Abstract
Knowledge of the biomechanical dynamics of blunt force trauma is indispensable for forensic reconstruction of a wounding event. In this study, we describe and interpret wound features on a synthetic skin model under defined laboratory conditions. To simulate skin and the sub-dermal tissues we used open-celled polyurethane sponge (foam), covered by a silicone layer. A drop tube device with three tube lengths (300, 400, and 500 mm), each secured to a weighted steel scaffold and into which a round, 5-kg Federal dumbbell of length 180 mm and diameter 8 cm was placed delivered blows of known impact. To calculate energy and velocity at impact the experimental set-up was replicated using rigid-body dynamics and motion simulation software. We soaked each foam square in 500 mL water, until fully saturated, immediately before placing it beneath the drop tube. We then recorded and classified both external and internal lacerations. The association between external wounding rates and the explanatory variables sponge type, sponge thickness, and height were investigated using Poisson regression. Tears (lacerations) of the silicone skin layer resembled linear lacerations seen in the clinical literature and resulted from only 48.6% of impacts. Poisson regression showed there was no significant difference between the rate of external wounding for different sponge types (P = 0.294) or different drop heights (P = 0.276). Most impacts produced “internal wounds” or subsurface cavitation (96%). There were four internal “wound” types; Y-shape (53%), linear (25%), stellate (16%), and double crescent (6%). The two-way interaction height by sponge type was statistically significant in the analysis of variance model (P = 0.035). The other two-way interactions; height by thickness and sponge type by thickness, were also bordering on statistical significance (P = 0.061 and P = 0.071, respectively). The observation that external wounds were present for less than half of impacts only, but that nearly all impacts resulted in internal wounds, might explain the observed haematoma formation and contusions so often associated with blunt-force injuries. Our study also confirms the key role of hydrodynamic pressure changes in the actual tearing of subcutaneous tissue. At the moment and site of impact, transferred kinetic energy creates a region of high pressure on the fluid inside the tissue. As a result of the incompressibility of the fluid, this will be displaced away from the impact at a rate that depends on the velocity (or kinetic energy) of impact and the permeability and stiffness of the polymeric foam and skin layer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A significant number of skin wounds encountered by forensic experts are non-ballistic in nature, offering potential insights into causation of death, timing of the insult, weapon used, and the force of impact. The ability to reconstruct a wounding event hinges on the use of as many lines of evidence as possible. Historically, most inferences of non-ballistic, blunt force wound reconstruction have relied on visual examination, photography, and experience [1–3], whereas more recently, techniques such as X-ray examination, scanning electron microscopy, and optical 3D surface digitization have been used [4–6]. Concomitantly, our understanding of molecular biological phenomena associated with wounding has advanced, fuelled by the availability of ever more sophisticated laboratory techniques and tests [7, 8]. Yet to interpret the causation and to estimate the forces involved in a particular wound, a better understanding of the biomechanics of severe impact-stresses generated in skin during blunt force wounding is crucial.
Previous biomechanical models of wounding are generally limited to ballistic injuries [e.g. 9, 10] or stabbing [11–13]. Silver et al. [14] reviewed the mechano-biology of external forces applied to the skin, with special reference to the mechanical properties and the cellular and extracellular components of the dermis. In two key papers, Shergold and Fleck [15, 16] developed micromechanical models of deep penetration of skin by small diameter sharp and blunt punches, and showed that the penetration mechanism depended on the geometry of the punch tip. These authors used foam-based models and showed that although a sharp tip penetrated the skin by wedging open a planar (mode I) crack, a blunt tip penetrated via a ring (mode II) crack. Recently, we reviewed craniofacial blunt force trauma from a biomechanical perspective, and introduced our own model and its preliminary findings [17]. We concluded that wounding can be modelled in a basic simulation of the contact events during blunt force impact and that these results can be evaluated quantitatively. The purpose of this study was to describe and interpret wound features on a synthetic skin model under defined laboratory conditions. Limited data of such approaches are available from wounding models. In an early study, Lee et al. [18] created artificial blunt-force injuries using nineteen cadavers, and assessed these according to frequency, length, and depth of wounding. A more recent study by Thali et al. [19] saw the introduction of an artificial skin–skull–brain model consisting of silicone rubber casts, on to which a mass was dropped to create lacerations. Unfortunately, neither the impact forces used, nor quantitative data on the injuries caused were published. The authors did, however, find that their drop tube model produced “injuries” that were fully comparable to the morphology of actual blunt-force injuries observed in the crania of humans. For this reason, the current laboratory study was undertaken to provide benchmark data describing aspects of blunt-force injury to an organ like skin that can be built upon in terms of understanding the features of wounding found in forensic cases. An intrinsic assumption of our model is that the dermis and underlying subcutaneous tissue including fat and muscle, often overlying bone, is composed essentially of water-filled semi-permeable cells similar to the porous water-filled foam investigated. We were interested in developing a simple, replicable model of the biomechanical dynamics of non-ballistic skin wounding, which could form the basis of future research into skin trauma. Our model clearly demonstrates the key role played by hydrodynamic pressure changes in the actual tearing of subcutaneous tissue. At the moment and site of impact, kinetic energy is transferred, creating a region of high pressure inside the tissue, which will be displaced away from the impact at a rate that depends primarily on the velocity of the impacting object and the permeability of the fluid filled foam. The extent of the “damaged” tissue will depend on the diameter and kinetic energy of the impacting object.
