Abstract
Background
Spontaneous intracerebral hemorrhage is a disease with high morbidity and mortality. Extension of the hemorrhage into the ventricles is associated with the development of acute hydrocephalus and a poor outcome. Although it can be managed by external ventricular drainage (EVD), a subset of these patients require placement of permanent ventricular shunts. This study aimed to examine the factors on admission that can predict shunt dependency after EVD management.
Methods
Seventy-two patients who underwent EVD were included in this study. Seventeen of these patients underwent placement of a ventriculoperitoneal shunt. Variables analyzed included age, intraventricular hemorrhage (IVH) score, bicaudate index, acute hydrocephalus, initial Glasgow Coma Scale scores, and blood volume in each ventricle.
Results
In univariate analysis, IVH score (p = 0.020), bicaudate index (p < 0.001), blood volume in lateral ventricles (p = 0.025), blood volume in the fourth ventricle (p = 0.038), and the ratio of blood volume in lateral ventricles to that in third and fourth ventricles (p = 0.003) were significantly associated with persistent hydrocephalus. The best multiple logistic regression model included blood volume parameters and bicaudate index as predictors with the area under a receiver operating characteristic curve of 0.849. The variance inflation factor (VIF) showed that collinearity was not found among predictors. Patients diagnosed with acute hydrocephalus had less blood volume in the lateral ventricles (OR = 0.910) and had more blood volume in the third ventricle (OR = 3.174) and fourth ventricle (OR = 2.126).
Conclusions
These findings may promote more aggressive monitoring and earlier interventions for persistent hydrocephalus after intraventricular hemorrhage in patients at risk.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Spontaneous intracerebral hemorrhage (sICH) is a disease with high morbidity and mortality, accounting for 10–15% of all strokes [1]. Intraventricular hemorrhage (IVH) occurs in approximately 30–50% of patients with sICH and carries a 30-day mortality rate of 43–68% [2, 3]. Additionally, IVH is associated with the development of acute hydrocephalus and a poor outcome [4, 5]. In fact, acute hydrocephalus is an independent predictor of 30-day mortality in sICH patients [6]. Location of the parenchymal origin of ICH, distribution of ventricular blood, and IVH volumes predict outcomes in patients with spontaneous ICH and intraventricular extension [6, 7].
External ventricular drainage (EVD) is a procedure commonly used as a life-saving measure to manage intracranial pressure and acute hydrocephalus in patients with IVH, which potentially reduces short-term mortality [8, 9]. IVH is sometimes responsible for the subsequent development of hydrocephalus, which requires permanent cerebrospinal fluid (CSF) diversion by placement of a ventriculoperitoneal (VP) shunt during follow-up, even with intraventricular clot resolution. The incidence of hydrocephalus in EVD-treated IVH with sICH is lower than that in patients with aneurysmal subarachnoid hemorrhage [10,11,12]. When persistent hydrocephalus develops without early detection and management, it presents as a deteriorating mental status or other neurological symptoms.
In daily practice, an evidence-based protocol for selecting patients who might benefit from VPS placement is lacking. Prolonged EVD drainage increases the risks of infection, length of hospital stays, and costs, but VPS placement is associated with the risks of shunt obstruction, malpositioning, and infection. It is important to identify the patients who are likely to benefit from shunt placement and to avoid unnecessary shunt surgeries. The aim of this single-center, retrospective analysis was to examine specific factors on admission and construct models that can predict shunt dependency in patients with sICH and IVH who underwent EVD.
