Abstract
Background
Changes in the perihemorrhagic zone (PHZ) of intracerebral hemorrhage (ICH) are variable. Different mechanisms contribute to secondary neuronal injury after ICH. This multimodal monitoring study investigated early changes in the PHZ of ICH.
Methods
Twenty-four swine were anesthetized, ventilated, and underwent monitoring of vital parameters. Next to an intracranial pressure-probe (ICP), microdialysis (MD), thermodiffusion cerebral blood flow (td-CBF), and oxygen probes (PbrO2) were placed into the gray white matter junction for 12 h of monitoring. ICH was induced using the autologous blood injection model. Pre-defined volumes were 0 ml (sham), 1.5 ml ipsilateral (1.5 ml), 3.0 ml ipsilateral (3.0 ml), and 3.0 ml contralateral (3.0 ml contra).
Results
ICP equally increased in all groups after ICH. In the 3.0 ml group tissue oxygenation decreased to ischemic values of 9 ± 7 mmHg early after 6 h of monitoring. This decrease was associated with a significant perfusion reduction from 36 ± 8 ml/100 g/min to 20 ± 10 ml/100 g/min. MD correlated with a threefold lactate/pyruvate ratio increase. Measurements in all other groups were unchanged.
Conclusion
Multimodal monitoring demonstrates volume-dependent changes of tissue oxygenation, blood flow, and ischemic MD markers in the PHZ independent of increased ICP suggesting early moderate ischemia. No evidence was found for the existence of a perihemorrhagic ischemia in the small hematoma groups.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intracerebral hemorrhage (ICH) accounts for 6.5 to 19.6 % of stroke cases with mortality rates in the first week and first year after onset ranging from 31 to 34 % and 53 to 59 % [1]. In theory large hematoma volumes cause an increase of ICP and consecutive decrease of CBF and PbrO2 leading to local or global ischemia. Whether cytotoxic or vasogenic edema plays a key role in perihemorrhagic pathophysiology remains a question of debate [2]. These secondary brain tissue changes could be the most remarkable factors that have an impact on outcome parameters. Although there are many advances in multimodal monitoring, the role of these initial pathophysiological factors during the first hours after the initial event, is not well understood [3].
We have previously established a porcine ICH model using multimodal monitoring (MMM) [4]. A volume-controlled ICH animal model with gyrencephalic brain could help to clarify the initial changes using MMM including ICP, CPP, CBF, PbrO2, temperature and microdialysis (MD) and determine the natural history of the perihematomal changes.
In this study, we investigated the hypothesis whether a nonICP-related volume-dependent damage occurs after induction of a right frontal subcortical ICH as measured by ICP, CBF, PbrO2 and MD.
Materials and Methods
Animal Preparation
Twenty-seven male pigs weighing 24 to 32 kg were used. All animal experiments were approved by the local University of Heidelberg and governmental (Regierungspräsidium Karlsruhe) committees for animal care and use (Protocol No.: 35-9185.81/G-60/06) and conducted in accordance with the guidelines set by §8 Abs. 1 Tierschutzgesetz (TierSchG) 2006.
Animals were sedated with ketamine hydrochloride (10 mg/kg i.m.), azaperon (3 mg/kg i.m.), and midazolam (1 mg/kg i.m.). A peripheral intravenous catheter was inserted into the ear for administration of drugs and to maintain fluid balance with Ringer’s solution. Anesthesia was induced with an intravenous bolus injection of midazolam (1 mg/kg) and ketamine hydrochloride (10 mg/kg). After endotracheal intubation, the animals were maintained on controlled positive-pressure ventilation with 35 % oxygen. Anesthesia was maintained by inhaled isoflurane (1.2–1.5 %). Tidal volume and ventilatory frequency were adjusted to maintain PaCO2 between 32 and 35 torr.
