Abstract
Purpose
The aim of this study was to determine if the measurement of blood biomarkers of glucose cerebral metabolism, performed with retrograde jugular catheter, could predict the outcome of poor-grade aneurysmal subarachnoid hemorrhage (aSAH) patients.
Methods
This study was conducted in 68 poor-grade aSAH patients. A total of 4,024 blood samples obtained from jugular and radial catheters were analyzed for glucose, lactate, and oxygen content every 8 h for 10 ± 0.5 days. Metabolic ratio (MR) and lactate–oxygen index (LOI) were obtained by ratios using arterio-jugular differences. Functional outcome was evaluated at 12 months with the Glasgow Outcome Scale.
Results
Outcome was unfavorable in 40 patients. In this group of patients, the MR was significantly lower (p < 0.0001) and the LOI was significantly higher (p = 0.0001) than in the group with favorable outcome. The MR cutoff value, below which the patients are likely to have an unfavorable outcome, was determined to be 3.35. More interestingly, the data obtained in this study demonstrated that the patients achieving an unfavorable outcome were distinguished from those with a favorable outcome by having at least three events of MR inferior to 3.35 (sensitivity = 90 %, specificity = 82.1 %). Moreover, in patients who developed cerebral vasospasm, we observed a significant decrease in the MR.
Conclusion
Our data provide additional support to the view that the MR is a reliable marker for predicting the outcome of poor-grade aSAH patients. Prospective studies are needed to confirm its value in multimodal monitoring.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Despite advances in the monitoring of patients with aneurysmal subarachnoid hemorrhage (aSAH), mortality remains high. About 46 % of the survivors develop cognitive and functional disorders and 25 % develop severe disability [1, 2]. In poor-grade aSAH patients (18–24 % approximately), the severity of bleeding, the development of global cerebral edema, acute ischemic injury, and vasospasm are pathological changes that determine a worse long-term functional outcome [3–5]. After brain injury, secondary pathological events involving the excitotoxic pathway and impairment of cerebral oxidative metabolism are likely to influence the outcome of the patients. Neuromonitoring is crucial for poor-grade aSAH patients in whom the neurological examination becomes limited. Brain metabolism monitoring in conjunction with cerebral dynamic parameters monitoring could help detect secondary brain insults that are still potentially reversible in routine clinical practice and could improve the long-term functional outcome. In addition to intracranial pressure (ICP) and cerebral perfusion pressure (CPP) measurement, several of different brain monitoring methods is currently available, including jugular venous catheterization, brain parenchymal oxygenation, positron emission tomography, and brain microdialysis [6–8]. Neuromonitoring was proposed to optimize treatment and improve long-term outcome [5, 9]. Secondary pathological events involving the excitotoxic pathway and impairment of cerebral oxidative metabolism are linked to the outcome of the patients. Glycolysis and lactate metabolism can affect neurological function recovery [10]. In 2006, using arterio-jugular differences in glucose and oxygen content, relative hyperglycolysis (RH) was reported to be associated with poor outcome in aSAH [11]. To our knowledge, these preliminary data were never reported again in others cohorts of SAH patients, leading us to question the utility of this monitoring in clinical routine.
The present observational study was therefore undertaken to revisit the utility of the biochemical ratios calculated from the measurements of oxygen, lactate, and glucose in jugular and arterial blood in a cohort of 68 aSAH patients with poor-grade clinical status.
Methods
Study Design and Patient Population
This observational study included 68 poor-grade aSAH patients who had been admitted to the Neurocritical Care Unit of the Neurological Hospital (Lyon University Hospital, France). It received local ethics committee approval. On admission, the patient’s clinical severity status was assessed according to the World Federation of Neurosurgical Societies (WFNS) scale [12]. Computed tomography (CT) scan was used to confirm the subarachnoid hemorrhage and to evaluate clot thickness. CT scan findings were categorized using Fisher’s scale [13]. The presence of an aneurysm was confirmed by cerebral angiography and aneurysms were treated within 48 h after admission by endovascular coiling or surgical clipping. Acute hydrocephalus was treated with immediate placement of a ventricular drain. Patients with a nonaneurysmal SAH, with a good clinical status (WFNS grades 1–3) and survivors without 12-month outcome assessment were excluded from this study.
Clinical Management
All patients were managed in the neurological intensive care unit following the standard guidelines for the management of SAH [14, 15]. Intubation, mechanical ventilation, and sedation with fentanyl associated to propofol, or midazolam were performed when required. All patients underwent multimodal monitoring. Management aimed to maintain the ICP below 20 mmHg and the CPP (CPP = MABP − ICP) above 70 mmHg by adjusting the mean arterial blood pressure (MABP). Cardiopulmonary functions were screened, body temperature was monitored, and normovolemia was maintained. Arterial blood glucose levels were targeted to be within a range of 4.0–8.0 mmol/L. In order to detect any onset of cerebral vasospasm, a transcranial Doppler was performed daily. Cerebral vasospasm was confirmed by angiography and treated by triple H-therapy and/or by angioplasty or intracranial artery nimodipine infusion. Since this study was observational, MR result values were not taken into account and consequently, did not influence patient management.
