Abstract
Our experiment investigated the mRNA expression of intestinal gonadotropin-releasing hormone (GnRH), proglucagon (PG), and glucagon-like peptide 1 receptor (GLP-1R) in the jejunum, ileum, and colon of rats fed with high-fat diet and Goto-Kakizaki (GK) rats and revealed the physiological role of intestinal GnRH. We found that the GnRH and PG mRNA levels in high-cholesterol (HCh) diet were higher than in the control. However, the GnRH receptor (GnRHR) and GLP-1R mRNA levels did not differ significantly between HCh and control. The GnRH, PG, and GLP-1R mRNA levels in GK rats were lower, respectively, than those in control rats, while the GnRHR levels did not differ significantly between GK rats and control rats. There were no difference in GnRH, PG, GnRHR, and GLP-1R mRNA levels in the ileum and colon tissue between HCh and control rats. The GnRH mRNA levels of GK rats were lower than those in control rats; however, the PG, GLP-1R, and GnRHR levels did not differ significantly between GK and control rats. The GLP-1R mRNA levels of GK rats were lower than those in control rats. The GnRH mRNA expression showed positive correlation with PG mRNA expression in different intestinal sections. The GnRH level in the jejunum showed a significant effect on blood glucose level, while the PG level in the jejunum showed a significant effect on insulin level. This may imply that, compared with the ileum and colon, the jejunum had greater impact on glucose metabolism; furthermore, GnRH might interact with intestinal GLP-1 and GLP-2 through the paracrine and autocrine ways and then regulate glucose metabolism and insulin secretion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As one of the major digestion and absorption organs, the intestinal tract is also known as the largest endocrine organ in vivo which can secrete a variety of intestinal hormones. It was confirmed that glucagon-like peptide 1 (GLP-1) and glucose-dependent insulinotropic peptide (GIP) secreted by the intestinal tract played an important role in pathogenesis and treatment of type 2 diabetes. Based on the role of incretins on regulating glucose metabolism, the “enteroinsular axis” is proposed. However, the mechanisms of the intestinal tract regulating type 2 diabetes are not clear.
As early as 1906, Moore tried to treat diabetes by administration of an acid extract of duodenal mucous membrane through the mouth and found that the sugar diminished gradually and finally disappeared from the urine [1]. Nauck found that oral glucose can stimulate higher insulin secretion than intravenous glucose administration [2]. Simultaneously, they also found that, despite higher glucose secretion, immunoreactive insulin and related peptide responses after oral glucose were delayed in diabetic patients [3]. It was also noticed that in vivo colonic administration of a-LA promoted the secretion of incretin GLP-1 by activating the ERK pathway in L cells and thereby enhanced the secretion of insulin [4]. Patriti reported that glucose tolerance improved in the ileal transposition diabetic group 30 and 45 days after surgery and there was no significant difference in insulin sensitivity between the diabetic and normal groups [5]. Moreover, GLP-1 levels were significantly higher in the ileal transposition diabetic rats compared with the sham-operated rats. The study of Rubino showed that bypass of the duodenum and jejunum can reduce fasting glycemia and improve both glucose tolerance and insulin action, not secondarily related with weight loss or treatment of obesity. It is considered that bypass of the duodenum and jejunum can directly control type 2 diabetes [6]. In addition, they also found that exclusion of the proximal small intestine from contacting with ingested nutrients was a critical component in the mechanism of improving glucose tolerance after duodenal–jejunal bypass in Goto-Kakizaki (GK) diabetic rats [7]. Recent study demonstrated that earlier after gastric bypass surgery (GBP), the greater GLP-1 and GIP release, and improvement of incretin effect are related not to weight loss but rather to the surgical procedure [8].
These studies showed us using the rearrangement of the anatomical position of the stomach and small intestine as new methods to treat diabetes. Although the mechanism is unclear, these experiments support a view that type 2 diabetes mellitus (T2DM) is an intestinal disease. These results also indicated that the intestinal system contained important pathophysiological mechanisms impacting diabetes development. Intestinal factors had a clear role in glucose regulation and even pathogenesis of type 2 diabetes. However, in addition to GLP-1 and GIP, little is known about the role of other gastrointestinal hormones on regulating glucose metabolism.
