Abstract
Neuroendocrine neoplasms (NENs) are a heterogeneous group of epithelial neoplastic proliferations that irrespective of their primary site share features of neural and endocrine differentiation including the presence of secretory granules, synaptic-like vesicles, and the ability to produce amine and/or peptide hormones. NENs encompass a wide spectrum of neoplasms ranging from well-differentiated indolent tumors to highly aggressive poorly differentiated neuroendocrine carcinomas. Most cases arise in the digestive system and in thoracic organs, i.e., the lung and thymus. A correct diagnostic approach is crucial for the management of patients with both digestive and thoracic NENs, because their high clinical and biological heterogeneity is related to their prognosis and response to therapy. In this context, immunohistochemistry represents an indispensable diagnostic tool that pathologists need to use for the correct diagnosis and classification of such neoplasms. In addition, immunohistochemistry is also useful in identifying prognostic and theranostic markers. In the present article, the authors will review the role of immunohistochemistry in the routine workup of digestive and thoracic NENs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The gastroenteropancreatic (GEP) system, lungs, and thymus are the most common sites of occurrence of neuroendocrine neoplasms (NENs). NENs are a heterogeneous group of epithelial neoplastic proliferations that irrespective of their primary site share features of neural and endocrine differentiation including the presence of secretory granules, synaptic-like vesicles, and the ability to produce amine and/or peptide hormones. NENs encompass a wide spectrum of neoplasms ranging from indolent to highly aggressive malignancies and their clinico-pathological features are mainly related to their morphology and immunohistochemical profile, which also depend on their site of origin.
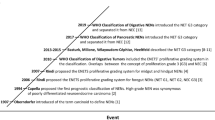
The term carcinoid (i.e., carcinoma-like) was proposed by Siegfried Oberndorfer in 1907 to define a series of intestinal epithelial neoplasms showing a blander morphology and a more benign/indolent behavior than intestinal adenocarcinomas [1]. The neuroendocrine nature of such lesions was only later unveiled by Masson, who demonstrated argentaffin granules in carcinoids [2]. Since then, this term has been used to diagnose neoplasms showing morphological and immunohistochemical features of neuroendocrine differentiation. However, as digestive NENs originate from several different neuroendocrine cell types and show heterogeneous clinical, pathological, and molecular features, the term “carcinoid” has been discouraged in diagnostic practice in favor of the more general “neuroendocrine tumor” [3, 4]. Conversely, in the lung and thymus, the term carcinoid has been retained over the years to describe low- to intermediate-grade NENs, because the spectrum of NENs, in terms of morphology, immunophenotype, and clinical syndromes, is more limited in these sites than in the GEP system. As a general principle, lung and thymic carcinoids correspond to well-differentiated neuroendocrine tumors (NETs), as classified in the GEP system. As far as poorly differentiated NENs are concerned, the term neuroendocrine carcinoma (NEC) of small and large cell types is used in both thoracic and GEP sites, as these neoplasms show comparable morphological and prognostic features in the two systems [5, 6]. In fact, the WHO classifications of both thoracic and digestive tumors (Table 1) recognize two separate groups of NENs with different morphological, clinical, and molecular features: well-differentiated tumors (carcinoids and NETs), which are indolent or low-grade malignant neoplasms, and poorly differentiated neuroendocrine carcinomas (NECs), which are highly aggressive diseases with a tendency to early dissemination and an ominous prognosis [5, 6]. This distinction is crucial for the different therapeutic approaches to the two categories, which are separate entities despite a similar neuroendocrine phenotype. Intriguingly, thoracic NECs, mainly of the small cell type, are more frequent than well-differentiated tumors (carcinoids) of the same site, whereas in the GEP system well-differentiated neuroendocrine tumors (NETs) occur more commonly than NECs [7].
A correct diagnostic approach is crucial for the management of patients with digestive and thoracic NENs, because of the high clinical and biological heterogeneity of these neoplasms. The most critical aspects in diagnosing NENs can be summarized as follows: (i) identifying the coexistent neuroendocrine and epithelial nature of the neoplasm, (ii) recognizing the aggressive potential of NETs, (iii) defining additional prognostic and predictive markers, and (iv) finding clues to the occult site of origin of NENs presenting as metastatic lesions. In this context, immunohistochemistry represents an indispensable tool for the practicing pathologist and several markers are now available in routine practice and several others are promising and under clinical validation (Table 2).
Is It Really Neuroendocrine?—General Neuroendocrine Markers
Although morphology alone may be sufficient in recognizing the neuroendocrine phenotype of thoracic and digestive NETs, immunohistochemistry is always required to confirm the diagnosis. The neuroendocrine nature of NECs may often be less evident and immunohistochemical stains for general neuroendocrine markers are mandatory in the differential diagnosis with both epithelial and non-epithelial poorly differentiated neoplasms. In the lung, although the morphological picture of small cell carcinoma is more characteristic of a neuroendocrine lesion, this might be misleading and sometimes worrisome in large cell neuroendocrine carcinoma as compared to other poorly differentiated non-neuroendocrine lung carcinomas, at first instance large cell carcinoma. Therefore, it might be advisable to test the presence of general neuroendocrine markers in lung carcinomas made of large cells and lacking squamous or glandular differentiation, even when neuroendocrine morphology is not clear-cut, since the clinical management of large cell carcinomas NOS (not otherwise specified) is significantly different to large cell neuroendocrine carcinomas. It is worth noting that according to the WHO 2015 classification of lung tumors, the positivity of at least one pan-neuroendocrine marker in > 10% of cells is sufficient for the identification of large cell neuroendocrine carcinoma in the presence of appropriate morphology [5].
Chromogranin A and Secretory Granule-Related Proteins
Chromogranin A, chromogranin B, and secretogranin II (chromogranin C) represent the major constituents of neuroendocrine secretory granules [8, 9]. The most commonly used anti-chromogranin antibody in routine diagnostic practice is the monoclonal antibody LK2H10, developed by Lloyd and Wilson, directed against chromogranin A [8]. Antibodies to chromogranin B and secretogranin II are available, but are not in general use. Chromogranin A is strongly expressed in normal neuroendocrine cells and, together with synaptophysin, it is the first-choice marker to confirm the neuroendocrine nature of a neoplasm. Chromogranin A is a very specific neuroendocrine marker but the immunostaining varies with the density of secretory granules in tumor cells. Consequently, the strong and granular cytoplasmic immunoreactivity seen in NETs and carcinoids may be weak or even absent in NECs, whose cells contain few mature secretory granules. Indeed, in positive cases, its pattern may be focal with a characteristic, but sometimes poorly recognizable, fine paranuclear dot-like pattern (Fig. 1). Furthermore, a subset of NETs, mainly including L-cell NETs of the hindgut, preferentially express chromogranin B and secretogranin II, rather than chromogranin A, which could be negative in these tumors [10, 11]. For these reasons, the combined use of chromogranin A and synaptophysin is always advisable.
In well-differentiated neuroendocrine tumors (NETs), chromogranin A immunoreactivity is strong and diffuse in the cytoplasm of almost all neoplastic cells (a). In contrast, in poorly differentiated neuroendocrine carcinomas (NECs), especially in the small cell subtype, chromogranin A expression can be focal and frequently shows a paranuclear dot-like immunoreactivity (b)
Synaptophysin and Synaptic Vesicle-Related Proteins
Synaptophysin is an integral membrane calcium-binding glycoprotein, which is the main constituent of synaptic vesicles of neurons [12]. In normal and neoplastic neuroendocrine cells, synaptophysin is present in cytoplasmic microvesicles and not in secretory granules [12], and it represents the most sensitive general neuroendocrine marker, being expressed both in well-differentiated and in poorly differentiated neoplasms. However, it is not a specific neuroendocrine marker, as it is also expressed in non-neuroendocrine neoplasms, such as adrenal cortical carcinomas, neuroblastomas, olfactory neuroblastomas, and Ewing sarcomas/PNETs [12, 13].
Other proteins associated with synaptic vesicles can be found in normal and neoplastic neuroendocrine cells and may be used as neuroendocrine markers. Among these is synaptic vesicle protein 2 (SVP-2) which is also intensely expressed in hindgut NETs, in which chromogranin A is generally absent and synaptophysin immunostaining may be weaker than elsewhere [14]. Vesicular monoamine transporters 1 and 2 (VMAT1 and VMAT2) are responsible for the vesicular transport of norepinephrine, epinephrine, dopamine, serotonin, and histamine and are differentially expressed in neurons and in neuroendocrine cells. They are also present in neuroendocrine cells and tumors, with different patterns of expression in specific tumor types. Among GEP NETs, VMAT1 is consistently expressed in ileal NETs, composed of enterochromaffin (EC) cells, whereas VMAT2 is a good marker for gastric enterochromaffin-like (ECL)-cell NETs (Fig. 2). Antibodies anti-VMATs have also been shown to stain pulmonary NENs and may be considered as general neuroendocrine markers [15,16,17].
Other Markers
A number of antigens have been proposed as general neuroendocrine markers. As a whole, most of them are not as sensitive and specific as synaptophysin and chromogranin A; however, they may be of use when the immunostaining for one of these markers is weak or absent.
Enzymes Involved in Hormone Synthesis and Metabolism
Neuron-specific enolase (NSE) has been widely used as a general neuroendocrine marker. However, its specificity has been debated because anti-NSE antibodies cross-react with other dimeric isoforms of enolase expressed in non-neuronal and non-neuroendocrine cells [18]. This marker is not currently included in the diagnostic immunohistochemical panel for NENs.
Another enzyme used as a general neuroendocrine marker is the protein gene product 9.5 (PGP9.5)/ubiquitin-C-terminal hydrolase 1 (UCHL-1) protein, a thiol protease that recognizes and hydrolyzes a peptide bond at the C-terminal of ubiquitin, and is involved in the processing of ubiquitin precursors and ubiquitinated proteins. PGP9.5 is expressed in neurons, nerve fibers, and in a variety of neuroendocrine cells and it has been proposed and used to confirm the neuroendocrine nature of a neoplasm [19, 20]. However, several studies have also demonstrated PGP 9.5 expression in non-neuroendocrine cells and tumors, both epithelial and not, such as pancreatic adenocarcinoma, plasma cell myeloma, and soft tissue neoplasms [21,22,23,24].
Other enzymes, which are active in the biosynthesis and metabolism of amine and peptide hormones, have been proposed as general neuroendocrine markers. In particular, L-DOPA decarboxylase (L-aromatic amino acid decarboxylase) is widely distributed in well- and poorly differentiated NENs [17, 25]. By contrast, enzymes such as tyrosine hydroxylase, dopamine β-hydroxylase, phenylethanolamine N-methyl transferase, and histidine decarboxylase have more limited tissue distribution and are confined to the sites of specific amine biosynthesis [17, 26]. In addition, a number of endopeptidases and carboxypeptidases, required in the activation of prohormones to biologically functioning hormones, have been used as general neuroendocrine markers. Among these, prohormone convertase PC1/PC3 and PC2 and carboxypeptidase H and E have been studied [27].