Jugular Bulb Catheterization
Jugular catheterization was performed within 48 h of onset and maintained in survivors for 10 ± 0.5 days (mean ± SEM). The catheter was inserted into the jugular vein ipsilateral to the aSAH in a retrograde way toward the skull base until a resistance was felt. Then, it was moved about 1 cm backwards. When the aneurysm was located on the anterior communicating artery, the catheter was inserted on the side of the more injured cerebral hemisphere. Correct position of the catheter in the jugular bulb was checked by lateral neck X-ray. Blood withdrawal was scheduled every 8 h.
Blood Sampling and Analysis for pH, PaCO2, Glucose, Lactate, and Oxygen Content
The jugular and arterial blood samples were collected in two syringes with lithium-heparin. Analysis was immediately performed on a blood gas analyzer (ABL system, Radiometer, Copenhagen, Denmark). Oxygen content, lactate, and glucose levels (expressed in mmol/L) and jugular venous oxygen saturation (SjVO2) were measured. Arterio-venous differences for oxygen (avDO2) and glucose (avDgluc) and jugular venous arterial differences for lactate (JaDL) were calculated. The lactate–oxygen index (LOI) was calculated as the ratio [JaDL (mmol/L)]/[avDO2 (mmol/L)]. The metabolic ratio (MR), which provides an assessment of the cerebral metabolic status, was defined as the ratio [avDO2 (mmol/L)]/[avDgluc (mmol/L)] [11]. Normal values for JaDL and LOI were obtained from reference study by Gibbs et al. [16]. In this text, a biochemical event was defined as a complete set of raw data obtained from a blood sampling including both an arterial and a jugular venous sample.
Outcome Measurement
Neurological outcome was evaluated 12 months after the aSAH using the Glasgow Outcome Scale (GOS) [17].
Data Processing and Statistical Analysis
Patients were assigned either to the unfavorable outcome group (GOS 1–3) or the favorable outcome group (GOS 4–5). They were also assigned either to the non-survivors group (GOS 1) or the survivors group (GOS 2–5). We first compared the global mean and median of biomarkers in these different outcome populations. Based on these results, we secondly determined for each patient, the mean of the 25 % lowest MR values (defined as MR min) and the mean of the 25 % highest LOI values (defined as LOI max) during follow-up. Then, we compared the MR min and the LOI max in the unfavorable and favorable outcome groups. Moreover, we determined the cutoff values using a ROC curve analysis able to discriminate between unfavorable and favorable outcome groups. Note that for SjVO2, we used the minimal SjVO2 (using the lowest values) and the maximal SjVO2 (using the highest values) obtained in the two different outcome groups.
Once the cutoff was determined for each biochemical marker, we used a ROC curve analysis to assess the prognostic utility of the number of events which are below or above the cutoff, depending on the biomarker studied.
Statistical Analyses Were Performed to Compare Groups of Patients
Analysis of variance was used for age, a 2 × 2 contingency analysis (Chi square test for sex ratios, WFNS grade, and treatment of aneurysm), a Fisher’s exact test for aneurysm location and a Mann–Whitney non-parametric U test or Student’s t test for blood biomarkers. Biomarker accuracy to predict outcome was characterized using a ROC analysis to determine the cutoff values. Multiple regression with backward selection was used to test the association between the different parameters evaluated (age, WFNS, LOI, SjVO2, and MR) and outcome. The Friedman test was used to compare the changes in MR values during cerebral vasospasm. Results were expressed either as mean ± standard deviation or as median (25th–75th percentiles). Differences were considered statistically significant at p < 0.05. Statistical analyses used MedCalc version 11.3.1.0 (http://www.medcalc.be).
Results
Description of the Population
A total of 68 patients were investigated (27 males, 41 females) with a mean age of 50 years (range 18–75 years). Endovascular coiling and surgical clipping were performed to treat aneurysms in 82.4 and 17.6 % of the patients, respectively. Demographic data are summarized in Table 1. The patients were monitored for a mean period of 10 days. At 12 months post-SAH, the mortality rate was 38.2 %. Overall, outcome was unfavorable in the majority of patients (59 %). No significant difference was found regarding age, sex, WFNS score, and treatment, between the patients with unfavorable (GOS 1–3) and those with favorable (GOS 4–5) outcome, a result which allows an unbiased comparison between the two groups of aSAH patients.
Raw Data in the Population
A total of 2,012 complete biochemical events were investigated (corresponding to 4,024 samples). Using the averaged values from each patient, the MR and LOI values were found significantly lower and higher, respectively, in the unfavorable group than those in the favorable outcome (p = 0.0001 and p < 0.0001, respectively) (Table 2). For arterial lactate, jugular venous lactate, JaDL, SjVO2, and avDO2, a statistically significant difference was found between the unfavorable and favorable outcome groups (Table 2).