Methods
Patients
The population consisted of consecutive patients admitted to the neurosurgical intensive care unit, who underwent surgery for EVD insertion with a diagnosis of sICH with IVH, at the National Taiwan University Hospital, Yun-Lin Branch. Inclusion criteria were: (1) age ≥ 18; (2) spontaneous primary IVH with supratentorial origin or spontaneous intracerebral hemorrhage with extension into ventricles; (3) admittance to Emergency Services within 12 h after onset and EVD performed. Patients with brainstem hemorrhage, cerebellar hemorrhage, intracranial aneurysm, or arteriovenous malformation complicated with hemorrhage were excluded. Patients with a history of preexisting brain diseases such as brain tumor, stroke, meningitis, or substance abuse were excluded. During the entire hospital stay, CSF infection or radiographic IVH growth after EVD placement were also excluded. Patients with a plan for palliative care or those who did not survive to discharge after EVD placement were excluded, as were patients who underwent endoscopic hematoma evacuation or intraventricular fibrinolysis using urokinase or tPA. This study was approved by National Taiwan University Hospital’s Institutional Review Board. Informed consent was specifically waived because this was a retrospective study in which patients’ information was de-identified before analysis by the researchers. On admission, patients’ Glasgow Coma Scale (GCS) scores were evaluated by emergency physicians. Patients were managed according to the current ICH guidelines by the American Heart Association and the American Stroke Association. All patients received initial imaging diagnostics of cerebral computed tomography (CT) scans with 5-mm slices. Demographic information collected at admission included age and sex. Head CT imaging at admission was used for assessment of radiographic characteristics including ICH location and IVH volume in each of the ventricles, and for calculation of IVH scores and the bicaudate index for hydrocephalus assessment [13]. The bicaudate index was considered abnormal if it was above the age-adjusted 95th percentile [14]. Location of ICH was classified into categories of thalamic and other supratentorial locations. In the presence of acute or impending hydrocephalus combined with neurological deterioration, EVD catheters were placed. The EVD insertion was preferentially performed at the Kocher point on the right side, unless there were relative contraindications such as hematoma in the planned path of the EVD or a completely blood-filled right lateral ventricle. Ventricular catheters are tunneled some distance from the insertion site to prevent infection. Intracranial pressure (ICP) was recorded hourly, and prophylactic antibiotics were used intravenously for the period that the EVD catheter remained in place.
External Ventricular Drain Challenge Protocol
After EVD catheter insertion, the drain is kept open at 10 cm above the external auditory canal (EAC), unless the patient fails to improve clinically with persistent dilation of the ventricular system. Weaning from the EVD was performed based on the patient’s neurological status, radiographic criteria including ventricular size and resolution of IVH, and daily CSF output. The EVD challenge was initiated 7–14 days after the first surgery, when there is no diagnosed CSF infection and no evidence of hydrocephalus. After a CT scan to confirm the absence of new bleeding, the EVD level above the EAC was adjusted to 15 cm. When the daily CSF drainage was less than 100 ml, the drain was clamped. ICP was monitored continuously, and the neurological status of the patient was checked hourly for 24 h. The EVD challenge test was considered unsuccessful if patients presented with a decline in the level of consciousness, sustained ICP > 20 mmHg for at least 1 h, CSF leakage from the incision site, or increased ventricular size after clamping the drain. When the challenge was passed, the EVD catheter was removed. When patients could not pass the challenge test, they received a VPS. For the patients who passed the EVD challenge test, either another routine CT scan was performed 30 days after the EVD insertion or additional imaging studies were conducted at a later point if new symptoms occurred. If chronic hydrocephalus was diagnosed, a VPS was implanted.
Clinical and Radiographic Variables
In this study, the variables reviewed as potential factors associated with shunt dependency were: (1) demographics including age and sex; (2) laboratory data including blood glucose level, platelet count, and white blood cell count, with samples collected from emergency room and intensive care unit admission; (3) history of hypertension and diabetes mellitus; (4) GCS scores, IVH scores, and the presence of hydrocephalus. Admission CT scans performed within 12 h of onset were reviewed for IVH location and volume. Hemorrhage severity was assessed by determining the IVH scores according to the previously published criteria [13].