Surface Antigens
Two cell surface proteins, classified as a cluster of differentiation (CD), have also been used as general neuroendocrine markers. CD56, which is the neural cell adhesion molecule (N-CAM), has been localized immunohistochemically in a wide spectrum of human cells, including natural killer and T lymphocytes, thyrocytes, renal cells, adrenal cortex cells, myocytes, and neuroendocrine cells [28]. It has high sensitivity in identifying the neuroendocrine phenotype of a neoplasm; however, it lacks specificity, as anti-CD56 antibodies also stain other neoplasms, such as well-differentiated thyroid carcinomas, lung squamous cell, carcinoma, hepatocellular carcinoma, cholangiocarcinoma, renal cell carcinoma, ovarian carcinoma, endometrial carcinoma, Wilms’ tumor, neuroblastoma, and plasma cell myeloma [28,29,30,31,32,33,34]. CD57, which was firstly identified on the surface of natural killer cells and on a subset of T-lymphocytes, is identified in immunohistochemistry by the HNK-1 antibody directed against the Leu7 antigen [35]. Further studies have showed CD57 immunohistochemical expression in a variety of normal and neoplastic cell types, including oligodendroglial cells, Schwann cells, epithelial cells, and neuroendocrine cells [36, 37].
Achaete-Scute Homolog 1
Achaete-scute complex-like 1 (ASCL1), or Achaete-scute homolog-1, termed mASH1 in rodents and hASH1 in humans, is a member of the basic helix-loop-helix family. It is a transcription factor involved in neuroendocrine cell differentiation and in the development of neuroendocrine cells of the thyroid, adrenal medulla, and foregut [38, 39]. Monoclonal antibody anti-mASH1 (Mab-ASH1) and polyclonal antisera anti-hASH1 (poly-ASH1) are available for immunohistochemistry, and Mab-ASH1 (which cross-reacts with hASH1) has shown a higher sensitivity and specificity in detecting neuroendocrine differentiation [40]. Although it was suggested that ASH1 could be a marker for poorly differentiated NECs of the lung [41], its expression in extra-pulmonary NECs, both of the digestive system and of other sites, has been well documented [40, 42]. The high value of ASH1 in the immunohistochemical workup of NENs relies on the fact that it seems to be expressed exclusively in NECs, whereas in NETs its expression is lacking, except for a subset of lung carcinoids [40, 42]. In small biopsies, ASH1 may thus be helpful, together with Ki-67, in the differential diagnosis between high-grade and low-grade NENs [40, 42]. In addition, as ASH1 expression seems to be restricted to NECs, it can also be used as a general neuroendocrine marker in the differential diagnosis of high-grade neoplasms [42]. However, its diagnostic sensitivity and specificity are not assessed in thymic tumors so far and deserve further investigation.
Hormonal Markers
In addition to general neuroendocrine markers, in specific cases, the use of hormonal markers can be included in the routine diagnostic workup. Indeed, their use can be of help in identifying the primary site of occult metastatic NETs (see the pertinent paragraph below). In addition, these additional immunohistochemical tests can be specifically requested by clinicians, in selected cases, to provide information for a better evaluation of the clinical profile and for the patient’s follow-up.
Is It Really Epithelial?—Cytokeratins
The demonstration of the epithelial nature of neoplastic cells is important in the diagnosis of both NETs and NECs because they have non-epithelial mimics. Although a fraction of NENs may not express epithelial markers, cytokeratin-negative NETs should be differentiated from paragangliomas [43]. In addition, cytokeratin-negative NECs, particularly in small biopsies, may be confused with other neuroectodermal neoplasms and with neuroendocrine markers-expressing sarcomas [44, 45].
The most useful epithelial markers are cytokeratins (CKs). The antibodies directed against pools of CKs (CK AE1/AE3) and low molecular weight CK8 (CAM 5.2, which cross-reacts with CK18) are the most commonly used in immunohistochemical routine practice. Antibodies directed against specific CKs may be useful in different settings. First, high molecular weight CKs are usually negative in NENs, with special reference to poorly differentiated forms such as lung small cell carcinomas and represent a negative surrogate neuroendocrine marker, useful in excluding, for example, small cell/basaloid squamous cell carcinoma variants. Moreover, CK20 expression is highly consistent with Merkel cell carcinoma, whereas it is negative in lung NECs [46,47,48].
High Grade or Low Grade?—Markers for Proliferation and Around
The discrimination between high-grade and low-grade NENs is one of the most important issues in diagnosing NENs. On this topic, the classifications of digestive and thoracic neoplasms diverge, so they will be approached separately.
Gastroenteropancreatic NENs
The prognostic classification of NENs of the tubular gut and pancreas largely relies on the proliferation fraction of tumor cells, defined both as mitotic rate and as Ki67-related proliferative index [6, 49]. Mitotic count represents an indirect method for estimating the proliferative fraction of tumor cells and it is incorporated in the classification of NENs of various sites [5, 6, 49, 50]. However, counting mitosis on histopathological sections may be very time-consuming and the intra- and inter-observer agreement is frequently poor. For GEP NENs, and especially for NETs, it is recommended to express the mitotic index as the number of mitotic figures in at least 50 HPFs in hot spot areas [51]. It has been recently demonstrated that the evaluation of mitotic count using phosphohistone H3 (PHH3)-immunostained sections improves the inter-observer agreement in mitotic rate assessment and in grade assignment in both cytological and histological specimens of well-differentiated NETs [52,53,54]. However, as mitosis represents only one aspect of the proliferating cell, to better assess the proportion of neoplastic cells in all phases of the cell cycle, immunohistochemical markers of proliferation have been optimized.
Ki-67 antigen is a cell proliferation marker that was first identified by the monoclonal antibody Ki-67 (named from Kiel, the city of the experiments, and from the number of the original clone in the 96-well plate), of which it kept the name [55]. Ki-67 antigen is expressed in the nuclei of normal and neoplastic proliferating cells, along all cell cycle phases (G1, S, G2, and M), while it is absent from resting cells in the G0 phase. The Ki-67 labeling index is the percentage of immunoreactive neoplastic nuclei over the total of neoplastic nuclei and it is considered a good proliferation marker, with a close correlation to the real growth fraction of the neoplastic population [56]. Since the first demonstration of its prognostic value in non-Hodgkin lymphoma [57], the role of the Ki-67 labeling index in defining tumor grade and in predicting patient outcome has been investigated in virtually all known human neoplasms. As the original Ki-67 antibody cannot be used on formalin-fixed and paraffin-embedded histological samples, alternative antibodies have been sought. Currently, the most used anti-Ki-67 antibody is MIB (Molecular Immunology Borstel) 1, which gives a good immunostaining on routine histopathological sections and has totally replaced the PC10 antibody, which recognizes the proliferating cell nuclear antigen (PCNA), another, less specific, proliferation marker [58]. The important prognostic value of the Ki-67 labeling index in NENs has gained almost universal consensus [59], and neuroendocrine neoplasms of the GEP system are currently classified by the World Health Organization (WHO) on the basis of morphological differentiation, mitotic count and the Ki-67 index (Table 1) [6, 49]. In light of the growing importance of the Ki-67 labeling index in the prognostic classification of NENs, methods for assessing it have been a matter of debate. The WHO grading defines the Ki-67 labeling index as the percentage of Ki-67-immunoreactive cells on a total of 500–2000 neoplastic cells, counted in the areas of higher nuclear labeling (“hot spots”). For the calculation of the Ki-67 index, all the immunohistochemically labeled nuclei, regardless of the staining intensity or whether the nuclei show a speckled expression pattern or are diffusely stained, need to be counted for the scoring process [59]. Different methods for counting Ki-67 immunoreactive cells can be used: eye-ball estimation, automated counting by image analyzer, manual eye-counting (eye under a microscope without a grid), and manual count of camera-captured/printed image. The accuracy and reproducibility of all these methods have recently been evaluated. Among them, manual count of a camera-captured, printed image (CCPI) has appeared to be the most reliable procedure, showing good reproducibility [60]. For this reason, this system of Ki-67 count has been recommended in the 2017 WHO classification of pancreatic NENs [49]. Another possible practical problem in assessing the Ki-67 index in well-differentiated NENs is the immunostaining of non-neoplastic nuclei of the microenvironment cells (e.g., lymphocytes and other inflammatory cells, endothelia, entrapped normal glands) which, particularly in small and crushed biopsies, may not be easily distinguished from tumor cells. To obviate this inconvenience and to improve the inter-observer agreement, the use of a double immunostaining for synaptophysin and Ki-67 has been proposed [61].
The distinction between low-intermediate grade NETs and high-grade NECs is usually straightforward and relies on morphology, which is generally well correlated with the Ki-67 proliferative index. According to the 2010 WHO classification of digestive neoplasms, all cases with a Ki-67 > 20% belong to the G3 category and should be, by definition, called NECs [6]. However, since the publication of this classification, it has become evident that a subset of histologically well-differentiated NENs shows a Ki-67 index greater than 20%. These tumors are associated with a worse prognosis than G2 NETs but still show a better outcome than poorly differentiated NECs [62, 63]. Moreover, well-differentiated NENs with a Ki-67 more than 20% show a poorer response to platinum-based therapy than poorly differentiated NECs, whereas they favorably respond to treatments based on somatostatin analogs, evorolimus, sutinib, and temozolomide, especially when the Ki-67 index is comprised between 20 and 55% [64,65,66]. In the last years, several attempts have been made to better characterize this peculiar category which has been found to share several features with “conventional” NETs such as hormone production, somatostatin receptor 2A expression, and association with endocrine syndromes [67]. In addition, they have been found to lack the typical genetic background of poorly differentiated NEC including the expression and mutations of TP53 and RB1 [62, 67, 68]. Conversely, they can bear mutations in MEN1 and DAXX/ARTX genes, which are observed in well-differentiated NETs [67, 69, 70]. Taken together, these data suggest that the group of NENs showing a Ki-67 index > 20% consists of two different entities. The term NET G3 has been proposed to define well-differentiated NENs with a Ki-67 > 20% and this new category has been included in the 2017 WHO classification of pancreatic NENs [49]. In some cases, the differential diagnosis between NET G3 and NEC can be difficult and immunohistochemistry may be a useful tool. Indeed, NETs G3 generally show nuclear immunoreactivity for Rb, strong cell membrane positivity for somatostatin receptor 2A, diffuse and strong chromogranin A immunoreactivity, and the lack of nuclear expression of p53. In some cases they lose the nuclear expression of DAXX or ATRX proteins (Fig. 3).