We previously demonstrated that the gonadotropin-releasing hormone (GnRH) and its receptor were expressed in rat gastrointestinal system, pancreas, and submaxillary glands, and its receptor has the same mRNA sequence with that of the hypothalamus, which demonstrated that GnRH was a brain–gut peptide [9–13]. Furthermore, we proved that GnRH and its receptor were also expressed in glucagon-immunoreactive cells of rat ileum and colon, and GnRH analogs had a regulatory role on intestinal glucagon-like immunoreactivity [14]. Glucagon and GLP-1 shared quite high homology, suggesting that intestinal GnRH may have a regulatory role on GLP-1. Many studies have shown that there was relationship between GnRH and glucose metabolism. Smith et al. found that GnRH agonists administration led to insulin resistance (IR) syndrome and decreased insulin sensitivity in patients with prostate cancer [15, 16]. GnRH agonists also increased IR in premenopausal women with symptomatic uterine leiomyomas [17].
Based on the above findings, we presumed that, as a gastrointestinal hormone, GnRH may play a role on gastrointestinal motility and absorption function and on regulating other intestinal hormones secretion such as GLP-1 through autocrine, paracrine, or neural reflex ways, which further affected glucose metabolism. This has not been reported at home and abroad, and the role of the physiological GnRH in the intestinal tract requires further study.
In this study, we detected intestinal GnRH and its receptor, proglucagon (PG), and GLP-1 receptor mRNA expression under different pathological conditions. In addition, we discerned the correlation between GnRH and PG. The aim of this study was to investigate the interaction of intestinal hormones and the relationship between intestinal hormones and insulin secretion and to provide new ideas for exploring the role of intestinal hormones in treating diabetes.
Material and Methods
Animals and Diets
Eight GK rats and 16 male Wistar rats (14 weeks old) were obtained from the Lake Animal Center in Chengdu. The rats were maintained at a stable temperature (22 ± 2°C) and humidity (55 ± 5%) with a 12-h light/dark cycle and were given free access to water. After feeding the rats on standard laboratory chow (Laboratory Animal Centre, The Fourth Military Medical University) for 7 days, Wistar rats were randomly divided into two groups. The first group of rats was given a standard laboratory chow (control), and the second group was given a high-cholesterol (HCh) diet. The HCh diet contained 1% cholesterol, 10% lard, 10% yolk, and 74% standard chow. The GK rats were given a standard laboratory chow. The rats in the groups were fed the respective diets for 14 weeks. The experimental procedure used in the present study met the guidelines of the National Institutes of Health and the regulations of The Fourth Military Medical University.
Biochemical Analyses
Blood (1 ml) was drawn from the tail vein into a disinfection centrifugal tube after overnight (12 h) fasting. The blood was centrifuged at 3,000×g for 10 min. Serum cholesterol (CH) and triglyceride (TG) were determined by biochemistry analyzer (Cobas Integra 400 Plus, Roche). Serum GnRH was measured by using the enzyme-linked immunosorbent assay kit (Adlitteram Diagnostic Laboratories).
Oral Glucose Tolerance Test and Insulin Releasing Test
The rats were orally administered with a glucose solution (2 g/kg body weight) after overnight (12 h) fasting, and blood samples were collected at fasting (0 min) and 30, 60,120, and 180 min from the tail vein after glucose administration. To determine the blood glucose and insulin levels, approximately 250 μL of blood was taken from the tail vein at each time indicated above. Blood glucose concentrations were determined by a blood glucose meter (SureStep, LifeScan). The blood was centrifuged at 3,000×g for 10 min, and the serum was stored at −20°C and used for determining the insulin level [18, 19]. The insulin level was determined by using the RIA kit (Peninsula Laboratories).
