Abstract
Purpose
Bone mineral density (BMD) impairment is one of the critical factors for long-term quality of life in adults growth hormone deficiency (AGHD). This study aims to investigate the annual changes in BMD in AGHD patients with different ages of onset and to identify predicting factors that influence BMD.
Methods
AGHD patients (n = 160) with available data for 4 years follow-up from a major tertiary medical center in China were retrospectively included (110 [68.8%] childhood-onset, 119 [74.4%] male). BMD of the axial bone (including total hip, neck of femur, and L1–4) derived from dual X-ray absorptiometry and final height were investigated at the first visit, 12 months, 24 months, 36 months, and 48 months thereafter. Low BMD was defined as Z-score ≤ −2.
Results
The prevalence of low BMD was 30.0% at baseline and 12.5% at 4 years of follow-up. The CO AGHD group presented a significantly lower BMD than the AO AGHD group at the baseline (P = 0.009). In contrast, the CO AGHD group had significantly greater median annual BMD change than the AO AGHD group (0.044 vs. −0.0003 g/cm2/year in L1–4, P < 0.001), indicating a significant difference in the overall BMD trend between CO and AO groups. Childhood-onset (odds ratio [OR] 0.326, P = 0.012), low serum testosterone (OR 0.847; P = 0.004) and FT4 (OR 0.595; P = 0.039) level were independent risk factors for BMD loss.
Conclusion
The annual changes of BMD show a different pattern in AGHD patients with varying ages of onset. Patients with CO AGHD have a lower bone mass, and in general, appropriate replacement therapy is necessary for long-term bone health in AGHD patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adult growth hormone deficiency (AGHD) is an uncommon condition caused by various etiologies, including hereditary and acquired disorders that impair the synthesis and secretion of growth hormone (GH) from the pituitary gland [1]. The main characteristics of AGHD include increased visceral adiposity, abnormal glucolipid metabolism, increased risk of cardiovascular diseases, low bone mass and increased risk of fracture, sarcopenia, impaired cognitive function, and decreased quality of life [2]. In recent decades, many studies have confirmed that recombinant human growth hormone (rhGH) is effective in improving metabolic disorders, low bone mass, and quality of life in AGHD patients [1, 3, 4].
The GH-insulin-like growth factor 1 (IGF-1) axis is a crucial regulator of bone homeostasis [5, 6]. In childhood, GH promotes the linear growth and maturation of the skeletal system [7]. The GH/IGF-1 axis and gonadosteroids synergistically build up appropriate peak bone mass from puberty until adulthood [8] and maintain average bone mass throughout life [9]. Peak bone mass is one of the most essential factors for osteoporosis and fracture risk [10] since a better peak bone mass is associated with a slower decrease in bone mass in the later stages of life.
According to the age of onset, AGHD patients can be divided into childhood-onset (CO) and adulthood onset (AO). There is a broad spectrum of etiology in both CO and AO AGHD patients. Congenital pituitary hypoplasia is a significant etiology of CO AGHD, which is caused by abnormal temporal and spatial expression of signaling molecules and transcription factors during pituitary development [11, 12]. Pituitary hypoplasia is often accompanied by multiple pituitary hormone deficiencies that may persist throughout a lifetime. Various acquired disorders also cause CO AGHD, mainly including craniopharyngioma and other neoplasia of the sellar region. The etiology of AO AGHD patients is all acquired diseases, including various tumors, traumatic brain injury, infectious diseases, inflammatory diseases, and deposits of abnormal substances in the sellar area [1]. Low bone mass is an essential factor affecting the long-term prognosis of AGHD patients, but there is currently limited research on whether the changes in BMD in patients with CO and AO are similar in natural history. At the same time, whether rhGH replacement therapy can achieve equal clinical benefits for patients with different ages of onset has always been controversial [13]. Long-term deficiency of GH and IGF-1 is a crucial cause of bone loss in AGHD patients. Various clinical studies suggest that IGF-1 is an independent risk factor for predicting bone loss in AGHD patients. In our previous work, IGF-1 was a positive predicting factor for total volumetric BMD in patients with CO AGHD [14]. While in other groups of patients with AO AGHD, serum testosterone level was an independent influencing factor of BMD of the femoral neck and lumbar spine [15].
