Abstract
Objective
To determine whether routine electroencephalography (EEG) detected electrical status epilepticus (ESE), masked by neuromuscular blockade, in comatose cardiac-arrest survivors receiving therapeutic hypothermia.
Design
Prospective 3-year study
Setting
Medical ICU
Patients
Fifty-one consecutive comatose cardiac-arrest patients treated between May 2005 and May 2008 using a standardized protocol of hypothermia with neuromuscular blockade.
Intervention
EEG was performed routinely as soon as possible after starting therapeutic hypothermia. EEG recordings were read by an independent neurophysiologist who was blinded to patient data.
Measurements and Main Results
Median body temperature at EEG recording was 33.0°C (range 32.4–33.8). ESE was found on 5 (10%) of the 51 EEG recordings: three patients had continuous rhythmic generalized spikes and two patients had continuous rhythmic focal spike-waves. Of the 17 (33%) patients who were discharged alive, 8 (8/51, 16%) had a CPC score of 1, 4 (8%) of 2, and 5 (10%) of 3. All patients with ESE died during their ICU stay.
Conclusion
These preliminary results indicate that postanoxic status epilepticus can be masked by neuromuscular blockade during our protocol of therapeutic hypothermia. Routine EEG monitoring might be helpful in cardiac-arrest survivors receiving therapeutic hypothermia. Further studies including continuous EEG monitoring are needed to determine whether early diagnosis and treatment of ESE during therapeutic hypothermia improves the outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Therapeutic hypothermia (TH) is now the standard of care for comatose survivors of cardiac arrest. Level 1 evidence exists to support this approach after out-of-hospital ventricular fibrillation. The indications for hypothermia have been extended, however, to other rhythm disorders and in-hospital cardiac arrest [1]. Neurological complications due to cerebral anoxia are the rule in cardiac-arrest patients, and prediction of their outcome is the focus of a recent review [2]. Seizure activity has been reported in 12–44% of patients, 5 h on average after cardiac arrest [3]. Seizure activity, even without clinical manifestations, can induce neuronal necrosis and activation of apoptosis, thereby causing further brain damage [4]. During TH, neuromuscular blockade, associated with sedation, is required to prevent cold-induced shivering. Neuromuscular blockade may mask the clinical manifestations of seizures. On the other hand, hypothermia, together with concomitant sedative therapy, may protect against seizures [5]. Although neuroprotection is the goal of TH and electrical seizure activity of theoretical concern after cardiac arrest, electroencephalography (EEG) monitoring is not specifically recommended during TH [6].
The aim of our pilot study was to evaluate whether routine EEG detected cases of electrical status epilepticus (ESE) masked by neuromuscular blockade in comatose cardiac-arrest survivors managed with hypothermia.
Patients and Methods
The ethics committee of the French Society for Critical Care approved this prospective study. Consecutive patients admitted to the ICU of the Andre Mignot Hospital over a 3-year period (May 2005–May 2008) for coma after successfully resuscitated cardiac arrest requiring TH were included. The Andre Mignot Hospital has 737 beds for both medical and surgical patients, including 15 beds in a closed medical–surgical ICU. Most ICU patients are admitted through the emergency department or prehospital emergency medical system [7]; only 25% of patients are referred from the wards. Patients managed in the ICU for postanoxic status epilepticus are discharged to the neurology department. In addition, a neurologist is available at all times for giving advice about diagnostic and therapeutic strategies in ICU patients with postanoxic status epilepticus. A cardiologist and sophisticated cardiological equipment are also available if necessary. In our ICU, all cardiac-arrest patients who remain comatose (Glasgow Coma Scale ≤8) after recovering spontaneous cardiac activity are managed with a standardized TH protocol (Fig. 1) according to international guidelines [8]; the only exclusion criteria are severe cardiogenic shock, life-threatening arrhythmias, pregnancy, and primary coagulopathy [1]. The protocol involves propofol (1–2 mg/kg bolus) for sedation and cisatracurium (0.15 mg/kg bolus) for neuromuscular blockade prior to hypothermia induction. During hypothermia, maintenance propofol (2–5 mg/kg/h) and cisatracurium (0.18 mg/kg/h) are given. The dosages are adjusted at 4-hour intervals to maintain the response to train-of-four stimulation at two of four twitches. Hypothermia is induced by ice-cold intravenous fluids at 4°C [9] then maintained by ice packs at the groin and neck and a cold-air tunnel around the patient’s body. Body temperature is maintained at 32–34°C for 24 h, as monitored continuously using a rectal probe. Rewarming is achieved passively, by covering the patient with a warm blanket and is allowed to proceed at a slow pace of 0.25–0.5°C per hour to avoid rebound hyperthermia.