Isolation of RNA and Degradation of Genomic DNA
The rats were anesthetized with sodium pentobarbital. The different intestinal sections (jejunum, ileum, and colon) were obtained from sacrificed rats; 100 mg intestinal mucosa were scraped by slide and immediately frozen in liquid nitrogen and stored at −80°C. Tissue samples were homogenized in TRIzol reagent (Invitrogen, Carlsbad, CA,USA), shaken rapidly, and kept at 4°C for 5 min; 200 ml chloroform, 200 ml isopropyl alcohol, and 1 ml 75% ethanol were added to the homogenate, which was then centrifuged at 7,500×g at 4°C for 5 min. The pellets were air dried and dissolved in RNase-free water. The sample was diluted by diethylpyrocarbonate-treated water. The RNA samples were quantified using a spectrophotometer (Beckman Coulter, CA, USA), and its purity was assessed on the same machine using 260:280 nM ratios. DNA contamination was removed by treatment with DNase I (TaKaRa Bio, Japan); 20–50 µg RNA in a reaction volume of 50 µl, containing DNase I (RNase-free) 2 µl, ribonuclease inhibitor 0.5 µl, buffer 5 µl, and RNase-free water up to 50 µl, was incubated for 30 min at 37°C. The procedures for degradation of genomic DNA were carried out following the instructions of the manufacturer. Integrity of the RNA was determined by fractionation on agarose gel and staining with ethidium bromide. Clear bands of 28S rRNA and 18S rRNA were shown in the electrophoresis, and the sharpness of 28S bands was twice that of the 18S bands. So, the total RNA was considered to be in integrity.
Relative Real-Time Polymerase Chain Reaction
RNA samples were reverse transcribed into cDNA using the real-time polymerase chain reaction (RT-PCR) kit (SYBR PrimeScript, TaKaRa Bio, Japan). In brief, 1 µg total RNA was dissolved in RNase-free water and 5× PrimeScript Buffer 2 µl, PrimeScript RT Enzyme Mix I 0.5 µl, oligo(dT) primer 0.5 µl, and random 6-mers 0.5 µl, giving a final volume of 10 µl. The sample was incubated at 37°C (15 min), and 85°C (5 s) using the polymerase chain reaction (PCR) detection system (the Bio-Rad IQ5 System). Target gene primers were produced by TaKaRa Bio (Japan). The primers' sequences are listed in Table 1. The GAPDH gene served as the endogenous reference gene. The real-time PCR was carried out in the real-time PCR detection system (Bio-Rad IQ5 System, Bio-Rad Laboratories, USA). For each gene, real-time PCR was conducted in duplicate with a 25-µl reaction volume containing 1 µl of cDNA, 12.5 µl 2× SYBR Premix EX Taq, 1 µl PCR forward primer, 1 µl PCR reverse primer, and 9.5 µl dH2O. The PCR was carried out as follows: 10 s at 95°C, 40 cycles of 95°C for 5 s, and 20 s at 62°C.
Statistical Analysis
Each value is presented as the mean ± standard error (SE). Significances of differences among groups were evaluated using a one-way analysis of variance and Dunnett's test. Correlation was assessed by Pearson's method. Regression among variables were assessed by stepwise method (alphaenter = 0.05, alpharemove = 0.10). All statistical analysis was performed using the SPSS 11.1 software. A probability value of <0.05 was considered to be statistically significant.
Results
Body Weight and Blood Biochemical Parameters
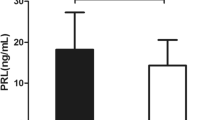
The body weight and blood biochemical parameters of rats are summarized in Table 2 and Fig. 1. At 14 days, body weight, CH, and TG were significantly higher in the HCh group than those in the control. However, body weight was significantly reduced in GK compared with that in the control. There was no difference of CH and TG between GK and control. The serum GnRH concentration was not significantly different in all groups (Table 2).
Variation in the serum glucose and insulin concentration and their AUC after feeding rats with experimental diets. a Changes of blood glucose levels at 0, 30, 60, 120, and 180 min after glucose administration. b Glucose AUC. c Changes of blood insulin levels at 0, 30, 60, 120, and 180 min after glucose administration. d Insulin AUC. Values are presented as the means ± SE, n = 8. Differences were considered significant for P < 0.05
Figure 1 illustrates the changes in the blood glucose levels and insulin levels during oral glucose tolerance test in rats. No significant differences were shown in glucose concentrations at different time points between HCh and control, whereas the glucose concentrations were significantly higher in GK than in the control (P < 0.01; Fig. 1a). The concentrations of insulin at 0, 60, 120, and 180 min were significantly higher in HCh than those in the control, while the concentrations of insulin were markedly decreased at different time points in GK compared with those of the control (Fig. 1c). There was no difference in the glucose area under the curve (AUC) value between HCh and control, but the glucose AUC value was higher in GK than in the control (Fig. 1b). The insulin AUC value showed a significant increase in HCh than in the control; however, it tended to be lower in GK than in the control (Fig. 1d).