In this retrospective cohort study, we aimed to investigate the annual changes of BMD in AGHD patients with different ages of onset and the predicting factors of BMD.
Participants and methods
Participants
One hundred sixty AGHD patients were consecutively enrolled in this study from April 2010 to January 2023 at Peking Union Medical College Hospital. The inclusion criteria were: (1) The diagnosis of AGHD was confirmed according to the diagnostic criteria of the guideline of the American Endocrine Society [4]. Fifteen patients had undergone insulin tolerance test with a peak GH value lower than 3 ng/ml. Another 145 patients had serum IGF-1 levels below the age-adjusted reference ranges, combined with deficiencies in three or more pituitary axes. (2) Prednisone and l-thyroxine were sustained as needed. (3) For those patients with hypogonadotropic hypogonadism, testosterone or estrogen and progesterone replacement therapy were sustained in male or female patients respectively. (4) There were twice, or more available data of BMD derived from dual X-ray absorptiometry scan. The exclusion criteria were: (1) patients with hypopituitarism secondary to functional pituitary adenomas, including corticotrophin, lactotrophin, somatotrophin, and thyrotrophin. (2) patients with autoimmune hypophysis (e.g., lymphocytic hypophysis or IgG4-related hypophysis) who have received pharmacological doses of glucocorticoids, which could harm bone health. The flowchart of this study is summarized in Fig. 1.
The study protocol was approved by the Institutional Review Board of Peking Union Medical College Hospital (Beijing, China).
Data extraction and management
Demographic, clinical, and biochemical data were extracted from the electronic medical records system. The time of the first bone health assessment by DXA was defined as the baseline. Data were collected at the baseline, 12 months, 24 months, 36 months, and 48 months. Body mass index (BMI) was calculated as weight (kg) divided by height (m) squared. Serum biochemical parameters included liver and kidney function, lipid profile [total cholesterol (TC), low-density lipoprotein cholesterol (LDL-c), high-density lipoprotein cholesterol (HDL-c), and triglycerides (TG)], fasting blood sugar, fasting insulin, and HbA1c. Hormonal parameters included insulin-like growth factor-1 (IGF-1), T, and thyroid function. BMD of the femur neck, total hip, and lumbar vertebrae 1–4 (L1–4) were measured at each visit. The standard deviation score of Insulin-like growth factor-1 (IGF-1 SDS) was calculated according to previously published data from healthy Chinese adults [16]. Final height was defined as the greatest height measurement with an annual increment <0.5 cm. Standardized deviation scores (SDS) for final height were calculated with the reference standard base on the normal population [17].
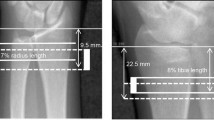
Bone mineral density investigation
BMD was assessed by dual-energy X-ray absorptiometry (Lunar Prodigy Advance, GE Lunar, Madison, WI, USA). The BMD of the axial bone (including total hip, neck of femur, and L1–4) were investigated at the first visit, 12 months, 24 months, 36 months, and 48 months thereafter. Based on the minimum BMD Z-score of axial bone, low BMD was defined as Z-score below −2. Osteopenia was defined as T-score between −1 and −2.5 or Z-score between −1 and −2. Osteoporosis was defined as T-score below −2.5 or Z-score below −2.
Statistical analysis
Statistical analysis was performed with IBM SPSS Statistics for Windows, version 27.0, and GraphPad, version 9. Data were presented as mean ± SD (or median with first to third quartile) for continuous variables normally (or not normally) distributed, respectively. All measures were checked for normality assumptions with Shapiro–Wilk test and visual inspection of QQ plots and histograms. Significance was accepted if P ≤ 0 .05.