Designing Cutoffs
Table 3 shows the mean of the 25 % lowest values for MR (MR min) and minimal SjVO2 (SjVO2 min) and the mean of the 25 % highest values for LOI (LOI max) and maximal SjVO2 (SjVO2 max). The ROC curves were generated from these values. We determined the cutoff values which reached the best area under the curve (AUC) for the LOI and MR (0.08 and 3.35, respectively; Table 3). We were unable to find any cutoff value for SjVO2. For further studies concerning the prediction of the outcome, we decided to set the cutoff at 55 and 75 %, respectively.
Predictors of the Outcome
A 2,012 results were recorded according to outcome group (GOS 1 = 718, GOS 2 = 176, GOS 3 = 356, GOS 4 = 356, GOS 5 = 406 biochemical events). Percentages of events of decreased MR (<3.35), increased LOI (>0.08) and SjVO2 (≤55 and ≥75 %) are presented according to outcome at 12 months after aSAH (Fig. 1). Favorable outcome was generally associated with fewer events of decreased MR, fewer events of increased LOI, and fewer events of increased SjVO2, in comparison with the poor outcome. For non-survivors, about 40 and 50 % of the biochemical events were characterized by increased LOI and SjVO2 values, respectively, whereas more than 20 % were characterized by a decreased MR (Fig. 1). This decreased MR in unfavorable outcome was associated with an increased avDgluc compared with favorable outcome [0.43 (0.33–0.63) and 0.35 (0.33–0.46), respectively, p < 0.0001] but also with a decreased avDO2 [1.07 (0.84–1.41) and 2.0 (1.93–2.46), respectively, p < 0.0001].
Percentage of events with MR <3.35 (a), with LOI >0.08 (b), with SjVO2 ≤55 and ≥75 % (c, d) according to outcome at 12 months. The percentage of events with metabolic ratio (MR < 3.35, a), lactate oxygen index (LOI > 0.08, b), and jugular venous saturation of oxygen [SjVO2 (≤55 and ≥75 %), c, d] is shown according to the Glasgow Outcome Scale at 12 months after aSAH. Overall, there was a decrease in the frequency of biochemical events with low MR and high LOI from unfavorable (GOS 1–3) to favorable (GOS 4–5) outcome. In patients with full recovery, the frequency of biochemical events with low MR is less than 5 %. Whereas the frequency of elevated SjVO2 was high in our cohort, the frequency of low SjVO2 was inferior to 10 %. In unfavorable outcome, we found lower SjVO2 ≤55 % and higher SjVO2 ≥75 % than in favorable outcome. Glasgow Outcome Scale: died (GOS 1), vegetative status (GOS 2), severe disability (GOS 3), moderate disability (GOS 4), good recovery (GOS 5)
Confirming these global observations, we found that the number of decreased MR events was significantly different between the unfavorable and favorable outcome groups [5 (4–8) vs. 1 (0–1.5), p < 0.0001]. The number of events with LOI >0.08 and SjVO2 ≥75 % was higher in the group with unfavorable outcome than in the group with favorable outcome [9.5 (3–13.5) vs. 1.5 (0–3), p < 0.0001 and 14 (8.5–19) vs. 7.5 (4–12.5), p = 0.0029, respectively]. Using a multiple regression analysis, we tested the numbers of MR, LOI, SjVO2, age, and WFNS to predict outcome. Only MR values were predictive of a poor outcome (p < 0.0001).
Using ROC curves, we confirmed the results obtained by multiple regression analysis: patients experiencing at least three events of MR <3.35 were likely to have a poor outcome whereas we did not find any cutoff value with sensitivity and specificity higher than 80 % for the number of LOI events (Fig. 2). Finally, the number of SjVO2 was too unspecific to predict the outcome.
ROC curves of numbers of metabolic ratio (Nb MR < 3.35), lactate oxygen index (Nb LOI > 0.08), and jugular venous saturation of oxygen (Nb SjVO2 ≤55 and ≥75 %). Patients experiencing at least three events of MR <3.35 were likely to have a poor outcome, the sensitivity, the specificity, and the area under the curve being at 90, 82.1, and 0.88 %, respectively. None of the others biomarkers reach enough sensitivity and specificity up to 80 %. ROC receiver operating characteristic
For non-survivors, we observed that the number of MR <3.35 and LOI >0.08 events was significantly higher than for survivors [5 (0–17) vs. 1.5 (0–19), p = 0.0009 and 10 (2–53) vs. 2 (0–46), p = 0.0001, respectively]. However, no difference was seen between these two groups regarding the number of SjVO2 ≤55 % and SjVO2 ≥75 % events (p = 0.55 and p = 0.30, respectively).
