Abstract
Background
Myocardial injury after aneurysmal subarachnoid hemorrhage (aSAH) is associated with poor outcomes. Delayed cerebral ischemia (DCI) is also a complication of aSAH. We sought to determine whether (1) DCI could be predicted by demographics, aSAH severity/aneurysm location, or aSAH-associated myocardial injury (SAHMI), and (2) DCI is associated with increased mortality after aSAH.
Methods
Prospective longitudinal study of 149 aSAH subjects with definitive DCI evaluation, age 18–75 years, Hunt and Hess (HH) ≥ 3, and/or Fisher ≥ 2, and admitted to the Neurovascular ICU. DCI was defined by the presence of neurological deterioration accompanied by evidence of abnormal cerebral blood flow.
Results
Subjects were 48% DCI(+) and 52% DCI(−). DCI(+) subjects had more severe aSAH [HH (P = 0.002), Fisher (P = 0.004), admission Glasgow Coma Scale (P = 0.018)]. More DCI(+) subjects had pulmonary congestion than DCI(−) subjects (63 vs. 39%, P = 0.003). On echocardiogram, cardiac output (CO, liters per minute [LPM]) was significantly higher in DCI(+) than in DCI(−) subjects (6 ± 2 vs. 5 ± 1 LPM; P = 0.015). Multivariate analysis identified CO and Fisher grade as independent predictors of DCI (P = 0.02, 0.019). For each 1 LPM increase in CO, the odds of DCI increased by 1.5 (95% CI: 1.1–2.1). Fisher grade 4 increased the odds of DCI by 6.5 compared to Fisher grade 2 (95% CI: 1.6–25.8). After controlling for Fisher grade, CO remained an independent predictor of DCI (P = 0.02). Three-month mortality rate was not significantly different between DCI groups, P = 0.786.
Conclusion
Elevated CO and Fisher grade are predictors of DCI after aSAH. However, prevention of DCI may not decrease mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The annual incidence of aneurysmal subarachnoid hemorrhage (aSAH) is 1 per 10,000 North Americans with an annual hospitalization cost of more than $1.7 billion dollars [1, 2]. Mortality after aSAH remains high during the acute (36% during the first 2 days, 43% during the first week) and prolonged (57% mortality at 1 year) recovery periods [3]. Recent review studies reported overall mortality ranging from 32 to 67% [4, 5]. Demographic and clinical characteristics including the severity of neurological insult may influence recovery after aSAH. We and others have described aSAH-associated myocardial injury (SAHMI), including cardiac arrhythmia, elevated cardiac troponin I (cTnI), depressed left ventricular ejection fraction (LVEF), and myocardial wall motion abnormality (WMA), as a complication associated with poor outcome after aSAH [6, 7]. Delayed cerebral ischemia (DCI) is another complication that has been associated with poor outcomes after aSAH [8]. DCI occurs when there is a mismatch between available blood oxygen and cerebral tissue demand, and is characterized by the presence of neurological deterioration and abnormal cerebral blood flow. DCI can occur as early as 2 days after the onset of aneurysm rupture [9], and may persist throughout hospitalization. Understanding factors associated with the development of DCI may help clinicians to target at-risk individuals and potentially prevent this complication. The aims of this study were to determine whether demographics, aSAH severity and aneurysm location, or the presence of SAHMI predict DCI, and to determine whether DCI was associated with increased aSAH mortality.
Methods
Sample and Setting
The sample consisted of patients diagnosed with aSAH between 3/19/2003 and 3/30/2007 at the University of Pittsburgh Medical Center’s Neurovascular Intensive Care Unit (NICU) and enrolled in NIH R01HL074316. Diagnosis of aSAH was made by computed tomography (CT) and/or cerebral angiogram. Inclusion criteria were: adults 18–75 years of age with a spontaneous aneurysm rupture, Hunt and Hess (HH) score ≥ 3, and/or Fisher grade ≥ 2, and admitted to the Neurovascular ICU. Subjects were excluded if they had a preexisting chronic neurologic disease, traumatic or mycotic aneurysm, or recent myocardial infarction. Subjects were recruited within 5 days of aSAH onset and were followed for up to 14 days after aSAH or until discharge.
