Abstract
There is no approved therapy for food allergies, which affect 12 million people in the United States and millions more worldwide. In the last few years, our research team at Duke has begun to develop protocols to treat peanut and other food allergies. Two distinct therapies are being developed. Oral immunotherapy (OIT), which relies on ingestion of increasing amounts of the allergenic food, has been used to successfully desensitize more than 50 peanut allergic subjects. Sublingual immunotherapy (SLIT) involves placing small quantities of peanut allergens under the tongue and has shown promise in our initial placebo-controlled clinical trial. Immunologic changes associated with OIT and SLIT include reduction in mast cell reactivity as determined by skin prick test size, decreased basophil responses, decreased specific-IgE, increased IgG4, and induction of regulatory T cells. Development of these immunotherapy strategies has generated much excitement in the food allergy community; however, further studies are needed before these approaches are ready for clinical use.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Food allergy is caused by a breakdown in immunologic tolerance mechanisms. Typically, oral tolerance is induced by ingestion of antigen leading to one or more of the following mechanisms: deletion of antigen-specific T cells; induction of anergy in antigen-specific T cells; and/or production of regulatory T cells (Tregs) [1, 2]. In food allergic individuals, faulty mechanisms of tolerance give rise to food-specific T-cell responses with a Th2-type profile. Th2 cell secretion of IL-4 and IL-13 drives B cells to produce IgE [3]. IgE then binds to its high-affinity receptor, FcεRI, on mast cells, which line the skin and mucosal tissues. Upon a subsequent ingestion of the sensitizing food, an allergic reaction is triggered by cross-linking of IgE receptors on mast cells, leading to degranulation in which mast cells release their contents, including histamine, leukotrienes, and prostaglandins. These potent bioactive compounds give rise to allergic symptoms characterized by urticaria, angioedema, vomiting, wheezing, and anaphylaxis.
Food allergies affect an estimated 4–6% of young children and 2% of adults in the United States [4]. The Center for Disease Control and Prevention has reported an approximately 20% increase in US children affected in the period from 1997 to 2007 [5]; other allergic conditions such as asthma and atopic dermatitis are also increasing [6]. The underlying cause of this increase is unclear, although the “hygiene hypothesis” has received significant attention. This idea basically states that decreases in family size and bacterial and parasitic infections in Westernized societies cause the immune system to over-respond to innocuous antigens [7]. However, although an attractive concept, this is an insufficient immunologic explanation for the observed rise in Th2-polarized diseases. By contrast, there is evidence that food allergy is caused by a complex interplay between environmental factors and genetics, as well as the food allergens themselves [8]. It has been noted that some foods are highly allergenic, while others rarely cause sensitization [9, 10]. The “big 8” allergenic foods that account for ~90% of food allergies in the United States are milk, egg, peanut, tree nuts, soybeans, wheat, fish, and shellfish [8].
Many food allergies are naturally outgrown. Both egg and milk allergies commonly resolve without intervention during the first decade of life [11, 12]. IgE recognition of linear rather than conformational epitopes on milk and egg allergens may predict which children will eventually become tolerant versus those that will remain allergic [13]. In contrast to milk and egg allergies, peanut allergy is rarely outgrown. A natural history study estimated that only 20% of those diagnosed with peanut allergy will eventually become tolerant [14]. In addition, peanut allergy is considered to be a more severe disease, since it has been shown to be responsible for the majority of life-threatening and fatal allergic reactions to foods [15–17], and even minute amounts of peanut proteins (100 μg in one study [18]) have been shown to elicit clinical symptoms.
Currently, there is no accepted form of therapy for food allergies. Patients are instructed to strictly avoid the allergenic food(s) and carry rescue medicine, such as epinephrine and anti-histamines, with them at all times. However, constant vigilance erodes quality of life, and accidental reactions are common even among the most cautious patients [19, 20]. Previous attempts to treat food allergies included subcutaneous injections of peanut protein extracts [21], which is the preferred route for immunotherapy with aeroallergens and insect venom. Although some efficacy was reported, systemic reactions, including anaphylaxis, were very common, leading to the abandonment of this approach for food allergies. Another trial, using an anti-IgE monoclonal antibody, called TNX-901, was also studied for peanut allergy [22]. The highest dose studied caused a significant increase in eliciting dose threshold; however, it offered no improvement for ~25% of the study participants.
At Duke, we have developed oral immunotherapy (OIT) for food allergies, evolving over time from small open-label pilot studies to larger randomized designs. The concept is based on drug desensitization and involves administering increasing doses of the offending food over a period of several months. We have had extensive experience in OIT for egg and peanut allergies in several clinical trials. Additionally, we have recently completed the first double-blind placebo-controlled trial of sublingual immunotherapy (SLIT) for peanut allergy. Here, we will describe our experiences with OIT and SLIT in the clinical setting and examine the immunologic changes associated with these therapies.
