreas (Fig. 1). Magnetic resonance cholangiopancreatography was additionally implemented and revealed a lobulated mass at the vicinity of the body and tail of the pancreas. No filling defect was identified within the intra- or extra-hepatic biliary system.
The decision was made to completely remove the tumor due to its enormous size followed by histopathological studies. The distal pancreatectomy with splenectomy was accomplished successfully. The mass was nodular weighing about 550 g and measuring 15 × 12 × 6 cm. The cut surface was gray-white with areas of hemorrhage and no grossly evident necrosis.
Histopathological sections from the mass revealed a spindle cell tumor confined to the pancreatic capsule and lie approximately 5.0 mm from the pancreatic parenchymal margin. The tumor cells displayed abundant eosinophilic cytoplasm and cigar-shaped nuclei. Prominent nuclear atypia and frequent mitotic figures (39/10 HPF) were also identified as microscopic foci of abrupt tumor necrosis. Immunohistochemical labeling revealed that the tumor cells were strongly and diffusely expressing smooth muscle actin (SMA) and desmin. However, they were negative for CD34, myogenin, c-kit, creatine kinase, and epithelial membrane antigen (EMA). No lymphovascular invasion was identified. A diagnosis of grade two PLMSP was established.
Follow-up after one year, the patient was in good condition with no signs of local recurrence or metastasis of the tumor on the CT scan (Fig. 2).
Method of Review
A systematic literature search was applied via MEDLINE and EMBASE for cases reported in English-language journals. A similar search was made in the China Knowledge Resource Integrated (CNKI) database to identify the reported cases in Chinese journals. “Encyclopédie Médico Chirurgicale” (EMC) and uOttawa Library were used to reach reports in the French language. Google Translator aided in the translation process. The primary key words used were “leiomyosarcoma,” “pancreas and leiomyosarcoma,” and “pancreatic sarcoma.” Only cases originated from the pancreas were included in the study. Clinical features and long-term outcomes of these cases were summarized and analyzed using proper statistical methods. The complete summary of all cases is provided in the supplementary table (Suppl. 1).
Statistics
The data were presented as frequency distributions for categorical variables and mean ± standard error of the mean (SE) for continuous variables. The data was tested at a significance level of 0.05%. The Pearson χ2 test was used to investigate the significance of the association between categorical variables, while Student’s t test was applied to examine the significance level for continuous variables. The logistic regression model, including all factors, was performed to reveal the significant factors that contribute mostly to the 5-year mortality rate and their odds ratios.
Results
Demographics
We were able to retrieve 87 cases of pancreatic leiomyosarcoma from the literature since its first description in 1951. These included 21 cases reported in Chinese literature, three in Japanese, four in French, and 59 in the English literatures. Including our case, we had a total of 88 cases of PLMSP.
The patient demographics and the clinical features of the PLMSP are summarized in Table 1. The mean age of the patients with PLMSP was 53.8 years, the youngest patient was 14 years old and the oldest was 87 years old. The main clinical features (signs and symptoms) were found to be abdominal pain, abdominal mass, constitutional symptoms, nausea/vomiting, and obstructive jaundice. Other minor symptoms included melena, hematemesis, and hemoptysis. In addition, few cases were incidentally diagnosed.
The tumor size ranged from 1 to 30 cm, with an average of 11.2 cm. About one-third (31.8%) of the cases reported local invasion to adjacent organs or blood vessels. The distant metastasis was reported in 37.5% of the cases at the time of diagnosis or after a period of follow-up. Lymph node involvement was reported in one case only. The liver was the most common organ to be involved in distant metastasis (Table 1). The radical surgical treatment was reported in more than half of the cases (60.2%) and included the Whipple operation, distal pancreatectomy, or complete local excision.