Materials and method
The dermis subcutaneous tissue structure overlying bone consists primarily of fluid filled semi-permeable cells. The skin seals this semi-permeable structure until rupture occurs as a result of wounding. To simulate the sub-dermal tissues we used polyurethane sponge (foam). The internal architecture of a sponge is an important determinant of its biomechanical behaviour. Closed-cell sponges consist of cells completely enclosed in a polymer matrix, resulting in a dense material used traditionally for flotation and insulation purposes. In contrast, open-cell sponges have cell walls that are broken and bonded together, thus resulting in a soft, porous permeable material. In this study we used two open celled foams of different density—Dunlop Enduro 38–200, and Dunlop Elephant 34–115. Here the first number gives the sponge density (weight of polyurethane in kg m−3) and the second refers to its hardness (resistance to compression in N). In this study no attempt was made to match the permeability of the foam to that of subcutaneous tissue but rather to establish the response of the model matched observed and reported blunt object impact-induced wounding patterns. In line with the studies by Shergold and Fleck [15, 16] we used a silicone rubber layer on the foam to simulate the skin because it has similar physical properties (tensile strength skin = 10–20 MPa, silicone = 3.5–15 MPa; tear strength skin = 2–20 kN m−1, silicone = 5–40 kN m−1). A uniform layer of Deguform silicone was mixed to a 1:1 ratio in a Multivac stirring unit and then poured into a flat mould. Two thicknesses were used—1.5 and 3.5 mm. Before the layer had set, the sponge samples (each 25 mm thick, 150 mm × 150 mm) were gently placed on the silicone to ensure adhesion. Once set, each sample was peeled from the mould and the edges trimmed flush with the sponge. Attachment of the skin to the underlying foam was excellent and throughout all the tests undertaken no evidence of debonding of the silicone from the foam was observed.
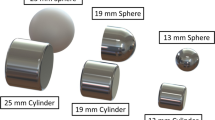
As suggested by Lee et al. [18] and Thali et al. [19], we used a drop tube device to deliver blows of known impact. We used three tube lengths (300, 400, and 500 mm), each secured to a weighted steel scaffold into which a round, 5-kg Federal dumbell of length 180 mm and diameter 8 cm was placed (Fig. 1). The target foam was placed unbonded on a wooden base.
To calculate energy and velocity at impact the experimental setup was replicated by rigid-body dynamics and motion simulation software (MSC VisualNastran 4D, MSC Software, USA). The results are summarised in Table 1. To simulate an aspect of the fluid-content of the subdermal tissues, we soaked each foam square in 500 mL water, until fully saturated immediately before placing it beneath the drop tube. Tests were also conducted on dry foam samples for comparison. The morphology of the “wounds” was assessed visually and their maximum lengths measured using a vernier scale (±0.05 mm).
All statistical analysis were conducted using SPSS 14.0 (SPSS, Chicago, USA) or STATA 9.1.2 (StataCorp, Texas, USA). A P-value < 0.05 was considered to be statistically significant. The association between external wounding rates and the explanatory variables sponge type, sponge thickness, and height were investigated using Poisson regression. We used Poisson regression because the outcome variable was rates (rather than the continuous outcomes that are needed for linear regression). All of the variables were included in the regression model. Interactions between the explanatory variables were also investigated. Group mean values of internal wound sizes were compared using three-way ANOVA grouped on sponge type, sponge thickness, and height. The main effect, all two way interactions, and the three way interaction were included in the model to investigate the effects of these factors on the size of the internal wound.