Oral immunotherapy
Our initial goal for OIT was to safely bring subjects to a maintenance dose equivalent to the amount of protein that would be present in a “bite” of the allergenic food, which would theoretically confer protection in the event of an accidental ingestion. This approach requires the subject to mix the powdered allergen dose in a vehicle food, such as applesauce or pudding, and ingest it each day at home. For egg and peanut, this dose was determined to be 300 mg, which is the equivalent of a few bites of egg in a baked good or one peanut. It was hypothesized that several months on OIT would lead to decreased specific-IgE levels, which would warrant an open food challenge to several grams of the allergenic food. Ninety-five percent confidence intervals have previously been reported, showing that IgE <2 kU/l for peanut or egg give the subject an approximately 50% chance to pass an open food challenge [23]. In addition to following specific-IgE, we also tracked IgG and IgG4, along with various cellular responses focused primarily on T cells and basophils.
Two concepts for effective outcomes have now become paramount in our research; the first is successful demonstration of desensitization and eventual tolerance to the allergenic food. In the context of immunotherapy, we define desensitization as the ability to raise the amount of food protein required to induce a clinical reaction, while still on daily immunotherapy. Tolerance is defined as a prolonged ability to ingest large amounts of the food proteins without daily intake of immunotherapy. We will review our experiences with both of these endpoints for food allergies.
Egg OIT
The first study of OIT undertaken was an open-label study for egg allergy in a pediatric population [24]. Egg allergy was chosen as a proof-of-concept for safety concerns, with some caution as to the severity of reactions that may result from OIT in peanut allergic patients. Subjects began the study with a first-day dose escalation beginning at 0.1 mg and escalating up to 200 mg of egg white powder and were then again observed the next day to ingest the highest tolerated dose. Subjects then began ingesting egg proteins daily at home during the build-up phase of OIT, increasing biweekly on the research unit until reaching the maintenance dose of 300 mg. Two food challenges were conducted to determine whether subjects were desensitized or tolerant.
The desensitization challenge occurred while subjects were taking daily egg doses. Four out of seven subjects passed the initial desensitization challenge, with all subjects consuming larger amounts than were tolerated at baseline. For the tolerance challenge, the four subjects that passed the desensitization challenge withheld daily egg ingestion for 3–4 months and received the same challenge. Two out of the four subjects passed the tolerance challenge [24]. Although these results indicated that egg OIT appeared safe and feasible, it was not clear whether it would alter the natural history of the disease. With this in mind, subjects were brought to higher maintenance doses to determine the effects of higher doses and longer treatment courses, on development of tolerance.
Six additional subjects were studied to investigate the effects of higher maintenance dosing (Vickery et al. Annals of Allergy, Asthma, and Immunology 2010–manuscript in press). Subjects ingested a median of 2,400 mg egg powder as maintenance dosing and were studied for up to 60 months. One hundred percent of these subjects passed the desensitization challenge and were then taken off OIT for 4 weeks. Following abstinence from egg OIT, all six subjects passed a tolerance challenge. These subjects now eat egg in their diets and are considered clinically tolerant. This study highlights the potential importance of higher OIT dosing and longer treatment courses.
Immunologic changes observed with egg OIT were encouraging in that they resembled known changes from other types of allergy immunotherapy, such as subcutaneous IT for pollen allergies [25]. Mast cell responses, as measured by skin prick testing with egg proteins, were decreased following egg OIT. Humoral responses to egg allergens changed during the course of OIT. Egg-specific-IgE was decreased, while egg-IgG and IgG4 were significantly increased [24]. The same pattern of decreased IgE and increased IgG4 was observed for the major egg allergen, ovomucoid. T cell responses to egg demonstrated a shift away from a Th2 profile, with increases in TGF-β and IL-10, known regulatory cytokines, although with the limited number of subjects these changes did not reach statistical significance. We were encouraged by these early results, although without a control group, we were unable to definitively conclude that these changes were due to OIT since most patients are expected to outgrow egg allergy.
Peanut OIT
Early success with egg OIT encouraged us to pursue OIT for peanut allergy, with protocols based on the egg OIT studies. In the original open-label study, subjects began with an escalation starting at 0.1 mg up to 50 mg of peanut protein on the first day [26]. Over the next several months, subjects were brought to a maintenance dose of 300 mg. Subjects were challenged following 4–22 months of maintenance dosing to assess desensitization. On the initial day, all subjects reacted at less than 50 mg protein, but at the desensitization challenge, 27 out of 29 subjects successfully consumed the entire challenge dose of 3,900 mg of peanut protein (equivalent to ~16 peanuts). This trial of peanut OIT is the largest study published, indicating that 93% of subjects reaching the maintenance dosing were desensitized. Although this was also an uncontrolled study, this dramatic improvement would be unexpected in typical untreated peanut allergic patients.