Schematic representation of gastroenteropancreatic neuroendocrine neoplasms considering both morphological differentiation and Ki-67 proliferative grade. Well-differentiated neuroendocrine tumors can be separated into three different categories with NET G1 showing a Ki-67 index < 3% and G2 NET with a Ki-67 index between 3 and 20%. In addition, there is a group of well-differentiated NETs showing a Ki67 > 20% (generally comprised between 20 and 55%) which shows a molecular background and an immunohistochemical profile similar to that of G1/G2 NETs. This category is defined NET G3. Poorly differentiated neuroendocrine neoplasms show a poorly differentiated morphology and a Ki-67 proliferative index > 20% and are defined NECs. Immunohistochemistry can be useful for the differential diagnosis between NET G3 and NEC in difficult cases. The immunoprofile is different with the former generally negative for p53, positive for Rb and somatostatin receptor 2 A (SSRT2A) and negative for DAXX/ATRX in about 30% of cases. NECs generally show the opposite immunophenotype
NENs of the Lung and Thymus
The WHO morphological criteria for the identification of the four major histotypes of lung and thymic neuroendocrine neoplasms have been nearly identical for the past 20 years, thus proving their reliability with special reference to surgical samples. In fact, the use of immunohistochemistry to define a specific histotype, once the neuroendocrine nature is proven, is of scarce, if not null, value in the post-surgical setting. A completely different situation concerns the characterization of the histotypes of lung NENs in small biopsies or cytological samples. In fact, the two major morphological parameters, mitotic count and assessment of necrosis, are highly dependent on the availability of tumor tissue to be analyzed, and the more the tissue is scarce, the more the parameters are unreliable. Moreover, sampling methods, both in biopsies and in cytological preparations, induce tissue artifacts (crushing, fragmentation, molding) that might further prevent the correct evaluation of such parameters. By contrast, with special reference to inoperable tumor patients, treatment strategies as well as the prognosis of carcinoids (typical or atypical) are extremely different compared to large/small cell NECs. In this context, pure neuroendocrine markers are of limited value, although a progressive decrease in positivity, with special reference to chromogranin A, is present in association with the progressive loss of differentiation. Thus, a diffuse and intense chromogranin A positivity partly contrasts with a diagnosis of high-grade NEC, whereas a focal dot-like pattern calls into question a diagnosis of a carcinoid. The same holds true, although in the opposite situation, for hASH-1 whose prevalence of expression increases with increased aggressiveness although not as sharply. The pattern of pan-cytokeratin staining might also be of little help, tending to be diffuse cytoplasmic staining in carcinoids and more frequently dot-like in high-grade forms, especially in small cell types.
The most useful marker in this setting is proliferation, as determined by Ki-67 labeling. In contrast with the GEP system, Ki-67 is not mandatory for the characterization of lung NENs. In fact, despite recent proposals that include its evaluation to determine a grading score in lung tumors [71, 72] and a prognostic role for tumors in the thymus [73], its assessment has not been incorporated in the most recent WHO classification and is not indicated for diagnostic purposes in surgical samples. However, the practical role of Ki-67 to segregating low from high-grade forms in the preoperative setting has been proposed in several papers [74, 75] and is supported by recent evidence of a strong correlation of Ki-67 assessed in pre-surgical vs. surgical lung samples [76], although few cases with borderline features can be encountered (Fig. 4). In fact, proliferation markers are the most relevant prognostic indicators in lung NENs, independently from the marker and the method used to determine them [77]. However, in clinical practice, Ki-67 evaluation has been by far the most widely studied and validated both in the lungs and thymus [72, 73] and, although not coded in the WHO classification system as a prognostic determinant to be required in the diagnostic report, its assessment is strongly recommended in clinical practice [78]. Indeed, its relatively high expression (using a cut-off of 10%) further segregates a subgroup of lung carcinoids with distinct pathological features and significantly worse outcome independently from the typical or atypical histotypes, which at least in part, resemble the pancreatic “NET G3” group of neoplasms [79].
Core biopsy sample (a) of a mediastinal mass, 6 cm in size, with associated multiple bilateral lung nodules, showing a well-differentiated morphology with no necrosis and no mitotic figures in the available material (b). The immunoprofiling showed pan-cytokeratin (AE1/AE3)-positive staining with a mixed cytoplasmic and dot-like pattern (c), a diffuse but dot-like chromogranin A-positive staining (d), a moderate Ki-67 proliferation index (up to 25%) (e), focal and weak p53 staining (with a “wild-type” pattern) (f), and strong and intense TTF-1 positivity (g)
Recent advances also indicate that the prevalence of molecular alterations in lung carcinoids vs. high-grade forms is different [80]. Transferring molecular data into immunohistochemical markers, the expression of p53 and retinoblastoma 1 (Rb1) proteins is of potential diagnostic impact, similarly to that proposed for pancreatic neuroendocrine neoplasms [67], although these markers have not been studied in this specific context, yet.
How Will It Behave?—Prognostic and Theranostic Markers
Prognostic and predictive markers in NENs differ from site to site. Since among thoracic NENs there is a much higher frequency of NECs than NETs, whereas the reverse is true for GEP NENs, the therapeutic options have been differently considered in the two sites. For these reasons, the two systems will be treated separately.
Gastroenteropancreatic NENs
Cell sensitivity to somatostatin is mediated through the members of the somatostatin receptors family (SSTRs), composed of at least 5 subtypes (SSTR1, 2, 3, 4, and 5). SSTRs are frequently expressed by GEP NENs, both in NETs and in NECs, and this is the rationale of the OctreoScan, in which the somatostatin analog octreotide is coupled to 111In which allows the identification of NENs by nuclear medicine imaging. In addition, somatostatin analogs are used as anti-secretory drugs in functioning tumors (including patients with carcinoid syndrome) and seem to have a tumoristatic activity in NETs [81]. Somatostatin analogs used in diagnostic and therapeutic settings have the highest affinity for the type 2A and type 5 receptors (SSTR2A and SSTR5), and for this reason, their detection in tumor tissue with immunohistochemistry has been implemented. The availability of a monoclonal anti-SSTR2A antibody has improved the specificity and sensitivity of the immunostaining on formalin-fixed and paraffin-embedded samples [82]. A three-tiered scoring system for the evaluation of SSTR2A immunoreactivity in neuroendocrine tumors has been proposed, taking into consideration both the subcellular localization and the extent of the staining [83]. In a recent paper, the determination of both SSTR2A and SSTR5 with the “Volante score” as well as the HER2 and H score has been demonstrated to be an easily standardizable tool in different laboratories and is highly reproducible irrespective of the method of evaluation used [84]. It is worth noting that an independent prognostic role of SSTR2A immunohistochemistry has been shown in GEP NETs. Indeed, SSTR2A membranous immunoreactivity (Fig. 5) has been reported to be associated with a longer overall and progression-free survival, both in NETs and in NECs [85,86,87].
Somatostatin receptor 2A expression showing membrane immunoreactivity in an ileal well-differentiated neuroendocrine tumor (score 3+ according to Volante et al. [83])
In recent years, the prognostic role of the Ki-67 index in GEP NENs has been clearly demonstrated [88, 89]. The cut-offs proposed by the WHO classifications, useful in separating the G1, G2, and G3 NEN categories (Fig. 6), correlate well with patient outcomes. However, it is worth noting that there is some evidence that Ki67 cut-offs should be refined in relation to tumor type and location. Moreover, it has recently been demonstrated that the best prognostic stratification of patients is obtained using a multiparametric approach, combining the Ki67 index with other clinico-pathological parameters [59].
Cytokeratin 19 (CK19) is an acidic cytokeratin highly expressed in the exocrine component of the human adult pancreas, including duct and centroacinar cells, whereas it is absent in normal islets of Langerhans [90, 91]. Aberrant CK19 expression was found to be an independent prognostic marker in well-differentiated pancreatic NETs [92, 93], although this finding was not confirmed in other studies [94].
CD117, also named c-kit, is a type III tyrosine kinase receptor of the platelet-derived growth factor subfamily. CD117 immunoreactivity was found to be an independent prognostic marker in pancreatic NETs [95, 96]. Overexpression of CD117 in NECs, including pulmonary, GEP, and cutaneous (Merkel cell carcinoma) carcinomas, has been demonstrated and associated with an adverse prognosis [95, 97,98,99,100], although it was not related to an underlying activating mutation of the c-kit gene [101, 102].
Loss of DAXX or ATRX expression, which are mutually exclusive, are due to DAXX and ATRX mutations and have been found in about 40% of pancreatic NETs (PanNETs) [69]. Interestingly, cases lacking DAXX/ATRX immunoreactivity frequently show mutation of the MEN1 gene, too. However, MEN1 mutation is considered an early event in PanNET development, whereas DAXX/ATRX loss is a late event, frequently observed in more aggressive cases of both sporadic and MEN1 tumors. Indeed, DAXX/ATRX-negative NETs are mainly G2 tumors and frequently present in advanced stage [103,104,105]. For this reason, immunohistochemistry for both DAXX and ATRX can be useful to identify a subset of cases with poor prognosis.
The coexistence of microsatellite instability (MSI) and widespread gene methylation is a predictor of a better outcome in patients with gastrointestinal NECs [106]. Since there is a good correlation between MSI and the immunohistochemical loss of mismatch repairs proteins, immunohistochemistry for hMLH1, hMSH2, hMSH6, and hPMS2 may be included in the diagnostic panel to identify a lower risk class among these very aggressive neoplasms.
NENs of the Lung and Thymus
Data from gene expression profiling identified several markers potentially applicable in immunohistochemistry. However, most of them are differentially expressed in the different forms of lung NENs but lose their prognostic value when assessed in comparison to histotyping. Among those, the only biomarker strongly and independently associated to adverse outcomes is OTP protein loss in lung carcinoids [107]. By contrast, immunohistochemical biomarkers of strong prognostic impact in high-grade lung forms as well as in thymic NENs overall are missing.
In terms of the prediction of a response to treatment, thoracic NENs are far behind their non-neuroendocrine lung counterparts. In carcinoids, molecular data have not been translated into phenotypical markers yet, despite the evidence of highly prevalent alterations involving druggable pathways, such as PI3K/AKT/mTOR, or the prognostic value of MEN1 gene mutation in atypical carcinoids [80]. Data on mTOR expression in these tumors remain descriptive in nature [108] and never validated in clinical practice. The role of somatostatin analogs in advanced lung carcinoids has been reinforced by a recent clinical trial assessing their clinical benefit in association with mTOR inhibitors [109]. The immunohistochemical expression of somatostatin receptors is described at a high prevalence in lung NENs, but the real impact on therapeutic strategy has not been defined, although somatostatin receptor type 2A has been recently associated with a response to somatostatin analogs in a series of NENs including a subset of lung primaries [84].