IVH Volume Measurement
IVH volume was extracted from CT images using our semiautomated segmentation tool, which was developed in MATLAB using Otsu’s method, an automatic clustering-based image thresholding process [15,16,17]. The Otsu thresholding scheme searches for an optimal threshold to reduce a gray level image to a binary image. The optimal threshold is determined by maximizing the separability between target and background classes. The measure of IVH volume starts with a selection of a reader-defined region of interest (Fig. 1). The area of the hemorrhage was calculated automatically in square centimeters for the selected region, and the volume of the region of interest was calculated by multiplying the slice thickness (5 mm) by the area. The volumes from a stack of CT slices were summed for a given section. Because the hemorrhage of a specific ventricle usually includes more than one section, the region of interest volume for each section was summed to obtain the volume of blood in each ventricle.
Image Processing and Reliability
Assessment of IVH volumes was performed independently by two investigators blinded to the radiologists’ reports and clinical outcomes. Using our assessment tool, IVH volume was automatically measured by the investigator selecting regions of interest around each section of intraventricular blood in every slice and in the lateral, third, and fourth ventricles separately. Through a pilot process, inter-reader reliability between the investigators was evaluated to test whether the volume was identified accurately. A comprehensive assessment process was then performed, and a session with the two investigators was called to work on discrepant ventricular volume to minimize bias.
Functional Outcome Assessment
The functional outcomes were recorded using the modified Rankin Scale score (mRS). Follow-up mRS scores at 3 months after IVH were determined by trained study staffs using standardized telephone interviews. A good outcome was defined as a mRs score of 0–2, and a poor outcome was defined as a mRS score of ≥ 3.
Statistical Analysis
In the descriptive analysis, numerical variables were presented as mean, median, standard deviation, and interquartile range. Categorical variables were presented in numbers and percentages. All patients were grouped into shunt dependency and no shunt dependency groups. Normally and non-normally distributed numerical variables were analyzed with a two-sided Student’s t test and Mann–Whitney U test, respectively. Significant associations between categorical variables were analyzed by cross-table statistics (Chi-square or Fisher’s exact test). Intra-class correlation (ICC) coefficients were used to verify the inter-rater reliability of the IVH volume assessment and yield a value between 0 and 1, where a value of one represents a perfect agreement between investigators and zero means no agreement [18, 19]. The discrimination ability was determined by performing ROC analysis to assess sensitivity, specificity, Younden Index, and AUROC (area under ROC curve). The Youden Index is the optimal measure at which the combination of sensitivity and specificity is maximal [20]. The AUROC, measuring a prediction model’s discriminative utility, is commonly used for classification of dichotomous outcomes in single diagnostic and imaging tests [21]. Its value is assessed at all cutoff points and is considered excellent for values between 0.9 and 1, good for values between 0.8 and 0.9, fair for values between 0.7 and 0.8, and poor for values less than 0.7 [22, 23]. Calibration ability was determined by using the Hosmer–Lemeshow goodness of fit test, and the plot of observed versus predicted VPS dependency. Univariate and multivariate logistic regression analyses were performed to identify the independent predictors of VPS dependency after stroke. Variance inflation factor (VIF) was calculated to estimate multicollinearity for each predictor. A predictor of VIF > 10 was considered as an indicative of serious collinearity and excluded from the logistic regression model. All tests were performed with two tails, with statistical significance at an α level of 0.05.
Results
During the study period, 108 consecutive patients underwent surgery for EVD insertion with a diagnosis of sICH with IVH. Five patients were excluded from our analysis due to incomplete data. Twenty-one patients were excluded due to the diagnosis of hematoma expansion at 24 h, which is defined as an increase in hematoma volume of > 33% or an absolute increase of hematoma volume of > 10 ml. Two patients with CSF infection after EVD placement and 8 patients who underwent endoscopic hematoma evacuation or intraventricular fibrinolysis using urokinase or tissue plasminogen activator (tPA) were also excluded. The baseline demographic and admission clinic variables of the 72 patients enrolled are outlined in Table 1. Hemorrhagic lesions were present in the thalamus, putamen, and other locations in 82.0, 12.4, and 5.6% of patients, respectively. The mean period of external ventricular drainage before VP shunt placement was 16.1 days (range 8–36 days). In the shunt dependency group, poor outcomes (mRS score ≥ 3) were noted in 14 patients (82.3%) at 3 months after IVH. In patients without shunt dependency, 42 (76.4%) had poor outcomes. There was no significant difference in terms of the functional outcomes between these two study groups.