MR and Lactate
Abnormal brain lactate production (JaDL greater than the 97.5th percentile of normal for awake humans, i.e., 0.20 mmol/L, Gibbs 1942) was not uncommon, occurring in 194 of the 2,012 biochemical events we reported (9.6 %). This phenomenon was uncommon in good outcome patients (4 %) and more present in the unfavorable outcome group (13 %). The jugular venous lactate and JaDL values were higher in the group of patients with MR <3.35 than in the group of patients with normal MR [1.15 (0.97–1.51) vs. 1.08 (0.90–1.36), p = 0.0001 and 0.1 (0.03–0.15) vs. 0.07 (0.03–0.13), p = 0.0036, respectively]. In the aSAH cohort, 161 of the 2,012 JaDL values were negative, indicating brain uptake of lactate, and 50 out of the 68 patients (74 %) had at least one episode of brain lactate uptake. Lactate uptake events were reported more frequently in the favorable than in the unfavorable outcome group (11.8 vs. 6.2 %, respectively). However, lactate uptake likely linked to RH was more frequent in the unfavorable outcome group (26.9 vs. 8.4 %).
MR and Cerebral Vasospasm
Cerebral vasospasm was detected in 34 patients (50 %). Nine patients were excluded due to early vasospasm before the jugular catheter was inserted. Among the 25 remaining patients, the outcome was favorable in 10 patients whereas it was unfavorable in the 15 other patients.
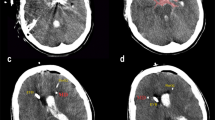
Near the detection time of the cerebral vasospasm, the MR was significantly decreased in comparison to the previous sample collected 8 h earlier [3.60 (3.09–4.81) vs. 5.76 (4.49–8.99), respectively, p = 0.0001]. After diagnosis and treatment of cerebral vasospasm, the MR generally increased, returning to initial values, although the values could be divided into two classes (low MR and normal MR) 32 h after cerebral vasospasm diagnosis and treatment as indicated by box plots in Fig. 3a–c.
MR values and cerebral vasospasm (CV) in favorable outcome (a), unfavorable outcome (b), and dead patients (c). MR values were represented before, during, and after detection and treatment of CV, in the favorable outcome group (a), in the unfavorable outcome group (b), and in died patients (c). Overall, MR is significantly decreased during the CV. In unfavorable (GOS 1–3) and in died patients, the decrease is more pronounced in the time than in favorable outcome (GOS 4–5). BCV before CV, T0CV time of diagnostic and treatment of CV, T1CV T0CV + 8 h, T2CV T0CV + 16 h, T3CV T0CV + 24 h, T4CV T0CV + 32 h, GOS Glasgow Outcome Scale
In the favorable outcome group, the decrease in the MR at the detection time of cerebral vasospasm was reported with a median statistically lower in comparison with baseline values [3.94 (3.26–5.36) vs. 5.90 (4.53–6.69), respectively, p = 0.004]. However, this decrease was not found in the following samples (Fig. 3a). In the unfavorable outcome group, the decrease in the MR was clearly shown with a median statistically lower at the time of detection of cerebral vasospasm in comparison with baseline values [3.60 (2.54–4.70) vs. 5.72 (4.57–9.66), respectively, p = 0.001]. Moreover, this decrease remained significant 8 h after the detection and treatment of cerebral vasospasm, with values mostly below the cutoff of 3.35. Finally, MR medians at following points increased and returned to normal values. However, the values obtained 32 h after cerebral vasospasm remained statistically lower than the baseline values (p = 0.04), highlighting that half of patients exhibited values below the cutoff of 3.35 (Fig. 3b). For these 15 patients, cerebral infarction was detected in all patients after cerebral vasospasm detection and death occurred in eight patients. Based only on the eight patients who died, the MR tended to be more decreased 8 h after cerebral vasospasm detection and treatment (Fig. 3c).
Discussion
Summary of Findings
Among the advantages provided by this study, it is worth to mention the clinical homogeneity of our poor-grade aSAH cohort, the high number of patients (n = 68) and of corresponding biochemical events (n = 2,012) recorded. Reproducible analysis of glucose measurement enabled the MR to be assessed and proposed as a marker of cerebral metabolism in aSAH patients for whom jugular and arterial samples were obtained. The major finding was that a decrease in the MR is predictive of a poor outcome in poor-grade aSAH patients. The frequency of MR decrease events was significantly associated with an unfavorable outcome. Moreover, in patients who developed a cerebral vasospasm, the MR decreased concomitantly with the development of vasospasm and lasted longer in patients with more severe outcomes.