Results
Morphology of “wounds”
All external “wounds” (i.e. lacerations of the silicone skin layer) resembled linear lacerations seen in the clinical literature (Fig. 2). In contrast, there were four internal “wound” shapes (i.e. those within the body of the foam); linear, Y-shaped, double crescent, and stellate (Fig. 3). Margins were irregular, with “tissue-bridges” often present. Of the four internal “wound” types, the most common was a Y-shape (53%), followed by linear (25%), stellate (16%), and double crescent (6%) forms. For the impact events of the unhydrated foam, no surface skin nor subsurface cracks in the foam were observed for either foam type or silicone skin thickness.
Example of a linear external “wound” produced by blunt trauma (top). Actual example of a linear external wound (bottom) (Source: Hamilton et al. [20])
Presence of external “wounding”
Overall, only 34 (48.6%) of impacts resulted in external “wounds”. Table 2 summarises our data for the presence of external “wounds” after blunt impacts on each of the foam squares investigated. From the Poisson regression analysis there was no significant difference between the rate of external wounding for the different sponge types (P = 0.294) or for the different heights (P = 0.276). There was a tendency toward the rate of external wounding being lower for the 3.5 mm skin compared to the 1.5 mm skin although it did not reach statistical significance (rate for 1.5 mm = 64.7%, rate for 3.5 mm = 33.3%, incidence rate ratio = 0.51, 95% CI: 0.25 to 1.03, P = 0.062). Interactions between the explanatory variables were not statistically significant and, therefore, these were not included in the final Poisson regression model (Table 3).
Internal “wounds”
Most impacts produced internal “wounds” or subsurface cavitation (96%). ANOVA did show that height had an effect on wounding. The effect of height on the size of the wound depended on the sponge type but it did not depend on the thickness of the sponge (the two-way interaction height/sponge type was statistically significant but the three way interaction height/sponge type/thickness was not). There was a tendency toward the effect of height depending on thickness but it was not statistically significant (height/thickness, P-value = 0.061).
The two-way interaction height/thickness was not statistically significant in the Poisson regression model. Hence if there is an effect of height on the presence of external wounding, it does not depend on the thickness of the sponge. In fact, the main factor, height, is not statistically significant and hence the presence of external wounding did not depend on height. Although not statistically significant, there was a tendency toward the rate of external wounding being higher in the 1.5 mm group than in the 3.5 mm group (irrespective of type of sponge or height).
Discussion
The objective of this study was to develop a simple, replicable model of the biomechanical dynamics of blunt force, non-ballistic skin wounding, which would enable us to better understand the mechanisms behind the traumatic end-results observed either clinically or in the morgue [20, 21]. Unlike previous such attempts, our model incorporates a simulation of skin fused to subcutaneous tissue. In other words, we are able to model the skin/subcutaneous complex as an integrated energy-absorbing system. Our first interesting observation was that although external wounds were present after 48.6% of impacts only, nearly all impacts (96%) resulted in internal wounds. The presence of internal wounds, irrespective of whether there was external laceration, corresponds with the observed transient lateral displacement of tissue, which occurs during trauma [22] and might explain haematoma formation and contusions so often associated with blunt-force injuries.
The impact of the object on the unsaturated foams, with either skin thickness, resulted in no surface or subsurface cracking or tearing wounds (Fig. 4). The tensile forces on the silicone skin were lower than the tear strength of the film and, therefore, no cracking was observed under the loads/impact conditions studied here. This may be explained by the ability of the unhydrated foam to readily compress or distort, as the empty cells are providing the compliance needed. The ability of the foams to collapse or densify results in buckling deformation of the local struts of the foam rather than a state of tension. Because of the localised strut collapse and the compressibility of the trapped air within the foam the rate of deceleration of the impacting body will be lower, resulting in the total kinetic energy being absorbed over a large volume of foam and skin layer. The tensile biaxial strain is relatively low, because the modulus of the skin is far greater than that of the foam, and is determined by the radius of curvature of the impacting object and extensional strain by the deflection of the foam. Consequently, the resistance force developed in the silicone skin was not sufficient to create a large biaxial tension, which would cause it to tear.