Radiographic Characteristics
The mean IVH scores were 13.1 in all patients. Of patients included, 68.1% were diagnosed with acute hydrocephalus using radiographic evidence by neurosurgeons, and 22 (30.6%) patients had an abnormal bicaudate index. ICC (3, 1) was used to verify inter-rater reliability, where each CT image was measured by two investigators [18, 19]. The ICC (3, 1) coefficients for the blood volume in the lateral, third, and fourth ventricles were 0.97, 0.93, and 0.95, respectively (Table 2), demonstrating excellent reliability among investigators. The mean IVH volumes were 8.1, 0.75, and 1.1 mm3 in the lateral, third, and fourth ventricles, respectively. The mean natural logarithm of the ratio of blood volume in lateral ventricles to the blood volume in third and fourth ventricles was 2.1, which was calculated for predictive purposes.
Univariate Analysis
Overall, 17 patients (23.6%) required shunt placement after removal of the EVD catheter (Table 1). The age, sex proportion, and GCS scores on arrival to the hospital were not statistically significant between patients without and with VPS placement. Patients in the shunt dependency group had significantly higher IVH scores (15.7 vs. 12.4) and a greater proportion of abnormal bicaudate index (64.7 vs. 20.0%) than the patients without shunt dependency. Some parameters of blood volume analysis in the ventricles were significantly associated with shunt dependency in the univariate analysis, including blood volume in lateral ventricles (p = 0.025), blood volume in fourth ventricle (p = 0.038), and the ratio of blood volume in lateral ventricles to blood volume in third and fourth ventricles (p = 0.003). The total volume of blood volume in all ventricles was not associated with shunt dependency.
Prediction of VPS Dependency
To predict the dependency on VPS after IVH, we constructed three multiple logistic regression models to compare their prediction ability between the predictors of IVH score and IVH volume (Table 3). The first model included IVH score and bicaudate index, while the second model included the blood volume in the lateral, third, and fourth ventricles, as well as a bicaudate index. The third model included blood volume in the third and fourth ventricles, the ratio of blood volume in the lateral ventricles to the sum of blood volume in the third and fourth ventricles, and bicaudate index. Since other clinical variables such as age, sex, or GCS score were not found to be significant for shunt placement in our univariate analysis, and additionally have not been reported to be associated with shunt dependency in prior studies, those variables were not included in our prediction models. The average VIFs were 1.29 for bicaudate index (max = 1.31), 1.73 for IVH score (max = 1.90), 1.80 for lateral IVH (max = 2.11), 1.73 for 3rd IVH (max = 1.85), 1.78 for 4th IVH (max = 1.90), and 2.25 for lateral IVH/(3rd IVH + 4th IVH) (max = 2.70). The VIFs suggested that collinearity was not found among predictors. The Hosmer–Lemeshow goodness of fit test suggested that three prediction models had good calibrations, where Cox and Snell R2 were 0.178, 0.235, and 0.241, and Nagelkerke R2 were 0.276, 0.360, and 0.374 for the first, second, and third models, respectively (Table 3). Three prediction models also showed excellent discrimination performances. The values of the AUROC were 0.808, 0.843, and 0.849 for the first, second, and third models, respectively. The sensitivity, specificity, and Youden index for each model are listed in Table 3. The values of R2, sensitivity, Younden index, and AUROC were notably increased through the first model to the second and third ones. The results are noteworthy in that the second and third models using IVH volume as predictors were superior in terms of calibration and discrimination indicators to the first one, using IVH score and bicaudate index to predict shunt dependency.