Cisatracurium is discontinued when normothermia is achieved. When the train-of-four response is four twitches, the propofol is stopped or decreased to the lowest dose needed to ensure tolerance of the endotracheal tube.
Complications related to TH were assessed prospectively. Blood cultures were performed routinely twice a day during the hypothermia phase, and patients were monitored closely for aspiration pneumonia and for bleeding of any severity. Continuous cardiovascular monitoring was used in all patients to detect cardiac arrhythmia. None of the study patients experienced complications related to TH.
The study data were collected on a standardized form and included demographic data and cardiac arrest characteristics according to Utstein-style guidelines [10]. Severity and organ dysfunction at ICU admission were assessed using the Simplified Acute Physiology Score II (SAPS-II) [11] and the Logistic Organ Dysfunction (LOD) system score [12], respectively. Neurological outcome at discharge was assessed using the Cerebral Performance Category (CPC) score [10], as follows: CPC 1, conscious and alert with normal function or slight disability; CPC 2, conscious and alert with moderate disability; CPC 3, conscious with severe disability; CPC 4, comatose or persistent vegetative state; and CPC 5, brain dead or death from other causes.
Myoclonus was defined as spontaneous or sound-sensitive, repetitive, regular (periodic) or irregular, rapid, brief jerks involving peripheral or axial muscles on both sides of the body [13–15]. Time of myoclonus occurrence, duration, and body temperature at onset were recorded.
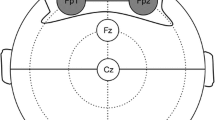
For the study, each patient underwent bipolar 8-channel EEG recording during and after TH, via scalp electrodes positioned according to the Standard International 10–20 system (Fp2-T4, T4-O2, Fp2-C4, C4-O2, Fp1-T3, T3-O1, Fp1-C3, and C3-O2). The EEGs were performed by a neurophysiology technician at our hospital during office hours; outside office hours, a technician from a private EEG laboratory in the region came in, as soon as possible. The time of EEG recording during TH was recorded, as well as body temperature during EEG. EEG recordings were read by a certified neurophysiologist at another hospital (HS) who was blinded to patient data and looked for ESE. ESE was defined as continuous or recurrent epileptiform activity including rhythmic focal or generalized spikes, sharp waves, spike and wave bursts, or rhythmic waves changing in amplitude, frequency, and/or spatial distribution [16], and lasting more than 10 min. Frequent or continuous EEG abnormalities such as spikes, sharp waves, rhythmic slow activity, PLEDs, BiPEDs, GPEDs, or triphasic waves, suggestive of ESE in anoxic brain damage, were also classified as ESE as recommended in recent guidelines. Recordings showing burst-suppression with epileptiform bursts were not classified as ESE [17]. Any EEG results obtained outside the period of neuromuscular blockade were also recorded.
Statistical Analysis
Quantitative parameters are reported as median and interquartile range (IQR, 25th–75th percentiles) and qualitative parameters as number and percentage.
Results
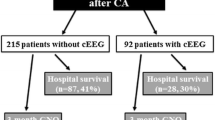
During the study period, 90 patients were admitted to the ICU after cardiac arrest. Among these patients, 51 were comatose after recovery of spontaneous cardiac activity and were treated with TH. These 51 patients underwent routine EEG recording during neuromuscular blockade for TH and form the basis for this study (Fig. 2).
Table 1 reports the characteristics and outcomes of these 51 patients. There were 39 men and 12 women, with a median age of 60 years (IQR, 52–74 years). Cardiac arrest occurred out of the hospital in 86% of patients and was witnessed in 84% of patients. The cause of cardiac arrest was presumed to be cardiac in 55% of patients. Ventricular fibrillation and tachycardia was the first recorded rhythm in 49% cases. Cardiopulmonary resuscitation was performed before emergency medical service arrival in 58% of patients, at a median of 5 min after collapse (IQR, 0–11 min). The median time from collapse to spontaneous circulation was 27 min (IQR, 15–35 min). The median duration of TH was 27 h (IQR, 22–34 h). Of the 17 (33%) patients who were discharged alive, eight (8/51, 16%) had a CPC score of 1, 4 (8%) of 2, and 5 (10%) of 3.
Median body temperature at the time of the EEG recording was 33.0°C (IQR, 32.4–33.8°C) (Fig. 2). Evidence of ESE was found in five (10%) patients (Table 2): continuous rhythmic generalized spikes were present in three patients and continuous rhythmic focal spike-waves in two patients. None of the patients exhibited periodic epileptiform discharges. The epileptiform activity lasted more than 30 min in all five patients.