Demographic and Clinical Characteristics
Age, race, and gender were obtained from the medical records. Past medical history was obtained by interviewing the patient and/or the family in addition to electronic medical records review. Past medical history was classified by system affected or disease state (cardiac, hypertension, pulmonary, neurologic, cancer, diabetes mellitus, renal failure, gastrointestinal, drug abuse, ethanol abuse, and others).
Severity of Injury and Site of Aneurysm
Aneurysm site, Fisher grade, and HH scores were determined by the attending neurosurgeon. The admission Glasgow coma score (GCS) was obtained from the Emergency Department records (prior to medications).
SAHMI: aSAH-Associated Myocardial Injury
SAHMI was evaluated by the following methods.
12-Lead Electrocardiogram (ECG): The first 12-lead ECG, completed on admission as a part of standard care, was reviewed to detect initial cardiac arrhythmias, QTc prolongation, ischemia, axis deviation, and left ventricular hypertrophy.
Echocardiography: LVEF, WMA, stroke volume (SV), and cardiac output (CO) were assessed using two-dimensional transthoracic echocardiography (Vivid 7 GE, Horten, Norway) performed ≤5 days after the onset of aneurysm rupture. LVEF was calculated using biplane Simpson’s rule and dichotomized with ≥50% as normal. Through a standard 16-segment model, wall motion score (1 = normal, 2 = hypokinesis, 3 = akinesis, and 4 = dyskinesis) was calculated and then used to calculate a wall motion score index (WMSI). WMSI was calculated by averaging the all segmental scores. A WMSI > 1 was considered abnormal and classified as a regional WMA [6].
Pulmonary congestion: Chest X-rays were assessed by attending radiologists for evidence of pulmonary congestion. Any of the following terms in the radiology report was considered as indication for pulmonary congestion: hilar edema, hilar fullness, interstitial edema, pulmonary congestion, or pulmonary edema.
Cardiac troponin I: cTnI was measured with a fluorescent enzyme immunoassay (Bayer Health Care, Tarrytown, NY, USA) during the first 5 days after the onset of aneurysm rupture. The peak cTnI was dichotomized with cTnI ≥ 0.3 ng/ml as abnormal.
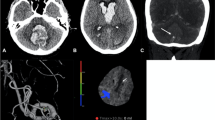
Delayed Cerebral Ischemia
DCI was defined by the presence of clinical neurological deterioration accompanied by evidence of abnormal cerebral blood flow. Neurologic deterioration was determined by the following physical examination changes as documented by the bedside practitioner: (a) decrease in level of consciousness, (b) presence of a new focal neurologic deficit, (c) deterioration in pupillary reaction, or (d) worsening GCS or National Institute of Health Stroke Scale. Causes of neurological deterioration other than vasospasm (i.e., rebleeding, seizures, hydrocephalus, and cerebral edema) were carefully excluded. Any assessment of cerebral blood flow that occurred within 12 h (before, after, or both) of the observed neurologic deterioration was then evaluated. Cerebral blood flow was determined by any of the following three methods. First, transcranial Doppler (TCD) assessments were performed daily, and categorized as indicating abnormal blood flow if (a) mean middle cerebral artery velocity was >120 ml/s; (b) systolic middle cerebral artery velocity was >200 ml/s, or (c) Lindegaard ratio was >3.0. Secondly, any head CT and head CT perfusion scans, which provide accurate and reliable measurement of blood flow [10], obtained within the 12-h temporal window of the clinical deterioration were reviewed for the presence of cerebral ischemia, infarction, or abnormal blood flow. Finally, cerebral angiography studies within the same temporal window were independently reviewed by a neurosurgeon and evaluated for vascular narrowing, with narrowing >25% considered as indication for cerebral vasospasm. Subjects were then categorized as DCI-present “(+)” if they had both neurologic deterioration and one or more indicator of abnormal cerebral blood flow. Conversely, subjects were categorized as DCI-absent “(−)” if they had no evidence of neurologic deterioration and no evidence of abnormal cerebral perfusion on any of the above-mentioned diagnostic modalities. Subjects with a DCI status that could not be definitively determined according to the above definition were excluded.
Mortality
Three-month mortality was determined from review of the medical record or interview of the patient or relatives.