Electrocardiographic (ECG) and pulse rate monitoring were started and continued throughout the whole experiment. Rectal and brain temperature (Tr, Tbr) were continuously monitored. Rectal temperature was maintained between 35.5 and 37 °C. After surgical exposure of the right femoral artery a 4-Fr catheter was inserted for permanent monitoring of mean arterial blood pressure (MAP). Peripheral oxygen saturation (SaO2) was monitored from the left ear. During experiments, hemodynamic parameters (pulse rate, systemic arterial blood pressure), and rectal temperature were monitored continuously with a Datex® AS/3 anesthesia monitor (Datex Inc.; Espoo, Finland). The intracerebral temperature was monitored with a Neurovent®-TO catheter (Raumedic, Helmbrechts, Germany).
Four groups were defined (sham, 1.5, 3.0 ml and 3.0 contra). In the sham group (n = 5), animals underwent MMM without ICH-injection to determine the physiological values in this ICH-porcine model.
In the 1.5 ml (n = 7) and 3.0 ml groups (n = 7) animals received an ICH of 1.5 ml and 3.0 ml, respectively, with MMM on the ipsilateral side. In 3.0 ml contra (n = 5) the MMM was carried out in the right hemisphere while the hematoma (3 ml) was injected into in the left hemisphere. Parts of this data of the sham group and 1.5 ml group have already been published [4]. Three animals did not enter data analysis as ICH could not be confirmed due to subarachnoid or ventricular extension.
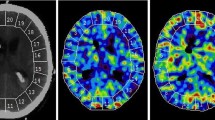
Experimental ICH
We used the autologous whole blood injection model described elsewhere [5]. Arterial non-heparinised autologous blood drawn from the femoral artery was loaded in calibrated polyvinyl chloride tubing to produce an ICH. After fixation of the animal’s head with a tape, a midline scalp incision was performed to expose the calvarium. The head was fixed in a stereotactic frame. Five burr holes (2 mm in diameter) were drilled on the right side of the cranium. One burr hole was placed parietally through which the ICP probe (Neurovent-P®, Raumedic AG, Helmbrechts, Germany) was inserted. Next to the coronal suture, three burr holes were placed 0.8, 1.2, and 1.6 next to the midline, respectively. Through these burr holes, the monitoring probes were inserted next to each other. Medially, the td-CBF-probe (Hemedex td-rCBF, Codman®, USA) followed by the PbrO2-probe (Neurovent®-TO, Raumedic AG, Helmbrechts, Germany) and MD probe (CMA 70, Solna, Sweden) most laterally (Fig. 1) were inserted. All intraparenchymal devices were introduced and secured transcutaneously prior to insertion into the brain. Further frontally, we used a 90° vertical and 20° lateral bent steel 20G cannula for induction of the ICH via the fifth burr hole which was located 1.5 cm in front of the coronal suture and 0.8 cm lateral to the sagittal suture. An autologous arterial hematoma was induced following the description of Quereshi et al. [5]. Polyvinyl chloride tubing was attached to a stopcock at the distal end of the spinal needle and to the femoral artery (Fig. 1). To initiate ICH formation, autologous blood was introduced into the brain under arterial pressure via this tubing. We aimed to target the cortico-subcortical area in order to avoid deep ICH location. Neither the catheters nor the syringes were flushed with heparin. After catheter placements and ICH-injection, the burr holes were sealed with bone wax and monitoring was conducted for an overall monitoring period of 12 h. Post-mortem brains were removed and intraparenchymal catheter locations and ICH size and position were visualized [4].
Schematic drawing of catheter positioning in relation to the injection site of the hematoma. The ICP probe is introduced parietally. Anteriorly three monitoring probes are placed in the following order from medial to lateral: td-CBF, PbrO2 and microdialysis. Further frontally the burr hole site for the hematoma is marked with a 90° bent steel cannula which is used for hematoma injection
Monitoring
All relevant physiological parameters such as mean arterial pressure (MAP), intracranial pressure (ICP), cerebral perfusion pressure (CPP), brain and rectal temperature (Tb, TR), heart rate (HR), oxygen saturation (SaO2), PbrO2, rCBF were continuously recorded. Microdialysates were perfused with a rate of 0.3 µl/min and samples were taken every 30 min. The MD vials were collected, refrigerated, and analyzed after the experiment was completed. Blood gas analyses were carried out every 2 h. Animals were kept cardiopulmonary stable and observed further on. Following an equilibration phase of 2 h after catheter placement, a baseline measurement was undertaken in the sham group and 30 min before ICH in 1.5, 3.0, and 3.0 ml contra groups (baseline). Further pre-defined measurements were repeated at 3, 6, and 9 h after ICH (3, 6, 9 h).