Regarding chemotherapy in high-grade neoplasms, recent data suggest that the molecular signature might influence the responsiveness to specific therapeutic regimens. In fact, in large cell NECs, unaltered Rb1 function is associated with a better response to protocols containing gemcitabine or taxanes (as in non-small cell lung cancer) compared to platinum-etoposide regimens [110]. Moreover, among novel therapeutic targets being developed, the significant impact of Notch signaling pathway deregulation in small cell lung cancer recently opened the way to improving clinical strategies targeting one of the Notch ligands, DLL3, with a specific drug-conjugated antibody, rovalpituzumab, with the efficacy being directly proportional to the immunohistochemical expression of DLL3 [111].
Where Does It Come from?—Site-Specific Markers
NENs are frequently metastatic at clinical presentation and in up to one third of the cases the site of origin of the tumor is unknown [112]. The identification of the primary neoplasm is important, especially in the case of NETs, because therapeutic protocols may vary also according to the site of origin. The identification of the thymic or pulmonary primary site in intra-thoracic NENs may be particularly challenging and should firstly be based on clinical and radiological findings. Indeed, in advanced cases with multiple locations and, sometimes, in locally advanced cases involving the mediastinum, the clinical definition of the primary site might not be straightforward, despite a strong impact on the management of the patient. In NECs, the major clinical problem is represented by cutaneous neoplasms, in which the distinction of Merkel cell carcinoma (MCC) from visceral NEC is crucial for correct management. Imaging techniques, including positron emission tomography, are able to identify the primary NEN in a consistent proportion of cases, but in more than 15% of patients, it remains occult [48]. The pathologist is therefore asked to give clues to the possible primary site, and the use of a correct panel of immunohistochemical markers is a powerful tool to answer this question. The most helpful markers in this setting are represented by transcription factors involved in site-specific tissue development and selectively expressed by normal and neoplastic cells of the adult organism. In addition, cell-specific hormonal products may be used in metastatic deposits to identify the primary site of GEP NENs.
Transcription Factors
Thyroid Transcription Factor-1 (TTF-1)
With regard to the definition of primary lung vs. extra-thoracic location, TTF-1 seems the most specific marker for lung carcinoids to discriminate them from other morphologically well-differentiated neuroendocrine neoplasms, including those of the thymus. Unfortunately, its sensitivity is very limited since TTF-1 expression is detectable in only about one third of cases. Interestingly, peripheral, spindle cell carcinoids seem to express TTF-1 more frequently than central carcinoids [113]. It should be noted that different anti-TTF-1 monoclonal antibodies are available, with variations in the sensitivity and specificity of the immunostaining. In fact, the SPT24 antibody, raised against a 123 amino acid sequence of the N-terminal region of human TTF-1, seems to be more sensitive in detecting lung carcinoids than the 8G7G3/1 antibody directed against the full length recombinant protein [113]. In the context of NEN, one should also bear in mind that TTF-1 expression is nearly always present in medullary carcinoid of the thyroid. In this setting, immunostaining for calcitonin and CEA helps to define the diagnosis [43]. In contrast with low- to intermediate-grade forms (typical and atypical carcinoids), the immunohistochemical definition of a primary thoracic location in a morphologically poorly differentiated and highly proliferative NEC is unreliable. TTF-1 is expressed in a high proportion of extra-pulmonary high-grade neuroendocrine carcinomas [114], whereas high-grade neuroendocrine carcinomas of the lung, in particular of the small cell type, might express a relatively high prevalence of extra-pulmonary-specific markers such as PAX8 [115]. However, in the differential diagnosis between a MCC and a cutaneous metastasis of a visceral poorly differentiated NEC, the use of an immunohistochemical panel including TTF-1, CK20, and, more recently, MCC polyomavirus (MCPyV) can reliably solve the problem. Indeed, immunoreactivity for CK20 and MCPyV, in the absence of TTF-1 immunostaining, is diagnostic for MCC [116, 117].
Paired Box Gene 8 (PAX8)
PAX8, a member of the paired box transcription factors family, is involved in thyroid, kidney, and müllerian tract development and is expressed in carcinomas arising in these organs [118,119,120]. Among neuroendocrine neoplasms, PAX8 has been reported to be a marker of thymic and pancreatic neoplasms [121, 122]. Among thoracic NENs, although sensitivity and specificity are not 100%, in low to intermediate forms, a TTF-1 +/PAX-8 − profile is more suggestive of primary lung tumors, whereas the opposite profile is more closely linked to thymic neuroendocrine neoplasms [121, 123]. In the field of GEP NENs, besides pancreatic tumors, it has been reported that also duodenal and rectal NETs express PAX8, whereas ileal NETs are not immunoreactive, making this marker useful in the differential diagnosis of metastatic localizations [122, 124]. However, it is worth knowing that commercially available anti-PAX8 polyclonal antibodies cross-react with other members of the PAX family, including PAX3, PAX5, and PAX6. As PAX8 mRNA is expressed at low levels at this site, it is conceivable that PAX8-immunostaining is due to cross-reactivity with PAX6, which is highly expressed in pancreatic islets. In fact, a monoclonal antibody, directed against a restricted epitope of PAX8, gives strong immunostaining in renal cells and ovarian cancers, whereas it does not stain neuroendocrine pancreatic cells [125, 126].
Orthopedia Homeobox Protein
Orthopedia homeobox protein (OTP) is a helix-turn-helix transcription factor essential for the development of specific subsets of diencephalic dopaminergic neurons. Immunohistochemical analysis using a specific rabbit polyclonal antibody has shown OTP to be selectively expressed by lung carcinoids compared to NENs of other locations, with a sensitivity of 100% for the typical carcinoid histotype [127, 128]. Interestingly, OTP was expressed in all TTF1-positive carcinoid tumors but not vice versa. Moreover, while TTF1-positive tumors tend to be associated with spindle cell morphology and peripheral location, such associations are not evident in OTP expressing tumors [127].
Caudal Type Homeobox 2 (CDX2)
CDX2 is a homeobox domain-containing transcription factor, which is involved in gut development and the maintenance of the intestinal phenotype in epithelial cells. It is expressed in the epithelium of the small and large intestines [129, 130]. CDX2 is also expressed by pancreatic centroacinar, intercalated, and intralobular duct cells and by scattered ductal cells [130]. CDX2 immunostaining is used in diagnostic pathology to assess the intestinal differentiation of adenocarcinomas because it is expressed in the vast majority of intestinal and appendiceal adenocarcinomas, in intestinal type adenocarcinomas of the stomach, esophagus, pancreas, gallbladder and extra-hepatic biliary tract, ovary, uterine cervix, urinary bladder, and nasal cavity [131,132,133]. It is worth noticing that aberrant expression of CDX2 has also been reported in carcinomas of the lung, in columnar cell variant of papillary thyroid carcinoma, and in hepatocellular carcinoma [134,135,136]. The mouse monoclonal antibody CDX2-88 is highly sensitive and fairly specific for a midgut origin of well-differentiated NETs [137,138,139]. A strong and diffuse CDX2 immunostaining is present in more than 90% jejunoileal and appendiceal NETs. By contrast, CDX2 immunoreactivity was detected only in about 30% of duodenal and rectal primaries, and in about 15% of gastric and pancreatic tumors, with faint and patchy staining. As few as 3% of lung carcinoids showed CDX2 expression [48]. The use of the rabbit monoclonal antibody EPR2764Y seems to further improve the sensitivity and the specificity of the immunostaining for midgut NETs to 100 and 87%, respectively [140].
Insulin Gene Enhancer Binding Protein Isl-1 (Islet 1)
Islet 1 is a homeodomain-containing transcription factor important in the embryonal development of neuroendocrine and neural cells and is highly expressed in islet cells [141]. It is a good marker of pancreatic origin in well-differentiated NETs and has superior sensitivity to PAX8, with which it also shares the immunostaining of ileal and rectal NETs [48].
Pancreatic and Duodenal Homeobox 1 (PDX1)
PDX1 is involved in the development of the pancreas and of the duodenum and in the adult, it is expressed in pancreatic islet cells, being absent in acinar and ductal structures [142]. Among well-differentiated NETs, PDX1 expression is neither a specific nor a sensitive marker for primary pancreatic neoplasms. However, as it has been detected in a subset of pancreatic, duodenal, and gastric NETs, whereas it is absent in ileal and pulmonary carcinoids, the main benefit of positive immunostaining for PDX1 seems to be the exclusion of a primary ileal or pulmonary neoplasm [143].
Amine and Peptide Hormones
Hormonal production of different neuroendocrine cell types of normal gut and pancreas is specifically site related. However, this is not completely true for NENs arising in the GEP tract, in which ectopic hormone secretion is not uncommon. However, there are some types of NETs, such as ileal and rectal tumors, in which the hormonal secretion may be useful in identifying the primary site. Commercially available antibodies which recognize a wide variety of amine and peptide hormones include, among others, serotonin, substance P, calcitonin, gastrin, pancreatic hormones (insulin, glucagon, somatostatin, pancreatic polypeptide), and intestinal hormone peptides (gastric inhibitory peptide, motilin, secretin, cholecystokinin, vasoactive intestinal polypeptide, glicentin, peptide YY). The use of these markers can be of help in the workup of selected cases.
The specific identification of the hormonal product in gastric neuroendocrine neoplasms of the oxyntic mucosa is difficult because commercial anti-histamine antibodies are not available for diagnostic purposes. Thus, ECL-cell NETs can be diagnosed after excluding other hormone/amines expression in presence of VMAT2 immunoreactivity. Occasional gastric NETs can express serotonin, which, however, is more frequently expressed in small intestine and pancreatic NETs. A relatively specific marker of gastric neoplasms of the oxyntic mucosa is ghrelin, although it has been also identified in a subgroup of pancreatic NETs and pre-sacral (tailgut cyst-associated) carcinoids [144,145,146,147]. It is worth noting that gastric NETs of the antral mucosa do not show a specific hormonal profile; the most frequently expressed hormones in this site are somatostatin, gastrin, or, more rarely, serotonin [148].
Duodenal neoplasms frequently show a definite hormonal profile, with NETs arising in the first portion of the duodenum expressing gastrin, whereas those of the ampullary region are immunoreactive for somatostatin and are characterized by a typical acinar/pseudoglandular architecture with frequent psammoma bodies [149].
The use of antibodies directed against pancreatic hormones can suggest a pancreatic origin of a metastatic NET, although somatostatin can also be positive in duodenal [149] and rectal NETs. It is worth noting that rare cases of duodenal NETs strongly positive for insulin and showing the full blown insulinoma syndrome have been described [150].
