Abstract
The aim of this study was to measure bone mineral density (BMD) in healthy people and examine the influence of age, anthropometry, and postmenopause on calculated bone mineral apparent density (BMAD). The study included 541 healthy subjects (249 men and 292 women), aged 20 to 79 years. Anthropometric measurements included height, weight, and body mass index (BMI). Bone mineral content (BMC) and areal BMD were measured at the lumbar spine and proximal femur, using dual-energy X-ray absorptiometry (DXA). The calculation of volumetric density relied on the formula BMAD=BMD/√BA (where BA = bone area). Association between densitometric parameters and age, height, weight, and postmenopause was analyzed with multiple regression. BMC and BMD decreased with age, especially in postmenopausal women. The average annual bone loss in spine was 0.2% in both sexes, whereas femur loss was 0.5% in men and 0.3% in women. Bone area slightly increased with age in both sexes, and BMD loss after the age of 50 could be attributed to bone area increase. To minimize the effect of bone size on bone density, volumetric density and areal density were regressed to age, anthropometry, and postmenopause. Age and postmenopause were significantly associated with BMD and BMAD in the spine and femur. Furthermore, BMD showed a stronger association with height and weight than BMAD, in both regions. Weaker association of body height and weight with BMAD than with BMD suggests that BMD depends on the bone size and body size and that the different BMDs could be the consequence of the difference in those parameters.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bone mass is determined by many factors including age, sex, body size, ethnicity, and behavioral factors. Analysis of the extent to which all of these factors contribute to bone mineral density (BMD) and age-dependent bone loss is important in predicting fracture incidence as the most important consequence of osteoporosis. Several studies have presented bone mineral density reference data for adults [1, 2, 3, 4, 5, 6]. Ethnic and geographic variations are usually well recognized. However, the different recruitment of study population and different techniques for BMD measurement can make comparison between populations less clear. Dual-energy X-ray absorptiometry (DXA) is the dominant method for evaluating bone mineral status. It measures areal BMD. Although BMD is a measurement of choice, it is influenced by body size and does not represent true volumetric density. In order to reduce the effect of bone and body size on area BMD measurement, several estimates of volumetric bone density have been proposed. Those parameters are less sensitive to differences in skeletal size than BMD [7, 8].
This study had three objectives. The first was to measure the BMD in healthy Croatians and compare the results with those from other countries. The second was to calculate bone mineral apparent density as an estimation of volumetric density which reduces the effect of body size on bone mass. The third objective was to assess the influence of age, body size, and postmenopause on densitometric parameters.
Methods
Subjects
The selection of the participants was partly performed from the local hospital and institute staff and their friends and relatives (36.4%). We also analyzed the database records of men and women who had been referred to densitometry at the Institute’s Center for Osteoporosis, in the period from 1992 to 1998. The exclusion criteria were diseases affecting bone metabolism (hyperparathyroidism, hyperthyroidism, Paget’s disease, renal or hepatic failure, and chronic gastrointestinal disease), prolonged immobilization, previous atraumatic fracture, and present or previous therapy with estrogen, corticosteroids, or thyroxine. Of 228 persons who were invited and agreed to participate in the study, 192 passed the exclusion criteria. Each subject was interviewed by the physician to obtain information about age, menopause (women), diseases, fracture history, and drug therapy.
Total study population comprised 541 subjects (249 men and 292 women). The mean age of men was 49.3 ± 13.5 years and of women 51.0 ± 10.1 years.
Measurements
Body height and weight were recorded. BMD (g/cm2) at the lumbar spine (L2–L4) and proximal femur was measured using a Lunar DPX (Madison, WI). BMD of the femur was expressed as the mean of the BMD values for the femoral neck, Ward’s triangle, and trochanter. Bone mineral content (BMC; g) and bone area (BA; cm2) were calculated using the original software of the densitometer. Volumetric, three-dimensional approximation of bone density, called bone mineral apparent density (BMAD; g/cm3) was calculated by dividing the bone mineral density in spine or femur by the square root of the spinal or femoral bone area [7]. Osteoporosis was diagnosed using WHO criteria(T-score lower than −2.5 standard deviations was defined as osteoporosis) [9].