Expression of Jejunum Tissue Genes
The results from the RT-PCR analyses of the total RNA prepared from the jejunum tissue of the rats were shown in Fig. 2. The relative expression levels of GnRH and PG mRNA in HCh rats were 1.42 and 1.55 times of those of control rats, respectively, with significant differences (P < 0.05). The GnRH receptor (GnRHR) and glucagon-like peptide 1 receptor (GLP-1R) mRNA levels did not differ significantly between HCh and control. The GnRH, PG, and GLP-1R mRNA levels in GK rats were 58%, 55%, and 64% lower, respectively, than those of control rats, while the GnRHR levels did not differ significantly between GK and control rats (Fig. 1).
The Correlation Between the GnRH mRNA and PG mRNA in Rat Jejunum
The association between the GnRH mRNA levels and PG mRNA levels in the jejunum was shown in Fig. 3. A positive association was observed between the GnRH mRNA levels and PG mRNA levels. The correlation coefficient (r) was 0.689 (P < 0.01).
Expression of Ileum Tissue Genes
The results from the RT-PCR analyses of the total RNA prepared from the ileum tissue of the rats were shown in Fig. 4. There were no difference in GnRH, PG, GnRHR, and GLP-1R mRNA expression levels in ileum tissue between HCh and control rats. The GnRH mRNA levels of GK rats were 52% lower than that of control rats; however, the PG, GLP-1R, and GnRHR levels did not differ significantly between GK and control rats (Fig. 4).
The Correlation Between the GnRH mRNA and PG mRNA in Rat Ileum
The correlation between the GnRH mRNA levels and PG mRNA levels in the ileum was shown in Fig. 5. A positive association was observed between the GnRH mRNA levels and PG mRNA levels. The correlation coefficient (r) was 0.640 (P < 0.01).
Expression of Colon Tissue Genes
The results from the RT-PCR analyses of the total RNA prepared from the colon tissue of the rats were shown in Fig. 6. There were no difference in GnRH, PG, GnRHR, and GLP-1R mRNA expression levels in colon tissue between HCh and control rats. The GLP-1R mRNA levels of GK rats were 56% lower than that of control rats; however, the GnRH, PG, and GnRHR levels did not differ significantly between GK and control rats (Fig. 6).
The Correlation Between the GnRH mRNA and PG mRNA in Rat Colon
The correlation between the GnRH mRNA levels and PG mRNA levels in the colon was shown in Fig. 7. A positive association was observed between the GnRH mRNA levels and PG mRNA levels. The correlation coefficient (r) was 0.612 (P < 0.01).
Regression Analysis
Table 3 shows the stepwise regression of blood glucose level at 180 min with GnRH and PG mRNA levels in the jejunum, ileum, and colon, respectively (alphaenter = 0.05, alpharemove = 0.10). The results showed that the GnRH mRNA level in the jejunum had a significant effect on blood glucose level at 180 min (P < 0.01; Table 3).
Table 4 shows the stepwise regression of insulin level at 180 min with GnRH and PG mRNA levels in the jejunum, ileum, and colon, respectively(alphaenter = 0.05, alpharemove = 0.10). The results showed that the PG mRNA level in the jejunum had a significant effect on insulin level at 180 min (P < 0.01; Table 4).
