Abstract
Objects: The major causes of death and disability in subarachnoid hemorrhage (SAH) may be early brain injury (EBI) and cerebral vasospasm. Although cerebral vasospasm has been studied and treated by a lot of drugs, the outcome is not improved even if vasospasm is reversed. Based on these data, EBI is considered a primary target for future research, and apoptosis may be involved in EBI after experimental SAH.
Methods: We reviewed the published literature about the relationship between SAH induced EBI and apoptosis in PubMed.
Result: Most available information can be obtained from the endovascular filament perforation animal model. After onset of SAH, intracranial pressure is increased and then cerebral blood flow is reduced. Many factors are involved in the mechanism of apoptotic cell death in EBI after SAH. In the neuronal cells, both intrinsic and extrinsic pathways of apoptosis can occur. Some antiapoptotic drugs were studied and demonstrated a protective effect against EBI after SAH. However, apoptosis in EBI after SAH has been little studied and further studies will provide us more beneficial findings. Conclusions: The study of apoptosis in EBI after experimental SAH may give us new therapies for SAH.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
Introduction
Subarachnoid hemorrhage (SAH) is associated with high mortality, and 12.4% of patients die suddenly before reaching the hospital [1]. These deaths were mostly due to the initial hemorrhage, and no effective treatment is available for brain injury after the hemorrhage [2]. For survivors, early brain injury (EBI) caused by the initial hemorrhage and delayed ischemic neurologic deficits due to cerebral vasospasm are major causes of the subsequent morbidity and mortality [3]. Although cerebral vasospasm has been studied and treated by a lot of drugs during the past several decades, the outcome is not improved by the reversal of vasospasm [4]. Based on these data, EBI is considered a primary target for future research and may be also an important factor in preventing symptomatic vasospasm because EBI may predispose the brain to ischemic injury due to vasospasm.
Recent studies showed that apoptosis is involved in the pathogenesis of EBI after experimental SAH or in a clinical setting [5, 6]. Therefore, it is thought that an antiapoptotic treatment can be one of the therapeutic candidates for EBI after SAH. In this review, we focus on the relationship between EBI after SAH and apoptotic mechanism in neuronal cells.
Pathophysiology of Early Brain Injury
Most available information about EBI after SAH comes from endovascular filament perforation animal models, which show a high mortality and acute metabolic changes similar to clinical settings [7–9]. Intracranial pressure (ICP) in this model was increased to 40mmHg immediately after SAH and then decreased to plateau (15–25mmHg), whereas cerebral perfusion pressure was decreased to 35–40mmHg from 70mmHg, cerebral blood flow (CBF) was 20–30% decreased from the baseline after SAH induction, and then each of the values were gradually recovered [10]. Interestingly, the mortality rate was 100% when CBF was reduced to less than 40% of the baseline for 60min after SAH, while less CBF reduction resulted in 19% mortality [11].
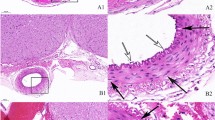
Many factors, such as global ischemia [12], microcirculatory disturbance [11], and subarachnoid blood toxicity [13] are involved in apoptosis-related mechanisms in EBI after SAH (Fig.1), whereas distribution of apoptotic cell death is controversial [12, 14]. Although apoptotic cell death detected by TUNEL was seen in both the cortex and subcortex, neuronal cell death in the hippocampus, which is related to global ischemia, might depend on ICP [6, 14]. Blood immediately spreads in the subarachnoid space after SAH, and then the cerebral cortex is covered with a thick blood clot. Hemoglobin is metabolized by neurons and microglia [15], and the released iron induces apoptosis via lipid peroxidation. Thus, subarachnoid blood clotting, which has been linked to cell injury and oxidative stress [13], may cause greater apoptotic cell death in the cerebral cortex compared with the subcortex.
Apoptotic cell death has been reported to occur in neurons [13, 16, 17] and endothelial cells [18–20] in EBI after SAH, and both of them may be correlated with brain edema [21]. In this review, we focus on neuronal cell apoptosis, which consists of the intrinsic and extrinsic pathways [22] (Fig.2).