Daily quality control was managed by performing calibrations with a machine-specific phantom. The in vitro coefficient of variation for BMD, calculated on a spine phantom, was 0.31. The in vivo coefficient of variation was obtained by scanning lumbar spine and proximal femur 10 times on one healthy volunteer. The coefficient was 1.36% for the spine, 1.87% for the femoral neck, 3.64% for Ward’s triangle and 2.01% for the trochanter.
Statistical analysis
Results are expressed as means ± standard deviation. Differences in means between men and women, between subjects with osteopenia/osteoporosis and those with normal BMD values were tested by Student’s t-test. The effect of age, height, weight, and duration of postmenopause on BMD and BMAD was tested with multiple regression analysis. The value p<0.05 was considered significant in all statistical tests.
Results
Table 1 shows bone mineral content, area of measurement, and bone mineral density in the spine and the proximal femur for men (A) and women (B) by decades. Men had a relatively stable spinal BMD at the age of 20 to 30 years. BMD in femur was the highest at age of 20 years. Separate analysis of 20- to 80-year-old men showed a continuous, although nonsignificant decline in BMD in both regions. Women had significantly lower BMD in spine after the age of 40 years (p<0.05) and nonsignificantly higher values after the age of 60 years. Femur BMD in women showed continuous but nonsignificant decline from age 40 to 70 years.
Spinal osteoporosis was found in 4% of men, as was femoral ostreoporosis, while 4% of women had spinal osteoporosis and 6% had femoral osteoporosis.
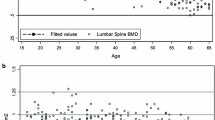
Figure 1 shows the changes in BMD, BMC and bone area by 10-year age groups. The differences in all three parameters were calculated between the youngest and the oldest age groups. In men, the spine region showed a significantly lower BMD (p<0.0001) and higher bone area (p<0.01). BMD changed mostly until the age of 50, from which point it plateaued in older age groups. Approximately 60% of the difference in spinal BMD between the youngest and oldest age groups (−11.4%) may be attributed to the difference in the bone area (+7.5%) and 40% to the difference in BMC (−4.5%). The difference of BMD and BMC of the femur between the youngest and oldest age groups was significant (p<0.0001 for BMD, and p<0.01 for BMC), while the difference of bone area (+8%) was nonsignificant. Therefore, the difference in BMC contributed to about 70% of difference in BMD in femur (−27.6%).
In women, BMD and BMC differences in spine were the biggest between the age groups of 40 and 60. There was a slight change in spinal bone area (−2.5%) between the youngest and the oldest age groups, while the changes of BMC and BMD were significant (p<0.01). There was an increase of BMC and bone area of the femur in women aged between 20 and 30. Later age groups showed similar BMD and BMC curves, while the bone area significantly increased in the age groups older than 50 (p<0.01) and contributed significantly (85%) to the difference of BMD in femur (−17.0%; p<0.001).
Subjects with normal BMD had a significantly higher body height (p<0.05 men; p<0.001 women) and weight (p<0.05) than those with osteopenia and osteoporosis (T-score <−1) (Table 2). Significantly smaller spinal bone area was found in subjects with osteopenia and osteoporosis (p<0.05, men; p<0.0001, women). In the femur, that difference was significant only in women (p<0.01).
The associations of BMD and BMAD with age, height, weight, and duration of postmenopause were assessed using the regression analysis (Table 3). Age was significant for the spine and femur BMD and BMAD in both sexes. The average annual bone loss in men was 0.2% in the spine and 0.5% in the femur. In women, the average loss rate was 0.2% in the spine and 0.3% in the femur. Height was significant for the spinal BMD in both sexes and for the BMD of the femur in men (p<0.05). Weight showed stronger association with BMD, than with BMAD, in both regions. The duration of postmenopause significantly correlated with BMD and BMAD in spine and with the BMD in femur, although that significance was weaker than for weight. Postmenopausal annual decrease in BMD, calculated by dividing the total bone loss in the spine (12.5%) and femur (17.0%) by the mean duration of postmenopause (9.5 + 7.5 years), was 1.3% in the spine and 1.8% in the femur.