Discussion
IR is closely related to glucose metabolism and lipid metabolism. By giving Wistar rats the HCh diet, we established the rat model of hyperlipidemia. The GK line was established by repeated inbreeding from Wistar rats selected at the upper limit of normal distribution for glucose tolerance. The rats showed IR, the typical feature of type 2 diabetes [20]. We observed glucose metabolism-related parameters using Wistar rats as control. Although no significant differences were apparent in glucose concentrations at different time points between HCh and control, the insulin levels in HCh were higher than those in the control at 0, 60, 120, and 180 min, the insulin secretion peak was postponed to 60 min, and the insulin AUC value showed a significant increase in the HCh than in the control. All these results showed that the ability of insulin secretion in the early phase was impaired, and the insulin secretion peak was postponed in HCh rats. In addition, insulin cannot be restored to normal levels at 180 min after glucose administration, which appeared as hyperinsulinemia and IR. However, in GK rats, the blood glucose increased significantly and the insulin level is lower compared with the control and without obvious secretion peak. The two rat models represented the two phases of insulin secretion impairment, respectively, high secretion phase and insufficient secretion phase.
In the present study, we carried out RT-PCR to observe the mRNA expression of GnRH, GnRHR, PG, and GLP-1R in the jejunum, ileum, and colon of rats at 3 h after glucose administration. Although IR existed in the two rat models, the change of GnRH mRNA expression in the jejunum was different. It increased significantly in HCh rats, while it decreased in GK rats. The same differences were found in PG mRNA expression in the jejunum. There were no changes of GnRH and PG mRNA expression in the ileum and colon in HCh rats; however, in GK rats, GnRH mRNA expression decreased in the ileum and only GLP-1R mRNA expression decreased in the colon. The PG family includes GRPP, glucagon, IP-1, GLP-1, GLP-2, IP-2, pairs of dibasic amino acid residues, etc. The main translation product of PG in pancreatic islet α cells is glucagon, while GLP-1 and GLP-2 are produced in the intestinal epithelial endocrine L cells by differential processing of PG [21]. Therefore, we presumed that the changes of PG mRNA expression in the jejunum were mainly due to the changes of GLP-1 and GLP-2. In our study, the changes of GnRH and PG mRNA expression were not consistent in different intestinal sections and in different experimental groups, but it showed a significant relationship between the two genes. In addition to its effects on insulin secretion, GLP-1 exerts other significant actions, including stimulation of insulin biosynthesis, increase of insulin sensitivity, inhibition of glucagon secretion, inhibition of gastric emptying and acid secretion, reduction of food intake, and trophic effects on the pancreas [22, 23]. For many years, the molecular mechanism of the physiological role of GLP-1 and factors promoting its secretion are not clear [24–26]. It was assumed that there existed an anti-incretin system, the antagonist of incretins, in the intestinal tract, which can reduce insulin secretion, reduce the functions of insulin, and inhibit β cell growth. The balance of incretins and anti-incretin system contributed to stabilize glucose metabolism. Excessive expression of incretins or anti-incretin system could lead to glucose metabolism disorder and then to hypoglycemia or diabetes [27]. The clinical observations that gastroduodenostomy and intestinal diversion surgery could improve glucose metabolism and control diabetes supported the above speculation. The anti-incretin system was screened out currently by the animal experiment without clinical trials. It may be an unknown hormone or its function is still not fully clear.
Our previous works showed that intestinal GnRH had a regulatory role on the endocrine and exocrine of the digestive system. We noticed that GnRH was related to gastric acid secreted by parietal cells, and its analogs had an effect on the function of gastrin cells in the digestive tract of rats and could promote glucagon release in the ileum of the rat; moreover, its receptor in the intestine and pancreas coexisted with glucagon-immunoreactive cells. It was well demonstrated that there was relationship between GnRH and glucose metabolism. Several investigators have reported that GnRH agonists could increase the risk of diabetes mellitus and cardiovascular disease [15, 16]. In premenopausal women with symptomatic uterine leiomyomas, GnRH agonists also increased IR [17]. Ansari et al. found that castration of the male nonobese mouse model of autoimmune diabetes (NOD mouse) led to an increased incidence of diabetes, and GnRH administration exerted reciprocal effects, leading to earlier timing of onset of diabetes. In addition, GnRHR antagonist prevented the increased incidence of diabetes in the castrated male mice [28]. GnRH modulates the expression of diabetes in the NOD mouse independently of gonadal steroids. It was confirmed that GnRH could inhibit insulin secretion by islet cells in vitro experiments [29]. These studies indicated that GnRH could increase the IR. All previous works together with clinical observation proved that GnRH was related to insulin secretion, and it played a regulatory role on glucose metabolism.