Intrinsic Mechanisms of Apoptosis and SAH
Caspase-Dependent Pathway
The intrinsic pathway (mitochondrial pathway), which is mediated by the Bcl-2 family, starts with the increase of outer mitochondrial membrane permeability. The change of membrane leads to the leakage of mitochondrial proteins, including cytochrome c. Cytochrome c is translocated from mitochondria to the cytosolic compartment and interacts with apoptotic protease, activating factor-1, forming the apoptosome and leading to caspase-9 activation. Caspase-9, which is an initiator of the cytochrome c-dependent cascade, activates caspase-3, and results in DNA damage [23]. Caspase-3 is well known as one of the effectors of apoptosis, and cleaved caspase-3 was upregulated in the hippocampus and cortex after SAH [12, 24, 25].
It has been reported that some protein kinases might directly interact with mitochondrial proteins in cerebral ischemia, and their role mainly concentrates on the phosphorylation of pro- and anti-apoptotic proteins (Bad, Bax, Bcl-2, Bcl-xL) [26]. Akt (protein kinase B) and mitogen-activated protein kinase (MAPK) were the best studied of them in EBI after SAH. Akt, which is a serine/threonine kinase, is a key antiapoptotic signaling downstream of phosphoinositide 3-kinase (PI3K) in a growth factor mediated signaling cascade. Stimulation of receptor tyrosine kinases or GTP-binding protein-coupled receptors activates Akt via PI3K, and activated Akt modulates many substrates, including Bax, Bad, glycogen synthase kinase-3, apoptosis signal-regulating kinase 1, and caspase-9, which inhibit apoptosis [27]. Moreover, Akt has also been shown to promote cyclic AMP response element-binding protein (CREB) phosphorylation and lead to Bcl-2 induction [28]. Decreased Akt activity is involved in ischemic neuronal cell death, and Akt activation is a principal factor in the prevention of apoptosis via the caspase-dependent pathway in cerebral ischemia [29–31].
Recent studies suggested that Akt might be involved in the mechanism for EBI after SAH, and this conclusion was drawn from using a PI3K inhibitor, which prevented phosphorylation of Akt and increased DNA damage [14, 32]. Moreover, Akt activation by overexpression of copper/zinc-superoxide dismutase (SOD1), which is one of the antioxidant enzymes, attenuated EBI caused by SAH [32]. Timing of Akt phosphorylation after SAH depended on brain regions; Akt were rapidly phosphorylated in the cortex, but it took 24h to phosphorylate Akt in the hippocampus [14]. Since EBI after SAH may be the most severe in the cortex, it is suggested that Akt phosphorylation depends on the severity of brain injury [14].
The roles of MAPKs are very important in EBI after SAH [33]. MAPK, including extracellular signal-regulated kinase (ERK), c-Jun N-terminal kinase (JNK) and p38, is involved in the survival and apoptotic responses in certain cell death paradigms in cerebral ischemia [34]. These kinases are activated by various stimulants, including vascular endothelial growth factor (VEGF), oxidative stress, and inflammatory cytokines [35–38]. After SAH in a perforation model, these kinases were phosphorylated and induced brain edema, continuous high ICP, and high mortality [33, 39, 40]. Since ERK is activated in response to growth and differentiation factors and might be part of the survival pathway, whether activation of ERK is protective or detrimental to neurons in cerebral ischemia is controversial [41]. In contrast, JNK and p38 are activated in response to inflammatory cytokines and cellular stress, which were highly elevated in the cerebrospinal fluid and in cerebral arteries after SAH [42, 43]. JNK phosphorylates c-Jun, which upregulates apoptotic cascades by inducing expression of the proapoptotic member of Bcl-2 family Hrk/DP5, Bim, and Fas [44, 45]. Phosphorylated JNK and expression of c-Jun were increased after SAH induction and c-Jun mRNA were upregulated in the rat cerebral cortex and hippocampus after SAH [46, 47]. p38 activation by TNF-α and IL-1β was associated with neuronal death, and suppression of p38 activation by Bcl-2 suggested that p38 might be involved in apoptosis [48, 49].
Caspase-Independent Pathway
The caspase-independent component of the intrinsic pathway is carried out by the mitochondria-released apoptosis-inducing factor (AIF), endonuclease G and Bcl-2/adenovirus E1B 19kDa-interacting protein (BNIP3) [50]. AIF, which is the best studied among them, is normally in the mitochondrial intermembrane space and is translocated to the nucleus by some stimulations, inducing large-scale DNA fragmentation and cell apoptosis, which is independent of caspase activity [51]. Nuclear AIF upregulation was reported in cerebral ischemia [52], and the translocation might be triggered by poly (ADP-ribose) polymerase activity [53]. There has not been much reported about AIF expression in EBI after SAH and it is not clear which compartment of AIF expression increases [24].