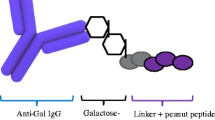
Immunologic changes associated with this desensitization were also reported [26] and are represented in Fig. 1. Effector cell responses to peanut were decreased as evidenced by skin prick testing and basophil hyporesponsiveness. Decreases in mast cell and basophil reactions to peanut allergens help explain the achievement of a desensitized state. Changes in antibody responses followed that of subcutaneous immunotherapy; namely, we measured significantly decreased peanut-IgE and increased IgG and IgG4. Interestingly, the epitope-specific nature of the subjects’ responses appears to shift from IgE to IgG4, such that IgG4 is directed at the same epitopes binding IgE prior to OIT [27]. A serum factor, presumably peanut-IgG4, induced by OIT was also shown to block the interaction of peanut allergen with IgE in a functional binding assay.
Schematic representation of relative changes in immunologic parameters during the course of OIT. The build-up phase occurs from 0 to approximately 10 months then maintenance doses are received. Desensitization occurs by 12 months, while it is unclear when tolerance may develop. Specific-IgE, specific-IgG4, Tregs, Th2 cytokines, skin prick test reactions, and basophil responses are represented as indicated on the Y-axis; allergen dosage is shown as a solid line, as indicated
Regulatory T cells (Tregs) are thought to play a critical role in oral tolerance and were recently demonstrated to increase in subjects outgrowing milk allergy [28]. In our peanut OIT study, CD4 + CD25 + FoxP3 + Tregs were increased at 12 months of OIT and began to return to baseline by 18 months. The transient increase in Tregs may drive the suppression of the Th2 response to peanut allergens. Indeed, Th2-type cytokines were significantly decreased by 12 months and remained decreased through 24 months of OIT [29]. Additional studies on T cells revealed an increased propensity for apoptosis as evidenced by changes in apoptosis-related gene expression.
Peanut OIT was shown to be safe in this open-label cohort [30]. In contrast to the experience with subcutaneously injected peanut immunotherapy, allergic side effects did occur, but these were generally mild, involving the skin and/or upper airway and responded to antihistamines. Importantly, the vast majority of side effects occurred early in the build-up phase, indicating that desensitization had not yet been achieved. Only one reaction required treatment with epinephrine for a systemic reaction in over 10,000 doses administered. It must be noted that 4 subjects withdrew from the study due to ongoing OIT-related allergic side effects, indicating that not all allergic subjects will tolerate OIT. Other triggers of side effects in subjects normally tolerating doses include ongoing infection, exercise following dosing, and dosing on an empty stomach [31].
A follow-up study was conducted to conclusively address desensitization in a randomized, double-blinded, placebo-controlled trial [32]. Subjects received peanut flour or oat flour as a placebo. Maintenance doses were increased to 4,000 mg in this study, which were achieved in ~10 months for most patients. All 16 peanut OIT subjects in the active treatment group passed the desensitization challenge, while none of the placebo subjects did. The active group ingested a median 5,000 mg peanut protein (~20 peanuts), while the placebo reached a median of 280 mg peanut protein (~1 peanut) before having allergic symptoms. This double-blind, placebo-controlled trial definitively demonstrated that successful desensitization was induced by OIT in a 12-month period.
In order to address tolerance, eight subjects in the open-label OIT study whose peanut-IgE levels had been reduced to <15 kU/l were taken off of OIT for 4 weeks and then challenged to peanut [33]. These subjects were on peanut OIT for 32–61 months prior to tolerance challenging. All eight subjects were able to successfully complete the challenges and are deemed clinically tolerant to peanut. We are still following these subjects and working on defining biomarkers to discriminate the factors that are decisive in tolerance development. Of note, in the 4 weeks off OIT, peanut-IgE did not increase, indicating a long-lasting effect on this vital allergic immune parameter.
A direct result of desensitization of peanut allergy is an increase in freedoms not present before OIT, such as eating at particular restaurants, attending social gatherings, and eating with non-allergic peers at lunch [34]. Previous studies have concluded that the quality of life of a food allergic child is comparable to that of a diabetic child [35]. In preliminary reports of our subjects and their families’ responses to quality of life assessments, we have seen a dramatic improvement in the quality of life (emotional, social, physical, and scholarly benefits) associated with having a food allergy both for the subject and that subject’s family [36].
Importantly, our findings have been replicated in subsequent oral immunotherapy trials at other medical centers. In particular, peanut OIT has been reported on by two European groups [37, 38]. These studies included pre-OIT challenge to establish baseline thresholds. Clark et al. reported on four subjects undergoing OIT and found an increase from baseline of 5–50 mg peanut protein required to cause clinical symptoms, up to 2,400 mg following OIT [37]. Blumchen et al. also reported a highly significant increase in threshold of peanut challenge following OIT in 14 of 23 subjects reaching maintenance dosing. Immunologic changes were similar to our previous report, namely, decreased skin prick tests, increased peanut-IgG4, and decreased Th2 cytokine production [38]. Both research groups concluded that desensitization of peanut allergy can be achieved by OIT in most patients.