Characteristics of the Population
In poor-grade SAH patients, many factors are likely to contribute to severe brain injury such as global cerebral edema, vasospasm, and cortical spreading depolarization. These conditions are known to increase the risk of mortality and to worsen the long-term functional outcome [18, 19]. In our study, 41 % of the patients achieved a favorable outcome at 12 months (GOS 4–5), while 38 % died and 21 % survived in a vegetative state or with a severe disability. Overall, these data are similar to those obtained in larger studies performed to predict the outcome at discharge in poor-grade aSAH patients. In a recent North-American study, in which a subgroup of 288 poor-grade (Hunt and Hess IV-V) aSAH patients was used, 36.8 % achieved a good outcome (GOS 4–5) and 40.9 % died [20]. However, the authors highlighted a limit of their study since the outcome could be measured at the first post-discharge clinical appointment (follow-up between 30 and 120 days post-SAH) or upon discharge when post-discharge follow-up was not available [21]. In our study, patients without assessment at 12 months were systematically excluded. In a recent Japanese study, 34 % of the 283 poor-grade (WFNS IV–V) aSAH patients included achieved a favorable outcome at discharge, whereas the mortality rate was only 23.7 % [22].
Oxygen, Glucose, and Lactate Metabolism
After aSAH, secondary oxidative stress causes mitochondrial damage and a dysfunction of oxidative phosphorylation leading to anaerobic glycolysis and acidosis [23]. Impairment of oxidative metabolism can lead or be linked to an increase in cerebral glycolysis for ATP synthesis.
It is known that lactate brain concentrations are modified in case of brain injury [24]. In the past, it was generally admitted that lactate rose in the jugular vein in response to ischemic insults [25]. This contributed to the use of LOI and JaDL as markers of ischemic insult, reflecting anaerobic lactate metabolism. However, more recent studies suggested that activated astrocytes modify lactate transport and its release into the blood [26]. It is now generally accepted that, in the brain, lactate is transported across cellular membranes by diffusion and also mediated by mono carboxylic acid transporters [27]. Lactate brain transfer is therefore conditioned by several factors, including its metabolism and the kinetics of its transporters [28–30]. According to the results of this study, it is interesting to note that we found a statistical increase in jugular venous lactate, LOI and/or JaDL in unfavorable outcome patients, with a high brain lactate release (JaDL > 0.2) found in 13 % of the total measurements. This high brain lactate release was found in 31 out of the 40 unfavorable outcome patients. However, it is difficult to claim that an increase in jugular venous lactate is always related to pathological accumulation of lactate, as we detected high levels of JaDL in 4 % of the total measurements and in 11 out of the 28 favorable outcome patients. Lactate increases in the jugular vein are difficult to interpret without measuring cerebral blood flow which provides the right cerebral metabolic rate of lactate (CMRlac) measurement. The lactate level in the jugular vein may be linked to oxygenation and perfusion disorder or related to disorder of its clearance. As previously reported by Oertel et al. [11], an increase in venous lactate was more frequent in RH events. Moreover, in our study, JaDL was also found frequently increased in studies with RH. As these repeated episodes of RH were associated with poor outcome, the concomitant presence of RH and increase in jugular lactate suggests a pathological situation where brain becomes unable to use cerebral lactate as a fuel. When metabolic crisis occurs, it has been shown that glycogen can be converted into lactate and that astrocytic transporters may easily react to this increased lactate flow to provide fuel [31]. In our study, brain lactate uptake occurred statistically more often in favorable than in unfavorable outcome patients (11 vs. 6.2 %) indicating that this source of lactate was efficiently used by the brain to compensate energy failure. Interestingly, Glenn et al. developed a theory with two different scenarios of brain lactate uptake after traumatic brain injury (TBI): in a favorable outcome scenario, uptake of lactate by the brain occurs by facilitated transport from blood in patients with less depressed cerebral metabolic rate of oxygen (CRMO2), and lactate is finally used as a fuel. In an unfavorable outcome scenario, large amounts of arterial lactate enter passively through a damaged blood–brain barrier in patients who have severely depressed CMRO2 [10]. In our study, in an unfavorable outcome scenario, lactate uptake was more often associated with RH and decrease in the avDO2. In the favorable outcome scenario, whereas brain lactate uptake was more frequent, it was rarely associated with RH events.
More recently, a study using microdialysis in 31 SAH patients showed an elevation of brain extracellular lactate more often associated with cerebral hyperglycolysis than with brain hypoxia [32]. In this study, the increase in extracellular lactate was more often associated with hyperglycolysis in patients with better long-term recovery, whereas this lactate increase was more often associated with hypoxia in patients who died. Lactate secondary to aerobic metabolism would be used to supply energy needs of neurons whereas the lactate secondary to anaerobic metabolism would be the result of cell energy failure and neuronal loss. Cerebral glucose metabolism was investigated by two different methods: our approach was general and used the differences between arterial and jugular metabolites, whereas their approach was local and used extracellular brain lactate, pyruvate, and cerebral oxygen. Clearly, a comparative study of aSAH combining these two approaches would be of great interest since they seem to be complementary.
Biomarkers as Predictors of Outcome
Our work confirms previous studies in TBI patients which demonstrated the prognostic importance of acute damage in cerebral oxidative metabolism and how its interaction with glycolysis impacts the long-term outcome [10, 33].