With the hydrated foams the situation is very different. On initial impact the water-filled foam acts as a highly rigid body because the amount of distortion in the structure depends on the ability of the water to flow away from the high-pressure region directly beneath the contact area (Fig. 5). As such the silicone skin will become highly compressed and squeezed to a much thinner layer between the impacting body and the water-filled foam. This results in high biaxial tensile stresses in the silicone skin and also in the foam attached to it, because the fluid prevents the foam from collapsing. The high tensile strains in the silicone may or may not initiate cracking dependent on the tensile strain developed in the skin layer. Because silicone has a large tensile extension before failure very limited cracking is observed. On the other hand, the polyurethane material has a much lower strain to failure (tensile strength of silicone is approx. 10.3 MPa, and elongation is 100–800%, whereas the polyurethane sponge has a tensile strength of 55 kPa and elongation to failure of 150–180% [23]. This difference in tensile strength and percentage elongation may explain the greater incidence of cracking of the foams than of the silicone skin surface. A curious and unexplained finding was that internal wound size was sometimes larger for lower drop heights. These findings were not statistically significant, however, and hence await further investigation.
Schematic representation of an impact on filled foam. The hydrated foam acts as highly rigid body, hence high biaxial tensile stresses in the skin and foam result in tearing. The polyurethane material is a much stiffer polymer and as such will not sustain large tensile strains before failure, thus the foam attached to the skin will exceed its tensile failure strain before the skin and hence a greater incidence of cracking occurs for the foams than for the silicone skin
Alternatively, for a solid polymeric material one must consider viscoelastic and viscoplastic deformation. When an indentor impacts such a body, there is the possibility of dynamic viscoelastic and viscoplastic deformation of the material. Viscoelastic deformation is recovered on removal of the load, and viscoplastic deformation remains. In the absence of fluid saturation of the foam, the deformation mechanism is, initially, buckling of the cell’s walls, which may then result in tension and fracture if the tensile strain in the cell walls is sufficiently high. As the strain rate increases, the yield stress of polymeric material increases and therefore failure requires higher deviatoric stresses. The second cause of tensile stress development in the cell walls during impact of a fluid filled foam is because of the gradient in macroscopic compressive stresses, owing to dynamic fluid flow to reduce this gradient. Fracture processes are controlled differently; they are less strain rate dependent than the yield process. When a cell has ruptured it will become a stress concentrator, and if the strain energy release rate exceeds a critical value, a crack will extend. In contact-induced loading the localised nature of the stresses result in limited crack extension before crack arrest.
Preliminary experiments during the development of our model clearly showed that our replica required water saturation for laceration to occur. This observation suggests that hydrodynamic pressure gradients in the subcutaneous region during a blunt impact event may play a key role in the actual tearing of tissue. The magnitude of the hydrostatic pressures developed in fluid-filled foams depends on the contact strain rate, the permeability of the foam, and the viscosity of the saturating medium. The water-soaked sponges therefore result in hydrostatic pressure within the trapped water. Such pressure will limit the deformation strain within the foam cell walls because they are unable to buckle, resulting in a higher deviatoric strain within the deformable skin layer. In this study there was no residual deformation of the foam structure after impact apart from cracking if, and only if, it occurred. Such observations rule out the possibility of yielding on the skin or subsurface polymer material. At the moment and site of impact, kinetic energy is transferred to the target, creating a region of high pressure localised about the contact site on the skin and subsurface fluid-filled tissue. In the event in which this fluid-structure interaction generates significant tensile stresses and strains in the tissue, rupture of the cellular components may occur. It has been suggested that an intense pressure pulse (e.g. blunt force trauma) will result in an instant shock wave that propagates through the material and results in changes in local physical properties, for example stress, strain, and density [24]. This is known as hydrodynamic cavitation and results in a rapid release of energy [25]. It has also been suggested that the shock-disturbed region will further unload as the magnitude of the shock strength decreases during wave propagation through the tissues [26]. Under the relatively low impact velocities of this study it is unlikely that such shock-induced cavitation processes occur as the stress wave velocities within the fluid-filled foam are expected to be much greater than the impact velocities. On this basis blunt impact injuries may be considered as equivalent to quasi-static contacts whereas ballistic impact injuries where the impact velocities exceed the stress wave velocities within the body do necessitate consideration of hydrodynamic cavitation events.
Educational message
-
1.
Biomechanical modelling tackles conceptual problems of wound reconstruction.
-
2.
A drop-tube system which delivers known impacts to a silicone–sponge model of skin and subcutaneous tissues can provide useful insights into the dynamics of non-ballistic wounding.
-
3.
Our model suggests impact with a blunt object generates hydrodynamic pressure gradients which may play a key role in the actual tearing of subcutaneous tissue.
-
4.
Although external wounds were only present in 48.6% of impacts, nearly all impacts (96%) resulted in internal wounds. This might explain the observed haematoma formation and contusions so often associated with blunt-force injuries.