Sublingual immunotherapy
Another approach being actively studied for food allergies is SLIT. SLIT involves placing drops of allergen extract under the tongue, then swallowing the liquid. SLIT has some convincing evidence for efficacy in allergies to pollens (i.e., allergic rhinitis) and is extensively used in Europe [39, 40]. This type of therapy is thought to work by interacting with tolerogenic Langerhan’s cells in the oral mucosa, which lead to down-regulation of the allergic response. Limited studies using SLIT for food allergies have been reported, the most cited of which was a trial for hazelnut allergy [41]. In this study, the majority of subjects appeared to have oral allergy syndrome (OAS; cross-reactivity of food proteins with IgE directed at environmental allergens [42]) and not systemic reactions on ingestion of hazelnut. Other reports are case reports for kiwi allergy [43] and another with peach for OAS patients [44]. Here, at Duke, we have conducted a SLIT study in peanut allergic subjects.
A randomized, double-blinded, placebo-controlled trial of SLIT for peanut allergy in young children (median age of 5 years) was conducted with 18 subjects (manuscript submitted—Kim et al. 2010). SLIT was administered daily with peanut extract in glycerinated saline given to subjects for 12 months prior to challenge. SLIT began at 250 ng of peanut protein and subjects were up-dosed to a maintenance dose of 2 mg peanut protein. On challenge, subjects on active treatment (n = 11) consumed a median of 1,710 mg peanut protein (~7 peanuts), while placebo subjects (n = 7) ingested a mere 85 mg before having an allergic reaction. Of note, there was a large range of peanut consumed on challenge in the active group (range: 35–2,500 mg), which shows that not all subjects were desensitized effectively. The amount consumed on challenge was modestly correlated with peanut-IgE levels, which may be important for the subset of subjects with extremely elevated peanut-IgE.
As with OIT, peanut SLIT was associated with decreases in skin prick test reactions and basophil activation assays. Peanut-IgG4 was significantly increased at 12 months, although the absolute levels of peanut-IgG4 in serum were much lower than subjects receiving high-dose OIT. Th2 cytokine decreases were also decreased for those on active treatment, which were not observed in placebo subjects. Lastly, an increase in Tregs was measured for the active treatment group, although it was not statistically different from placebo (P = 0.145).
SLIT appears to provide clinical benefits in this first DBPC trial. Although a smaller percentage of SLIT subjects were able to ingest the entire challenge when compared to the double-blinded, placebo-controlled peanut OIT study, this provides evidence that SLIT can be a viable treatment approach for food allergy. These findings are especially exciting since such a low dose is required (2 mg) compared to OIT (300–4,000 mg). SLIT may be a safe, effective option for subjects that cannot tolerate OIT.
Ongoing and future studies
We have begun a pilot study using a combination of Xolair (Omalizumab, Genentech) and peanut OIT. Xolair is an anti-IgE monoclonal antibody therapy that decreases free, circulating IgE in serum, decreases expression of FcεRI on mast cells and basophils, and is approved for treatment of allergen-induced asthma [45]. The hypothesis we are testing is that pre-treatment with Xolair will decrease allergic side effects and allow increasing to maintenance doses more quickly. Pre-treatment with Xolair was reported to increase the safety of aeroallergen (cat, dog, and house dust mite) subcutaneous immunotherapy [46].
Another trial recently begun at Duke Medical Center is titled Determining the Efficacy and Value of Immunotherapy on the Likelihood of Peanut Tolerance (DEVIL). The trial is designed to introduce peanut OIT to infants recently diagnosed with peanut allergy. We are interested if early intervention, while the peanut immune response is still developing, may prove beneficial. It is conceivable that the infant immune response will be more quickly amenable to treatment and will protect these children from severe reactions in later years. Additionally, two dosages, 300 and 3,000 mg, of peanut OIT are being compared and mechanistically studied for differences in cellular and humoral responses.
Researchers in Europe are investigating an interesting concept in which children are exposed to peanut before they ever develop IgE. The trial, called Learning Early About Peanut allergy (LEAP) is designed to give low, but frequent doses of peanut to induce oral tolerance before allergy develops. The concept is based on differences of peanut allergy prevalence in Jewish children in the United Kingdom and Israel. The prevalence is ~1.85% in the United Kingdom and 0.17% in Israel [47]. Infants in Israel aged 8–14 months had a median monthly intake of 7.1 g of peanut protein compared to 0 g in the United Kingdom. A recent publication in a mouse model supports this hypothesis [48].