Statistical Analysis
To determine potential predictors of DCI, Exact tests and Fisher’s Exact tests were used for categorical predictors. Mann–Whitney U-test and independent sample Student’s t-test were used for continuous dependent variables. Significant predictors with a P-value less than 0.05 were included in a multivariable binary logistic regression model.
Results
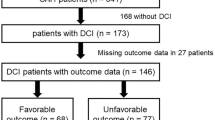
The study sample included 270 subjects, of whom 92 were excluded because of no blood flow information available. Of the remaining 178 subjects, 22 were excluded for the following reasons: (a) blood flow study abnormal but no definitive documentation of clinical neurological deterioration (n = 12), (b) abnormal physical exam but cerebral blood flow indicators were normal (n = 7), or (c) normal physical exam but cerebral blood flow indicators were abnormal (n = 3). Of the remaining 156 subjects, an additional 7 subjects were excluded due to missing data in other variables. The final sample consisted of 149 subjects who were relatively young (53.8 ± 10.5 years), mostly female (76%) and white (87%). The majority of subjects underwent coiling embolization (58%) as aneurysm repair method. 52% of the final sample (n = 78) were DCI(−), and 48% (n = 71) were DCI(+). The blood flow criteria whereby the DCI determinations were made for these 71 subjects are indicated in Table 1.
Comparisons of the demographic characteristics between DCI(+) and DCI(−) subjects are listed in Table 2, which indicates nonsignificant between-group differences in age, gender, race, or past medical history. When the groups were compared on severity of injury and aneurysm site (Table 3), DCI(+) subjects were found to have more severe SAH as measured by HH (P = 0.002), and Fisher grade (P = 0.004), and poorer level of consciousness measured by admission GCS (P = 0.018). However, aneurysm site was not significantly different between the two groups (P = 0.862).
The groups were then compared on variables related to SAHMI. Not all subjects had data available on all SAHMI variables, thus the total number of subjects available for comparison changed for each indicator (Table 4). On the admission ECG (n = 124), subjects with DCI tended to have longer QTc durations [in milliseconds “ms”] (459 ± 43 ms) than subjects without DCI (449 ± 37 ms), but the difference was not significant (P = 0.156).Footnote 1 When QTc was dichotomized (≥470 ms was considered prolonged) the difference remained nonsignificant (P = 0.849). No significant differences were observed between DCI(+) and DCI(−) subjects on the occurrence of admission arrhythmias (P = 0.53), ischemia (P = 0.121), axis deviation (P = 0.244), or left ventricular hypertrophy (P = 0.709).
Echocardiogram data were available in 96 subjects (Table 4). CO (liters per minute [LPM]) was significantly higher in subjects with DCI(+) (6 ± 1.7 LPM) than in subjects with DCI(−) (5 ± 1.3 LPM), P = 0.015. However, neither SV (P = 0.417) nor LVEF (P = 0.713) (see footnote 1) were significantly different between DCI groups. When LVEF was dichotomized (abnormal <50%), the difference between the DCI groups remained nonsignificant (P = 0.597). Although 23% of DCI(+) subjects displayed some degree of abnormal wall motion as compared to only 14% of DCI(−) subjects, the difference was not significant, P = 0.18.
The analysis of chest X-ray data in 148 subjects revealed that 63% of subjects with DCI(+) had pulmonary congestion as compared to only 39% of subjects with DCI(−), P = 0.003. Of the 149 subjects with peak cTnI levels available, DCI(+) subjects showed a trend of being more likely to have a peak cTnI ≥0.3 ng/ml (42%) compared to DCI(−) subjects (27%), P = 0.058.
When examining mortality at 3 months, there were no significant differences between DCI(+) subjects (12%) and DCI(−) subjects (16%), P = 0.786.
The logistic regression (Table 5) showed that CO and Fisher grade were significant predictors of DCI (other predictors in the starting model were GCS, HH, pulmonary congestion, and peak troponin I levels) after aSAH; P = 0.02 and 0.019, respectively. For each 1 LPM increase in the CO, the odds of DCI increased by 1.5 (95% CI: 1.1–2.1). Fisher grade 4 increased the odds of DCI by 6.5 compared to Fisher grade 2 (95% CI: 1.6–25.8). In addition, Fisher grade 3 increased the odds of DCI by 2.6 compared to Fisher grade 2, but this was not statistically significant (95% CI: 0.97–7.1). After controlling for the severity of injury (Fisher grade), CO remained an independent predictor of DCI after aSAH (P = 0.02). The interaction effect between CO and Fisher grade was also tested but was not significant (P = 0.447).