References
Zugibe FT, Costello JT. Identification of the murder weapon by intricate patterned injury measurements. J Forensic Sci 1986;31:773–7.
Takaziwa H, Nakamura I, Hashimoto M, Maekawa N, Yamamura M. Toolmarks and peculiar blunt-force injuries related to an adjustable wrench. J Forensic Sci 1989;34:258–62.
Clark EGI, Sperry KL. Distinctive blunt-force injuries caused by a crescent wrench. J Forensic Sci 1992;37:1172–8.
Ohshima T. Forensic wound examination. J For Sci 2000;113:153–64.
Rawson RB, Starich GH, Rawson RD. Scanning electron microscopic analysis of skin resolution as an aid in identifying trauma in forensic investigations. J Forensic Sci 2000;45:1023–7.
Thali MJ, Braun M, Dirnhofer R. Optical 3D surface digitizing in forensic medicine: 3D documentation of skin and bone injuries. J Forensic Sci 2003;137:203–8.
Hernandez-Cueto C, Girela E, Sweet DJ. Advances in the diagnosis of wound vitality: a review. Am J Forensic Med Pathol 2000;21:21–1.
Bonelli A, Bacci S, Norelli GA. Affinity cytochemistry analysis of mast cells in skin lesions: a possible tool in the timing of lesions after death. Int J Leg Med 2004;117:331–4.
Thali MJ, Kneubuehl BP, Zollinger U, Dirnhofer R. A high-speed study of the dynamic bullet-body interactions produced by grazing gunshots with full metal jacket and lead projectiles. For Sci Int 2003;132:93–8.
Jain SK, Bhattachareyya CN, Badonia B, Sing RP. Study of unusual phenomenon of contact firing on gelatine block using .38 Special revolver—forensic importance. For Sci Int 2003;133:183–9.
Knight B. The dynamics of stab wounds. Forensic Sci 1975;6:249–55.
Green MA. Stab wound dynamics—recording technique for use in medico-legal investigations. J Forensic Sci 1978;18:161–3.
Ankerson J, Birbeck AE, Thomson RD, Vanezis P. Puncture resistance, tensile strength of skin. Proc Int Mech Eng 1999;213H:493–501.
Silver FH, Siperko LM, Seehra GP. Mechanobiology of force transduction in dermal tissue. Skin Res Tech 2003;9:3–23.
Shergold OA, Fleck NA. Mechanism of deep penetration of soft solids, with application to the injection and wounding of skin. Proc Roy Soc Lond A 2004;460:3037–58.
Shergold OA, Fleck NA. Experimental investigation into the deep penetration of soft solids by sharp and blunt punches, with application to the piercing of skin. Trans ASME 2005;127:838–48.
Kieser JA, Whittle K, Wong B, Ichim I, Waddell JN, Swain M, Taylor M, Nicholson H. Understanding craniofacial blunt-force injury: a biomechanical perspective. Forensic Path Rev (in press).
Lee R, Gamble W, Meyer M, Manson P. Patterns of facial laceration from blunt force trauma. Plast Reconstr Surg 1996;99:1544–54.
Thali M, Kneubeul B, Dirnhofer R. A skin-skull-brain model for the biomechanical reconstruction of blunt forces to the human head. Forensic Sci Int 2002;125:195–200.
Hamilton J, Sunter J, Cooper P. Fatal hemorrage from simple lacerations of the scalp. For Sci Med Pathol 2005;1:267–71.
O’Callaghan P, Jones M, James D, Leadbeatter S, Holt C, Nokes L. Dynamics of stab wounds: force required for penetrating of various cadaveric human tissues. Forensic Sci Int 1999;104:173–8.
United States of America Department of Defence. Emergency war surgery. 3rd ed. Borden Institute, Washington DC; 2004, p.12–13.
Callister WD. Materials science and engineering. New York: John Wiley; 2007.
Cooper GJ, Townsend DJ, Cater SR, Pearce BP. The role of stresswaves in thoracic visceral injury from blast loading: modification of stress transmission by foams and high-density materials. J Biomech 1991;24:273–85.
Young F. Cavitation. London: Imperial College Press, 1999.
Li QM, Reid SR. About one-dimensional shock propagation in a cellular material. Int J Impact Eng 2006;32:1898–906.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Whittle, K., Kieser, J., Ichim, I. et al. The biomechanical modelling of non-ballistic skin wounding: blunt-force injury. Forensic Sci Med Pathol 4, 33–39 (2008). https://doi.org/10.1007/s12024-007-0029-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12024-007-0029-y