To determine if there are any significant differences in BMD, Z-score, the annual BMD changes (g/cm2 per year), and frequencies of low BMD between patients with AO and CO AGHD, generalized estimating equation (GEE) models were built to test for significance of AGHD patients with different onset time. Repeated measure logistic regression analyses were established using the GEE models to assess the association between the clinical parameters and BMD variables. The models accounted for the correlation of repeated measures of BMD from the same subject and produced the population-averaged effect over time. BMD variables were analyzed as ordered variables with three risk groups, including normal bone mass, osteopenia, and osteoporosis. Exchangeable working correlation and robust standard error were used in GEE analysis. Adjusted factors for sex, BMI, FT4, and significant variables were selected in multivariable analysis. The model results are reported as odds ratio and pooled adjusted OR, with 95% confidence intervals.
Results
Clinical characteristics at the baseline
The baseline clinical characteristics of the 160 AGHD patients were presented in Table 1. There were 110 CO AGHD patients with pituitary hypoplasia and 50 AO AGHD patients with various acquired disorders. Among these patients, 71.4% had adrenal insufficiency and 94.6% had central hypothyroidism. All patients had hypogonadotropic hypogonadism. Diabetes insipidus occurred in 15 patients (17.0%).
In the AO AGHD group, there were 12 with intracranial germ cell tumors (24%), 14 with nonfunctioning pituitary adenomas (28%), 1 with craniopharyngioma (2%), and 23 with other disorders which caused structural damage of the saddle area, including infection, Langerhans cell histiocytosis and Rathke cyst (46%). The frequency of adrenal insufficiency, central hypothyroidism, and hypogonadotropic hypogonadism was 93.6%, 89.6%, and 80.4%, respectively. The incidence of diabetes insipidus was 57.4%.
The mean age of the CO AGHD group (27.4 ± 5.1 years) was younger than the AO AGHD group (34.4 ± 8.1 years), and the proportion of males was higher (81.8% vs 58.1%). All CO AGHD patients received rhGH replacement therapy, among which 24 patients stopped treatment due to economic burden, non-compliance, and other reasons, and their treatment stopped at a median of 3 years (first to third quartile: 1–5) prior to the first visit. The remaining patients were still receiving rhGH therapy during the follow-up period. None of the AO AGHD patients had received rhGH treatment. All male patients received intramuscular or oral testosterone undecanoate. All female patients were treated with oral replacement therapy of estrogen and progesterone combination. The IGF-1 SDS of the CO AGHD group was significantly lower than the AO AGHD group (−4.04 vs. −2.40, P = 0.000). All AGHD patients had a final height of 167.0 cm with −0.40 SDS within the normal range. The final height SDS of CO patients was significantly lower than that of AO AGHD patients (−1.14 ± 1.83 vs. −0.18 ± 1.05, P < 0.001) (Table 1).
The BMD of L1–4, total hip, and neck of femur in the CO AGHD group were significantly lower than those in the AO AGHD group (P = 0.001, P = 0.002, P < 0.001, respectively). The AO AGHD group had higher BMI SDS (0.95 vs. 0.56, P = 0.032), FT4 (1.08 VS. 0.96, P = 0.002), TC (5.11 vs. 4.57, P = 0.023) and TG (1.92 vs. 1.07, P < 0.001) levels than the CO AGHD group, while there was no significant difference in LDL-c and HDL-c levels. No differences were observed in serum T levels, and glucose metabolism parameters, including blood glucose, fasting insulin, and HbA1c between the two groups.