Oxidative Stress and Early Brain Injury
It is important to hold the balance between reactive oxygen species (ROS) and antioxidants, which control oxidative stress. ROS such as superoxide anion (O− 2 -), hydrogen peroxide (H2O2), and hydroxyl radical (OH−-) are generated at low levels and play important roles in signaling pathways [54]. Under normal conditions, they are regulated by endogenous antioxidants including SOD, glutathione peroxidase, glutathione, and catalase [55]. Overproduction of ROS and/or inactivation of antioxidants cause tissue injury from oxidative damage [54]. Oxidative stress can play important roles in the pathogenesis of EBI after SAH [56]. Mitochondria disruption, the production of hydroxyl radicals from extravasated hemoglobin, and disruption of the intrinsic antioxidant systems have all been reported in either experimental or human SAH [56–59]. O2 −- production was observed 1h after SAH, and overexpression of SOD1 inhibited the production and reduced apoptotic cell injury after SAH [32]. The reduction in oxidative stress by SOD1 overexpression attenuated EBI after SAH via activation of Akt [32].
DNA Damage
p53 is a tumor suppressor gene involved in the regulation of apoptosis [60]. Responding to cell damage, p53 upregulates proapoptotic molecules including Bax, p53-upregulated modulator of apoptosis, and Bid, and downregulates antiapoptotic molecules Bcl-2 and Survivin [60]. p53 is upregulated after an ischemia insult and induces mitochondrial damage and activation of caspases [61]. It was reported that in SAH, p53 is one of the key factors in neuronal cell death. p53 was upregulated both at 24 and 72h after SAH, and p53 inhibitor decreased brain edema and neuronal cell death [24, 62, 63].
Extrinsic Pathway of Apoptosis
The death receptors, which are located on the cell surface, are involved in the extrinsic apoptosis pathway [31]. The receptor ligands expression, including Fas and tumor necrosis factor (TNF), are upregulated after cerebral ischemia [64, 65]. The death receptors can activate caspase-8 or -10, which then directly activate caspase-3 or cause Bid/Bax activation, inducing cytochrome c release [66]. Moreover, forkhead transcriptional factors were activated after cerebral ischemia and then expression of Fas ligand increased, resulting in neuronal cell death [67]. However, little is known regarding the relationship between EBI and death receptors or their ligands, whereas TNF-α were upregulated after SAH [68].
Treatments
Studies of neuronal apoptosis are summarized in Table1. For evaluating neuronal apoptosis in EBI after SAH, neurological examination should be needed to examine the outcome of neuronal cell injury. These molecular apoptotic pathways in neurons may induce brain edema, neurological deficit, and higher mortality. Previous studies showed that apoptotic related pathway modulation by treatment could improve the outcome in EBI after SAH.
Conclusion
A lot of studies have demonstrated the apoptosis mechanism in cerebral ischemia, whereas relatively few have studied the relationship between apoptosis and SAH, especially in EBI. It would be helpful for us to study the relationship between SAH and another apoptotic mechanism, including autophagy and endoplasmic reticulum stress, which may lead to novel therapies in EBI. Studies regarding EBI after SAH are limited, and further studies are needed for clarifying the exact mechanism. For example, MAPKs, including ERK, JNK, and p38, were reported to induce apoptosis in the brain and cerebral artery after SAH [33], whereas it has reported that ERK phosphorylation induced a beneficial effect on cerebral vasospasm [74]. It is suggested that elevated ERK phosphorylation blocks apoptosis by enhancing the antiapoptotic protein Bcl-2 via CREB activation in cerebral ischemia [41]. The opposite effects may depend on the localization in the brain including neurons, glia, and endothelial cells.
In conclusion, apoptosis may play an important role in EBI after SAH. Further studies regarding apoptosis may lead to the development of new therapies and the improvement of outcome of SAH patients.
References
Huang J, van Gelder JM. The probability of sudden death from rupture of intracranial aneurysms: a meta-analysis. Neurosurgery 2002;51:1101–5.