Outcome
Mortality rate (MR) was used as the prognostic tool to measure the outcome. The MR was measured at 1 year, 5 years, and 10 years after the diagnosis. The MR at 1, 5, and 10 years was 36.5%, 77.8%, and 85.7%, respectively. Statistical analysis showed that the presence of distant metastasis (P < 0.01) and the absence of radical surgical treatment (P < 0.05) were the significantly associated factors with the poor outcome (Table 2). Almost two-thirds (64.3%) of patients who died within 5 years after diagnosis were among those who did not undergo radical surgery. In addition, patients with distant metastasis accounted for 64.3% of patients who died within 5 years. Furthermore, after controlling all factors involved in the study, the logistic regression analysis revealed that patients with distant metastasis were at 5-fold (P < 0.01) increased risk of mortality within a period of 5 years compared with patients without distant metastasis.
Racial Differences
We classified the reported cases into East Asian and non-East Asian groups. The East Asian group encompassed the cases of Chinese, Japanese, and South Korean origins and accounted for 36 (40.9%) cases. Non-East Asian group included the remaining cases and accounted for 52 (59.1%) cases. The statistical analysis showed a significant association between the East Asian group and the presence of regional invasion when compared with the non-East Asian group. No other racial differences were detected (Table 3).
Discussion
To the best of our knowledge, this is the most updated study that comprehensively reviewed all reported cases in the literature about the PLMSP. It aimed to investigate the demographic distribution and the major risk and prognostic factors associated with this neoplasm. The study showed that distant metastasis of this tumor is the most important prognostic factor which was positively associated with the 5-year mortality rate. However, radical surgery was the treatment of choice to increase survival and prevent a recurrence. In addition, the study revealed for the first time the high prevalence of this type of tumor in the East Asian ethnicity. It also showed a high incidence of regional invasion, as a complication of this tumor, in the East Asian race compared with other races.
It is impossible to diagnose PLMSP depending on the clinical presentation and imaging only. For example, it usually appears as a heterogeneous-enhancing lesion under CT [8,9,10,11,12]. However, the mass appeared as a poorly enhanced hypo-attenuated lesion in our case. Accordingly, histopathology with immunohistochemical investigations is mandatory for a confirmed diagnosis [9, 12, 13]. The PLMSP appears histopathologically as intersecting groups of spindle cells. The nuclei of the tumor cells are characteristically elongated and blunt-ended [5]. However, this histopathological picture also raises the suspicion of other differential diagnoses like liposarcoma, inflammatory myofibroblastic tumor, fibrosarcoma, rhabdomyosarcoma, malignant fibrous histiocytoma, and gastrointestinal stromal tumor [5]. Immunohistochemical labeling plays the critical role in distinguishing leiomyosarcoma from other tumor types. The most common labeling antigens in myogenic-origin tumors including leiomyosarcoma are desmin and SMA [11].
The tumor underwent cystic degeneration in 32 (36.4%) cases. These cystic changes should not be mistaken with other pathologies such as pseudocyst [11, 14] or cystadenocarcinoma [11, 15]. It is important to exclude the secondary involvement of the pancreas by leiomyosarcoma from the adjacent organ or distant metastasis. Leiomyosarcoma originating from the stomach, duodenum, inferior vena cava, and retroperitoneum can invade the pancreas and appears as PLMSP [16,17,18,19]. Also, the pancreas can be involved from distant places such as the uterus and the thigh tissue [20,21,22]. In order to differentiate secondary from PLMSP, a radiological and/or histological study should be obtained [6]. It is considered secondary when the center of the mass is located in the peripancreatic soft tissue, or when multiple lesions existed radiologically [6].
The PLMSP has a high tendency to metastasize hematologically as well known for the sarcomas [23]. In fact, distant metastasis was the most important factor to affect the mortality rate. Patients with distant metastasis are five times more likely to die of the disease within a period of 5 years compared with patients without distant metastasis. In all cancer types, the presence of distant metastasis promotes the cancer into its final stages, as the neoplasm is becoming no more controllable [23]. Therefore, early detection and treatment are considered the main crucial factors in the management of these malignancies.