The use of hormonal markers is more useful and specific to define the immunophenotype of EC-cell NETs of the midgut (lower jejunal, ileal, and right colonic). These neoplasms express serotonin and substance P, which, together with the expression of VMAT1 and CDX2, strongly support a midgut origin of an occult metastatic NET (Fig. 7). By contrast, rectal L-cell NETs, which show a characteristic trabecular pattern of growth, have a specific immunophenotype including the expression of glicentin, PP, PYY, and prostatic acidic phosphatase (Fig. 8) [151, 152]. It is worth recalling that rare cases of rectal NETs are negative for glicentin, PP, or PYY and express serotonin. This different immunophenotyped show a correlation with prognosis, with serotonin-positive cases being the most aggressive [153].
Rectal neuroendocrine L-cell tumor showing the typical trabecular/gyriform architectural pattern (a). Tumor cells are positive for glicentin which is also positive in normal L-cells present in the rectal crypts (arrows) (b). In addition to glicentin, tumor cells are positive for PP (c) and prostatic acid phosphatase (d)
Is it Inherited?
Both digestive and lung NENs can develop either as sporadic or, more rarely, as inherited proliferations being part of several inherited tumor syndromes. In some instances, the pathologist is asked to identify potential inherited cases, because a digestive or broncopulmonary neuroendocrine tumor may represent the first clinical manifestation of a familial tumor syndrome involving endocrine and neuroendocrine organs. The suspect of inherited NENs generally starts from specific morphological features (i.e., multiple pancreatic microadenomas) and can be sometime confirmed using immunohistochemical markers. However, it is worth noting that immunohistochemical markers alone are not diagnostic and they need to be integrated in the morphological and clinical context. Indeed, the lack of menin expression in tumor tissue, which is related to MEN1 gene mutation, can also be observed in sporadic pancreatic and gastric NETs and in lung carcinoids [154, 155]. For this reason, the immunohistochemical loss of menin expression in a NET should be carefully evaluated in the morphological background.
MEN4 is an autosomal dominant tumor syndrome caused by germline mutation of CDKN1B gene which results in an endocrine syndrome including parathyroid, pituitary, and pancreatic NETs [156]. CDKN1B encodes p27kip1, a cyclin-dependent kinase inhibitor, which controls the cell cycle. Mutation in CDKN1B results in low nuclear and weak cytoplasmic expression of p27kip1. Conversely, strong p27KIP1nuclear staining has been described in tumor cells of sporadic NETs [157].
PanNETs can also arise in the context of the von Hippel-Lindau (VHL) syndrome which is caused by germline mutations of the VHL gene [158]. Although PanNETs belonging to the VHL syndrome have been firstly described to be composed of clear cells [159], further studies have demonstrated that clear cell PanNETs can also be sporadic or associated with the MEN1 syndrome [160, 161]. Clear cell duodenal and PanNETs associated with the VHL syndrome seem to be positive for inhibin and CAIX, so this specific immunophenotype, if associated with a clear cell appearance, should alert the possibility of a VHL syndrome, especially considering that inhibin expression in sporadic digestive NETs is exceptional [162]. However, as a general rule, every case showing multiple microadenomas should alert for a possible inherited tumor syndrome and the suspect should be specified in the pathology report.
A PanNET showing absence of SDHB immunoreactivity has been described in a patient with SDHD mutation, who was also affected by oligodendroglioma and multiple paragangliomas [163]. This recent report suggests that PanNET can expand the spectrum of non-paraganglionic tumors with SDH mutation. This finding might have potential implications for the surveillance of patients with a germline SDHD mutation.
Concluding Remarks
Immunohistochemistry is a cornerstone in the diagnostic and prognostic classification of thoracic and GEP NENs. Both the pathologists and the oncologists involved in the management of these neoplasms should be aware of the meaning of the different immunohistochemical markers used in diagnostic practice. The minimum panel for the correct classification of NENs at these sites includes the general neuroendocrine markers (synaptophysin and chromogranin A) and Ki-67, the latter being indispensable in the categorization of GEP NENs and highly advisable, at least in pre-operatory small biopsies, in thoracic NENs. Additional markers, useful in predicting prognosis and response to therapy, vary for different sites, as well as site-specific markers, which can give clues to an unknown primary when well-differentiated NENs firstly present with a metastatic localization (Fig. 9). Only an integrated and critical approach, primarily based on the careful interpretation of the clinico-radiological and histological data, may assist the pathologist in the selection of a tailored panel of immunohistochemical markers, which will be the basis for an effective personalized therapeutic approach.
References
Oberndorfer S (1907) Karzinoide tumoren des Dünndarms. Frankf Z Pathol 1:425–432.
Masson P (1924) Appendicite neurogéne and carcinoides. Ann Anat Pathol 1:3–59.
Capella C, Heitz PU, Höfler H, Solcia E, Klöppel G (1995) Revised classification of neuroendocrine tumors of the lung, pancreas and gut. Virchows Arch 425:547–560.
Chetty R (2008) Requiem for the term “carcinoid tumour” in the gastrointestinal tract? Can J Gastroenterol 22:357–358.
Travis WD, Brambilla E, Burke AP, Marx A, Nicholson AG (2015) WHO classification of tumours of the lung, pleura, thymus and heart. IARC Press, Lyon.
Rindi G, Arnold R, Bosman FT, Capella C, Klimstra DS, Klöppel G, Komminoth P, Solcia E (2010) Nomenclature and classification of neuroendocrine neoplasms of the digestive system. In: Bosman FT, Carneiro F, Hruban RH, Theise ND (eds) WHO classification of tumours of the digestive system. IARC Press, Lyon, pp 13–14
Yao JC, Hassan M, Phan A, et al (2008) One hundred years after “carcinoid”: epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol 26:3063–3072.
Lloyd RV, Wilson BS (1983) Specific endocrine tissue marker defined by a monoclonal antibody. Science 222:628–630.
Taupenot L, Harper KL, O’Connor DT (2003) The chromogranin–secretogranin family. N Engl J Med 348:1134–1149.
Weiler R, Feichtinger H, Schmid KW, et al (1987) Chromogranin A and B and secretogranin II in bronchial and intestinal carcinoids. Virchows Arch A Pathol Anat Histopathol 412:103–109.
Fahrenkamp AG, Wibbeke C, Winde G, et al (1995) Immunohistochemical distribution of chromogranins A and B and secretogranin II in neuroendocrine tumours of the gastrointestinal tract. Virchows Arch 426:361–367.
Gould VE, Lee I, Wiedenmann B, Moll R, Chejfec G, Franke WW (1986) Synaptophysin: a novel marker for neurons, certain neuroendocrine cells, and their neoplasms. Hum Pathol 17:979–983.
Komminoth P, Roth J, Schröder S, Saremaslani P, Heitz PU (1995) Overlapping expression of immunohistochemical markers and synaptophysin mRNA in pheochromocytomas and adrenocortical carcinomas. Implications for the differential diagnosis of adrenal gland tumors. Lab Invest 72:424–431.
Portela-Gomes GM, Lukinius A, Grimelius L (2000) Synaptic vesicle protein 2, a new neuroendocrine cell marker. Am J Pathol 157:1299–1309.
Jakobsen AM, Andersson P, Saglik G, et al (2001) Differential expression of vesicular monoamine transporter (VMAT) 1 and 2 in gastrointestinal endocrine tumours. J Pathol 195:463–472.
Graff L, Castrop F, Bauer M, Höfler H, Gratzl M (2001) Expression of vesicular monoamine transporters, synaptosomal-associated protein 25 and syntaxin1: a signature of human small cell lung carcinoma. Cancer Res 61:2138–2144.
Uccella S, Cerutti R, Vigetti D, et al (2006) Histidine decarboxylase, DOPA decarboxylase, and vesicular monoamine transporter 2 expression in neuroendocrine tumors: immunohistochemical study and gene expression analysis. J Histochem Cytochem 54:863–867.
Schmechel DE (1985) Gamma-subunit of the glycolytic enzyme enolase: nonspecific or neuron specific? Lab Invest 52:239–242.
Rode J, Dhillon AP, Doran JF, Jackson P, Thompson RJ (1985) PGP 9.5, a new marker for human neuroendocrine tumours. Histopathology 9:147–158.
Lauweryns JM1, Van Ranst L (1988) Protein gene product 9.5 expression in the lungs of humans and other mammals. Immunocytochemical detection in neuroepithelial bodies, neuroendocrine cells and nerves. Neurosci Lett 85:311–316.
Tezel E, Hibi K, Nagasaka T, Nakao A (2000) PGP9.5 as a prognostic factor in pancreatic cancer. Clin Cancer Res 6:4764–4767.
Gunia S, Erbersdobler A, Koch S, Otto W, Staibano S, D'Alterio C, Brookman-May S (2013) Protein gene product 9.5 is diagnostically helpful in delineating high-grade renal cell cancer involving the renal medullary/sinus region from invasive urothelial cell carcinoma of the renal pelvis. Hum Pathol 44:712–717.
Otsuki T1, Yata K, Takata-Tomokuni A, et al (2004) Expression of protein gene product 9.5 (PGP9.5)/ubiquitin-C-terminal hydrolase 1 (UCHL-1) in human myeloma cells. Br J Haematol 127:292–298.
Campbell LK, Thomas JR, Lamps LW, Smoller BR, Folpe AL (2003) Protein gene product 9.5 (PGP 9.5) is not a specific marker of neural and nerve sheath tumors: an immunohistochemical study of 95 mesenchymal neoplasms. Mod Pathol 16:963–969.
Lauweryns JM1, Van Ranst L (1988) Immunocytochemical localization of aromatic L-amino acid decarboxylase in human, rat, and mouse bronchopulmonary and gastrointestinal endocrine cells. J Histochem Cytochem 36:1181–1186.
Lloyd RV, Sisson JC, Shapiro B, Verhofstad AA (1986) Immunohistochemical localization of epinephrine, norepinephrine, catecholamine-synthesizing enzymes, and chromogranin in neuroendocrine cells and tumors. Am J Pathol 125:45–54.
Scopsi L, Gullo M, Rilke F, Martin S, Steiner DF (1995) Proprotein convertases (PC1/PC3 and PC2) in normal and neoplastic human tissues: their use as markers of neuroendocrine differentiation. J Clin Endocrinol Metab 80:294–301.
Shipley WR, Hammer RD, Lennington WJ, Macon WR (1997) Paraffin immunohistochemical detection of CD56, a useful marker for neural cell adhesion molecule (NCAM), in normal and neoplastic fixed tissues. Applied Immunohistochemistry 5:87–93.
Jin L, Hemperly JJ, Lloyd RV (1991) Expression of neural cell adhesion molecule in normal and neoplastic human neuroendocrine tissues. Am J Pathol 138:961–969.
Chu PG, Arber DA, Weiss LM (2003) Expression of T/NK-cell and plasma cell antigens in nonhematopoietic epithelioid neoplasms. An immunohistochemical study of 447 cases. Am J Clin Pathol 120:64–70.