In our study, although the changes of GnRH and PG mRNA expression are not consistent in different intestinal sections and in different experimental groups, it shows significant relativity between the two genes. In the stepwise regression analysis for GnRH and PG mRNA levels on insulin or glucose level at 180 min, GnRH mRNA level in the jejunum showed a significant effect on blood glucose level, while PG mRNA level in the jejunum showed a significant effect on insulin level. The results proved that, compared with the ileum and colon, the jejunum had a greater impact on glucose metabolism; furthermore, GnRH might interact with intestinal GLP-1 and GLP-2 through the paracrine and autocrine ways and then regulate glucose metabolism and insulin secretion. Based on these results, we presumed that gastrointestinal GnRH may be one of anti-incretin systems and it maintained the stability of glucose metabolism with incretin. However, the mechanism of that is not clear. Our further mission is to explore the interaction between intestinal GnRH and incretins and its impact on glucose metabolism, and then providing new ideas for intestinal factors treating T2DM.
References
Moore B, Eille ES, Abram JH. On the treatment of diabetes mellitus by acid extract of duodenal mucous membrane. Biochem J 1:28–38, 1906.
Nauck MA, Homberger E, Siegel EG, Allen RC, Eaton RP, Ebert R, Creutzfeldt W. Incretin effects of increasing glucose loads in man calculated from venous insulin and C-peptide responses. J Clin Endocrinol Metab 63:492–8, 1986.
Nauck MA, Stockmann F, Ebert R, Creutzfeldt W. Reduced incretin effect in type 2 (non-insulin-dependent) diabetes. Diabetologia 29:46–52, 1986.
Adachi T, Tanaka T, Takemoto K, Koshimizn TA, Hirasawa A, Tsujimoto G. Free fatty acids administered into the colon promote the secretion of glucagons-like peptide-1 and insulin. Biochem Biophys Res Commun 340:332–7, 2006.
Partriti A, Facchiano E, Annetti C, Aisa MC, Galli F, Fanelli C, Donini A. Early improvement of glucose tolerance after ileal transposition in a non-obese type 2 diabetes rat model. Obes Surg 15:1258–64, 2005.
Rubino F, Marescaux J. Effect of duodenal-jejunal exclusion in a non-obese animal model of type 2 diabetes: a new perspective for an old disease. Ann Surg 239:1–11, 2004.
Rubino F, Forgione A, Cummings D, Vix M, Gnuli D, Mingrone G, Castagneto M, Marescaux J. The mechanism of diabetes control after gastrointestinal bypass surgery reveals a role of the roximal small intestine in the pathophysiology of type 2 diabetes. Ann Surg 244:741–9, 2006.
Laferrère B, Teixeira J, McGinty J, Tran H, Egger JR, Colarusso A, Kovack B, Bawa B, Koshy N, Lee H, Yapp K, Olivan B. Effect of weight loss by gastric bypass surgery versus hypocaloric diet on glucose and incretin levels in patients with type 2 diabetes. J Clin Endocrinol Metab 93:2479–85, 2008.
Huang QW, Zhang ZL. Study of distribution on GnRH immunity activity cell and nerves in gastroenteropancreatic system. Acta Anatomica Sinica 21:20–30, 1990.
Huang QW, Xiang ZH, Meng L. Study of distribution on GnRH mRNA-positive epithelial cells and nerve cells in rat gastroenteropancreatic system. Acta Anatomica Sinica 27:35–7, 1996.
Huang QW, Yao B, Sun L, Pu RL, Wang L, Zhang RQ. Immunohistochemical and in situ hybridization of gonadotropin releasing hormone (GnRH) and its receptor in rat digestive tract. Life Sci 68:1727–34, 2001.
Yao B, Huang QW, Pu RL, Sun L. In situ hybridization study of gonadotropin releasing hormone receptor mRNA in rat digestive tract. Acta Anatomica Sinica 31:248–52, 2000.