Bone mineral density assessment at follow-up
In BMD assessment from the first visit to the end of 4-year follow-up, all patients had at least 2 separate measurements, 24 patients had 3 separate measurements, and 3 patients had 4 separate measurements. As shown in Fig. 2a, b, mean BMD and Z-score of all AGHD patients increased over the follow-up period, with the mean BMD increasing from 0.983 ± 0.015 to 1.101 ± 0.034 (mean Z-score from −1.251 ± 0.113 to −0.88 ± 0.293) at L1–4, from 0.858 ± 0.012 to 0.930 ± 0.027 (mean Z-score ranged from −0.844 ± 0.087 to −0.286 ± 0.204) at the neck of femur, and from 0.887 ± 0.012 to 0.972 ± 0.024 (average Z-score ranged from −0.695 ± 0.085 to 0.010 ± 0.179) at total hip (all P < 0.001, Table S1). The prevalence of low BMD (Z-score below −2) decreased from 30.0% (at the first presentation) to 12.5% (at 4 years) (Table S2), and it occurred more often in patients with CO AGHD than in AO AGHD patients (P = 0.011).
The point estimates and GEE analysis of the mean absolute (g/cm2) and Z-score BMD in lumbar vertebrae, total hip, and neck of femur were visualized and summarized in Fig. 3 and Table S3, and as such, the overall significant different trend in BMD change in the CO and AO AGHD groups was visible. Trends in measured BMD changes showed that BMD increased over time in CO AGHD patients and fluctuated above and below baseline in AO AGHD patients. At baseline, a significantly lower BMD was measured in the CO AGHD group compared with the AO AGHD group in all three sits. In the area of L1–4, a gradual BMD increase from 0.926 ± 0.016 to 1.168 ± 0.031 with an annual change of 0.044 ± 0.003 g/cm2, and an average BMD Z-score increase from −1.61 ± 0.11 to −0.39 ± 0.27 were measured at 4 years follow-up for CO AGHD patients, whereas those were slightly fluctuating with a significantly lower annual BMD change of −0.0003 (−0.022, 0.023) g/cm2 for AO AGHD patients (P < 0.001, Table 2). The BMD data in the femoral neck (median 0.024 g/cm2) and total hip (0.017 g/cm2) similarly increased gradually in the CO AGHD group. In contrast, the median overall BMD of the femoral neck (0.005 g/cm2) and the total hip (0.006 g/cm2) in AO AGHD patients fluctuated less over 4 years in patients with AO AGHD (Table 2).
Analysis of factors influencing BMD change
We further investigated the factors associated with decreased BMD by analyzing patients with normal bone mass, osteopenia, and osteoporosis (Table 3). The univariable regression analyses showed that BMD tended to be lower in the CO AGHD group than in the AO AGHD group (OR 0.338; P = 0.001). Higher serum T level (OR 0.929; P = 0.019) was associated with less bone loss, whereas no significant correlation was found between IGF-1 SDS (OR 0.957; P = 0.486), FT4 (OR 0.667; P = 0.290) and BMD. The multivariable regression analysis adjusted for gender and BMI showed that the CO AGHD (OR 0.326, P = 0.012) and low serum T level (OR 0.847; P = 0.004) were both independent risk factors and low FT4 (OR 0.595; P = 0.039) was also found to be one of the contributing factors for decreased BMD.
Discussion
In this retrospective cohort study, we focused on longitudinal BMD changes in AGHD patients with different ages of onset. Our results showed that (1) there was an overall high frequency of low bone mass in both CO and AO AGHD patients; (2) CO AGHD patients presented a significantly lower BMD than AO AGHD patients; (3) CO, low serum T level and FT4 were independent risk factors for osteoporosis.
The GH/IGF-1 axis is an essential regulator of bone homeostasis throughout life [18]. GH and IGF-1 have comprehensive physiological actions on bone mineral metabolism, remodeling, and skeletal muscle [19]. Studies in rodents confirmed that IGF-1 promotes the proliferation of chondrocytes in the growth plate and regulates bone remodeling via the effects on the osteoclast, osteoblast, and osteocyte. It has also been proposed that the effects of IGF-1 on skeletal muscle precede its effects on bone. In animal models, it has been found that increased muscle mass was associated with more prominent bones in mice overexpressing IGF-1 [20]. In addition, studies have reported that circulating IGF-1 may indirectly promote periosteal apposition and mass accumulation by stimulating muscle growth [21], and a muscle-mediated link between IGF-1 and bone mass accumulation throughout adolescence has been proposed [22]. GH/IGF-1 consistently promotes linear growth during childhood and adolescent development and contributes to achieving good bone peaks. IGF-1 levels gradually decrease in adulthood and continue to play a role in maintaining bone remodeling [19].