Myoclonus occurred outside the TH period in 23 of the 51 patients, at a median time of 29 h (IQR, 3–39 h) after cardiac arrest. All 23 patients experienced continuous myoclonus for more than 30 min. Myoclonus started before TH in eight patients, in whom a propofol loading dose led to resolution of visible jerks before neuromuscular blockade; four of these patients had recurrent myoclonus after TH completion. In the remaining 15 patients, myoclonus occurred only after the end of TH, at median times of 32 h (IQR, 27–46 h) after cardiac arrest and 2 h (IQR, 1–4 h) after neuromuscular blocker withdrawal, at a median body temperature of 36.3°C (IQR, 34.4–38.8°C). Of the five patients with ESE, four experienced myoclonus outside the TH phase. Myoclonus occurred only after TH completion in two of these four patients. Myoclonus started before TH in two patients, one of whom experienced a recurrence after TH completion.
All patients with myoclonus and/or ESE received intravenous antiepileptic treatment before further EEG recording, which showed persistent ESE in 13 patients. EEGs were repeated in these 13 patients, with a median number of six [3–8] EEGs per patient. The median number of anticonvulsant drugs received in patients with myoclonus was four (2.5–4.0). Anticonvulsant therapy included clonazepam in all but five patients (78%), propofol in 16 (70%), phenobarbital in 13 (57%), midazolam in nine (39%), phenytoin in eight (35%), valproate in five (22%), and thiopenthal in 2 (9%).
Discussion
To our knowledge, this is the first study designed to evaluate the potential usefulness of EEG monitoring for detecting ESE during TH requiring continuous neuromuscular blockade. We found ESE in 10% of patients during TH.
Several factors may have influenced the incidence of ESE detected during hypothermia. First, TH protected against seizure activity in experimental studies [5, 18, 19] and was used successfully to treat seizures in three pediatric [20] and four adult [21] patients. The underlying neurophysiologic mechanisms remain poorly understood but may involve diminished excitatory transmission via epileptogenic threshold elevation [22]. The anticonvulsant effects of hypothermia were potentiated by concomitant antiepileptic drug use in rats [5] and humans [20]. Second, propofol, the sedative used in our study, exerts powerful antiepileptic effects related to activation of gamma-aminobutyric-acid (GABA)A receptors and enhancement of inhibitory GABAA receptor-mediated responses [23]. In both experimental [24] and clinical [25] studies, propofol was effective in controlling status epilepticus. Propofol is recommended for the treatment of subtle or refractory status epilepticus [26] and may hold promise for controlling postanoxic status epilepticus [15]. Finally, propofol blood concentrations are higher at 34°C than at 37°C [27], suggesting that hypothermia may potentiate the anticonvulsant effects of propofol.
Myoclonus occurred in 19 of 51 patients after TH completion in our study. In addition to discontinuation of hypothermia and propofol, the development of myoclonus may be influenced by the rewarming time [28]. Rebound seizures have been reported during rapid rewarming after prolonged TH [5, 19, 29]. In a recent study [30] of amplitude-integrated EEG as a potential tool for outcome prediction after cardiac arrest treated with hypothermia, seven (21%) of 34 patients had electrical and clinical status epilepticus; however, EEG recording started before, and ended after, the TH period, and the time of seizure onset relative to the hypothermic period was not reported. Because none of our patients underwent EEG during rewarming, we cannot exclude that critical EEG activity began during this phase.
In our study, all five patients with ESE during TH died. This finding supports previous evidence that ESE during hypothermia may predict a poor outcome [30]. Among them, two had myoclonus at ICU admission that recurred after TH completion. Moreover, in the five patients with ESE, anticonvulsant therapy provided only temporary control, suggesting highly refractory epileptic activity. However, our study was not designed to evaluate the usefulness of anticonvulsant therapy in these patients. Myoclonus occurring after cardiac arrest is usually pharmacoresistant and carries a poor prognosis [2]. Postanoxic status epilepticus was recently identified in a retrospective study as an independent factor of adverse prognostic significance and, therefore, as a potential target for aggressive early treatment although evidence of brain damage is less common in nonconvulsive than in convulsive status epilepticus, there is some support for anticonvulsant therapy, particularly in comatose patients [31]. Moreover, some of our patients may have had mild ESE that was controlled by the sedatives used for TH [32]. A recent report describing favorable outcomes in comatose survivors after cardiac arrest with postanoxic status epilepticus [33] supports this hypothesis. Thus, the five patients with detected ESE probably had highly refractory seizure activity. Finally, recent guidelines recommend a reappraisal of prognostic factors in cardiac arrest survivors receiving TH [2]. It would be of interest to conduct prospective studies aimed at determining whether postanoxic status epilepticus is not only a consequence of initial brain anoxia, but also a cause of further cerebral brain damage.