Yao B, Huang W, Huang Y, Chui Y, Wang Y, Li H, Pu R, Wan L, Zhang R. A study on the localization and distribution of GnRH and its receptor in rat. Life Sci 72:2895–904, 2003.
Gao B, Ji QH, Huang WQ. Immunohistochemical localization of glucagon, gonadotropin releasing hormone receptor in rat digestive tract. Chinese Journal of Anatomy 27:372–9, 2004.
Smith MR. Osteoporosis and obesity in men receiving hormone therapy for prostate cancer. J Urol 172:S52–6, 2004.
Smith MR, Lee H, Nathan DM. Insulin sensitivity during combined androgen blockade for prostate cancer. J Clin Endocrinol Metab 91:1305–8, 2006.
Palomba S, Russo T, Orio Jr F, Sammartino A, Sbano FM, Nappi C, Colao A, Mastrantonio P, Lombardi G, Zullo F. Lipid, glucose and lomocysteine metabolism in women treated with a GnRH agonist with or without raloxifene. Hum Reprod 19:415–21, 2004.
Tietz NW. Textbook of clinical chemistry. New York: Saunders; 1986.
Mello de Mello MA, de Souza CT, Braga LR, dos Santos JW, Ribeiro IA, Gobatto CA. Glucose tolerance and insulin action in monosodium glutamate (MSG) obese exercise-trained rats. Physiol Chem Phys Med NMR 33:63–71, 2001.
Portha B. Programmed disorders of beta-cell development and function as one cause for type 2 diabetes? The GK rat paradigm. Diabetes Metab Res Rev 21:495–504, 2005.
Holst JJ. The physiology of glucagon-like peptide 1. Physiol Rev 87: 1409–39, 2007.
Gautier JF, Fetita S, Sobngwi E, Salaun-Martin C. Biological actions of the incretins GIP and GLP-1 and therapeutic perspectives in patients with type 2 diabetes. Diabetes Metab 31:233–42, 2005.
Bojanowska E. Physiology and pathophysiology of glucagon-like peptide-1 (GLP-1): the role of GLP-1 in the pathogenesis of diabetes mellitus, obesity, and stress. Med Sci Monit 11:RA271–8, 2005.
Pories WJ, Swanson MS, MacDonald KG, Long SB, Morris PG, Brown BM, Barakat HA, deRamon RA, Israel G, Dolezal JM, Lynis D. Who would have thought it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann Surg 222:339–50, 1995.
Pories WJ, Albrecht RJ. Etiology of type II diabetes mellitus: role of the foregut. World J Surg 25:527–31, 2001.
Rubino F, Gagner M. Potential of surgery for curing type 2 diabetes mellitus. Ann Surg 236:554–9, 2002.
Rubino F. Is type 2 diabetes an operable intestinal disease? A provocative yet reasonable hypothesis. Diabetes Care 31: S290–6, 2008.
Ansari MA, Dhar M, Spieker S. Modulation of diabetes with gonadotropin-releasing hormone antagonists in the nonobese mouse model of autoimmune diabetes. Endocrinology 145:337–42, 2004.
Klier M, Schusdziarra V, Pfeiffer EF. Effect of luteinizing hormone-releasing hormone upon insulin release from rat islets in vitro. FEBS Lett 121:363–4, 1980.
Acknowledgements
This work was supported by a grant of the National Natural Science Foundation of China (30870948) “Eleventh five-year plan AIDS and viral hepatitis prevention and treatment of infectious diseases and other major special major science and technology”—Early-Warning System for Tuberculosis (no. 2008ZX100(03-008)) and Investigation on Methodology for Estimation and Prediction of HIV/AIDS Epidemic (no. 2008ZX10100(01-003)).
Conflict of interest statement
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Li Wang and Jing Wu equally contributed to this work.
Rights and permissions
About this article
Cite this article
Wang, L., Wu, J., Cao, H. et al. The Correlation Between Intestinal Gonadotropin-Releasing Hormone (GnRH) and Proglucagon in Hyperlipidemic Rats and Goto-Kakizaki (GK) Rats. Endocr Pathol 20, 227–234 (2009). https://doi.org/10.1007/s12022-009-9086-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12022-009-9086-y