Our research team at Duke also participates in the Consortium of Food Allergy Research (CoFAR), which has several ongoing multi-site trials at Mount Sinai School of Medicine, National Jewish Research and Medical Center, University of Arkansas for Medical Sciences, and Johns Hopkins School of Medicine. An observational study is underway [49], which is aimed at understanding how the immune response to various food allergens progresses over several years. In particular, we are interested in egg and milk allergic children that go on to develop peanut allergy. Interesting outcomes will be mechanisms of natural resolution of egg and milk allergy, and how the peanut immune response develops into either allergy or tolerance. Other studies conducted by CoFAR include randomized, double-blinded, placebo-controlled trials of egg OIT in children with persistent egg allergy and peanut SLIT for adults. Additionally, clinical studies have begun using engineered, mutated peanut allergens expressed in E. coli, which were previously shown to decrease peanut allergy in animal models [50] possibly by interacting with Toll-like receptors [51].
Our research group was also involved in a trial of milk OIT in collaboration with researchers at Johns Hopkins [52]. Skripak et al. reported on a randomized, double-blinded, placebo-controlled trial with entry challenge to milk. Baseline thresholds of milk required to induce reactions had a median of 40 mg. Subjects were built-up to a 500 mg maintenance dose, then challenged again. The median challenge threshold post-OIT was 5,100 mg, a significant increase, while no change was seen in subjects receiving placebo. This study indicates that regardless of food allergen, desensitization should be possible, as has now been demonstrated for egg, peanut, and milk allergies.
A non-allergen-specific therapy that has shown impressive efficacy in mouse models of food allergy for peanut, as well as a multi-allergic model for egg, fish, and peanut allergy, is the Food Allergy Herbal Formula (FAHF-2) developed at Mount Sinai [53, 54]. The researchers developed this herbal formula based on allergy formulas used in traditional Chinese medicine. Clinical trials are underway [55].
At Duke, we will also begin clinical trials to address tree nut (walnut, cashew, etc.) allergies. Tree nut allergy is similar to peanut allergy in that less than 10% of diagnosed patients will go on to outgrow the allergy and life-threatening and fatal reactions are associated with tree nuts. Additionally, tree nut allergy is often not restricted to one nut but frequently involves reactions to multiple nuts. A recent study from Europe showed that up to 80% of patients with an allergy to one nut will also have IgE to other nuts [56]. We will test the hypothesis that OIT with a single tree nut will down-regulate allergic responses to co-sensitizing tree nuts. Immunologic investigations will focus on serologic changes, basophil and mast cell changes, as well as ability of OIT to induce Tregs that will suppress multiple tree nut allergic responses. Pre-clinical studies in mice demonstrate the feasibility of this study [57].
Conclusions
OIT appears to be safe and effective for the vast majority of food allergic patients. Our experiences with peanut and egg OIT have demonstrated a significant increase in the amount of protein allergen needed to cause a reaction. Because this increase exceeds the amount of protein that would be expected in an accidental encounter, desensitization is clinically useful and provides a sense of relief for food allergic subjects and their families. The clinical effect of OIT is supported by relevant and consistent immunologic changes across multiple studies, including decreased mast cell and basophil responses; decreased IgE and increased IgG and IgG4; as well as a transient increase in Tregs and a sustained decrease in Th2 cytokines. SLIT also appears to be effective, although more work is required, including optimizing the dosage and length of treatment. Current studies are focused on which immune parameters may predict eventual tolerance, such that patients are not required to consume daily doses of the allergenic food. Both OIT and SLIT are relatively simple and feasible approaches and are likely to be cost-effective. Therefore, it may be expected that either or both may be adopted as the first treatment to modify the natural history of food allergy. However, it must be noted that the studies described herein were all conducted in relatively small samples at large medical centers with appropriate support staff and are not ready to be implemented into clinical practice [58].
References
Burks AW, Laubach S, Jones SM. Oral tolerance, food allergy, and immunotherapy: implications for future treatment. J Allergy Clin Immunol. 2008;121:1344–50.
Chehade M, Mayer L. Oral tolerance and its relation to food hypersensitivities. J Allergy Clin Immunol. 2005;115:3–12 [quiz 13].
Burks AW. Peanut allergy. Lancet. 2008;371:1538–46.
Sicherer SH, Sampson HA. Food allergy: recent advances in pathophysiology and treatment. Annu Rev Med. 2008.
Branum AM, Lukacs SL. Food allergy among children in the United States. Pediatrics. 2009;124:1549–55.
Ker J, Hartert TV. The atopic march: what’s the evidence? Ann Allergy Asthma Immunol. 2009;103:282–9.
Okada H, Kuhn C, Feillet H, Bach JF. The ‘hygiene hypothesis’ for autoimmune and allergic diseases: an update. Clin Exp Immunol. 2010;160:1–9.
Lee LA, Burks AW. Food allergies: prevalence, molecular characterization, and treatment/prevention strategies. Annu Rev Nutr. 2006;26:539–65.