The treatment modality for PLMSP is mainly by radical resection of the tumor. This is achieved by either pancreaticoduodenectomy, if the tumor is in the head of the pancreas, or distal pancreatectomy, with or without splenectomy, for tumors in the body or tail of the pancreas. Adjuvant chemotherapy is of unknown significance regarding the prognosis [12,13,14, 24]. Another surgical modality is the local excision which was reported in two cases only. In these two cases, the safe margins were negative macroscopically and microscopically [10, 11]. In cases of non-resected tumor, palliative chemotherapy as doxorubicin-based chemotherapy or palliative surgical options as gastrostomy were the choices [25, 26]. Nevertheless, the only treatment procedure that affects the outcome was the radical surgery. Radical surgery is, also, the mainstay treatment in other types of pancreatic cancer as ductal adenocarcinoma [26]. This is because, from a theoretical point of view, more extended surgery in cases of pancreatic cancer might improve long-term survival rates in cases where no tumor is left behind. However, the drawback is that not every patient is a candidate for this type of surgery. Two main factors are limiting the utilization of this method: the status of the patients and the degree of the tumor [25]. When the patient is unfit for surgery due to a chronic medical illness, or when the tumor is distantly metastasizing, the patient is no longer a candidate for such surgery.
It seems that PLMSP has a higher tendency to occur in the East Asian race, as East Asian patients attributed to about 41% of the reported cases. In addition, the tumor showed a higher trend of regional invasion in the East Asians compared with the other ethnicities. Certain malignancies are well known to occur more frequently in the Asian ethnicity such as gastric cancer [27]. This variation could be attributed to either genetic susceptibility or environmental factors.
In conclusion, PLMSP is a rare but grievous type of tumor, which is associated with a high rate of mortality. The most critical factor associated with this high mortality is the distant metastasis. However, the radical surgical modality was found to be the most important prognostic factor in this tumor. Our review of the literature revealed the high incidence in reported cases of this tumor in the East Asian population. Interestingly, the regional invasion of the tumor was disclosed to be the most common complication scenario in the East Asian reported cases. More studies about PLMSP and its genetic and racial correlations are required to reveal a more conclusive picture.
References
Bosman FT, Carneiro F, Hruban RH, Theise ND. WHO classificiation of tumours of the digestive system. 4th editiom. Lyon: IARC Press; 2010.
Kloppel G, Maillet B. Classification and staging of pancreatic nonendocrine tumors. Radiol Clin N Am. 1989;27:105–19.
Ferrozzi F, Zuccoli G, Bova D, Calculli L. Mesenchymal tumors of the pancreas: CT findings. J Comput Assist Tomogr. 2000;24:622–7.
Fletcher CDM. WHO classification of tumours of soft tissue and bone. Lyon: IARC Press; 2013.
Kim JY, Song JS, Park H, et al. Primary mesenchymal tumors of the pancreas: single-center experience over 16 years. Pancreas. 2014;43:959–68.
Baylor SM, Berg JW. Cross classification and survival characteristics of 5000 cases of cancer of the pancreas. J Surg Oncol. 1973;5:335–58.
Ross CF. Leiomyosarcoma of the pancreas. Br J Surg. 1951;39:53–6.
Reyes MC, Huang X, Bain A, Ylagan L. Primary pancreatic leiomyosarcoma with metastasis to the liver diagnosed by endoscopic ultrasound-guided fine needle aspiration and fine needle biopsy: a case report and review of literature. Diagn Cytopathol. 2016;44:1070–3.
Kocakoc E, Havan N, Bilgin M, Atay M. Primary pancreatic leiomyosarcoma. Iran J Radiol. 2014;11:e4880.
Aihara H, Kawamura YJ, Toyama N, Mori Y, Konishi F, Yamada S. A small leiomyosarcoma of the pancreas treated by local excision. HPB (Oxford). 2002;4:145–8.
Milanetto AC, Liço V, Blandamura S, Pasquali C. Primary leiomyosarcoma of the pancreas: report of a case treated by local excision and review of the literature. Surg Case Rep. 2015;1:98.