O’Hare TH. Subarachnoid hemorrhage: a review. J Emerg Med. 1987;5:135–4
Tseng MY, Czosnyka M, Richards H, Pickard JD, Kirkpatrick PJ. Effects of acute treatment with pravastatin on cerebral vasospasm, autoregulation, and delayed ischemic deficits after aneurysmal subarachnoid hemorrhage: a phase II randomized placebo-controlled trial. Stroke 2005;36:1627–32.
Schievink WI, Riedinger M, Jhutty TK, Simon P. Racial disparities in subarachnoid hemorrhage mortality: Los Angeles County, California, 1985–1998. Neuroepidemiology 2004;23:299–305.
Nau R, Haase S, Bunkowski S, Brück W. Neuronal apoptosis in the dentate gyrus in humans with subarachnoid hemorrhage and cerebral hypoxia. Brain Pathol. 2002;12:329–36.
Prunell GF, Mathiesen T, Diemer NH, Svendgaard NA. Experimental subarachnoid hemorrhage: subarachnoid blood volume, mortality rate, neuronal death, cerebral blood flow, and perfusion pressure in three different rat models. Neurosurgery 2003;52:165–75.
Bederson JB, Germano IM, Guarino L. Cortical blood flow and cerebral perfusion pressure in a new noncraniotomy model of subarachnoid hemorrhage in the rat. Stroke 1995;26:1086–91.
Schwartz AY, Masago A, Sehba FA, Bederson JB. Experimental models of subarachnoid hemorrhage in the rat: a refinement of the endovascular filament model. J Neurosci Methods. 2000;96:161–7.
Veelken JA, Laing RJ, Jakubowski J. The Sheffield model of subarachnoid hemorrhage in rats. Stroke 1995;26:1279–83
Török E, Klopotowski M, Trabold R, Thal SC, Plesnila N, Schöller K. Mild hypothermia (33 degrees C) reduces intracranial hypertension and improves functional outcome after subarachnoid hemorrhage in rats. Neurosurgery 2009;65:352–9.
Bederson JB, Levy AL, Ding WH, Kahn R, DiPerna CA, Jenkins AL III et al. Acute vasoconstriction after subarachnoid hemorrhage. Neurosurgery 1998;42:352–62.
Park S, Yamaguchi M, Zhou C, Calvert JW, Tang J, Zhang JH. Neurovascular protection reduces early brain injury after subarachnoid hemorrhage. Stroke 2004;35:2412–7.
Matz PG, Copin JC, Chan PH. Cell death after exposure to subarachnoid hemolysate correlates inversely with expression of CuZn-superoxide dismutase. Stroke 2000;31:2450–9.
Endo H, Nito C, Kamada H, Yu F, Chan PH. Akt/GSK3beta survival signaling is involved in acute brain injury after subarachnoid hemorrhage in rats. Stroke 2006;37:2140–6.
Xi G, Keep RF, Hoff JT. Erythrocytes and delayed brain edema formation following intracerebral hemorrhage in rats. J Neurosurg. 1998;89:991–6.
Matz PG, Fujimura M, Chan PH. Subarachnoid hemolysate produces DNA fragmentation in a pattern similar to apoptosis in mouse brain. Brain Res. 2000;858:312–9.
Matz PG, Fujimura M, Lewen A, Morita-Fujimura Y, Chan PH. Increased cytochrome c-mediated DNA fragmentation and cell death in manganese-superoxide dismutase-deficient mice after exposure to subarachnoid hemolysate. Stroke 2001;32:506–15.
Kimura H, Gules I, Meguro T, Zhang JH. Cytotoxicity of cytokines in cerebral microvascular endothelial cell. Brain Res. 2003;990:148–56.
Meguro T, Klett CP, Chen B, Parent AD, Zhang JH. Role of calcium channels in oxyhemoglobin-induced apoptosis in endothelial cells. J Neurosurg. 2000;93:640–6.
Ogihara K, Zubkov AY, Bernanke DH, Lewis AI, Parent AD, Zhang JH. Oxyhemoglobin-induced apoptosis in cultured endothelial cells. J Neurosurg. 1999;91:459–65.
Bazán NG, Rodríguez de Turco EB. Membrane lipids in the pathogenesis of brain edema: phospholipids and arachidonic acid, the earliest membrane components changed at the onset of ischemia. Adv Neurol. 1980;28:197–205.