Statistical Analysis
Statistical analysis was performed using SigmaPlot (version 11.0.0.77, Systat Software, San Jose, California, USA). Differences between baseline measurement and final measurements at 9 h were determined by the Student’s t test for each parameter (ICP, PbrO2, CBF, and MD) if the data were normally distributed or by the Mann–Whitney rank sum test if the normality assumption failed. Significance levels are reported for comparisons with the two-tailed test (P < 0.05).
Results
Intracranial Pressure (ICP)
There were no significant changes in the sham group. In all ICH-groups there was a significant immediate rise in ICP associated with the induction of blood and this increase persisted for the duration of the whole experiment (Table 1). However, ICP never exceeded 15 mmHg with maximum mean ICP values of 13 mmHg in the 3.0 ml ICH volume group.
Cerebral Perfusion (CBF)
In the 3.0 ml group CBF values started at 36 mL/100 g/min and subsequently dropped to subcritical values of 20 ml/100 g/min at 9 h. This result was statistically significant with a P value < 0.05. However, CBF in all other groups did not change significantly compared with the baseline value (Table 1).
Brain Tissue Oxygen Partial Pressure (PbrO2)
In the 3.0 ml group there was a progressive significant decrease of PbrO2 after ICH induction from 41 ± 11 mmHg at baseline (0 h) to 10 ± 5 mmHg at 9 h (P < 0.001). In all other groups we could not show any significant changes at any time point after ICH as compared to baseline (Table 1).
Cerebral Metabolism
Microdialysis was utilized in all groups, and the brain concentrations of glucose, lactate, pyruvate, and glutamate were analyzed. Lactate/pyruvate ratio (L/P ratio) did not increase in sham, 1.5 and 3.0 ml contra groups over time, whereas a significant 1.6-fold increase was observed in 3.0 ml group (Table 1, P < 0.05). Likewise, lactate increased significantly from 1.6 ± 0.8 to 4.5 ± 1.8 mmol/l (P < 0.01). Glucose utilizations changed only in 3.0 ml contra group. After induction of the contralateral hematoma, extracellular glucose concentrations increased threefold from 1.1 ± 0.7 to 3.5 ± 3.3 mmol/l. Concordant to this a 1.4-fold decrease in L/P ratio was observed over time. Glutamate concentrations did not change significantly in all groups.
Discussion
It is well-recognized that ICH volume may represent a major predictor of edema formation and eventually outcome [2]. A volume-dependent impairment of intact perihematomal physiology has been recently demonstrated in a CT-perfusion study. The authors conclude from their findings that the PHZ correlates to hematoma volume as measured by the 360° cortical banding CT-perfusion method [6]. Furthermore, clinically available monitoring tools such as multimodality probes have not been used to address this question. It has been discussed that cerebral ischemia contributes to secondary neuronal damage after ICH, but the results of different experimental and clinical trials are inconclusive and the existence of a “perihemorrhagic penumbra” is still an area of debate [7–10]. Our monitoring data suggest that perihemorrhagic ischemia may occur depending on ICH volume.
Most of the experimental ICH projects have used rodent models. In theory, a porcine ICH model has the advantage of the large brain volume (about 40 times larger than the rat’s brain) which enables bedside-to-bench translation of multimodal neuromonitoring and surgical procedures used in clinical settings. However, simulating human ICH in an animal model is complex. One frequent question in experimental project design is whether the results can be applied to human pathologies [11]. In the blood induction animal model there is no hematoma enlargement, but timing and location of hemorrhage are more controlled [11]. This model allows investigating the toxic effect of blood products, edema formation, and it allows for volume-controlled studies.