Analyzing data obtained from a large number of repeated measurements performed in individuals is problematic from a statistical point of view. To predict the outcome, we chose to calculate the number of events of pathophysiological phenomenon which can occur at multiple times in a patient, such as LOI and MR. Prior to calculate the number of events, we needed to define the cutoff value for each parameter using ROC curves. A RH was defined as a MR <3.35. This cutoff value for MR (<3.35) was found slightly lower than that designed by Glenn et al. [10] in a prospective TBI study (<3.44), which was further used by Oertel et al. [11] in SAH patients. With our cutoff value, we increased the specificity from 75 to 82.1 % compared with a value of 3.44. This can be explained by the fact that our studied population was different from that of Glenn et al. These authors defined the cutoff of RH using the value below the 2.5th percentile of a normal cohort constituted of 30 healthy volunteer subjects. The cutoff value obtained for LOI (>0.08) in our study was identical to the value previously reported in patients who developed cerebral infarction [23, 34]. Since we did not obtain any value able to give an AUC ≥0.800 for SjVO2, we decided to use the extreme values given by White et al. (55 and 75 %) [35].
We identified at least one event of RH in 83 % of patients and more frequently in unfavorable outcome patients. These events were generally related to both avDO2 decrease and avDgluc increase. However, as avDO2 and avDgluc did not predict accurately the outcome, the use of the MR preferentially to avDO2 or avDgluc alone was justified. A number of three or more RH events during the monitoring of the patient was highly specific and sensitive to predict the outcome, confirming the data obtained by Oertel et al. [11], who suggested that MR values are probably predictive of outcome in a study of 21 different grades in SAH patients.
In this study, as for glucose, the disturbances in lactate concentrations and ratios using lactate were different depending on the outcomes. However, if a statistically significant difference was found in lactate concentrations between poor and favorable outcomes, the number of pathological LOI events did not reach enough sensitivity and specificity, to be considered an reliable biomarker. The LOI is dependent on the JaDL and avDO2 values. The clinical use of the LOI and/or JaDL using jugular bulb catheters remains debated since its interest was shown in ischemic injury in comatose TBI patients [36], with etiologies such as aSAH or cardiovascular disease [25, 37, 38], whereas others studies concluded that the JaDL values did not correlate with increased cerebral lactate concentration measured by cerebral microdialysis [39].
MR and Vasospasm
Early brain injury and vasospasm are likely to be the major causes of death and disability in SAH [40]. In our cohort, the MR was clearly decreased when the vasospasm occurred. We observed that this decrease could be explained by several mechanisms: (1) In some cases, a large increase in avDgluc was associated with a smaller increase in avDO2 (decrease in SjVO2), representing an increase in cerebral glucose and oxygen extraction during cerebral vasospasm. However, other factors could increase cerebral metabolic demand such as seizures or pyrexia. (2) In other cases, the MR decrease was associated with a large decrease in avDO2 (increase in SjVO2). This suggested that brain tissue was unable to extract oxygen from the blood or that a vascular shunt was present, leading to ischemic injury. It was reported that SjVO2 decrease may be frequently associated with hyperemia [35]. Independently, several studies reported that low SjVO2 and high SjVO2 were associated with poorer outcomes after severe head injury [34, 41]. In our population of poor-grade aSAH patients with cerebral vasospasm, the kinetic of MR values was different between the unfavorable and the favorable outcomes. Whereas the MR remained normal for 32 h after the detection of cerebral vasospasm in patients with good recovery, it seems that the MR was decreased for a longer period in unfavorable outcome patients. This point could be used in prospective studies to confirm the occurrence of vasospasm.
Study Limitations
Our study has several limitations: (1) The general measurements that we obtained by jugular venous catheterization may not adequately reflect regional metabolic differences. (2) Measurements were obtained discontinuously every 8 h, which is a limit for parameters with rapid kinetic. (3) Although this single-center cohort is the most important cohort reported which uses catheter jugular biomarkers in poor-grade aSAH patients, other centers should confirm our data before validating them in a prospective cohort and finally proposing this use of the MR as a routine test. (4) Without a direct measurement of cerebral blood flow (i.e., by functional imaging), cerebral metabolism should be cautiously interpreted.
Conclusion
This study confirms the interest of the MR in cerebral glucose metabolism monitoring, especially in poor-grade SAH patients in whom neurological deterioration may happen unrecognized. The MR was shown as a predictor of outcome in poor-grade aSAH patients at 12 months. Poor-grade SAH patients required different monitoring techniques to identify secondary brain insults. Interventional prospective studies should be designed to verify its clinical utility in guiding therapy and its value in early detection of secondary brain injuries that are still potentially reversible, including vasospasm.
References
Hackett ML, Anderson CS. Health outcomes 1 year after subarachnoid hemorrhage: an international population-based study. The Australian Cooperative Research on Subarachnoid Hemorrhage Study Group. Neurology. 2000;55:658–62.