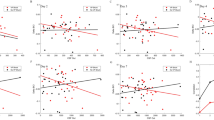
IVH Volume Associated with Acute Hydrocephalus and IVH Score
The multivariate logistic regression analysis using IVH volume in ventricles as a dependent variable, and acute hydrocephalus (yes/no) as an independent variable, demonstrating that the blood volume in individual ventricles was significantly associated with acute hydrocephalus (Table 4). The odds ratios indicated that patients diagnosed with acute hydrocephalus had less blood volume in the lateral ventricles (OR = 0.910) and had more blood volume in the third ventricle (OR = 3.174) and fourth ventricle (OR = 2.126). There were significant positive correlations between IVH score and IVH volume in the lateral ventricles (γ = 0.651), third ventricle (γ = 0.396), and fourth ventricle (γ = 0.451).
Discussion
The primary findings of this study are that IVH scores, bicaudate index, blood volume in the lateral ventricles and the fourth ventricle, and the ratio of blood volume in the lateral ventricles to that in the third and fourth ventricles are associated with permanent shunt dependency after EVD catheter placement in patients with IVH. This study is the first to calculate the blood volume in each ventricle and analyze the predictive value of blood distribution in addition to the total volume of intraventricular hemorrhage. Herrick et al. concluded that EVD catheter placement in patients with spontaneous IVH is an independent predictor of reduced mortality and improved functional status at discharge [24]. In the current study, 17 (23.6%) of these patients had a permanent VP shunt placed after termination of EVD. Generally, the incidence of chronic hydrocephalus in patients with IVH is reported to be lower than that in patients with aneurysmal subarachnoid hemorrhage [11, 12, 25].
In the univariate analysis, IVH score, bicaudate index, blood volume in the lateral ventricles, the fourth ventricle, and the third and fourth ventricles, and ratio of blood volume in the lateral ventricles to that in the third and fourth ventricles were significantly associated with shunt dependency after EVD placement. We excluded those patients who underwent head CT studies more than 12 h since the onset of symptoms, given the time-dependent characteristics of the development of acute hydrocephalus. We also excluded IVH with infratentorial origin or aneurysm rupture, which may lead to acute and chronic hydrocephalus under different mechanism from supratentorial IVH. In this study, 82% of patients had thalamic ICH, which has been demonstrated to be an independent predictor of shunt dependency [26]. In previous studies, predictors of shunt dependency also included elevated ICP after EVD catheter placement [26, 27]. We found no association between shunt dependency with admission neurological status, age, or sex, consistent with prior investigations [26, 28]. We also excluded patients who underwent intraventricular fibrinolysis (IVF) using urokinase or tPA or endoscopy-assisted surgery to help intraventricular blood removal, since the effects of these procedures on chronic hydrocephalus were previously found to be inconclusive. None of our patients received lumbar drainage during any time of the treatment. A recent randomized controlled trial demonstrated that in patients with supratentorial ICH and severe IVH, the combined IVF with lumbar drainage, as compared to IVF alone, significantly reduced the rates of permanent shunt dependency [29]. This treatment focuses on the rapid removal of the IVH and clot-breakdown products over the spinal subarachnoid space.
Herrick et al. (2014) showed that a larger total IVH volume predicted higher mortality in patients with acute hydrocephalus, but the value of blood distribution in the ventricles was not analyzed [24]. Zacharia et al. found no association between total IVH volume and the development of shunt-dependent hydrocephalus [26]. In our study, we concluded that the blood distribution in ventricles is a significant predictor for shunt dependency. However, the total IVH volume in four ventricles was not associated with the development of chronic hydrocephalus.
Acute hydrocephalus was not shown to be a significant predictor of shunt dependency in either the univariate analysis or multivariate analysis in our study, which was consistent with some previous studies [27]. Bicaudate index is one of the common tools used to define hydrocephalus in daily practice, and a normal range for different ages has been previously defined by studies, with some variations [30]. We chose to use relatively strict criteria of 0.13 for age under 30 years, 0.15 for age of 31–40 years, 0.19 for age of 41–50 years, and 0.25 after the age of 50. We found that analysis using the bicaudate index to dichotomize the patients was a useful way to predict shunt dependency in univariate and multivariate analyses. IVH score was also selected for the analysis, because IVH, Graeb, and LeRoux scores are equally useful for assessing IVH severity [31]. IVH score was shown to be a significant predictor in the univariate analysis.