Discussion
The main findings of our study are that elevated CO and Fisher grade 4 predict DCI after aSAH, and that pulmonary congestion and elevated CO are associated with the development of DCI after aSAH.
For this analysis, we defined DCI by the presence of neurological deterioration accompanied by evidence of abnormal cerebral blood flow obtained by any of the three methods mentioned earlier. Recently, DCI has undergone more intense exploration as a cause of poor outcome after aSAH. The incidence of DCI has been reported to range from 19 to 35% [8, 9, 11–15] (although four of these papers [8, 9, 11, 12] were from the same center). However, comparison of DCI prevalence is difficult due to inconsistency of DCI definition in the literature [16]. For example, the lower prevalence of 19% reported by Carrera et al. [9] utilized clinical deterioration and/or new infarct on CT that was not present on admission or in the immediate postoperative period, due to vasospasm as the DCI indicators. Using this same definition, Frontera et al. [8] reported a 21% DCI prevalence rate. The higher DCI prevalence of 35% reported by Dankbaar et al. [15] utilized the following indicators: clinical deterioration lasting for two or more hours, with no evidence of rebleeding or hydrocephalus on CT scan in the absence of other medical causes. Our study utilized a DCI definition of clinical deterioration (decrease in level of consciousness, presence of a new focal neurologic deficit, deterioration in pupillary reaction, worsening GCS or National Institute of Health Stroke Scale scores, none of which could be explained by rebleeding, seizures, hydrocephalus, or cerebral edema) as well as abnormal cerebral blood flow on TCD, CT scan, CT perfusion scan, or angiography. Yet our study reported a higher prevalence of DCI at 48%. This may be explained by our elimination form the analyses of subjects who did not have definitive information available for both clinical examination and accompanying blood flow determination. Retaining these excluded subjects would have enlarged the denominator and produced a smaller DCI prevalence.
Although the mean age for DCI subjects in this study (53 years) was lower than the mean age for DCI subjects in some studies (59 years) [17, 18], it was similar to mean age for DCI subjects (54 years) and overall SAH population (52 years) in other studies [9], and we saw no between-group difference. We did not find a relationship between DCI and other demographic characteristics (Table 2) which is consistent with the literature [8, 13]. These findings suggest that DCI is more likely to develop as a result of the bleeding process rather than being influenced by certain demographic or pre-bleeding clinical characteristics (i.e., past medical history). This hypothesis is supported by the findings of Claassen et al. [12] who reported that a thick clot which fills any fissure is the best predictor of DCI. This is further corroborated by our findings that HH (≥3), Fisher grade (≥2), and admission GCS (<9) were significantly associated with the occurrence of DCI in our sample (Table 3). Likewise, in a study of 580 subjects with spontaneous aSAH, HH score (≥3) has been reported as a risk factor for DCI [8]. In our study, Fisher grade (≥2) remained a significant predictor for DCI in univariate and multivariate analyses, suggesting that the blood load evident on the admission CT scan is a strong predictor of DCI. Hijdra et al. [19] also reported that the amount of subarachnoid blood is the best predictor for DCI, and that an admission GCS <12 and DCI were positively associated (P < 0.01). Other studies reported an association between GCS <12 and death [20]. Moreover, significant association between the duration of unconsciousness (>1 h) and DCI has been reported in the literature [13]. These results suggest that HH, Fisher grade, and GCS are important parameters for predicting DCI, and those patients with high bleeding grades or low GCS scores should be closely monitored for later DCI.
When examining the relationship between indicators of SAHMI and DCI, we did not see a relationship between admission 12-lead ECG variables such as QTc interval, axis deviation, left ventricular hypertrophy, and myocardial ischemia and DCI. Similar findings were reported by Schuiling et al. [21] who concluded that admission ECG abnormalities do not have a predictive value for the DCI except for ST depression. Although ST depression was a predictor for DCI in univariate analysis, its value for prognosticating DCI was not remarkable [21]. We did note a trend that subjects with DCI tended to have elevated peak cTnI (42%) as compared to the subjects without DCI (27%), although this did not demonstrate statistical significance (P = 0.058). The data on the relationship between cTnI and DCI is scant in the literature. Naidech et al. [22] found a significant relationship between elevated cTnI and DCI. Thus, there is conflicting evidence of the association between elevated cTnI and DCI.