Gules I, Satoh M, Nanda A, Zhang JH. Apoptosis, blood-brain barrier, and subarachnoid hemorrhage. Acta Neurochir Suppl. 2003;86:483–7.
Chan PH. Mitochondria and neuronal death/survival signaling pathways in cerebral ischemia. Neurochem Res. 2004;29:1943–9.
Cheng G, Wei L, Zhi-Dan S, Shi-Guang Z, Xiang-Zhen L. Atorvastatin ameliorates cerebral vasospasm and early brain injury after subarachnoid hemorrhage and inhibits caspase-dependent apoptosis pathway. BMC Neurosci. 2009; doi:10,1186/14712202107.
Yan J, Chen C, Hu Q, Yang X, Lei J, Yang Let al., The role of p53 in brain edema after 24 h of experimental subarachnoid hemorrhage in a rat model. Exp Neurol. 2008;214:37–46.
Zhang F, Yin W, Chen J. Apoptosis in cerebral ischemia: executional and regulatory signaling mechanisms. Neurol Res. 2004;26:835–45.
Hemmings BA. Akt signaling: linking membrane events to life and death decisions. Science 1997;275:628–30.
Pugazhenthi S, Nesterova A, Sable C, Heidenreich KA, Boxer LM, Heasley LE et al. Akt/protein kinase B up-regulates Bcl-2 expression through cAMP-response element-binding protein. J Biol Chem. 2000;275:10761–6.
Hasegawa Y, Hamada J, Morioka M, Yano S, Kawano T, Kai Yet al., Neuroprotective effect of postischemic administration of sodium orthovanadate in rats with transient middle cerebral artery occlusion. J Cereb Blood Flow Metab. 2003;23:1040–51.
Hasegawa Y, Morioka M, Hasegawa S, Matsumoto J, Kawano T, Kai Y et al. Therapeutic time window and dose dependence of neuroprotective effects of sodium orthovanadate following transient middle cerebral artery occlusion in rats. J Pharmacol Exp Ther. 2006;317:875–81.
Shioda N, Ishigami T, Han F, Moriguchi S, Shibuya M, Iwabuchi Y et al. Activation of phosphatidylinositol 3-kinase/protein kinase B pathway by a vanadyl compound mediates its neuroprotective effect in mouse brain ischemia. Neuroscience 2007;148:221–9.
Endo H, Nito C, Kamada H, Yu F, Chan PH. Reduction in oxidative stress by superoxide dismutase overexpression attenuates acute brain injury after subarachnoid hemorrhage via activation of Akt/glycogen synthase kinase-3beta survival signaling. J Cereb Blood Flow Metab. 2007;27:975–82.
Kusaka G, Ishikawa M, Nanda A, Granger DN, Zhang JH. Signaling pathways for early brain injury after subarachnoid hemorrhage. J Cereb Blood Flow Metab. 2004;24:916–25.
Irving EA, Bamford M. Role of mitogen- and stress-activated kinases in ischemic injury. J Cereb Blood Flow Metab. 2002;22:631–47.
Chakraborti S, Chakraborti T. Oxidant-mediated activation of mitogen-activated protein kinases and nuclear transcription factors in the cardiovascular system: a brief overview. Cell Signal. 1988;10:675–83.
Chow J, Ogunshola O, Fan SY, Li Y, Ment LR, Madri JA. Astrocyte-derived VEGF mediates survival and tube stabilization of hypoxic brain microvascular endothelial cells in vitro. Brain Res Dev Brain Res. 2001;130:123–32.
Parker LC, Luheshi GN, Rothwell NJ, Pinteaux E. IL-1 beta signalling in glial cells in wildtype and IL-1RI deficient mice. Br J Pharmacol. 2002;136:312–20.
Sugden PH, Clerk A. “Stress-responsive” mitogen-activated protein kinases (c-Jun N-terminal kinases and p38 mitogen-activated protein kinases) in the myocardium. Circ Res. 1998;83:345–52.
Sozen T, Tsuchiyama R, Hasegawa Y, Suzuki H, Jadhav V, Nishizawa Set al., Role of interleukin-1beta in early brain injury after subarachnoid hemorrhage in mice. Stroke 2009;40:2519–25.
Yatsushige H, Ostrowski RP, Tsubokawa T, Colohan A, Zhang JH. Role of c-Jun N-terminal kinase in early brain injury after subarachnoid hemorrhage. J Neurosci Res. 2007;85:1436–48.