In the current study, the blood volumes in each ventricle, calculated with high inter-rater variability, were associated with the incidence of acute hydrocephalus and IVH score. This indicates that the distribution pattern of blood in the ventricles may affect the severity of the disease and the incidence of acute hydrocephalus. The proposed mechanism of acute hydrocephalus is the increased resistance of CSF flow caused by blood clots in the ventricular system. In contrast, chronic hydrocephalus may be caused by the persistent obstruction of the arachnoid granulations by blood-breaking products and their inflammatory reactions [32, 33]. Although the decision to place EVD catheters in this population is multifactorial, the EVD catheter placement has been associated with IVH volume and reduced mortality [24]. In the current study, the mean period of external ventricular drainage before VP shunt placement was 16.1 days, which was similar to some previous studies [26, 27]. Because there is no worldwide consensus of EVD weaning strategy, this relatively long duration of EVD drainage may be due to our challenge protocol. In addition, 82% of our patients had thalamic ICH, which may lead to more IVH in third and fourth ventricles with longer time of EVD drainage.
We compared three models composed of different parameters and identified a multiple logistic regression model that includes blood volumes in the third and fourth ventricles, the bicaudate index, and the ratio of blood volume in the lateral ventricles to that in the third and fourth ventricles to predict shunt dependency with relatively high AUC. Previously established models for prediction of shunt dependency included ICH location and ICP after EVD catheter placement as variables [27]. Early and accurate prediction of shunt-dependent hydrocephalus may help avoid the risky EVD challenge procedure and prolonged EVD drainage in patients with a high risk of failure, shorten the course of treatment, decrease the incidence of EVD-related CSF infections, and decrease medical expenses.
This study has some limitations. This was a retrospective analysis with a relatively small sample size and a low average IVH volume for a single institution. Currently, there is no consensus for the EVD challenge protocol or for the definition of shunt-dependent hydrocephalus, which makes it difficult to generalize the results of any single study in this field. Some clinical parameters, such as headaches or vomiting, were not included for analysis because many patients at the acute stage were comatose. The daily drainage amount of CSF was not included in this study due to different rates of progressive elevation of the EVD drip chamber and the variation in duration of drainage for individual patients.
In conclusion, shunt-dependent hydrocephalus after IVH in our patients was associated with IVH scores, the bicaudate index, blood volume in the lateral ventricles and the fourth ventricle, and the ratio of blood volume in the lateral ventricles to that in the third and fourth ventricles in the univariate analysis. The best multiple logistic regression model included blood volume parameters and bicaudate index as predictors with the area under a receiver operating characteristic curve of 0.849. These findings may promote more aggressive monitoring and earlier interventions for shunt dependency after IVH in patients at risk.
References
Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Magid D, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, Moy CS, Mussolino ME, Nichol G, Paynter NP, Schreiner PJ, Sorlie PD, Stein J, Turan TN, Virani SS, Wong ND, Woo D, Turner MB. Executive summary: heart disease and stroke statistics–2013 update: a report from the American Heart Association. Circulation. 2013;127(1):143–52.
Leira R, Davalos A, Silva Y, Gil-Peralta A, Tejada J, Garcia M, Castillo J. Early neurologic deterioration in intracerebral hemorrhage: predictors and associated factors. Neurology. 2004;63(3):461–7.
Tuhrim S, Horowitz DR, Sacher M, Godbold JH. Volume of ventricular blood is an important determinant of outcome in supratentorial intracerebral hemorrhage. Crit Care Med. 1999;27(3):617–21.
Bhattathiri PS, Gregson B, Prasad KS, Mendelow AD. Intraventricular hemorrhage and hydrocephalus after spontaneous intracerebral hemorrhage: results from the STICH trial. Acta Neurochir Suppl. 2006;96:65–8.