Hur YH, Kim HH, Park EK, et al. Primary leiomyosarcoma of the pancreas. J Korean Surg Soc. 2011;81(suppl 1):S69–73.
Makimoto S, Hatano K, Kataoka N, Yamaguchi T, Tomita M, Nishino E. A case report of primary pancreatic leiomyosarcoma requiring six additional resections for recurrences. Int J Surg Case Rep. 2017;41:272–6.
Sato T, Asanuma Y, Nanjo H, Arakawa A, Kusano T, Koyama K, et al. A resected case of giant leiomyosarcoma of the pancreas. J Gastroenterol. 1994;29:223–7.
Ishikawa O, Matsui Y, Aoki Y, Iwanaga T, Terasawa T, Wada A. Leiomyosarcoma of the pancreas. Report of a case and review of the literature. Am J Surg Pathol. 1981;5:597–602.
Nordback I, Mattila J, Tarkka M. Resectable leiomyosarcoma of inferior vena cava presenting as carcinoma of the pancreas. Case report. Acta Chir Scand. 1990;156:577–80.
Biswas S, Amin A, Chaudry S, Joseph S. Leiomyosarcoma of the inferior vena cava - radical resection, vascular reconstruction and challenges: a case report and review of relevant literature. World J Oncol. 2013;4:107–13.
Stauffer JA, Fakhre GP, Dougherty MK, Nakhleh RE, Maples WJ, Nguyen JH. Pancreatic and multiorgan resection with inferior vena cava reconstruction for retroperitoneal leiomyosarcoma. World J Surg Oncol. 2009;7:3.
Olurin EO, Solanke TF. Case of leiomyosarcoma of the duodenum and a review of the literature. Gut. 1986;9:672–7.
Burke JP, Maguire D, Dillon J, Moriarty M, O’Toole GC. Whipple’s procedure for an oligometastasis to the pancreas from a leiomyosarcoma of the thigh. Ir J Med Sci. 2012;181:361–3.
Ozturk S, Unver M, Ozturk BK, et al. Isolated metastasis of uterine leiomyosarcoma to the pancreas: report of a case and review of the literature. Int J Surg Case Rep. 2014;5:350–3.
Ogura T, Masuda D, Kurisu Y, et al. Multiple metastatic leiomyosarcoma of the pancreas: a first case report and review of the literature. Intern Med. 2013;52:561–6.
Kumar V, Abbas AK, Fausto N, Mitchell RN. Robbins basic pathology. 8th ed: SaundersElseevier; 2007.
ESMO/European Sarcoma NetworkWorking Group. Soft tissue and visceral sarcomas: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2014;25(Suppl 3):iii102–12.
Birk D, Beger HG. Pancreatic cancer. In: Holzheimer RG, Mannick JA, editors. Surgical treatment: evidence-based and problem-oriented. Munich: Zuckschwerdt; 2001.
Rahman R, Asombang AW, Ibdah JA. Characteristics of gastric cancer in Asia. World J Gastroenterol. 2014;20:4483–90.
Izumi H, Okada K, Imaizumi T, et al. Leiomyosarcoma of the pancreas: report of a case. Surg Today. 2011;41:1556–61.
Acknowledgments
The authors are grateful to Dr. Faisal Kanaan for his efforts in the histopathological study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
There are no conflicts of interest to declare.
Informed Consent
Written informed consent was obtained from the patient for publication. No institutional approval was required.
Additional information
This article has not been published or presented elsewhere in part or in entirely and is not under consideration by another journal.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 33 kb)
Rights and permissions
About this article
Cite this article
Aleshawi, A.J., Allouh, M.Z., Heis, F.H. et al. Primary Leiomyosarcoma of the Pancreas: a Comprehensive Analytical Review. J Gastrointest Canc 51, 433–438 (2020). https://doi.org/10.1007/s12029-019-00282-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12029-019-00282-1