Bone loss is a prominent clinical manifestation of AGHD. So far, many clinical studies have confirmed AGHD patients have decreased BMD, decreased bone mineral content, and increased fracture risk [23,24,25]. In our study, the IGF-1 level, and BMD of the CO group were significantly lower than that of the AO group, and the incidence of low BMD at follow-up was also significantly higher than that of the AO group. Even though all patients had received rhGH replacement therapy during follow-up, the CO AGHD group was far from achieving good bone peak value, consistent with reports from other research centers [24, 26]. It should be noted that patients with CO AGHD were shorter than AO AGHD and this might contribute to the poorer BMD in the CO AGHD group since BMD depends on height and BMD measured by DAX may be underestimated in short patients [27]. In addition, we recalculated after removing a small number of patients in the CO AGHD group who had stopped rhGH treatment prior to enrollment for personal reasons and found that there was still a significant statistical difference in BMD between the AO and CO groups (Table S3). This may be due to the short time since stopping treatment and the small number of patients. Further investigations are advocated to evaluate the effects of rhGH treatment and BMD improvement in AGHD patients with different ages of onset.
Regarding trends in BMD in AGHD patients, several studies of long-term rhGH replacement over 5–15 years have reported a sustained increase, plateau phase, or return towards baseline values in BMD value at the lumbar spine, femoral neck, or total body [28,29,30,31,32]. In our data, the mean BMD and Z-score of CO AGHD patients showed gradual increases at all three measured sites during 4 years of follow-up, and the rate of change was significantly higher than that of patients with AO AGHD. This may be because the patients with CO AGHD are relatively young, and some patients have not yet reached peak bone value. Therefore, even if rhGH treatment is stopped for various reasons and sex hormone supplementation is continued, BMD continues to increase during follow-up.
Subsequently, multivariate analysis model showed that childhood-onset AGHD, T, and FT4 levels were independent risk factors for BMD changes, which also provided a possible explanation for the more adverse BMD outcomes in CO AGHD patients and the more significant BMD increase after hormone replacement during follow-up. Although many studies have suggested that IGF-1 level was a risk factor associated with BMD, there are some controversies. In our previous work, we also found that in middle-aged male AGHD patients, childhood-onset and T level were independent risk factors for bone mass loss, but not IGF-1 level [15]. Several studies have confirmed a clear gender difference in the effect of sexual dimorphism on bone outcomes of rhGH treatment, with males showing more favorable outcomes [28]. FT4 showed inconsistent significance in univariable and multivariable analyses in this study, suggesting possible statistical confounding factors. Since significant differences in FT4 in the CO AGHD and AO AGHD groups suggested an association between the two factors, a multivariate model was then constructed to adjust for confounders to show that low FT4 was an independent risk factor for lower BMD. Thyroid dysfunction has detrimental effects on bone structures, and deficiency of FT4 impairs bone turnover by reducing osteoclastic bone resorption and osteoblastic activity [33, 34]. However, no precise data show any relationship between adult BMD and hypothyroidism, and thyroid hormone’s cellular and molecular effects on bone structure still need further investigation. There are also some evidence supports the significant role of T in enhancing the biological effect of growth hormone receptor (GHR) by promoting the expression of GHR and increasing the tissue reactivity to growth hormone. for example, replacement of both T and growth hormones are necessary for men with hypopituitarism to achieve full anabolic effects [35, 36].
In our data, significantly lower IGF-1 and FT4 levels in CO AGHD patients at baseline, as well as T levels that remained within the normal range but were relatively lower than in AO AGHD patients, may be factors associated with bone mineral density loss in CO AGHD patients. Conversely, the significantly higher proportion of men in CO AGHD patients and the faster BMD growth rate during rhGH, T, and FT4 replacement therapy also fully indicate the positive role of normal T and thyroid function in BMD changes. Therefore, although more standardized clinical studies are still needed, IGF-1, T, and FT4 levels and their complex interactions may collectively contribute to differences in AGHD patients at different age of onset.