There is limited evidence for invasive MMM in ICH patients and therefore, there are no specific guidelines about the usage of monitoring in ICH population [12]. The present study used a MMM approach measuring parameters with the clinically available techniques ICP, td-CBF, PbrO2, and MD.
ICP and CPP are determinants of outcome in neurosurgical/neurological patients [13]. Secondary ischemic injuries due to compression of local arterioles, venous congestion, perifocal edema, and also due to toxic metabolic effects of the blood products and their impact on vasoconstriction cannot be monitored by ICP/CPP monitoring alone especially if ICP levels are normal [14, 15].
In control animals ICP was constant during the entire experiment. After ICH induction there was a significant increase in ICP at all timepoints in comparison to the baseline in all groups (Table 1). ICP increased to its’ maximum and plateaued at this level 6 h after ICH induction in all groups. We, therefore, suspect that ICP is mainly influenced by the initial bleeding event but much less affected by processes of the perihemorrhagic zone in the acute phase after ICH. ICP never reached critical levels (>15 mmHg). Therefore, ICP did not indicate disease severity in our study.
According to a study by Kauffmann et al. [16] the penumbra was defined by a CBF of 8–20 ml/100 g/min in the perihemorrhagic zone. In many animal experiments on ICH a decrease of CBF was demonstrated globally and/or in the PHZ [17–20]. The exact cause for this hypoperfusion is unclear; it may be due to a perihemorrhagic-induced mechanical pressure, the release of vasoactive substances like adrenaline, a no-reflow phenomenon during the reperfusion phase, and the successive global increase of the ICP.
There were no significant CBF-changes during the experiment in sham, 1.5 and 3.0 ml contra groups. In the 3.0 ml group CBF decreased during the first 3 h after ICH induction. For the last 3 h of the experiment the CBF stayed at the penumbra threshold of 20 ± 10 ml/100 g/min. All experiments were continued for 9 h after ICH induction. It could be argued, that CBF might have continued to decrease in the PHZ successively. On the other hand, it has been suggested that after 12–24 h of ictus the reperfusion phase begins [14]. The reperfusion phase is a result of the revocation of perihemorrhagic-induced pressure, the autoregulation effect and the initiation of the collateral circulation. More studies with longer monitoring and observation would be necessary to prove or disprove this concept.
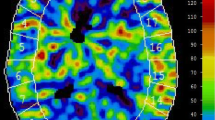
Similar to our data it was demonstrated in a clinical study that hypoperfusion in the PHZ did not lead to ischemia and it was argued whether these changes might indicate diaschisis [21]. Our study demonstrates early hypoperfusion in the PHZ which is pronounced with increasing ICH volume (Fig. 2). This might be either a consequence of reduced focal blood supply (preischemia) or a result of decreased metabolic requirement of injured brain tissue, too [21]. The constant volume increase in the white matter of the PHZ, resulting from perihemorrhagic edema, accompanied by a lower metabolic rate could also account for this. Hypoperfusion in the 3.0 ml group most likely occurred due to the direct mechanical effect of the larger lesion. Increase of ICH volume may have triggered development of ischemia in our study, but toxic effects of blood components like thrombin, iron, and matrix metalloproteinase could also contribute to the change in CBF [22, 23]. In an earlier study, we reported that there is no relevant ischemic tissue in the PHZ [8]. However, we did not correlate MR-findings to different ICH volumes in that previous study.