Our study has many limitations. First, continuous EEG monitoring throughout neuromuscular blockade might have detected cases of early transient ESE missed by our study. Second, surface EEG electrodes fail to detect status myoclonus [15], which is not of epileptic nature and presumably originates in the subcortical reticular system and/or spinal cord [13]. This fact may explain the discrepancy between presence of ESE and presence of myoclonus. However, 13 of the 23 patients with clinical myoclonus outside the TH period had concomitant ESE documented by EEG. Third, to define status epilepticus, we used the recent operational definition requiring a seizure activity of more than 10 min and corresponding to impending status epilepticus, instead of 30 min (corresponding to established status epilepticus). Recent findings showed significantly higher mortality rates in patients with seizure activity lasting 30 min or more [34]. However, all five patients with ESE had epileptiform activity for 30 min at least. Finally, the high proportion of patients with no ventricular fibrillation and/or with myoclonus before TH may explain the high mortality rate, compared to previous studies of patients successfully treated with TH [35–37]. However, our results are consistent with those of patient cohorts managed with the extended indication of TH after cardiac arrest [38].
In conclusion, our preliminary results show that postanoxic status epilepticus can be masked by neuromuscular blockade in patients treated with TH after cardiac arrest. Our findings suggest that EEG may be useful in these patients as a tool for promptly identifying ESE. Additional studies using continuous EEG monitoring are needed to confirm our findings and to determine whether early ESE treatment during TH improves outcomes in cardiac-arrest survivors with ESE.
References
Nolan JP, Deakin CD, Soar J, Bottiger BW, Smith G. European Resuscitation Council guidelines for resuscitation 2005. Sect. 4. Adult advanced life support. Resuscitation. 2005;67(Suppl 1):S39–86.
Wijdicks EF, Hijdra A, Young GB, Bassetti CL, Wiebe S. Practice parameter: prediction of outcome in comatose survivors after cardiopulmonary resuscitation (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2006;67:203–10.
Krumholz A, Stern BJ, Weiss HD. Outcome from coma after cardiopulmonary resuscitation: relation to seizures and myoclonus. Neurology. 1988;38:401–5.
Fujikawa DG. Prolonged seizures and cellular injury: understanding the connection. Epilepsy Behav. 2005;7(Suppl 3):S3–11.
Schmitt FC, Buchheim K, Meierkord H, Holtkamp M. Anticonvulsant properties of hypothermia in experimental status epilepticus. Neurobiol Dis. 2006;23:689–96.
Neumar RW, Nolan JP, Adrie C, et al. Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication. A consensus statement from the International Liaison Committee on Resuscitation (American Heart Association, Australian and New Zealand Council on Resuscitation, European Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Asia, and the Resuscitation Council of Southern Africa); the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Perioperative, and Critical Care; the Council on Clinical Cardiology; and the Stroke Council. Circulation. 2008;118:2452–83.
Adnet F, Lapostolle F. International EMS systems: France. Resuscitation. 2004;63:7–9.
Nolan JP, Morley PT, Hoek TL, Hickey RW. Therapeutic hypothermia after cardiac arrest. An advisory statement by the Advancement Life support Task Force of the International Liaison Committee on Resuscitation. Resuscitation. 2003;57:231–5.
Polderman KH, Rijnsburger ER, Peerdeman SM, Girbes AR. Induction of hypothermia in patients with various types of neurologic injury with use of large volumes of ice-cold intravenous fluid. Crit Care Med. 2005;33:2744–51.
Jacobs I, Nadkarni V, Bahr J, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa). Circulation. 2004;110:3385–97.
Le Gall JR, Lemeshow S, Saulnier F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA. 1993;270:2957–63.
Le Gall JR, Klar J, Lemeshow S, et al. The Logistic Organ Dysfunction system. A new way to assess organ dysfunction in the intensive care unit. ICU Scoring Group. JAMA. 1996;276:802–10.
Young GB, Gilbert JJ, Zochodne DW. The significance of myoclonic status epilepticus in postanoxic coma. Neurology. 1990;40:1843–8.
Wijdicks EF, Parisi JE, Sharbrough FW. Prognostic value of myoclonus status in comatose survivors of cardiac arrest. Ann Neurol. 1994;35:239–43.