Discussion
In this study, we presented the bone mineral density in healthy Croatians and adjusted those values for apparent bone volume. Croatia is a southeastern European country on the Adriatic sea. Approximately 60% of the population is urban [10]. Data show that 34.1% men and 26.6% women are regular smokers, while regional differences have been observed with respect to alcohol consumption and diet. Milk and cheese consumption is more frequent in coastal Croatia (more than twice a week in 64.6% of the population vs in 41.7% of those in the capital, Zagreb) [10].
Most studies on BMD normative data were based on random population samples [3, 4, 10, 11, 12, 13, 14]. But there are also several studies which have not been based on a random population sample [1, 2, 5, 15, 16]. We decided to include healthy people from the Croatian population and to apply exclusion criteria to identify a more homogenous subset of that population. Nonrandom selection could result in inclusion of subjects who had already complained about bone problems or menopause, which can influence and depress the mean BMD. But in our study, subjects with atraumatic fractures, diseases, therapy, or other risk factors which interfere with bone metabolism, were excluded. We found that our values were similar to those reported in England [5] and Germany [3]. Many studies included only a female population [1, 2, 4, 16] or only one site of measurement (spine or femur) [3, 5, 16, 17]. In addition, different sample procedures and different sample sizes were used in different studies. The North American BMD values for women, reported by Mazess and Barden [1], are significantly higher in the femur and approximately 2.0% higher in the spine than in our women (+12.5%). In contrast, the Rancho Bernardo study [6] of men and women older than 50 years showed a significantly lower spinal BMD than did our study, in women of the same age, while BMD was significantly higher in proximal femur and male population of the same age. BMD values in our study are higher than those of Swedish women [4] or Japanese women and men [15]. As Guglielmi proposed [18], due to geographic variations in bone density and interscanner variability, BMD data should ideally be obtained locally in accordance with similar studies from other countries [19, 20, 21, 22]. BMD decreased by age in both regions and in both sexes. Although this partly reflects the expansion of the projected skeletal area, it was mostly due to the decreased BMC. A similar pattern of area and BMC changes was observed in the United States [1] and in the United Kingdom [5]. A relatively large increase in the projected area was obvious in the proximal femur, and it significantly correlated with age. Mazess and Barden [1] reported that 42% of the area of the total femur proximal region was located in the trochanteric region; Ward’s triangle and the neck area kept relatively constant with age, while the trochanter area showed an increase with age, reaching its peak at the age of 50–59 years. This is similar to our results for women.
Regression analysis showed that body weight was significantly associated with BMD and BMAD. Other studies also showed the importance of considering body weight in evaluation of osteoporosis [23, 24]. Mazess and Barden proposed that body weight be used as an indication for bone densitometry in asymptomatic subjects [1]. The dependence of BMD on bone and body size was corrected by calculating BMAD as a more accurate indicator of volumetric density [7]. When BMD and BMAD were regressed against age, height, weight, and postmenopause, we found that the areal density correlated more with anthropometric predictors than with volumetric density. Other studies also found that BMAD was less dependent on body size than BMD [7, 24, 25, 26]. It became obvious that the differences in bone density between subjects with normal BMD and those with osteopenia and osteoporosis could be the consequence of smaller bone areas and smaller bones. Therefore, we may presume that small bones are a risk factor for osteoporosis. Measuring the true volumetric bone density could improve the accuracy of predicting the risk for fracture.