Moreno FJ, Clemente A. 2S albumin storage proteins: what makes them food allergens? Open Biochem J. 2008;2:16–28.
Breiteneder H, Radauer C. A classification of plant food allergens. J Allergy Clin Immunol. 2004;113:821–30 [quiz 831].
Savage JH, Matsui EC, Skripak JM, Wood RA. The natural history of egg allergy. J Allergy Clin Immunol. 2007;120:1413–7.
Skripak JM, Matsui EC, Mudd K, Wood RA. The natural history of IgE-mediated cow’s milk allergy. J Allergy Clin Immunol. 2007;120:1172–7.
Jarvinen KM, Beyer K, Vila L, Bardina L, Mishoe M, Sampson HA. Specificity of IgE antibodies to sequential epitopes of hen’s egg ovomucoid as a marker for persistence of egg allergy. Allergy. 2007;62:758–65.
Skolnick HS, Conover-Walker MK, Koerner CB, Sampson HA, Burks W, Wood RA. The natural history of peanut allergy. J Allergy Clin Immunol. 2001;107:367–74.
Bock SA, Munoz-Furlong A, Sampson HA. Further fatalities caused by anaphylactic reactions to food, 2001–2006. J Allergy Clin Immunol. 2007;119:1016–8.
Bock SA, Munoz-Furlong A, Sampson HA. Fatalities due to anaphylactic reactions to foods. J Allergy Clin Immunol. 2001;107:191–3.
Yunginger JW, Squillace DL, Jones RT, Helm RM. Fatal anaphylactic reactions induced by peanuts. Allergy Proc. 1989;10:249–53.
Taylor SL, Hefle SL, Bindslev-Jensen C, Bock SA, Burks AW Jr, Christie L, Hill DJ, Host A, Hourihane JO, Lack G, Metcalfe DD, Moneret-Vautrin DA, Vadas PA, Rance F, Skrypec DJ, Trautman TA, Yman IM, Zeiger RS. Factors affecting the determination of threshold doses for allergenic foods: how much is too much? J Allergy Clin Immunol. 2002;109:24–30.
Boyano-Martinez T, Garcia-Ara C, Pedrosa M, Diaz-Pena JM, Quirce S. Accidental allergic reactions in children allergic to cow’s milk proteins. J Allergy Clin Immunol. 2009;123:883–8.
Yu JW, Kagan R, Verreault N, Nicolas N, Joseph L, St Pierre Y, Clarke A. Accidental ingestions in children with peanut allergy. J Allergy Clin Immunol. 2006;118:466–72.
Oppenheimer JJ, Nelson HS, Bock SA, Christensen F, Leung DY. Treatment of peanut allergy with rush immunotherapy. J Allergy Clin Immunol. 1992;90:256–62.
Leung DY, Sampson HA, Yunginger JW, Burks AW Jr, Schneider LC, Wortel CH, Davis FM, Hyun JD, Shanahan WR Jr. Effect of anti-IgE therapy in patients with peanut allergy. N Engl J Med. 2003;348:986–93.
Sampson HA, Ho DG. Relationship between food-specific IgE concentrations and the risk of positive food challenges in children and adolescents. J Allergy Clin Immunol. 1997;100:444–51.
Buchanan AD, Green TD, Jones SM, Scurlock AM, Christie L, Althage KA, Steele PH, Pons L, Helm RM, Lee LA, Burks AW. Egg oral immunotherapy in nonanaphylactic children with egg allergy. J Allergy Clin Immunol. 2007;119:199–205.
Akdis M, Akdis CA. Mechanisms of allergen-specific immunotherapy. J Allergy Clin Immunol. 2007;119:780–91.
Jones SM, Pons L, Roberts JL, Scurlock AM, Perry TT, Kulis M, Shreffler WG, Steele P, Henry KA, Adair M, Francis JM, Durham S, Vickery BP, Zhong X, Burks AW. Clinical efficacy and immune regulation with peanut oral immunotherapy. J Allergy Clin Immunol. 2009;124:292–300 [300 e291–297].
Vickery B, Lin J, Kulis M, Steele P, Jones SM, Bardina L, Sampson H, Burks AW. Peanut oral immunotherapy (OIT) induces epitope-specific isotype shift from IgE to IgG4. J Allergy Clin Immunol. 2010;125:AB20.
Shreffler WG, Wanich N, Moloney M, Nowak-Wegrzyn A, Sampson HA. Association of allergen-specific regulatory T cells with the onset of clinical tolerance to milk protein. J Allergy Clin Immunol. 2009;123:43–52 [e47].
Breslin M, Pons L, Yue X, Kulis M, Jones SM, Vickery B, Burks AW. Peanut oral immunotherapy (OIT) confers long-term tolerance mediated by decreased T-helper Type 2 (Th2) cytokines and cytokines generated by regulatory T cells (Tregs). J Allergy Clin Immunol. 2010;125:AB20.