Thomke F, Marx JJ, Sauer O, et al. Observations on comatose survivors of cardiopulmonary resuscitation with generalized myoclonus. BMC Neurol. 2005;5:14.
Kaplan PW. The EEG of status epilepticus. J Clin Neurophysiol. 2006;23:221–9.
Walker M, Cross H, Smith S, et al. Non convulsive status epilepticus : Epilepsy Research Foundation Workshop Reports. Epileptic Disord. 2005;7:253–96.
Maeda T, Hashizume K, Tanaka T. Effect of hypothermia on kainic acid-induced limbic seizures: an electroencephalographic and 14C-deoxyglucose autoradiographic study. Brain Res. 1999;818:228–35.
Liu Z, Gatt A, Mikati M, Holmes GL. Effect of temperature on kainic acid-induced seizures. Brain Res. 1993;631:51–8.
Orlowski JP, Erenberg G, Lueders H, Cruse RP. Hypothermia and barbiturate coma for refractory status epilepticus. Crit Care Med. 1984;12:367–72.
Corry JJ, Dhar R, Murphy T, Diringer MN. Hypothermia for refractory status epilepticus. Neurocrit Care. 2008;9:189–97.
Lundgren J, Smith ML, Blennow G, Siesjo BK. Hyperthermia aggravates and hypothermia ameliorates epileptic brain damage. Exp Brain Res. 1994;99:43–55.
Ohmori H, Sato Y, Namiki A. The anticonvulsant action of propofol on epileptiform activity in rat hippocampal slices. Anesth Analg. 2004;99:1095–101. table of contents.
Holtkamp M, Tong X, Walker MC. Propofol in subanesthetic doses terminates status epilepticus in a rodent model. Ann Neurol. 2001;49:260–3.
Parviainen I, Uusaro A, Kalviainen R, Mervaala E, Ruokonen E. Propofol in the treatment of refractory status epilepticus. Intensive Care Med. 2006;32:1075–9.
Meierkord H, Boon P, Engelsen B, et al. EFNS guideline on the management of status epilepticus. Eur J Neurol. 2006;13:445–50.
Leslie K, Sessler DI, Bjorksten AR, Moayeri A. Mild hypothermia alters propofol pharmacokinetics and increases the duration of action of atracurium. Anesth Analg. 1995;80:1007–14.
Legriel S, Troche G, Bedos JP. Status epilepticus after discontinuation of induced hypothermia—an incidental association? Resuscitation. 2006;70:159.
Battin M, Bennet L, Gunn AJ. Rebound seizures during rewarming. Pediatrics. 2004;114:1369.
Rundgren M, Rosen I, Friberg H. Amplitude-integrated EEG (aEEG) predicts outcome after cardiac arrest and induced hypothermia. Intensive Care Med. 2006;32:836–42.
Jirsch J, Hirsch LJ. Nonconvulsive seizures: developing a rational approach to the diagnosis and management in the critically ill population. Clin Neurophysiol. 2007;118:1660–70.
Rossetti AO, Logroscino G, Liaudet L, et al. Status epilepticus: an independent outcome predictor after cerebral anoxia. Neurology. 2007;69:255–60.
Rossetti AO, Oddo M, Liaudet L, Kaplan PW. Predictors of awakening from postanoxic status epilepticus after therapeutic hypothermia. Neurology. 2009;72:744–9.
Legriel S, Mourvillier B, Bele N, et al. Outcomes in 140 critically ill patients with status epilepticus. Intensive Care Med. 2008;34:476–80.
Hypothermia after Cardiac Arrest Study Group, et al. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002;346:549–56.
Bernard SA, Gray TW, Buist MD, et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002;346:557–63.
Oddo M, Schaller MD, Feihl F, Ribordy V, Liaudet L. From evidence to clinical practice: effective implementation of therapeutic hypothermia to improve patient outcome after cardiac arrest. Crit Care Med. 2006;34:1865–73.
Gueugniaud PY, David JS, Chanzy E, et al. Vasopressin and epinephrine vs. epinephrine alone in cardiopulmonary resuscitation. N Engl J Med. 2008;359:21–30.
Acknowledgment
We thank A. Wolfe MD for helping to prepare the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was performed in the Intensive care unit of André Mignot Hospital, France.
Rights and permissions
About this article
Cite this article
Legriel, S., Bruneel, F., Sediri, H. et al. Early EEG Monitoring for Detecting Postanoxic Status Epilepticus during Therapeutic Hypothermia: A Pilot Study. Neurocrit Care 11, 338–344 (2009). https://doi.org/10.1007/s12028-009-9246-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-009-9246-4