Bösmüller HC1, Wagner P, Pham DL, et al (2017) CD56 (Neural Cell Adhesion Molecule) expression in ovarian carcinomas: association with high-grade and advanced stage but not with neuroendocrine differentiation. Int J Gynecol Cancer 27:239–245.
Vasei M, Moch H, Mousavi A, Kajbafzadeh AM, Sauter G (2008) Immunohistochemical profiling of Wilms tumor: a tissue microarray study. Appl Immunohistochem Mol Morphol 16:128–134.
Wachowiak RT, Metzger R, Quaas A, et al (2008) Universal expression of cell adhesion molecule NCAM in neuroblastoma in contrast to L1: implications for different roles in tumor biology of neuroblastoma? Pediatr Surg Int 24:1361–1364.
Van Camp B, Durie BGM, Spier C (1990) Plasma cells in multiple myeloma express a natural killer cell associated antigen: CD56 (NKH-1; Leu-19). Blood 76:377–382.
McGarry RC, Helfand SL, Quarles RH, et al (1983) Recognition of the myelin associated glycoprotein by the monoclonal antibody HNK-1. Nature 306:376–378.
Arber DA, Weirs LM (1995) CD57: a review. Appl Immunohistochem 3:137–152.
Tischler AS, Mobtaker H, Mann K, et al (1986) Anti-lymphocyte antibody Leu 7 (HNK-1) recognizes a constituent of NE granule matrix. J Histochem Cytochem 34:1213–1216.
Ball DW, Azzoli CG, Baylin SB, et al (1993) Identification of a human achaete scute homolog highly expressed in neuroendocrine tumors. Proc Natl Acad Sci USA 90:5648–5652.
Ball DW (2004) Achaete-scute homolog-1 and Notch in lung neuroendocrine development and cancer. Cancer Lett 204:159–169.
La Rosa S, Marando A, Gatti G, et al (2013) Achaete-scute homolog 1 as a marker of poorly differentiated neuroendocrine carcinomas of different sites: a validation study using immunohistochemistry and quantitative real-time polymerase chain reaction on 335 cases. Hum Pathol 44:1391–1399.
Jiang SX, Kameya T, Asamura H, et al (2004) hASH1expression is closely correlated with endocrine phenotype and differentiation extent in pulmonary neuroendocrine tumors. Mod Pathol 17:222–229.
Altree-Tacha D, Tyrrell J, Li F (2017) mASH1 is highly specific for neuroendocrine carcinomas: an immunohistochemical evaluation on normal and various neoplastic tissues. Arch Pathol Lab Med 141:288–292.
Duan K, Mete O (2016) Algorithmic approach to neuroendocrine tumors in targeted biopsies: Practical applications of immunohistochemical markers. Cancer 124:871–884.
Bahrami A, Truong LD, Ro JY (2008) Undifferentiated tumor: true identity by immunohistochemistry. Arch Pathol Lab Med 132:326–348.
Bahrami A, Gown AM, Baird GS, Hicks MJ, Folpe AL (2008) Aberrant expression of epithelial and neuroendocrine markers in alveolar rhabdomyosarcoma: a potentially serious diagnostic pitfall. Mod Pathol 21:795–806.
Zhang C, Schmidt LA, Hatanaka K, Thomas D, Lagstein A, Myers JL (2014) Evaluation of napsin A, TTF-1, p63, p40, and CK5/6 immunohistochemical stains in pulmonary neuroendocrine tumors. Am J Clin Pathol 142:320–324.
Lyda MH, Weiss LM (2000) Immunoreactivity for epithelial and neuroendocrine antibodies are useful in the differential diagnosis of lung carcinomas. Hum Pathol 31:980–987.
Bellizzi AM (2013) Assigning site of origin in metastatic neuroendocrine neoplasms: a clinically significant application of diagnostic immunohistochemistry.Adv Anat Pathol 20:285–314.
Klöppel G, Couvelard A, Hruban RH, Klimstra DS, Komminoth P, Osamura RY, Perren A, Rindi G (2017) Neoplasms of the neuroendocrine pancreas. Introduction. In: Lloyd RV, Osamura RY, Klöppel G, Rosai J (eds) WHO classification of tumours of endocrine organs. IARC Press, Lyon, pp 211–214
El-Naggar AK, Chan JKC, Grandis JR, Takata T, Slootweg PJ (2017) WHO classification of head and neck tumours. IARC Press, Lyon
Rindi G, Petrone G, Inzani F (2014) The 2010 WHO classification of digestive neuroendocrine neoplasms: a critical appraisal four years after its introduction. Endocr Pathol 25:186–192.
Voss sM, Riley MP, lokhandwala PM, Wang M, Yang Z (2015) Mitotic count by phosphohistone H3 immunohistochemical staining predicts survival and improves interobserver reproducibility in well-differentiated neuroendocrine tumors of the pancreas. Am J Surg Pathol 39:13–24.
Ozturk Sari S, Taskin OC, Gundogdu G, et al (2016) The impact of phosphohistone-H3-assisted mitotic count and Ki67 score in the determination of tumor grade and prediction of distant metastasis in well-differentiated pancreatic neuroendocrine tumors. Endocr Pathol 27:162–170.
Tsuta K, Liu DC, Kalhor N, Wistuba II, Moran CA (2011) Using the mitosis-specific marker anti-phosphohistone H3 to assess mitosis in pulmonary neuroendocrine carcinomas. Am J Clin Pathol 136:252–259.
Gerdes J, Schwab U, Lemke H, Stein H (1983) Production of a mouse monoclonal antibody reactive with a human nuclear antigen associated with cell proliferation. Int J Cancer 31:13–20.
Scholzen T, Gerdes J (2000) The Ki-67 protein: from the known and the unknown. J Cell Physiol 182:311–322.
Gerdes J, Lemke H, Baisch H, Wacker H-H, Schwab U, Stein H (1984) Cell cycle analysis of a cell proliferation-associated human nuclear antigen defined by the monoclonal antibody Ki-67. J Immunol 133:1710–1715.
Cattoretti G, Becker MH, Key G, Duchrow M, Schlüter C, Galle J, Gerdes J (1992) Monoclonal antibodies against recombinant parts of the Ki-67 antigen (MIB 1 and MIB 3) detect proliferating cells in microwave-processed formalin-fixed paraffin sections. J Pathol 168:357–363.
Klöppel G, La Rosa S (2017) Ki67 labeling index: assessment and prognostic role in gastroenteropancreatic neuroendocrine neoplasms. Virchows Arch Nov 13. [Epub ahead of print] DOI: https://doi.org/10.1007/s00428-017-2258-0
Reid MD, Bagci P, Ohike N, et al (2015) Calculation of the Ki67 index in pancreatic neuroendocrine tumors: a comparative analysis of four counting methodologies. Mod Pathol 28:686–694.
Matsukuma K, Olson KA, Gui D, Gandour-Edwards R, Li Y, Beckett L (2017) Synaptophysin-Ki67 double stain: a novel technique that improves interobserver agreement in the grading of well-differentiated gastrointestinal neuroendocrine tumors. Mod Pathol 30:620–629.
Basturk O, Yang Z, Tang LH et al (2015) The high-grade (WHO G3) Pancreatic neuroendocrine tumor category is morphologically and biologically heterogenous and includes both well differentiated and poorly differentiated neoplasms. Am J Surg Pathol 39: 683–690.
Milione M, Maisonneuve P, Spada F, et al (2017) The clinicopathologic heterogeneity of grade 3 gastroenteropancreatic neuroendocrine neoplasms: morphological differentiation and proliferation identify different prognostic categories. Neuroendocrinology 104:85–93.
Vélayoudom-Céphise FL, Duvillard P, Foucan L et al (2013) Are G3 ENETS neuroendocrine neoplasms heterogeneous? Endocr Relat Cancer 20: 649–657.
Heetfeld M, Chougnet CN, Olsen IH, et al (2015) Characteristics and treatment of patients with G3 gastroenteropancreatic neuroendocrine neoplasms. Endocr Relat Cancer 22:657–664.
Sorbye H, Welin S, Langer SW et al (2013) Predictive and prognostic factors for treatment and survival in 305 patients with advanced gastrointestinal neuroendocrine carcinoma (WHO G3): the NORDIC NEC study. Ann Oncol 24: 152–160.
Konukiewitz B, Schlitter AM, Jesinghaus M, et al (2017) Somatostatin receptor expression related to TP53 and RB1 alterations in pancreatic and extrapancreatic neuroendocrine neoplasms with a Ki67-index above 20. Mod Pathol 30:587–598.
Yachida S, Vakiani E, White CM, et al (2012) Small cell and large cell neuroendocrine carcinomas of the pancreas are genetically similar and distinct from well-differentiated pancreatic neuroendocrine tumors. Am J Surg Pathol 36:173–184.
Jiao Y, Shi C, Edil B H, de Wilde R F et al (2011) DAXX/ATRX, MEN1, and mTOR pathway genes are frequently altered in pancreatic neuroendocrine tumors. Science 331:1199–1203.
Scarpa A, Chang DK, Nones K, et al (2017) Whole-genome landscape of pancreatic neuroendocrine tumours. Nature 543:65–71.
Rindi G, Klersy C, Inzani F, et al (2013) Grading the neuroendocrine tumors of the lung: an evidence-based proposal. Endocr Relat Cancer 21:1–16.
Pelosi G, Rindi G, Travis WD, Papotti M (2014) Ki-67 antigen in lung neuroendocrine tumors: unraveling a role in clinical practice. J Thorac Oncol 9:273–284
Cardillo G, Rea F, Lucchi M, et al (2012) Primary neuroendocrine tumors of the thymus: a multicenter experience of 35 patients. Ann Thorac Surg 94:241–245
Lin O, Olgac S, Green I, Zakowski MF, Klimstra DS (2003) Immunohistochemical staining of cytologic smears with MIB-1 helps distinguish low-grade from high-grade neuroendocrine neoplasms. Am J Clin Pathol 120:209–216.
Pelosi G, Rodriguez J, Viale G, Rosai J (2005) Typical and atypical pulmonary carcinoid tumor overdiagnosed as small-cell carcinoma on biopsy specimens: a major pitfall in the management of lung cancer patients. Am J Surg Pathol 29:179–187.
Fabbri A, Cossa M, Sonzogni A, et al (2017) Ki-67 labeling index of neuroendocrine tumors of the lung has a high level of correspondence between biopsy samples and surgical specimens when strict counting guidelines are applied. Virchows Arch 470:153–164.
Neubauer E, Wirtz RM, Kaemmerer D, Athelogou M, Schmidt L, Sänger J, Lupp A (2016) Comparative evaluation of three proliferation markers, Ki-67, TOP2A, and RacGAP1, in bronchopulmonary neuroendocrine neoplasms: issues and prospects. Oncotarget 7:41959–41973.