Intracerebral monitoring of PbrO2 reflects the efficiency of CBF and local tissue oxygenation and is increasingly used on neuro-ICUs [24]. PbrO2 threshold of ischemic hypoxia was defined as below 10 mmHg [25]. It has been consistently shown that low PbrO2 (<15 mm Hg) is a strong predictor of poor outcome in aneurysmal SAH and TBI and might decrease despite normal ICP and CPP [10, 26, 27]. The PbrO2 technique in ICH was first described by Hemphill et al. They used similar monitoring methods in patients and animal models to understand ICH pathophysiology and the correlation with ICP [10]. In accordance with our CBF findings, no significant difference was observed for PbrO2 under control conditions. Following ipsilateral ICH (1.5 and 3.0 ml), PbrO2 was affected by acute hematoma formation, declining in parallel with acute increase in ICP. Interestingly, in the 1.5 ml group PbrO2 never reached pathological values leveling below 20 mmHg (Table 1), despite a moderately increased ICP. We suggest that this observation is due to compensatory effects induced by autoregulation which seems to be intact at this small volume ICH. In contrast, PbrO2 decreased significantly after hematoma induction in the 3.0 m ICH group below the critical threshold of 10 mm Hg after 6 h and did not recover until the end of the experiments. Microdialysis allows nearly real-time measurement of the cerebral extracellular concentrations of markers of energy metabolism like glucose, pyruvate and lactate, and of neuronal injury (glycerol and glutamate) [28–31].
Experimental studies support the hypothesis that there is an increased accumulation of glutamate, which is an indicator of pending ischemia in the early stage after ICH formation [32]. Here, glutamate did not change consistently over the observation time in all groups (data not shown).
Increased glycolysis and anaerobic metabolism in neurons and glia may trigger increased lactate concentrations under ischemic conditions. Hereby, lactate is also transferred to neurons as energy substrate alternative to glucose.
In the 1.5 ml group did not show any significant changes in lactate concentrations. In the 3.0 ml group lactate increased in a volume-dependent manner significantly from 1.6 ± 0.8 to 4.5 ± 1.8 mmol/l (P < 0.002). Furthermore, in our setting lactate concentrations correlated with CBF and PbrO2 values in this group.
The lactate/pyruvate ratio (L/P ratio) has been established as a more specific indicator of ischemia than lactate alone [33]. Our study showed no significant changes in the L/P ratio in sham, 1.5, and 3.0 ml groups. The L/P ratio increased significantly in 3.0 ml group after ICH-injection over a time period of 9 h. In this group the L/P ratio correlated well with CBF and PbrO2. Taken together these findings may reflect mild cerebral hypoxia with local ischemia due to changes in cerebral circulation after moderate volume ICH induction.
There are limitations to our study. The MD sample quality might be affected after implantation of the catheter by environmental factors such as edema and mechanical instability in the experimental setup. This might be reflected in relatively high standard deviations. Furthermore, td-CBF recordings are prone to temperature changes and mechanical instability as well. As the probes were not implanted using cranial bolts minimal movements due to breathing or shivering of the animals may have disturbed recordings. In fact, recalibration procedures were initiated frequently during the experiments leading to partially non continuous CBF recordings. Post-ICH observation time was limited to 9 h. Further experiments with larger ICH volumes and longer observation times may add more information about the above mentioned mechanisms and possible recovery mechanisms. The injection method chosen for these experiments do not allow to study spontaneous ICH progression and may show higher inflammatory responses in longer observations periods. Furthermore, as autologous ICH creation does not emulate small vessel rupture, microvascular breakdown effects are difficult to assess. Intraoperative confirmation of monitoring probe positions in relation to the hemorrhage site could not be performed due to the risk of probe dislocation during animal transfer to the imaging unit, therefore, we confirmed hematoma size and probe position post-mortem.
Conclusion
In this porcine model of ICH, we demonstrated that increasing hematoma volume is associated with ischemia like oxygenation and metabolism in the perihemorrhagic zone as demonstrated by multimodal neuromonitoring techniques. This was observed independent of ICP. This experimental setup is suitable for future studies with extended observation times, histological analyses, and therapeutic interventions.
References
Flaherty ML, Haverbusch M, Sekar P, Kissela B, Kleindorfer D, Moomaw CJ, et al. Long-term mortality after intracerebral hemorrhage. Neurology. 2006;66:1182–6.
Butcher KS, Baird T, MacGregor L, Desmond P, Tress B, Davis S. Perihematomal edema in primary intracerebral hemorrhage is plasma derived. Stroke. 2004;35:1879–85.