In addition, we also found that the BMD in lumbar vertebrae increased significantly faster than in the total hip and neck of the femur. Although previous studies have demonstrated that GH has a more pronounced effect on cortical bone (femoral neck, total hip) than trabecular bone (lumbar vertebrae) [37], data from male populations showed the opposite, with lumbar trabecular bone sensitivity to gonadosteroids while BMD in femur decreasing with age in both genders [32, 38].
The final height of our CO AGHD patients was not impaired but was still significantly lower than that of the AO AGHD group. Our data reinforced the importance of appropriate rhGH substitution for pituitary hypoplasia patients during childhood and adolescence to gain final height. Our result is similar to the findings of Kendall-Taylor et al. in craniopharyngioma patients (CP) [39], who found a significantly shorter height in CO patients than in AO patients. Our data is inconsistent with another study in which the final height of patients with AO CP and CO CP was not impaired and was similar to each other [40]. These suggested that there might be heterogeneity in the clinical management of AGHD in different regions and cultures.
This is the first longitudinal study to compare the changes in BMD in CO and AO AGHD patients over 4 years of follow-up. However, there are some limitations to be acknowledged. First, this is a single-center retrospective study with a small sample size and a relatively short follow-up period of only 4 years to allow the identification of risk factors for osteoporosis in AGHD patients. Second, although only those with twice or more available data on dual X-ray absorptiometry scan results for BMD were included in the present analysis, only 10% had data at 4 years of follow-up, which is a major weakness of the study and could also introduce selection bias. Third, considering that bone mineral density is influenced by lifestyle factors, including dietary and exercise habits, these data, as well as vitamin D level and bone turnover indicators, are difficult to achieve in the retrospective study. Multicenter prospective studies to evaluate the benefits of rhGH replacement therapy in CO and AO AGHD patients are thus advocated.
In conclusion, our findings indicate that the annual changes of BMD show a different pattern in AGHD patients with different ages of onset. Patients with CO AGHD have a lower bone mass and that in general in GHD appropriate replacement therapy is necessary for long-term bone health in AGHD patients.
Data availability
All data supporting the conclusions of this manuscript are included in this published article or available from the corresponding author upon request.
References
S. Melmed, Pathogenesis and diagnosis of growth hormone deficiency in adults. N. Engl. J. Med. 380(26), 2551–2562 (2019)
N.A. Tritos, B.M.K. Biller, Current concepts of the diagnosis of adult growth hormone deficiency. Rev. Endocr. Metab. Disord. 22(1), 109–116 (2021)
C.C. van Bunderen, D.S. Olsson, Growth hormone deficiency and replacement therapy in adults: impact on survival. Rev. Endocr. Metab. Disord. 22(1), 125–133 (2021)
M.E. Molitch, D.R. Clemmons, S. Malozowski, G.R. Merriam, M. Lee Vance; Endocrine Society, Evaluation and treatment of adult growth hormone deficiency: an Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 96(6), 1587–1609 (2011)
N.A. Tritos, B.M.K. Biller, Growth hormone and bone. Curr. Opin. Endocrinol. Diabetes Obes. 16(6), 415–422 (2009)
P.S. Dixit M, S. Yakar, Effects of GH/IGF axis on bone and cartilage. Mol. Cell Endocrinol. 519, 111052 (2021)