Hofmann AM, Scurlock AM, Jones SM, Palmer KP, Lokhnygina Y, Steele PH, Kamilaris J, Burks AW. Safety of a peanut oral immunotherapy protocol in children with peanut allergy. J Allergy Clin Immunol. 2009;124:286–291 [291 e281–86].
Varshney P, Steele PH, Vickery BP, Bird JA, Thyagarajan A, Scurlock AM, Perry TT, Jones SM, Burks AW. Adverse reactions during peanut oral immunotherapy home dosing. J Allergy Clin Immunol. 2009;124:1351–2.
Jones SM, Scurlock AM, Pons L, Perry TT, Morgan AR, Kulis M, Vickery B, Steele P, Kamilaris J, Hiegel AM, Burks AW. Double-blind, placebo-controlled trial of oral immunotherapy (OIT) in peanut (PN) allergic children: a follow-up. J Allergy Clin Immunol. 2010;125:AB58.
Varshney P, Jones SM, Pons L, Kulis M, Steele P, Kemper AR, Scurlock AM, Perry TT, Burks AW. Peanut oral immunotherapy (OIT) induces immunologic changes supporting the development of tolerance. J Allergy Clin Immunol. 2010;125:AB59.
Sicherer SH, Sampson HA. Food allergy. J Allergy Clin Immunol. 2010;125:S116–25.
Avery NJ, King RM, Knight S, Hourihane JO. Assessment of quality of life in children with peanut allergy. Pediatr Allergy Immunol. 2003;14:378–82.
Edie AH, Steele P, Kamilaris J, Stowe R, Dunn A, Chin W, Jones SM, Burks AW. Improvement of quality of life in children with peanut allergy upon development of tolerance to peanut. J Allergy Clin Immunol. 2010;125:AB52.
Clark AT, Islam S, King Y, Deighton J, Anagnostou K, Ewan PW. Successful oral tolerance induction in severe peanut allergy. Allergy. 2009;64:1218–20.
Blumchen K, Ulbricht H, Staden U, Dobberstein K, Beschorner J, de Oliveira LC, Shreffler WG, Sampson HA, Niggemann B, Wahn U, Beyer K. Oral peanut immunotherapy in children with peanut anaphylaxis. J Allergy Clin Immunol. 2010;126:83–91 [e81].
Canonica GW, Bousquet J, Casale T, Lockey RF, Baena-Cagnani CE, Pawankar R, Potter PC, Bousquet PJ, Cox LS, Durham SR, Nelson HS, Passalacqua G, Ryan DP, Brozek JL, Compalati E, Dahl R, Delgado L, van Wijk RG, Gower RG, Ledford DK, Filho NR, Valovirta EJ, Yusuf OM, Zuberbier T, Akhanda W, Almarales RC, Ansotegui I, Bonifazi F, Ceuppens J, Chivato T, Dimova D, Dumitrascu D, Fontana L, Katelaris CH, Kaulsay R, Kuna P, Larenas-Linnemann D, Manoussakis M, Nekam K, Nunes C, O’Hehir R, Olaguibel JM, Onder NB, Park JW, Priftanji A, Puy R, Sarmiento L, Scadding G, Schmid-Grendelmeier P, Seberova E, Sepiashvili R, Sole D, Togias A, Tomino C, Toskala E, Van Beever H, Vieths S. Sub-lingual immunotherapy: world allergy organization position paper 2009. Allergy. 2009;64(Suppl 91):1–59.
Passalacqua G, Lombardi C, Troise C, Canonica GW. Sublingual immunotherapy: certainties, unmet needs and future directions. Eur Ann Allergy Clin Immunol. 2009;41:163–70.
Enrique E, Pineda F, Malek T, Bartra J, Basagana M, Tella R, Castello JV, Alonso R, de Mateo JA, Cerda-Trias T, San Miguel-Moncin Mdel M, Monzon S, Garcia M, Palacios R, Cistero-Bahima A. Sublingual immunotherapy for hazelnut food allergy: a randomized, double-blind, placebo-controlled study with a standardized hazelnut extract. J Allergy Clin Immunol. 2005;116:1073–9.
Webber CM, England RW. Oral allergy syndrome: a clinical, diagnostic, and therapeutic challenge. Ann Allergy Asthma Immunol. 2010;104:101–08 [quiz 109–10, 17].
Kerzl R, Simonowa A, Ring J, Ollert M, Mempel M. Life-threatening anaphylaxis to kiwi fruit: protective sublingual allergen immunotherapy effect persists even after discontinuation. J Allergy Clin Immunol. 2007;119:507–8.
Fernandez-Rivas M, Garrido Fernandez S, Nadal JA, Diaz de Durana MD, Garcia BE, Gonzalez-Mancebo E, Martin S, Barber D, Rico P, Tabar AI. Randomized double-blind, placebo-controlled trial of sublingual immunotherapy with a Pru p 3 quantified peach extract. Allergy. 2009;64:876–83.