Sawe N, Steinberg G, Zhao H. Dual roles of the MAPK/ERK1/2 cell signaling pathway after stroke. J Neurosci Res. 2008;86:1659–69.
Fassbender K, Hodapp B, Rossol S, Bertsch T, Schmeck J, Schütt Set al., Inflammatory cytokines in subarachnoid haemorrhage: association with abnormal blood flow velocities in basal cerebral arteries. J Neurol Neurosurg Psychiatry. 2001;70:534–7.
Hirashima Y, Nakamura S, Endo S, Kuwayama N, Naruse Y, Takaku A. Elevation of platelet activating factor, inflammatory cytokines, and coagulation factors in the internal jugular vein of patients with subarachnoid hemorrhage. Neurochem Res. 1997;22:1249–55.
Kuan CY, Whitmarsh AJ, Yang DD, Liao G, Schloemer AJ, Dong Cet al., A critical role of neural-specific JNK3 for ischemic apoptosis. Proc Natl Acad Sci USA. 2003;100:15184–9.
Yuan J, Yankner BA. Apoptosis in the nervous system. Nature 2000;407:802–9.
Harada S, Kamiya K, Masago A, Iwata A, Yamada K. Subarachnoid hemorrhage induces c-fos, c-jun and hsp70 mRNA expression in rat brain. Neuroreport 1997;8:3399–404.
Kawamura Y, Yamada K, Masago A, Katano H, Matsumoto T, Mase M. Hypothermia modulates induction of hsp70 and c-jun mRNA in the rat brain after subarachnoid hemorrhage. J Neurotrauma. 2000;17:243–50.
Cheng A, Chan SL, Milhavet O, Wang S, Mattson MP. p38 MAP kinase mediates nitric oxide-induced apoptosis of neural progenitor cells. J Biol Chem. 2001;276:43320–7.
Nito C, Kamada H, Endo H, Niizuma K, Myer DJ, Chan PH. Role of the p38 mitogen-activated protein kinase/cytosolic phospholipase A2 signaling pathway in blood-brain barrier disruption after focal cerebral ischemia and reperfusion. J Cereb Blood Flow Metab. 2008;28:1686–96.
Elmore S. Apoptosis: a review of programmed cell death. Toxicol Pathol. 2007;35:495–516.
Cho BB, Toledo-Pereyra LH. Caspase-independent programmed cell death following ischemic stroke. J Invest Surg. 2008;21:141–7.
Li X, Nemoto M, Xu Z, Yu SW, Shimoji M, Andrabi SA, et al. Influence of duration of focal cerebral ischemia and neuronal nitric oxide synthase on translocation of apoptosis-inducing factor to the nucleus. Neuroscience 2007;144:56–65.
Yu SW, Wang H, Poitras MF, Coombs C, Bowers WJ, Federoff HJet al., Mediation of poly(ADP-ribose) polymerase-1-dependent cell death by apoptosis-inducing factor. Science 2002;297:200–1.
Loh KP, Huang SH, De Silva R, Tan BK, Zhu YZ. Oxidative stress: apoptosis in neuronal injury. Curr Alzheimer Res. 2006;3:327–37.
Sugawara T, Chan PH. Reactive oxygen radicals and pathogenesis of neuronal death after cerebral ischemia. Antioxid Redox Signal. 2003;5:597–607.
Ayer RE, Zhang JH. Oxidative stress in subarachnoid haemorrhage: significance in acute brain injury and vasospasm. Acta Neurochir Suppl. 2008;104:33–41.
Asano T. Oxyhemoglobin as the principal cause of cerebral vasospasm: a holistic view of its actions. Crit Rev Neurosurg. 1999;9:303–18.
Gaetani P, Lombardi D. Brain damage following subarachnoid hemorrhage: the imbalance between anti-oxidant systems and lipid peroxidative processes. J Neurosurg Sci. 1992;36:1–10.
Kaynar MY, Tanriverdi T, Kemerdere R, Atukeren P, Gumustas K. Cerebrospinal fluid superoxide dismutase and serum malondialdehyde levels in patients with aneurysmal subarachnoid hemorrhage: preliminary results. Neurol Res. 2005;27:562–7.
Fridman JS, Lowe SW. Control of apoptosis by p53. Oncogene 2003;22:9030–40.