Coppadoro A, Citerio G. Subarachnoid hemorrhage: an update for the intensivist. Minerva Anestesiol. 2011;77:74–84.
Bederson JB, Connolly ES Jr, Batjer HH, Dacey RG, Dion JE, Diringer MN, Duldner JE Jr, Harbaugh RE, Patel AB, Rosenwasser RH. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a statement for healthcare professionals from a special writing group of the Stroke Council, American Heart Association. Stroke. 2009;40:994–1025.
Risselada R, Lingsma HF, Bauer-Mehren A, Friedrich CM, Molyneux AJ, Kerr RS, Yarnold J, Sneade M, Steyerberg EW, Sturkenboom MC. Prediction of 60 day case-fatality after aneurysmal subarachnoid haemorrhage: results from the International Subarachnoid Aneurysm Trial (ISAT). Eur J Epidemiol. 2010;25:261–6.
Wartenberg KE. Critical care of poor-grade subarachnoid hemorrhage. Curr Opin Crit Care. 2011;17:85–93.
Vespa PM. The implications of cerebral ischemia and metabolic dysfunction for treatment strategies in neurointensive care. Curr Opin Crit Care. 2006;12:119–23.
Stuart RM, Claassen J, Schmidt M, Helbok R, Kurtz P, Fernandez L, Lee K, Badjatia N, Mayer SA, Lavine S, Connolly ES. Multimodality neuromonitoring and decompressive hemicraniectomy after subarachnoid hemorrhage. Neurocrit Care. 2011;15:146–50.
Lieutaud T, Dailler F, Artru F, Renaud B. Neurochemical monitoring in neurointensive care using intracerebral microdialysis. In: Westerink BHC, Cremes IFH, editors. Handbook of microdialysis: methods, applications and clinical aspects. 1st ed. London: Elsevier; 2007. p. 659–74.
Le Roux PD, Elliott JP, Newell DW, Grady MS, Winn HR. Predicting outcome in poor-grade patients with subarachnoid hemorrhage: a retrospective review of 159 aggressively managed cases. J Neurosurg. 1996;85:39–49.
Glenn TC, Kelly DF, Boscardin WJ, McArthur DL, Vespa P, Oertel M, Hovda DA, Bergsneider M, Hillered L, Martin NA. Energy dysfunction as a predictor of outcome after moderate or severe head injury: indices of oxygen, glucose, and lacate metabolism. J Cereb Blood Flow Metab. 2003;23:1239–50.
Oertel MF, Schwedler M, Stein M, Wachter D, Scharbrodt W, Schmidinger A, Boker DK. Cerebral energy failure after subarachnoid hemorrhage: the role of relative hyperglycolysis. J Clin Neurosci. 2007;14:948–54.
Teasdale GM, Drake CG, Hunt W, Kassell N, Sano K, Pertuiset B, De Villiers JC. A universal subarachnoid hemorrhage scale: report of a committee of the World Federation of Neurosurgical Societies. J Neurol Neurosurg Psychiatry. 1988;51:1457.
Fisher CM, Kistler JP, Davis JM. Relation of cerebral vasospasm to subarachnoid hemorrhage visualized by computerized tomographic scanning. Neurosurgery. 1980;6:1–9.
Mayberg MR, Batjer HH, Dacey R, Diringer M, Haley EC, Heros RC, Sternau LL, Torner J, Adams HP Jr, Feinberg W, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage. A statement for healthcare professionals from a special writing group of the Stroke Council, American Heart Association. Stroke. 1994;25:2315–28.
Rabinstein AA. The AHA guidelines for the management of SAH: what we know and so much we need to learn. Neurocrit Care. 2009;10:414–7.
Gibbs EL, Lennox WG, Nims LF, Gibbs FA. Arterial and cerebral venous blood: arterial-venous difference in man. J Biol Chem. 1942;144:325–32.
Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet. 1975;1:480–4.
Feigin VL, Lawes CM, Benett DA, et al. Worldwide stroke incidence and early case fatality reported in 56 population-based studies: a systematic review. Lancet. 2009;8:355–69.
Taylor CJ, Robertson F, Brealey D, et al. Outcome in poor grade subarachnoid hemorrhage patients treated with acute endovascular coiling of aneurysms and aggressive intensive care. Neurocrit Care. 2010;14:341–7.
Hunt WE, Hess RM. Surgical risk as related to time of intervention in the repair of intracranial aneurysm. J Neurosurg. 1968;28:14–20.
Naval NS, Chang T, Caserta F, Kowalski RG, Carhuapoma JR, Tamargo RJ. Improved aneurysmal subarachnoid hemorrhage outcomes: a comparison of 2 decades at an academic center. J Crit Care. 2012. doi:10.1016/j.jcrc.2012.05.008.