H.L. Racine, M.A. Serrat, The actions of IGF-1 in the growth plate and its role in postnatal bone elongation. Curr. Osteoporos. Rep. 18(3), 210–227 (2020)
S.J. Holmes, S.M. Shalet, Role of growth hormone and sex steroids in achieving and maintaining normal bone mass. Horm. Res. 45(1–2), 86–93 (1996)
J.S. Walsh, Y. Henry, D. Fatayerji, R. Eastell, Hormonal determinants of bone turnover before and after attainment of peak bone mass. Clin. Endocrinol. 72(3), 320–327 (2010)
Q. Wang, E. Seeman, Skeletal growth and peak bone strength. Best Pract. Res. Clin. Endocrinol. Metab. 22(5), 687–700 (2008)
S. Zhang, Y. Cui, X. Ma, J. Yong, L. Yan, M. Yang, J. Ren, F. Tang, L. Wen, J. Qiao, Single-cell transcriptomics identifies divergent developmental lineage trajectories during human pituitary development. Nat. Commun. 11(1), 5275 (2020)
M. Gangat, S. Radovick, Pitutary hypoplasia. Endocrinol. Metab. Clin. N. Am. 46(2), 247–257 (2017)
J.J. Díez, S. Sangiao-Alvarellos, F. Cordido, Treatment with growth hormone for adults with growth hormone deficiency syndrome: benefits and risks. Int J. Mol. Sci. 19(3), 893 (2018)
H. Yang, K. Yan, X. Yuping, Q. Zhang, L. Wang, F. Gong, H. Zhu, W. Xia, H. Pan, Bone microarchitecture and volumetric bone density impairment in young male adults with childhood-onset growth hormone deficiency. Eur. J. Endocrinol. 180(2), 145–153 (2019)
S. Liu et al. Reduced bone mineral density in middle-aged male patients with adult growth hormone deficiency. Horm. Metab. Res. 54(7), 450–457 (2022)
H. Zhu, Y. Xu, F. Gong, G. Shan, H. Yang, K. Xu, D. Zhang, X. Cheng, Z. Zhang, S. Chen, L. Wang, H. Pan, Reference ranges for serum insulin-like growth factor I (IGF-I) in healthy Chinese adults. PLoS ONE 12(10), e0185561 (2017)
H. Li, C.-Y. Ji, X.-N. Zong, Y.-Q. Zhang, Height and weight standardized growth charts for Chinese children and adolescents aged 0 to 18 years. Zhonghua Er Ke Za Zhi 47(7), 487–492 (2009)
A. Giustina, G. Mazziotti, E. Canalis, Growth hormone, insulin-like growth factors, and the skeleton. Endocr. Rev. 29(5), 535–559 (2008)
S. Yakar, H. Werner, C.J. Rosen, Insulin-like growth factors: actions on the skeleton. J. Mol. Endocrinol. 61(1), T115–T137 (2018)
J. Banu, L. Wang, D.N. Kalu, Effects of increased muscle mass on bone in male mice overexpressing IGF-I in skeletal muscles. Calcif. Tissue Int. 73(2), 196–201 (2003)
L. Xu et al. Concerted actions of insulin-like growth factor 1, testosterone, and estradiol on peripubertal bone growth: a 7-year longitudinal study. J. Bone Min. Res. 26(9), 2204–2211 (2011)
M.E. Breen et al. 25-hydroxyvitamin D, insulin-like growth factor-I, and bone mineral accrual during growth. J. Clin. Endocrinol. Metab. 96(1), E89–E98 (2011)
R. Bouillon et al. Bone status and fracture prevalence in Russian adults with childhood-onset growth hormone deficiency. J. Clin. Endocrinol. Metab. 89(10), 4993–4998 (2004)
T. Rosén, T. Hansson, H. Granhed, J. Szucs, B.A. Bengtsson, Reduced bone mineral content in adult patients with growth hormone deficiency. Acta Endocrinol. 129(3), 201–206 (1993)
P.V. Carroll et al. Growth hormone deficiency in adulthood and the effects of growth hormone replacement: a review. Growth Hormone Research Society Scientific Committee. J. Clin. Endocrinol. Metab. 83(2), 382–395 (1998)
J.M. Kaufman, P. Taelman, A. Vermeulen, M. Vandeweghe, Bone mineral status in growth hormone-deficient males with isolated and multiple pituitary deficiencies of childhood onset. J. Clin. Endocrinol. Metab. 74(1), 118–123 (1992)