Plosker GL, Keam SJ. Omalizumab: a review of its use in the treatment of allergic asthma. BioDrugs. 2008;22:189–204.
Massanari M, Nelson H, Casale T, Busse W, Kianifard F, Geba GP, Zeldin RK. Effect of pretreatment with omalizumab on the tolerability of specific immunotherapy in allergic asthma. J Allergy Clin Immunol. 2010;125:383–9.
Du Toit G, Katz Y, Sasieni P, Mesher D, Maleki SJ, Fisher HR, Fox AT, Turcanu V, Amir T, Zadik-Mnuhin G, Cohen A, Livne I, Lack G. Early consumption of peanuts in infancy is associated with a low prevalence of peanut allergy. J Allergy Clin Immunol. 2008;122:984–91.
Lopez-Exposito I, Song Y, Jarvinen KM, Srivastava K, Li XM. Maternal peanut exposure during pregnancy and lactation reduces peanut allergy risk in offspring. J Allergy Clin Immunol. 2009;124:1039–46.
Sicherer SH, Wood RA, Stablein D, Burks AW, Liu AH, Jones SM, Fleischer DM, Leung DY, Grishin A, Mayer L, Shreffler W, Lindblad R, Sampson HA. Immunologic features of infants with milk or egg allergy enrolled in an observational study (Consortium of Food Allergy Research) of food allergy. J Allergy Clin Immunol. 2010;125:1077–83 [e1078].
Li XM, Srivastava K, Grishin A, Huang CK, Schofield B, Burks W, Sampson HA. Persistent protective effect of heat-killed Escherichia coli producing “engineered”, recombinant peanut proteins in a murine model of peanut allergy. J Allergy Clin Immunol. 2003;112:159–67.
Pochard P, Vickery B, Berin MC, Grishin A, Sampson HA, Caplan M, Bottomly K. Targeting Toll-like receptors on dendritic cells modifies the T(H)2 response to peanut allergens in vitro. J Allergy Clin Immunol. 2010;126:92–7 [e95].
Skripak JM, Nash SD, Rowley H, Brereton NH, Oh S, Hamilton RG, Matsui EC, Burks AW, Wood RA. A randomized, double-blind, placebo-controlled study of milk oral immunotherapy for cow’s milk allergy. J Allergy Clin Immunol. 2008;122:1154–60.
Srivastava KD, Kattan JD, Zou ZM, Li JH, Zhang L, Wallenstein S, Goldfarb J, Sampson HA, Li XM. The Chinese herbal medicine formula FAHF-2 completely blocks anaphylactic reactions in a murine model of peanut allergy. J Allergy Clin Immunol. 2005;115:171–8.
Srivastava KD, Qu C, Zhang T, Goldfarb J, Sampson HA, Li XM. Food allergy herbal formula-2 silences peanut-induced anaphylaxis for a prolonged posttreatment period via IFN-gamma-producing CD8 + T cells. J Allergy Clin Immunol. 2009;123:443–51.
Wang J, Patil SP, Yang N, Ko J, Lee J, Noone S, Sampson HA, Li XM. Safety, tolerability, and immunologic effects of a food allergy herbal formula in food allergic individuals: a randomized, double-blinded, placebo-controlled, dose escalation, phase 1 study. Ann Allergy Asthma Immunol. 2010;105:75–84.
Clark AT, Ewan PW. The development and progression of allergy to multiple nuts at different ages. Pediatr Allergy Immunol. 2005;16:507–11.
Kulis M, Li Y, Pons L, Burks AW. Walnut immunotherapy (IT) as treatment for both cashew and walnut allergy. J Allergy Clin Immunol. 2009;123:S175.
Thyagarajan A, Varshney P, Jones SM, Sicherer S, Wood R, Vickery BP, Sampson H, Burks AW. Peanut oral immunotherapy is not ready for clinical use. J Allergy Clin Immunol. 2010;126:31–2.
Acknowledgments
We would like to thank the subjects and their families for their dedication to the clinical studies at Duke. We would also like to thank the various funding agencies that made this research possible: National Institutes of Health, Food Allergy Initiative, Food Allergy and Anaphylaxis Network, Wallace Research Foundation, Thrasher Research Fund, and National Peanut Board.
Author information
Authors and Affiliations
Corresponding author
Additional information
Mike Kulis, Brian P. Vickery contributed equally to this manuscript.
Rights and permissions
About this article
Cite this article
Kulis, M., Vickery, B.P. & Burks, A.W. Pioneering immunotherapy for food allergy: clinical outcomes and modulation of the immune response. Immunol Res 49, 216–226 (2011). https://doi.org/10.1007/s12026-010-8183-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12026-010-8183-9