To our knowledge, this is the first study that has investigated the relationship between echocardiographic variables and DCI. The only echocardiographic variable that predicted DCI was the elevated CO, which remained a significant predictor in the multivariate analysis even after controlling for the severity of bleeding (Fisher grade). Because SV was not significantly related with DCI, we hypothesize that a tachycardic reflex or stress state might be explanatory for the increased CO. In this study, pulmonary congestion on chest X-ray was significantly associated with DCI. Similar association has been reported in the literature [8]. Although induced hypervolemia may be a cause for pulmonary congestion, a post hoc review of our subjects’ charts did not corroborate excessive fluid administration as a cause. Neurogenic pulmonary congestion has been noticed after aSAH. Although the exact mechanism is still unclear, a hypothesized massive sympathetic discharge forms the basis for explaining neurogenic pulmonary congestion after aSAH [23]. It is possible that the higher CO and pulmonary congestion we noted with DCI only serve as indicators of the stress state, rather than having a direct mechanistic link to the development of DCI.
Our 3-month overall mortality rate was 15%, which is slightly lower but still consistent with that reported by others (16–21%) [7, 24, 25]. Frontera et al. [8] reported significant association between DCI and poor MRS [4–6] score, but DCI was not significantly associated with death or MRS score of 6 [8]. Schutz et al. [26] reported similar results using Glasgow Outcome Score (GOS). They reported that DCI has no impact on case fatality ratio; however, they found significant difference on the incidence of DCI between subjects with poor GOS [2, 3] and good GOS [4, 5], P < 0.001. Thus, DCI seems to be related to poor functional recovery, but not death per se. Our study confirms that DCI is not significantly associated with mortality.
Conclusion
There is little agreement on how to define DCI in the literature, which makes the comparison between our study findings and others’ difficult. Under the current definition of DCI we have utilized, we have demonstrated that blood load on CT scan (Fisher grade) and elevated CO are predictors for DCI after aSAH. Further studies are needed to determine if the relationship between DCI and CO is causal or coincidental. In this study, as well as in other studies, the amount of bleeding has been found to be linked to DCI. This may suggest that early interventions to counteract the bleeding process may be a key factor in DCI prevention. Further, the prevention of DCI may not decrease mortality after aSAH.
Notes
Student’s t-test results were consistent with Mann–Whitney U-test results.
References
King JT Jr. Epidemiology of aneurysmal subarachnoid hemorrhage. Neuroimaging Clin N Am. 1997;7:659–68.
Wiebers DO, Torner JC, Meissner I. Impact of unruptured intracranial aneurysms on public health in the United States. Stroke. 1992;23:1416–9.
Bonita R, Thomson S. Subarachnoid hemorrhage: epidemiology, diagnosis, management, and outcome. Stroke. 1985;16:591–4.
Hop JW, Rinkel GJ, Algra A, van Gijn J. Case-fatality rates and functional outcome after subarachnoid hemorrhage: a systematic review. Stroke. 1997;28:660–4.
Ingall T, Asplund K, Mahonen M, Bonita R. A multinational comparison of subarachnoid hemorrhage epidemiology in the WHO MONICA stroke study. Stroke. 2000;31:1054–61.
Hravnak M, Frangiskakis JM, Crago EA, et al. Elevated cardiac troponin I and relationship to persistence of electrocardiographic and echocardiographic abnormalities after aneurysmal subarachnoid hemorrhage. Stroke. 2009;40:3478–84.
Crago EA, Kerr ME, Kong Y, et al. The impact of cardiac complications on outcome in the SAH population. Acta Neurol Scand. 2004;110:248–53.
Frontera JA, Fernandez A, Schmidt JM, et al. Defining vasospasm after subarachnoid hemorrhage: what is the most clinically relevant definition? Stroke. 2009;40:1963–8.