Kirkman MA, Smith M. Supratentorial intracerebral hemorrhage: a review of the underlying pathophysiology and its relevance for multimodality neuromonitoring in neurointensive care. J Neurosurg Anesthesiol. 2013;25:228–39.
Orakcioglu B, Kentar M, Uozumi Y, Santos E, Schiebel P, Unterberg A, et al. Multiparametric characterisation of the perihemorrhagic zone in a porcine model of lobar ICH. Acta Neurochir. Suppl. 2011;111:19–23.
Qureshi AI, Wilson DA, Hanley DF, Traystman RJ. No evidence for an ischemic penumbra in massive experimental intracerebral hemorrhage. Neurology. 1999;52:266–72.
Beseoglu K, Etminan N, Turowski B, Steiger H-J, Hänggi D. The extent of the perihemorrhagic perfusion zone correlates with hematoma volume in patients with lobar intracerebral hemorrhage. Neuroradiology. 2014; epub ahead of print.
Herweh C, Juttler E, Schellinger PD, Klotz E, Jenetzky E, Orakcioglu B, et al. Evidence against a perihemorrhagic penumbra provided by perfusion computed tomography. Stroke. 2007;38:2941–7.
Orakcioglu B, Fiebach JB, Steiner T, Kollmar R, Juttler E, Becker K, et al. Evolution of early perihemorrhagic changes–ischemia vs. edema: an MRI study in rats. Exp Neurol. 2005;193:369–76.
Pascual AM, Lopez-Mut JV, Benlloch V, Chamarro R, Soler J, Lainez MJ. Perfusion-weighted magnetic resonance imaging in acute intracerebral hemorrhage at baseline and during the 1st and 2nd week: a longitudinal study. Cerebrovasc Dis. 2007;23:6–13.
Hemphill JC, Morabito D, Farrant M, Manley GT. Brain tissue oxygen monitoring in intracerebral hemorrhage. Neurocrit Care. 2005;3:260–70.
Kirkman MA, Allan SM, Parry-Jones AR. Experimental intracerebral hemorrhage: avoiding pitfalls in translational research. J Cereb Blood Flow Metab. 2011;31:2135–51.
Morgenstern LB, Hemphill JC 3rd, Anderson C, Becker K, Broderick JP, Connolly ES Jr, et al. Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2010;41:2108–29.
Juul N, Morris GF, Marshall SB, Marshall LF. Intracranial hypertension and cerebral perfusion pressure: influence on neurological deterioration and outcome in severe head injury. The Executive Committee of the International Selfotel Trial. J Neurosurg. 2000;92:1–6.
He D, Zhao L, Li L, Liu H, Zhang L, Yew DT. Changes of blood flow perfusion by MR and NF-kappabeta expression in the region of perihematoma after experimental intracerebral hemorrhage: a correlation study. Int J Neurosci. 2009;119:806–14.
Powers WJ, Zazulia AR, Videen TO, Adams RE, Yundt KD, Aiyagari V, et al. Autoregulation of cerebral blood flow surrounding acute (6 to 22 hours) intracerebral hemorrhage. Neurology. 2001;57:18–24.
Kaufmann AM, Firlik AD, Fukui MB, Wechsler LR, Jungries CA, Yonas H. Ischemic core and penumbra in human stroke [see comments]. Stroke. 1999;30:93–9.
Bullock R, Brock-Utne J, van Dellen J, Blake G. Intracerebral hemorrhage in a primate model: effect on regional cerebral blood flow. Surg Neurol. 1988;29:101–7.
Belayev L, Saul I, Curbelo K, Busto R, Belayev A, Zhang Y, et al. Experimental intracerebral hemorrhage in the mouse: histological, behavioral, and hemodynamic characterization of a double-injection model. Stroke. 2003;34:2221–7.
Mendelow AD. Mechanisms of ischemic brain damage with intracerebral hemorrhage. Stroke. 1993;24:I115–7; discussion I118–9.