Culmsee C, Mattson MP. p53 in neuronal apoptosis. Biochem Biophys Res Commun. 2005;331:761–77.
Cahill J, Calvert JW, Marcantonio S, Zhang JH. p53 may play an orchestrating role in apoptotic cell death after experimental subarachnoid hemorrhage. Neurosurgery 2007;60:531–45
Gao C, Liu X, Liu W, Shi H, Zhao Z, Chen Het al., Anti-apoptotic and neuroprotective effects of Tetramethylpyrazine following subarachnoid hemorrhage in rats. Auton Neurosci. 2008;141:22–30.
Martin-Villalba A, Herr I, Jeremias I, Hahne M, Brandt R, Vogel J et al. CD95 ligand (Fas-L/APO-1L) and tumor necrosis factor-related apoptosis-inducing ligand mediate ischemia-induced apoptosis in neurons. J Neurosci. 1999;19:3809–17.
Rosenbaum DM, Gupta G, D’Amore J, Singh M, Weidenheim K, Zhang Het al., Fas (CD95/APO-1) plays a role in the pathophysiology of focal cerebral ischemia. J Neurosci Res. 2000;61:686–92.
Yuan J, Horvitz HR. A first insight into the molecular mechanisms of apoptosis. Cell 2004;116(Suppl):53–6
Kawano T, Morioka M, Yano S, Hamada J, Ushio Y, Miyamoto E et al. Decreased akt activity is associated with activation of forkhead transcription factor after transient forebrain ischemia in gerbil hippocampus. J Cereb Blood Flow Metab. 2002;22:926–34.
Ma CX, Yin WN, Cai BW, He M, Wu J, Wang JY, et al. Activation of TLR4/NF-kappaB signaling pathway in early brain injury after subarachnoid hemorrhage. Neurol Res. doi:10,1179/016164109x12445616596283.
Ostrowski RP, Colohan AR, Zhang JH. Mechanisms of hyperbaric oxygen-induced neuroprotection in a rat model of subarachnoid hemorrhage. J Cereb Blood Flow Metab. 2005;25:554–71.
Ostrowski RP, Tang J, Zhang JH. Hyperbaric oxygen suppresses NADPH oxidase in a rat subarachnoid hemorrhage model. Stroke 2006;37:1314–8.
Sugawara T, Jadhav V, Ayer R, Chen W, Suzuki H, Zhang JH. Thrombin inhibition by argatroban ameliorates early brain injury and improves neurological outcomes after experimental subarachnoid hemorrhage in rats. Stroke 2009;40:1530–2.
Ersahin M, Toklu HZ, Cetinel S, Yüksel M, Yeğen BC, Sener G. Melatonin reduces experimental subarachnoid hemorrhage-induced oxidative brain damage and neurological symptoms. J Pineal Res. 2009;46:324–32.
Lu H, Zhang DM, Chen HL, Lin YX, Hang CH, Yin HX, et al. N-acetylcysteine suppresses oxidative stress in experimental rats with subarachnoid hemorrhage. J Clin Neurosci. 2009;16:684–8.
Lin CL, Dumont AS, Tsai YJ, Huang JH, Chang KP, Kwan AL, et al. 17beta-estradiol activates adenosine A(2a) receptor after subarachnoid hemorrhage. J Surg Res. doi:10,3171/20093JNS081660.
Acknowledgments
This study was partially supported by grants (NS053407) from the National Institutes of Health to J.H.Z.
Conflict of interest statement We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2011 Springer-Verlag/Wien
About this paper
Cite this paper
Hasegawa, Y., Suzuki, H., Sozen, T., Altay, O., Zhang, J.H. (2011). Apoptotic Mechanisms for Neuronal Cells in Early Brain Injury After Subarachnoid Hemorrhage. In: Feng, H., Mao, Y., Zhang, J.H. (eds) Early Brain Injury or Cerebral Vasospasm. Acta Neurochirurgica Supplements, vol 110/1. Springer, Vienna. https://doi.org/10.1007/978-3-7091-0353-1_8
Download citation
DOI: https://doi.org/10.1007/978-3-7091-0353-1_8
Publisher Name: Springer, Vienna
Print ISBN: 978-3-7091-0352-4
Online ISBN: 978-3-7091-0353-1
eBook Packages: MedicineMedicine (R0)