Carrera E, Schmidt JM, Oddo M, et al. Transcranial Doppler for predicting delayed cerebral ischemia after subarachnoid hemorrhage. Neurosurgery. 2009;65:316–23. discussion 23-4.
Wintermark M, Thiran JP, Maeder P, Schnyder P, Meuli R. Simultaneous measurement of regional cerebral blood flow by perfusion CT and stable xenon CT: a validation study. AJNR Am J Neuroradiol. 2001;22:905–14.
Carrera E, Schmidt JM, Oddo M, et al. Transcranial Doppler ultrasound in the acute phase of aneurysmal subarachnoid hemorrhage. Cerebrovasc Dis. 2009;27:579–84.
Claassen J, Bernardini GL, Kreiter K, et al. Effect of cisternal and ventricular blood on risk of delayed cerebral ischemia after subarachnoid hemorrhage: the Fisher scale revisited. Stroke. 2001;32:2012–20.
Hop JW, Rinkel GJ, Algra A, van Gijn J. Initial loss of consciousness and risk of delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage [see comment]. Stroke. 1999;30:2268–71.
Vergouwen MD, van Geloven N, de Haan RJ, Kruyt ND, Vermeulen M, Roos YB. Increased cortisol levels are associated with delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. Neurocrit Care. 2010;12:342–5.
Dankbaar JW, Rijsdijk M, van der Schaaf IC, et al. Relationship between vasospasm, cerebral perfusion, and delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. Neuroradiology. 2009;51:813–9.
van der Bilt IA, Hasan D, Vandertop WP, et al. Impact of cardiac complications on outcome after aneurysmal subarachnoid hemorrhage: a meta-analysis. Neurology. 2009;72:635–42.
Rijsdijk M, van der Schaaf IC, Velthuis BK, Wermer MJ, Rinkel GJ, Rinkel GJE. Global and focal cerebral perfusion after aneurysmal subarachnoid hemorrhage in relation with delayed cerebral ischemia. Neuroradiology. 2008;50:813–20.
van der Schaaf I, Wermer MJ, van der Graaf Y, et al. CT after subarachnoid hemorrhage: relation of cerebral perfusion to delayed cerebral ischemia. Neurology. 2006;66:1533–8.
Hijdra A, van Gijn J, Nagelkerke NJ, Vermeulen M, van Crevel H. Prediction of delayed cerebral ischemia, rebleeding, and outcome after aneurysmal subarachnoid hemorrhage. Stroke. 1988;19:1250–6.
Ramappa P, Thatai D, Coplin W, et al. Cardiac troponin-I: a predictor of prognosis in subarachnoid hemorrhage. Neurocrit Care. 2008;8:398–403.
Schuiling WJ, Algra A, de Weerd AW, Leemans P, Rinkel GJ, Rinkel GJE. ECG abnormalities in predicting secondary cerebral ischemia after subarachnoid haemorrhage. Acta Neurochir. 2006;148:853–8. discussion 8.
Naidech AM, Kreiter KT, Janjua N, et al. Cardiac troponin elevation, cardiovascular morbidity, and outcome after subarachnoid hemorrhage. Circulation. 2005;112:2851–6.
Friedman JA, Pichelmann MA, Piepgras DG, et al. Pulmonary complications of aneurysmal subarachnoid hemorrhage. Neurosurgery. 2003;52:1025–31. discussion 31–32.
Frontera JA, Parra A, Shimbo D, et al. Cardiac arrhythmias after subarachnoid hemorrhage: risk factors and impact on outcome. Cerebrovasc Dis. 2008;26:71–8.
Frangiskakis JM, Hravnak M, Crago EA, et al. Ventricular arrhythmia risk after subarachnoid hemorrhage. Neurocrit Care. 2009;10:287–94.
Schutz H, Krack P, Buchinger B, et al. Outcome of patients with aneurysmal and presumed aneurysmal bleeding. A hospital study based on 100 consecutive cases in a neurological clinic. Neurosurg Rev. 1993;16:15–25.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yousef, K., Crago, E., Kuo, CW. et al. Predictors of Delayed Cerebral Ischemia After Aneurysmal Subarachnoid Hemorrhage: A Cardiac Focus. Neurocrit Care 13, 366–372 (2010). https://doi.org/10.1007/s12028-010-9408-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-010-9408-4