Hallevi H, Albright KC, Aronowski J, Barreto AD, Martin-Schild S, Khaja AM, Gonzales NR, Illoh K, Noser EA, Grotta JC. Intraventricular hemorrhage: anatomic relationships and clinical implications. Neurology. 2008;70(11):848–52.
Diringer MN, Edwards DF, Zazulia AR. Hydrocephalus: a previously unrecognized predictor of poor outcome from supratentorial intracerebral hemorrhage. Stroke J Cereb Circ. 1998;29(7):1352–7.
Juvela S. Risk factors for impaired outcome after spontaneous intracerebral hemorrhage. Arch Neurol. 1995;52(12):1193–200.
Adams RE, Diringer MN. Response to external ventricular drainage in spontaneous intracerebral hemorrhage with hydrocephalus. Neurology. 1998;50(2):519–23.
Engelhard HH, Andrews CO, Slavin KV, Charbel FT. Current management of intraventricular hemorrhage. Surg Neurol. 2003;60(1):15–21.
Findlay JM, Jacka MJ. Cohort study of intraventricular thrombolysis with recombinant tissue plasminogen activator for aneurysmal intraventricular hemorrhage. Neurosurgery. 2004;55(3):532–7.
Gaberel T, Magheru C, Parienti JJ, Huttner HB, Vivien D, Emery E. Intraventricular fibrinolysis versus external ventricular drainage alone in intraventricular hemorrhage: a meta-analysis. Stroke J Cereb Circ. 2011;42(10):2776–81.
Varelas PN, Rickert KL, Cusick J, Hacein-Bey L, Sinson G, Torbey M, Spanaki M, Gennarelli TA. Intraventricular hemorrhage after aneurysmal subarachnoid hemorrhage: pilot study of treatment with intraventricular tissue plasminogen activator. Neurosurgery. 2005;56(2):205–13.
Hallevi H, Dar NS, Barreto AD, Morales MM, Martin-Schild S, Abraham AT, Walker KC, Gonzales NR, Illoh K, Grotta JC, Savitz SI. The IVH score: a novel tool for estimating intraventricular hemorrhage volume: clinical and research implications. Crit Care Med. 2009;37(3):969–974, e961.
van Gijn J, Hijdra A, Wijdicks EF, Vermeulen M, van Crevel H. Acute hydrocephalus after aneurysmal subarachnoid hemorrhage. J Neurosurg. 1985;63(3):355–62.
Sezgin M, Sankur B. Survey over image thresholding techniques and quantitative performance evaluation. J Electron Imaging. 2004;13:146–68.
Liu CC, Tsai CY, Liu J, Yu CY, Yu SS. A pectoral muscle segmentation algorithm for digital mammograms using Otsu thresholding and multiple regression analysis. Comput Math Appl. 2012;64:1100–7.
Otsu N. A threshold selection method from gray-level histograms. IEEE Trans Syst Man Cybern. 1979;9:62–8.
Koch GG. Intraclass correlation coefficient. In: Kotz S, Johnson NL, editors. Encyclopedia of statistical sciences. 4th ed. New York: Wiley; 1982. p. 213–7.
Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86(2):420–8.
Youden WJ. Index for rating diagnostic tests. Cancer. 1950;3(1):32–5.
Hajian-Tilaki K. Receiver operating characteristic (ROC) curve analysis for medical diagnostic test evaluation. Caspian J Intern Med. 2013;4(2):627–35.
Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143(1):29–36. https://doi.org/10.1148/radiology.143.1.7063747.
Obuchowski NA. Receiver operating characteristic curves and their use in radiology. Radiology. 2003;229(1):3–8. https://doi.org/10.1148/radiol.2291010898.
Herrick DB, Ullman N, Nekoovaght-Tak S, Hanley DF, Awad I, LeDroux S, Thompson CB, Ziai WC. Determinants of external ventricular drain placement and associated outcomes in patients with spontaneous intraventricular hemorrhage. Neurocrit Care. 2014;21(3):426–34. https://doi.org/10.1007/s12028-014-9959-x.