However, although the BMAD is less dependent on height, it does not always seem to be superior to BMD in distinguishing between normal and osteoporotic patients [25, 27]. BMAD is an approximation of the real volumetric bone density and it seems that it increases the effect of larger bone sizes [28]. Therefore, the BMAD values could be lower than volumetric bone density measured with QCT. Mazess et al. [29] suggest that BMD still remains superior to its alternatives, which diminish the dependence of BMD on bone area and body size.
As the number of subjects included in this study was relatively low, we may conclude that our data are only an anticipation of a normative Croatian database. Furthermore, as the subjects were not selected at random from the population census data, selection bias could not have been eliminated. A comparison with other BMD studies which have used a different selection of subjects, and different sizes of study samples, measurement techniques, and statistical models, suggests that our BMD data are similar to those from countries of central and western Europe. As expected, men had a higher BMD than women, who in turn showed a significant BMD decrease in the 5th decade of their life. Thanks to BMAD, which minimized the effect of body size on the bone mass, we were able to infer that the differences in the bone mass between subjects could be due to differences in bone areas and bone sizes.
The prevalence of osteoporosis in our population was based on the manufacturer’s (NHANES) data, which might have led to a more frequent diagnosis of osteoporosis in men. As an illustration of this, Lehmann et al., relying on manufacturer’s reference range, found that 10% of men were below the –2.0 SD limit, instead of the expected 2.2% [3]. We also found that the average bone loss rate in the femur was higher in men than in women. We may assume that the differences between men and women in lifestyle (30.8% of men and 17.3% of women were smokers; 21.4% of men and 3.6% of women were regular alcohol consumers) and sample sizes could have played a role. The most likely reason is a cohort effect, in that one cohort and not the other experienced an unknown effect, which is the reason for biases in many studies.
In conclusion, this study showed that BMD data for Croatians closely resemble that from other European studies. In addition, we showed that the estimated volumetric mineral density minimized the confounding effects in differences in bone size resulting from differences in age, height, and weight, and that it was a better indicator of true bone density and bone strength than areal bone density.
References
Mazess RB, Barden H (1999) Bone density of the spine and femur in adult white females. Calcif Tissue Int 65:91–99
Dougherty G, Al-Marzouk N (2001) Bone density measured by dual energy X-ray absorptiometry in healthy Kuwaiti women. Calcif Tissue Int 68:225–229
Lehmann R, Wapniarz M, Randerath O et al (1995) Dual energy X-ray absorptiometry at the lumbar spine in German men and women: a cross-sectional study. Calcif Tissue Int 56:350–354
Löfman O, Larsson L, Ross L, Toss G, Berglund K (1997) Bone mineral density in normal Swedish women. Bone 20:167–174
Truscott JG, Oldroyd B, Simpson M et al (1993) Variation in lumbar spine and femoral neck bone mineral measured by dual energy X ray absorption: a study of 329 normal women. Br J Radiol 66:514–521
Blunt BA, Kaluber MR, Barret-Connor EL, Edelstein SL (1994) Sex differences in bone mineral density in 1653 men and women in the sixth through tenth decades of life: the Rancho Bernardo study. J Bone Miner Res 9:1333–1338
Carter DR, Bouxsein ML, Marcus R (1992) New approaches for interpreting projected bone densitometry data. J Bone Miner Res 7:137–145
Braillon PM (1999) Volumetric bone mineral density derived from dual-energy X-ray absorptiometry measurements. Nucl Med Commun 20:106
World Health Organization. (1994) Assessment of risk fracture risk and its association to screening for postmenopausal osteoporosis. Report of a WHO Study Group. World Health Organ Tech Rep Ser 843:1