S. Cvijetić, M. Korsić, Apparent bone mineral density estimated from DXA in healthy men and women. Osteoporos. Int. 15(4), 295–300 (2004)
N.M. Appelman-Dijkstra et al. Effects of up to 15 years of recombinant human GH (rhGH) replacement on bone metabolism in adults with growth hormone deficiency (GHD): the Leiden Cohort Study. Clin. Endocrinol. 81(5), 727–735 (2014)
N.M. Appelman-Dijkstra et al. Long-term effects of recombinant human GH replacement in adults with GH deficiency: a systematic review. Eur. J. Endocrinol. 169(1), R1–R14 (2013)
W.M. Drake et al. The influence of gender on the short and long-term effects of growth hormone replacement on bone metabolism and bone mineral density in hypopituitary adults: a 5-year study. Clin. Endocrinol. 54(4), 525–532 (2001)
G. Götherström et al. Ten-year GH replacement increases bone mineral density in hypopituitary patients with adult onset GH deficiency. Eur. J. Endocrinol. 156(1), 55–64 (2007)
M. Elbornsson et al. Fifteen years of GH replacement increases bone mineral density in hypopituitary patients with adult-onset GH deficiency. Eur. J. Endocrinol. 166(5), 787–795 (2012)
A.P. Delitala, A. Scuteri, C. Doria, Thyroid hormone diseases and osteoporosis. J. Clin. Med. 9(4), 1034 (2020)
D. Tuchendler, M. Bolanowski, The influence of thyroid dysfunction on bone metabolism. Thyroid Res. 7(1), 12 (2014)
V. Birzniece, K.K.Y. Ho, Sex steroids and the GH axis: implications for the management of hypopituitarism. Best Pract. Res. Clin. Endocrinol. Metab. 31(1), 59–69 (2017)
J. Gibney et al. Growth hormone and testosterone interact positively to enhance protein and energy metabolism in hypopituitary men. Am. J. Physiol. Endocrinol. Metab. 289(2), E266–E271 (2005)
G. Götherström et al. A prospective study of 5 years of GH replacement therapy in GH-deficient adults: sustained effects on body composition, bone mass, and metabolic indices. J. Clin. Endocrinol. Metab. 86(10), 4657–4665 (2001)
A. Rossini et al. Bone and body composition analyses by DXA in adults with GH deficiency: effects of long-term replacement therapy. Endocrine 74(3), 666–675 (2021)
P. Kendall-Taylor et al. The clinical, metabolic and endocrine features and the quality of life in adults with childhood-onset craniopharyngioma compared with adult-onset craniopharyngioma. Eur. J. Endocrinol. 152(4), 557–567 (2005)
S.S. van Santen et al. Fractures, bone mineral density, and final height in craniopharyngioma patients with a follow-up of 16 years. J. Clin. Endocrinol. Metab. 105(4), e1397–e1407 (2020)
Acknowledgements
The authors thank the technical support of the PUMCH-EMERALD platform.
Funding
This work was supported by the National Natural Science Foundation of China (No. 81970678); National High Level Hospital Clinical Research Funding (2022-PUMCH-B-016); and CAMS Innovation Fund for Medical Sciences (CIFMS 2021-I2M-1-003).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Hongbo Yang and Meiping Chen wrote the draft of the manuscript and prepared figures and tables; Huijuan Zhu and Hui Pan designed the study; Linjie Wang, Lian Duan, Yunfeng Zhen, and Hanyuan Xu collected the clinical data; Fengying Gong helped analyze biochemical data; Yuelun Zhang guided the data processing and statistical analysis. All authors reviewed and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yang, H., Chen, M., Xu, H. et al. Bone mineral density in adults growth hormone deficiency with different ages of onset: a real-world retrospective study. Endocrine 85, 347–355 (2024). https://doi.org/10.1007/s12020-024-03786-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-024-03786-4