Cheung RT, Zou LY. Use of the original, modified, or new intracerebral hemorrhage score to predict mortality and morbidity after intracerebral hemorrhage. Stroke J Cereb Circ. 2003;34(7):1717–22.
Zacharia BE, Vaughan KA, Hickman ZL, Bruce SS, Carpenter AM, Petersen NH, Deiner S, Badjatia N, Connolly ES Jr. Predictors of long-term shunt-dependent hydrocephalus in patients with intracerebral hemorrhage requiring emergency cerebrospinal fluid diversion. Neurosurg Focus. 2012;32(4):E5. https://doi.org/10.3171/2012.2.FOCUS11372.
Miller C, Tsivgoulis G, Nakaji P. Predictors of ventriculoperitoneal shunting after spontaneous intraparenchymal hemorrhage. Neurocrit Care. 2008;8(2):235–40. https://doi.org/10.1007/s12028-007-9018-y.
Rincon F, Gordon E, Starke RM, Buitrago MM, Fernandez A, Schmidt JM, Claassen J, Wartenberg KE, Frontera J, Seder DB, Palestrant D, Connolly ES, Lee K, Mayer SA, Badjatia N. Predictors of long-term shunt-dependent hydrocephalus after aneurysmal subarachnoid hemorrhage. Clinical article. J Neurosurg. 2010;113(4):774–80.
Staykov D, Kuramatsu JB, Bardutzky J, Volbers B, Gerner ST, Kloska SP, Doerfler A, Schwab S, Huttner HB. Efficacy and safety of combined intraventricular fibrinolysis with lumbar drainage for prevention of permanent shunt dependency after intracerebral hemorrhage with severe ventricular involvement: a randomized trial and individual patient data meta-analysis. Ann Neurol. 2017;81(1):93–103.
Kukuljan M, Kolic Z, Bonifacic D, Vukas D, Miletic D. Normal bicaudate index by aging. J Med Image Rev. 2009;5:72–4.
Hwang BY, Bruce SS, Appelboom G, Piazza MA, Carpenter AM, Gigante PR, Kellner CP, Ducruet AF, Kellner MA, Deb-Sen R, Vaughan KA, Meyers PM, Connolly ES Jr. Evaluation of intraventricular hemorrhage assessment methods for predicting outcome following intracerebral hemorrhage. J Neurosurg. 2012;116(1):185–92. https://doi.org/10.3171/2011.9.JNS10850.
Chen CC, Liu CL, Tung YN, Lee HC, Chuang HC, Lin SZ, Cho DY. Endoscopic surgery for intraventricular hemorrhage (IVH) caused by thalamic hemorrhage: comparisons of endoscopic surgery and external ventricular drainage (EVD) surgery. World Neurosurg. 2011;75(2):264–8.
Lodhia KR, Shakui P, Keep RF. Hydrocephalus in a rat model of intraventricular hemorrhage. Acta Neurochir Suppl. 2006;96:207–11.
Funding
There was no funding for this study.
Author information
Authors and Affiliations
Contributions
L-T Kuo provided research conception, collected clinical data and wrote manuscript. Dr. Kuo also made final approval of the version to be published. H-Y Lu conducted imaging process and statistical analysis, interpreted research data and wrote manuscript. Dr. Lu also made final approval of the published version. J-C Tsai helped in data analysis and manuscript evaluation. Y-K Tu contributed to data collection and manuscript revision.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
This study was approved by National Taiwan University Hospital’s Institutional Review Board (IRB case #201211025RIB).
Rights and permissions
About this article
Cite this article
Kuo, LT., Lu, HY., Tsai, JC. et al. Prediction of Shunt Dependency After Intracerebral Hemorrhage and Intraventricular Hemorrhage. Neurocrit Care 29, 233–240 (2018). https://doi.org/10.1007/s12028-018-0532-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-018-0532-x