Turek S, Rudan I, Smolej-Narabčić N et al (2001) A large cross-sectional study of health attitudes, knowledge, behaviour and risks in the post-war Croatian population: the First Health Croatian Project. Coll Antropol 25:77–96
Diaz Curiel M, Carrasco de la Pena JL, Honorato Perez J, Perez Cano R, Rapado A, Ruiz Martinez I (1997) Study of bone mineral density in lumbar spine and femoral neck in a Spanish population. Osteoporos Int 7:59–64
Burger H, van Daele PLA, Algra D et al (1994) The association between age and bone mineral density in men and women aged 55 years and over: the Rotterdam study. Bone Miner 25:1–13
Kröger H, Tuppurainen M, Honkanen R, Alhava E, Saarikoski S (1994) Bone mineral denisty and risk factors for osteoporosis—a population based study of 1600 perimenopausal women. Calcif Tissue Int 55:1–7
Sowers M, Crutchfield M, Bandekar R et al (1998) Bone mineral density and its change in pre-and perimenopausal white women: the Michigan Bone Health Study. J Bone Miner Res 13:1134–1140
Norimatsu H, Mori S, Uesato T, Yoshikawa T, Katsuyama N (1989) Bone mineral density of the spine and proximal femur in normal and osteoporotic subjects in Japan. Bone Miner 5:213–222
Petley GW, Cotton AM, Murrillis AJ et al (1996) Reference ranges of bone mineral density for women in southern England: the impact of local data on the diagnosis of osteoporosis. Br J Radiol 69:655–660
Looker AC, Wahner HW, Dunn WL et al (1996) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 1998; 8:468–489
Guglielmi G, Giannatempo GM, Blunt BA et al (1995) Current methods and advances in bone densitometry. Eur Radiol 5:269–273
Nilsson M, Johnell O, Jonsson K, Redlund-Johnell I (1988) Quantitative computed tomography in measurement of vertebral trabecular bone mass. A modified method. Acta Radiol 29:719–725
Compston JE, Evans WD, Crawley EO, Evans C (1988) Bone mineral content in normal UK subjects. Br J Radiol 61:631–636
Harbison J, Daly L, Murphy B, McCoy C, Masterson J (1992) Normal bone density in Irish women: is American normative data suitable for use in Ireland? Irish J Med Sci 161:66–69
Michaelsson K, Bergstrom R, Holmberg L, Mallmin H, Wolk A, Ljunghall S (1996) Calcium intake among women aged 40–76 in Sweden. Study Group MRS SWEA (Multiple Risk Survey on Swedish Women for Eating Assessment). J Epidemiol Community Health 50:577–578
Ensrud KE, Lipschutz RC, Cauley JA et al (1997) Body size and hip fracture risk in older women: a prospective study. Study of Osteoporotic Fractures Research Group. Am J Med 103:274–280
Tsai KS, Cheng WC, Chen CK et al (1997) Effect of bone area on spine density in Chinese men and women in Taiwan. Bone 21:547–551
Jergas M, Breitenseher M, Gluer CC, Yu W, Genant HK (1995) Estimates of volumetric bone density from projectional measurements improve the discriminatory capability of dual X-ray absorptiometry. J Bone Miner Res 10:1101–1110
Cummings SR, Marcus R, Palermo L, Ensrud KE, Genant HK (1994) Does estimating volumetric bone density of the femoral neck improve the prediction of hip fracture? a prospective study. Study of Osteoporotic Fractures Research Group. J Bone Miner Res 9:1429–1432
Peel NF, Eastell R (1994) Diagnostic value of estimated volumetric bone mineral density of the lumbar spine in osteoporosis. J Bone Miner Res 9:317–320
Kalender WA, Felsenberg D, Louis O, et al. Reference values for trabecular and cortical vertebral bone density in single and dual-energy quantitative computed tomography. Europ J Radiol 1989; 9:75–80.
Mazess RB, Barden H, Mautalen C, Vega E (1994) Normalization of spine densitometry. J Bone Miner Res 9:541–548
Acknowledgements
This study was supported by the International Atomic Energy Agency, project no. 8193/R1 (“Studies of osteoporosis in Croatia using isotope related techniques”).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cvijetić, S., Koršić, M. Apparent bone mineral density estimated from DXA in healthy men and women. Osteoporos Int 15, 295–300 (2004). https://doi.org/10.1007/s00198-003-1525-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-003-1525-x