Shirao S, Yoneda H, Kunitsugu I, et al. Preoperative prediction of outcome in 283 poor-grade patients with subarachnoid hemorrhage: a project of the Chugoku–Shikoku Division of the Japan Neurosurgical Society. Cerebrovasc Dis. 2010;30:105–13.
Robertson CL. Mitochondrial dysfunction contributes to cell death following traumatic brain injury in adult and immature animals. J Bioenerg Biomembr. 2004;36:363–8.
Yang MS, DeWitt DS, Becker DP, Hayes RL. Regional brain metabolite levels following mild experimental head injury in the cat. J Neurosurg. 1985;63:617–21.
Artru F, Dailler F, Burel E, Bodonian C, Grousson S, Convert J, Renaud B, Perret-Liaudet A. Assessment of jugular blood oxygen and lactate indices for detection of cerebral ischemia and prognosis. J Neurosurg Anesthesiol. 2004;16:226–31.
Erlichman JS, Hewitt A, Damon TL, Hart M, Kurascz J, Li A, Leiter JC. Inhibition of monocarboxylate transporter 2 in the retrotrapezoid nucleus in rats: a test of the astrocyte-neuron lactate-shuttle hypothesis. J Neurosci. 2008;28:4888–96.
Bergersen LH. Is lactate food for neurons? Comparison of monocarboxylate transporter subtypes in brain and muscle. Neuroscience. 2007;145:11–9.
Hertz L, Dienel GA. Lactate transport and transporters: general principles and functional roles in brain cells. J Neurosci Res. 2005;79:11–8.
Gandhi GK, Cruz NF, Ball KK, Dienel GA. Astrocytes are poised for lactate trafficking and release from activated brain and for supply of glucose to neurons. J Neurochem. 2009;111:522–36.
Pellerin L, Magistretti PJ. Food for thought: challenging the dogmas. J Cereb Blood Flow Metab. 2003;23:1282–6.
Dienel GA, Hertz L. Astrocytic contributions to bioenergetics of cerebral ischemia. Glia. 2005;50:362–88.
Oddo M, Levine JM, Frangos S, Maloney-Wilensky E, Carrera E, Daniel RT, Leviver M, Magistretti PJ, LeRoux PD. Brain lactate metabolism in humans with subarachnoid hemorrhage. Stroke. 2012;43:1418–21.
Vespa P, Prins M, Ronne-Engstrom E, Caron M, Shalmon E, Hovda DA, Martin NA, Becker DP. Increase in extracellular glutamate caused by reduced cerebral perfusion pressure and seizures after human traumatic brain injury: a microdialysis study. J Neurosurg. 1998;89:971–82.
Gopinath SP, Robertson CS, Contant CF, et al. Jugular venous desaturation and outcome after head injury. J Neurol Neurosurg Psychiatry. 1994;57:717–23.
White H, Baker A. Continous jugular venous oximetry in the neurointensive care unit—a brief review. Can J Anesth. 2002;49:623–9.
Cruz J, Hoffstad OJ, Jaggi JL. Cerebral lactate–oxygen index in acute brain injury with acute anemia: assessment of false versus true ischemia. Crit Care Med. 1994;22:1465–70.
Robertson CS, Narayan RK, Gokaslan ZL, Pahwa R, Grossman RG, Caram P Jr, Allen E. Cerebral arteriovenous oxygen difference as an estimate of cerebral blood flow in comatose patients. J Neurosurg. 1989;70:222–30.
Moritz S, Kasprzak P, Woertgen C, Taeger K, Metz C. The accuracy of jugular bulb venous monitoring in detecting cerebral ischemia in awake patients undergoing carotid endarterectomy. J Neurosurg Anesthesiol. 2008;20:8–14.
Poca MA, Sahuquillo J, Vilalta A, Garnacho A. Lack of utility of arteriojugular venous differences of lactate as a reliable indicator of increased brain anaerobic metabolism in traumatic brain injury. J Neurosurg. 2007;106:530–7.
Hasegawa Y, Suzuki H, Sozen T, Altay O, Zang JH. Apoptotic mechanisms for neuronal cells in early brain injury after subarachnoid hemorrhage. Acta Neurochir Suppl. 2011;110:43–8.
Cormio M, Valadka AB, Robertson CS. Elevated jugular venous oxygen saturation after severe head injury. J Neurosurg. 1999;90:9–15.
Acknowledgments
The authors acknowledge the substantial contribution made by the staff of the Neurocritical Care Unit at Lyon University Hospital. We sincerely thank Dr. Benjamin Rich (Unit of Biostatistics, HCL) and Dr. Olivier Dauwalder (Unit of Bacteriology, HCL) for their invaluable assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Barcelos, G.K., Tholance, Y., Grousson, S. et al. Outcome of Poor-Grade Subarachnoid Hemorrhage as Determined by Biomarkers of Glucose Cerebral Metabolism. Neurocrit Care 18, 234–244 (2013). https://doi.org/10.1007/s12028-012-9810-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-012-9810-1