Caplin ME, Baudin E, Ferolla P, et al (2015) Pulmonary neuroendocrine (carcinoid) tumors: European Neuroendocrine Tumor Society expert consensus and recommendations for best practice for typical and atypical pulmonary carcinoids. Ann Oncol 26:1604–1620.
Marchiò C, Gatti G, Massa F, et al (2017) Distinctive pathological and clinical features of lung carcinoids with high proliferation index. Virchows Arch 471:713–720.
Simbolo M, Mafficini A, Sikora KO, et al (2017) Lung neuroendocrine tumours: deep sequencing of the four World Health Organization histotypes reveals chromatin-remodelling genes as major players and a prognostic role for TERT, RB1, MEN1 and KMT2D. J Pathol 241:488–500.
Rinke A, Muller HH, Schade-Brittinger C, et al (2009) Placebo controlled, double-blind, prospective, randomized study on the effect of octreotide LAR in the control of tumor growth in patients with metastatic neuroendocrine midgut tumors: a report from the PROMID Study Group. J Clin Oncol 27:4656–4663.
Korner M, Waser B, Schonbrunn A, et al (2012) Somatostatin receptor subtype 2A immunohistochemistry using a new monoclonal antibody selects tumors suitable for in vivo somatostatin receptor targeting. Am J Surg Pathol 36:242–252.
Volante M, Brizzi MP, Faggiano A, et al (2007) Somatostatin receptor type 2A immunohistochemistry in neuroendocrine tumors: a proposal of scoring system correlated with somatostatin receptor scintigraphy. Mod Pathol 20:1172–1182.
Kasajima A, Papotti M, Ito W, et al (2017) High interlaboratory and interobserver agreement of somatostatin receptor immunohistochemical determination and correlation with response to somatostatin analogs. Hum Pathol Nov 24. doi: https://doi.org/10.1016/j.humpath.2017.11.008 [Epub ahead of print]
Kaemmerer D, Specht E, Sänger J, Wirtz RM, Sayeg M, Schulz S, Lupp A (2015) Somatostatin receptors in bronchopulmonary neuroendocrine neoplasms: new diagnostic, prognostic, and therapeutic markers. J Clin Endocrinol Metab 100:831–840.
Qian ZR, Li T, Ter-Minassian M, et al (2016) Association between somatostatin receptor expression and clinical outcomes in neuroendocrine tumors. Pancreas 45:1386–1393.
Brunner P, Jörg AC, Glatz K, et al (2017) The prognostic and predictive value of sstr2-immunohistochemistry and sstr2-targeted imaging in neuroendocrine tumors. Eur J Nucl Med Mol Imaging 44:468–475.
Norlen O, Stalberg P, Oberg K, Eriksson J, Hedberg J, Hessman O, Janson ET, Hellman P, Akerstrom G (2012) Long-term results of surgery for small intestinal neuroendocrine tumors at a tertiary referral center World J Surg 36:1419–1431.
Rosentraeger MJ, Garbrecht N, Anlauf M, Raffel A, Knoefel WT, Wiedenmann B, Klöppel G (2016) Syndromic versus non-syndromic sporadic gastrin-producing neuroendocrine tumors of the duodenum: comparison of pathological features and biological behavior Virchows Arch 468:277–287.
Real FX, Vila MR, Skoudy A, Ramaekers FC, Corominas JM (1993) Intermediate filaments as differentiation markers of exocrine pancreas. II. Expression of cytokeratins of complex and stratified epithelia in normal pancreas and in pancreas cancer. Int J Cancer 54:720–727.
Bouwens L (1998) Cytokeratins and cell differentiation in the pancreas. J Pathol 184:234–239.
Deshpande V, Fernandez-del Castillo C, Muzikansky A, Deshpande A, Zukerberg L, Warshaw AL, Lauwers GY (2004) Cytokeratin 19 is a powerful predictor of survival in pancreatic endocrine tumors. Am J Surg Pathol 28:1145–1153.
Schmitt AM, Anlauf M, Rousson V, et al (2007) WHO 2004 criteria and CK19 are reliable prognostic markers in pancreatic endocrine tumors. Am J Surg Pathol 31:1677–1682.
La Rosa S, Rigoli E, Uccella S, Novario R, Capella C (2007) Prognostic and biological significance of cytokeratin 19 in pancreatic endocrine tumours. Histopathology 50:597–606.
Zhang L, Smyrk TC, Oliveira AM, Lohse CM, Zhang S, Johnson MR, Lloyd RV (2009) KIT is an independent prognostic marker for pancreatic endocrine tumors: A finding derived from analysis of islet cell differentiation markers. Am J Surg Pathol 33: 1562–1569.
Han Xl, Zhao J, Ji Y, Xu X, Lou W (2013) Expression of CK19 and KIT in resectable pancreatic neuroendocrine tumors. Tumour Biol 34:2881–2889.
Ferrari L, Della Torre S, Collini P, et al (2006) Kit protein (CD117) and proliferation index (Ki-67) evaluation in well and poorly differentiated neuroendocrine tumors. Tumori 92:531–535.
Araki K, Ishii G, Yokose T, et al (2003) Frequent overexpression of the c-kit protein in large cell neuroendocrine carcinoma of the lung. Lung Cancer 40:173–180.
Naeem M, Dahiya M, Clark J, et al (2003) Analysis of c-kit protein expression in small-cell lung carcinoma and its implication for prognosis. Human Pathol 33:1182–1187.
La Rosa S, Marando A, Furlan D, Sahnane N, Capella C (2012) Colorectal poorly differentiated neuroendocrine carcinomas and mixed adenoneuroendocrine carcinomas: Insights into the diagnostic immunophenotype, assessment of methylation profile, and search for prognostic markers. Am J Surg Pathol 36:601–611.
Ishikubo T, Akagi K, Kurosumi M, Yamaguchi K, Fujimoto T, Sakamoto H, Tanaka Y, Ochiai A (2006) Immunohistochemical and mutational analysis of c-kit in gastrointestinal neuroendocrine cell carcinoma. Jpn J Clin Oncol 36:494–498.
Gross DJ, Munter G, Bitan M, et al (2006) The role of imatinib mesylate (Glivec) for treatment of patients with malignant endocrine tumors positive for c-kit or PDGF-R. Endocr Relat Cancer 13:535–540.
Marinoni I, Kurrer AS, Vassella E, Dettmer M et al (2014) Loss of DAXX and ATRX are associated with chromosome instability and reduced survival of patients with pancreatic neuroendocrine tumors. Gastroenterology 146: 453-460e5.
de Wilde RF, Heaphy CM, Maitra A, et al (2012) Loss of ATRX or DAXX expression and concomitant acquisition of the alternative lengthening of telomeres phenotype are late events in a small subset of MEN-1 syndrome pancreatic neuroendocrine tumors. Mod Pathol 25:1033–1039.
Singhi AD, Liu TC, Roncaioli JL, et al (2017) Alternative lengthening of telomeres and loss of DAXX/ATRX expression predicts metastatic disease and poor survival in patients with pancreatic neuroendocrine tumors. Clin Cancer Res 23:600–609.
Sahnane N, Furlan D, Monti M, et al (2015) Microsatellite unstable gastrointestinal neuroendocrine carcinomas: A new clinicopathologic entity. Endocr Relat Cancer 22:35–45.
Swarts DR, Henfling ME, Van Neste L, et al (2013) CD44 and OTP are strong prognostic markers for pulmonary carcinoids. Clin Cancer Res 19:2197–2207.
Righi L, Volante M, Rapa I, Tavaglione V, Inzani F, Pelosi G, Papotti M (2010) Mammalian target of rapamycin signaling activation patterns in neuroendocrine tumors of the lung. Endocr Relat Cancer 17:977–987.
Ferolla P, Brizzi MP, Meyer T, et al (2017) Efficacy and safety of long-acting pasireotide or everolimus alone or in combination in patients with advanced carcinoids of the lung and thymus (LUNA): an open-label, multicentre, randomised, phase 2 trial. Lancet Oncol 18:1652–1664.
Derks JL, Leblay N, Thunnissen E, et al (2018) Molecular subtypes of pulmonary large-cell neuroendocrine carcinoma predict chemotherapy treatment outcome. Clin Cancer Res 24:33–42.
Rudin CM, Pietanza MC, Bauer TM, et al (2017) Rovalpituzumab tesirine, a DLL3-targeted antibody-drug conjugate, in recurrent small-cell lung cancer: a first-in-human, first-in-class, open-label, phase 1 study. Lancet Oncol 18:42–51.
Kaemmerer D, Posorski N, von Eggeling F, et al (2014) The search for the primary tumor in metastasized gastroenteropancreatic neuroendocrine neoplasm. Clin Exp Metastasis 31:817–827.
La Rosa S, Chiaravalli AM, Placidi C, Papanikolaou N, Cerati M, Capella C (2010) TTF1 expression in normal lung neuroendocrine cells and related tumors: immunohistochemical study comparing two different monoclonal antibodies. Virchows Arch 457:497–507.
Verset L, Arvanitakis M, Loi P, Closset J, Delhaye M, Remmelink M, Demetter P (2011) TTF-1 positive small cell cancers: don’t think they’re always primary pulmonary! World J Gastrointest Oncol 3:144–147.
Haynes CM, Sangoi AR, Pai RK (2011) PAX8 is expressed in pancreatic well-differentiated neuroendocrine tumors and in extrapancreatic poorly differentiated neuroendocrine carcinomas in fine-needle aspiration biopsy specimens. Cancer Cytopathol 119:193–201.
Cheuk W, Kwan MY, Suster S, Chan JK (2001) Immunostaining for thyroid transcription factor 1 and cytokeratin 20 aids the distinction of small cell carcinoma from Merkel cell carcinoma, but not pulmonary from extrapulmonary small cell carcinomas. Arch Pathol Lab Med 125:228–231.
Ly TY, Walsh NM, Pasternak S (2012) The spectrum of Merkel cell polyomavirus expression in Merkel cell carcinoma, in a variety of cutaneous neoplasms, and in neuroendocrine carcinomas from different anatomical site. Hum Pathol 43:557–566.
Bowen NJ, Logani S, Dickerson EB, et al (2007) Emerging roles for PAX8 in ovarian cancer and endosalpingeal development. Gynecol Oncol 104:331–337.
Fabbro D, Di Loreto C, Beltrami CA, et al (1994) Expression of thyroid specific transcription factors TTF-1 and PAX-8 in human thyroid neoplasms. Cancer Res 54:4744–4749.
Poleev A, Fickenscher H, Mundlos S, et al (1992) PAX8, a human paired box gene: isolation and expression in developing thyroid, kidney and Wilms’ tumors. Development 116:611–623.