Yang GY, Betz AL, Chenevert TL, Brunberg JA, Hoff JT. Experimental intracerebral hemorrhage: relationship between brain edema, blood flow, and blood-brain barrier permeability in rats. J Neurosurg. 1994;81:93–102.
Zazulia AR, Diringer MN, Videen TO, Adams RE, Yundt K, Aiyagari V, et al. Hypoperfusion without ischemia surrounding acute intracerebral hemorrhage. J Cereb Blood Flow Metab. 2001;21:804–10.
Xi G, Reiser G, Keep RF. The role of thrombin and thrombin receptors in ischemic, hemorrhagic and traumatic brain injury: deleterious or protective? J Neurochem. 2003;84:3–9.
Keep RF, Hua Y, Xi G. Intracerebral haemorrhage: mechanisms of injury and therapeutic targets. Lancet Neurol. 2012;11:720–31.
Rose JC, Neill TA, Hemphill JC. Continuous monitoring of the microcirculation in neurocritical care: an update on brain tissue oxygenation. Curr Opin Crit Care. 2006;12:97–102.
Dings J, Meixensberger J, Jager A, Roosen K. Clinical experience with 118 brain tissue oxygen partial pressure catheter probes. Neurosurgery. 1998;43:1082–95.
Maloney-Wilensky E, Gracias V, Itkin A, Hoffman K, Bloom S, Yang W, et al. Brain tissue oxygen and outcome after severe traumatic brain injury: a systematic review. Crit. Care Med. 2009;37:2057–63.
Oddo M, Levine JM, Mackenzie L, Frangos S, Feihl F, Kasner SE, et al. Brain hypoxia is associated with short-term outcome after severe traumatic brain injury independently of intracranial hypertension and low cerebral perfusion pressure. Neurosurgery. 2011;69:1037–45 discussion 1045.
Nilsson OG, Polito A, Saveland H, Ungerstedt U, Nordstrom CH. Are primary supratentorial intracerebral hemorrhages surrounded by a biochemical penumbra? A microdialysis study. Neurosurgery. 2006;59:521–8 discussion 521–8.
Zazulia AR, Videen TO, Powers WJ. Transient focal increase in perihematomal glucose metabolism after acute human intracerebral hemorrhage. Stroke. 2009;40:1638–43.
Goodman JC, Valadka AB, Gopinath SP, Uzura M, Robertson CS. Extracellular lactate and glucose alterations in the brain after head injury measured by microdialysis. Crit Care Med. 1999;27:1965–73.
Unterberg AW, Sakowitz OW, Sarrafzadeh AS, Benndorf G, Lanksch WR. Role of bedside microdialysis in the diagnosis of cerebral vasospasm following aneurysmal subarachnoid hemorrhage. J Neurosurg. 2001;94:740–9.
Qureshi AI, Ali Z, Suri MF, Shuaib A, Baker G, Todd K, et al. Extracellular glutamate and other amino acids in experimental intracerebral hemorrhage: an in vivo microdialysis study. Crit Care Med. 2003;31:1482–9.
Persson L, Valtysson J, Enblad P, Warme PE, Cesarini K, Lewen A, et al. Neurochemical monitoring using intracerebral microdialysis in patients with subarachnoid hemorrhage. J Neurosurg. 1996;84:606–16.
Conflict of interest
Berk Orakcioglu, Modar M. Kentar, Patrick Schiebel, Yoichi Uozumi, Andreas Unterberg, Oliver W. Sakowitz declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Berk Orakcioglu and Modar M. Kentar have contributed equally to the manuscript.
Rights and permissions
About this article
Cite this article
Orakcioglu, B., Kentar, M.M., Schiebel, P. et al. Perihemorrhagic Ischemia Occurs in a Volume-Dependent Manner as Assessed by Multimodal Cerebral Monitoring in a Porcine Model of Intracerebral Hemorrhage. Neurocrit Care 22, 133–139 (2015). https://doi.org/10.1007/s12028-014-0027-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-014-0027-3