Weissferdt A, Tang X, Wistuba II, Moran CA (2013) Comparative immunohistochemical analysis of pulmonary and thymic neuroendocrine carcinomas using PAX8 and TTF-1. Mod Pathol 26:1554–1560.
Sangoi AR1, Ohgami RS, Pai RK, Beck AH, McKenney JK, Pai RK (2011) PAX8 expression reliably distinguishes pancreatic well-differentiated neuroendocrine tumors from ileal and pulmonary well-differentiated neuroendocrine tumors and pancreatic acinar cell carcinoma. Mod Pathol 24:412–424.
Bi Y, Deng Y, Li S, Zhou X, Chen Y, Ma D, Mao X, Guan Y, Chen J, Meng Y (2016) Immunophenotypic and prognostic analysis of PAX8 and TTF-1 expressions in neuroendocrine carcinomas of thymic origin: A comparative study with their pulmonary counterparts. J Surg Oncol 114:697–702.
Koo J, Zhou X, Moschiano E, De Peralta-Venturina M, Mertens RB, Dhall D (2013) The immunohistochemical expression of islet 1 and PAX8 by rectal neuroendocrine tumors should be taken into account in the differential diagnosis of metastatic neuroendocrine tumors of unknown primary origin. Endocr Pathol 24:184–190.
Lorenzo PI, Jimenez Moreno CM, Delgado I, et al (2011) Immunohistochemical assessment of Pax8 expression during pancreatic islet development and in human neuroendocrine tumors. Histochem Cell Biol 136:595–607.
Tacha D, Qi W, Zhou D, et al (2013) PAX8 mouse monoclonal antibody [BC12] recognizes a restricted epitope and is highly sensitive in renal cell and ovarian cancers but does not crossreact with b cells and tumors of pancreatic origin. Appl Immunohistochem Mol Morphol 21:59–63.
Nonaka D, Papaxoinis G, Mansoor W (2016) Diagnostic Utility of Orthopedia Homeobox (OTP) in Pulmonary Carcinoid Tumors. Am J Surg Pathol 40:738–744.
Hanley KZ, Dureau ZJ, Cohen C, Shin DM, Owonikoko TK, Sica GL (2018) Orthopedia homeobox is preferentially expressed in typical carcinoids of the lung. Cancer. Jan 9. doi: https://doi.org/10.1002/cncy.21969 [Epub ahead of print]
Silberg DG, Swain GP, Suh ER, Traber PG (2000) Cdx1 and cdx2 expression during intestinal development. Gastroenterology 119:961–971.
Moskaluk CA, Zhang H, Powell SM, et al (2003) Cdx2 protein expression in normal and malignant human tissues: an immunohistochemical survey using tissue microarrays. Mod Pathol 16:913–919.
Li MK, Folpe AL (2004) CDX-2, a new marker for adenocarcinoma of gastrointestinal origin. Adv Anat Pathol 11:101–105.
De Lott LB, Morrison C, Suster S, Cohn DE, Frankel WL (2005) CDX2 is a useful marker of intestinal-type differentiation: a tissue microarray-based study of 629 tumors from various sites. Arch Pathol Lab Med 129:1100–1105.
Ortiz-Rey JA, Alvarez C, San Miguel P, Iglesias B, Anton I (2005) Expression of CDX2, cytokeratins 7 and 20 in sinonasal intestinal-type adenocarcinoma. Appl Immunohistochem Mol Morphol 13:142–146.
Rossi G, Murer B, Cavazza A, et al (2004) Primary mucinous (so-called colloid) carcinomas of the lung: a clinicopathologic and immunohistochemical study with special reference to CDX-2 homeobox gene and MUC2 expression. Am J Surg Pathol 28, 442–452.
Enriquez ML, Baloch ZW, Montone KT, Zhang PJ, LiVolsi VA (2012) CDX2 expression in columnar cell variant of papillary thyroid carcinoma. Am J Clin Pathol 137:722–726.
Shah SS., Wu TT, Torbenson MS, Chandan VS (2017) Aberrant CDX2 expression in hepatocellular carcinomas: an important diagnostic pitfall. Hum Pathol doi: https://doi.org/10.1016/j.humpath.2016.12.029.
Erickson LA, Papouchado B, Dimashkieh H, Zhang S, Nakamura N, Lloyd RV (2004) Cdx2 as a marker for neuroendocrine tumors of unknown primary sites. Endocr Pathol 15:247–252.
La Rosa S, Rigoli E, Uccella S, Chiaravalli AM, Capella C (2004) CDX2 as a marker of intestinal EC-cells and related well-differentiated endocrine tumors. Virchows Arch 445:248–254.
Barbareschi M, Roldo C, Zamboni G, et al (2004) CDX-2 homeobox gene product expression in neuroendocrine tumors: its role as a marker of intestinal neuroendocrine tumors. Am J Surg Pathol 28:1169–1176.
Koo J, Mertens RB, Mirocha JM, Wang HL, Dhall D (2012) Value of Islet 1 and PAX8 in identifying metastatic neuroendocrine tumors of pancreatic origin. Mod Pathol 25:893–901.
Ahlgren U, Pfaff SL, Jessell TM, et al (1997) Independent requirement for ISL1 in formation of pancreatic mesenchyme and islet cells. Nature 385:257–226.
Ark JY, Hong SM, Klimstra DS, et al (2011) Pdx1 expression in pancreatic precursor lesions and neoplasms. Appl Immunohistochem Mol Morphol 19:444–449.
Srivastava A, Hornick JL (2009) Immunohistochemical staining for CDX-2, PDX-1, NESP-55, and TTF-1 can help distinguish gastrointestinal carcinoid tumors from pancreatic endocrine and pulmonary carcinoid tumors. Am J Surg Pathol 33:626–632.
Volante M, Allìa E, Gugliotta P, et al (2002) Expression of ghrelin and of the GH secretagogue receptor by pancreatic islet cells and related endocrine tumors. J Clin Endocrinol Metab 87:1300–1308.
Papotti M, Cassoni P, Volante M, Deghenghi R, Muccioli G, Ghigo E (2001) Ghrelin-producing endocrine tumors of the stomach and intestine. J Clin Endocrinol Metab 86:5052–5059.
La Rosa S, Boni L, Finzi G, et al (2010) Ghrelin-producing well-differentiated neuroendocrine tumor (carcinoid) of tailgut cyst. Morphological, immunohistochemical, ultrastructural, and RT-PCR study of a case and review of the literature. Endocr Pathol 21:190–198.
Falkmer UG, Gustafsson T, Wenzel R, et al (2015) Malignant presacral ghrelinoma with long-standing hyperghrelinaemia. Ups J Med Sci 120:299–304.
La Rosa S, Vanoli A (2014) Gastric neuroendocrine neoplasms and related precursor lesions. J Clin Pathol 67:938–948.
Vanoli A, La Rosa S, Klersy C, et al (2017) Four Neuroendocrine Tumor Types and Neuroendocrine Carcinoma of the Duodenum: Analysis of 203 Cases. Neuroendocrinology 104:112–125.
La Rosa S, Pariani D, Calandra C, Marando A, Sessa F, Cortese F, Capella C (2013) Ectopic duodenal insulinoma: a very rare and challenging tumor type. Description of a case and review of the literature. Endocr Pathol 24:213–219.
Fiocca R, Capella C, Buffa R, et al (1980) Glucagon-, glicentin-, and pancreatic polypeptide-like immunoreativities in rectal carcinoids and related colorectal cells. Am J Pathol 100:81–92.
Azumi N, Traweek ST, Battifora H (1991) Prostatic acid phosphatase in carcinoid tumors. Immunohistochemical and immunoblot studies. Am J Surg Pathol 15:785–790.
Sohn JH, Cho MY, Park Y, et al (2015) Prognostic significance of defining L-cell type on the biological behavior of rectal neuroendocrine tumors in relation with pathological parameters. Cancer Res Treat 47:813–822.
Moore P S, Missiaglia E, Antonello D, Zamo A, et al (2001) Role of disease-causing genes in sporadic pancreatic endocrine tumors: MEN1 and VHL. Genes Chromosomes Cancer 32:177–181.
Komminoth P, Klöppel G, Korbonits M, Mete O, Scoazec JY, Stratakis CA (2017) Multiple endocrine neoplasia type 1. In: Lloyd RV, Osamura RY, Klöppel G, Rosai J (eds) WHO classification of tumours of endocrine organs. IARC Press, Lyon, pp 243–247.
Pellegata NS, Klöppel G (2017) Multiple endocrine neoplasia type 4. In: Lloyd RV, Osamura RY, Klöppel G, Rosai J (eds) WHO classification of tumours of endocrine organs. IARC Press, Lyon, pp 253–254.
Occhi G, Regazzo D, Trivellin G, et al (2013) A novel mutation in the upstream open reading frame ofthe CDKN1B gene causes a MEN4 phenotype. PLoS Genet 9:e1003350.
Couvelard A, Hammel P, Komminoth P, Mete O, Pacak K, Perren A, Stratakis CA (2017) von Hippel-Lindau syndrome. In: Lloyd RV, Osamura RY, Klöppel G, Rosai J (eds) WHO classification of tumours of endocrine organs. IARC Press, Lyon, pp 157–261.
Hoang MP, Hruban RH, Albores-Saavedra J (2001) Clear cell endocrine pancreatic tumor mimicking renal cell carcinoma: a distinctive neoplasm of von Hippel-Lindau disease. Am J Surg Pathol 25:602–609.
Singh R, Basturk O, Klimstra DS, et al (2006) Lipid-rich variant of pancreatic endocrine neoplasms. Am J Surg Pathol 30:194–200.
Fryer E, Serra S, Chetty R (2012) Lipid-rich (“clear cell”) neuroendocrine tumors of the pancreas in MEN 1 patients. Endocr Pathol 3:243–246.
La Rosa S, Uccella S, Marchet S, Capella C, Lloyd RV (2004) Localization of inhibins and activins in normal endocrine cells and endocrine tumors of the gut and pancreas: an immunohistochemical and in situ hybridization study. J Histochem Cytochem 52:217–222.
Niemeijer ND, Papathomas TG, Korpershoek E, et al (2015) Succinate dehydrogenase (SDH)-deficient pancreatic neuroendocrine tumor expands the SDH-related tumor spectrum. J Clin Endocrinol Metab 100:E1386–E1393.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
SU and SLR declare that they have no conflict of interest. MV received honoraria from Novartis and MSD. MP received honoraria from Novartis, Roche, AstraZeneca, MSD, and Pfizer.
Rights and permissions
About this article
Cite this article
Uccella, S., La Rosa, S., Volante, M. et al. Immunohistochemical Biomarkers of Gastrointestinal, Pancreatic, Pulmonary, and Thymic Neuroendocrine Neoplasms. Endocr Pathol 29, 150–168 (2018). https://doi.org/10.1007/s12022-018-9522-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12022-018-9522-y