Abstract
Gastroenteropancreatic (GEP) neuroendocrine tumors (NETs) are rare neoplasms with heterogeneous clinical behavior and potential long-term survival. In 2006/2007, the European Neuroendocrine Tumors Society introduced an important parameter, grade (based on mitoses and Ki-67 proliferation rate), which became part of the latest 2010-WHO classification. Since this is an important tool in the choice of therapeutic algorithm of patients with NETs, our aim was to audit whether retrospective reclassification is possible and feasible and correlate pathological findings with survival. From the histopathology archive, 338 GEP-NETs (1994–2014) were identified, of which 250 were diagnosed pre-2010 and 80 of these have needed, up till now, classification (morphology and grade—mitotic count/Ki-67). Morphology was well differentiated (WD) in 74 cases while only 6 cases were poorly differentiated (PD). Grade was reclassified: G1—45 cases (56 %); G2—28 cases (35 %); G3—7 cases (9 %). Overall survival (OS) in WD NETs was strikingly better compared to PD neoplasms. Differences in OS between grade were statistically significant (p < 0.0001) and, in particular, grade identified a subgroup of patients with WD lesions but with less favorable clinical behavior (OS at 5 years: G1—89 %; G2—48 %; G3—0 %; G1 vs G2 p = 0.03). Feasibility analysis quantified time for reclassification to be between 45 and 64 min/case. Our series confirms the importance of grade in prognostic stratification and underlines that reclassification is feasible, and may prove worthwhile in patient management, especially in view of the potential long survival of patients with NETs and risk of use of inappropriate therapies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastroenteropancreatic (GEP) neuroendocrine tumors (NETs) are rare neoplasms with heterogeneous clinical behavior and potential long-term survival [1, 2]. In the last decade, GEP-NET nomenclature and classification have been twice reviewed. The 2000 WHO classification [3] distinguished well and poorly differentiated tumors and this distinction proved to be prognostically important. Further improvements in prognostic stratification were made with the introduction of two new important parameters: grade and stage, by ENETS [4, 5]. Grade is proliferation-based (either mitotic count and/or Ki-67 proliferation index) and has also been introduced into the new 2010 WHO classification [6]. Stage has also been shown to be prognostically important and site specific [4, 5, 7].
Several research groups have proved the reliability of the new grading system, for prognostic stratification, in many cohorts of patients [8–10] and grade has a pivotal role in the therapeutic algorithm of NET-patients [10]. Even though the importance of grade has been shown, retrospective reclassification of all GEP-NET cases has however not yet been advocated. In view of new targeted therapies, which may be indicated for specific grade NETs [11], reclassification may become ever more important. Our aim was, therefore, to audit whether retrospective reclassification is possible and feasible and correlate pathological findings with survival.
Materials and methods
From the Histopathology archives of the IRCCS San Martino-IST University Hospital, 338 GEP-NETs (dating from 1994 to 2014) have been identified. Of these, 250 were diagnosed before 2010 (year of the revised WHO classification [6]) while 165 were diagnosed before 2006 (year of the first ENETs GEP-NET staging and grading system publication [4, 5]).
Reassessment is on-going and, at this point, 80 pre-2010 patients have needed to be reassessed, including patients who are still alive or whose cases are recruited in research trials. Clinical follow-up data were obtained from patient’s charts and imaging studies for all 80 patients. The study was approved by the local ethics committee.
Morphological reassessment and reclassification
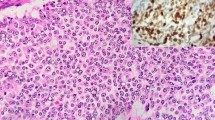
All pathologic characteristics were re-evaluated either on original slides or on new 4-micron-thick sections stained with Haematoxylin–Eosin (H&E). In particular, data on differentiation (well differentiated—WD, and poorly differentiated—PD), presence/absence of necrosis, vascular/lymphatic invasion, perineural invasion were collected. Data on classification at the time of diagnosis, according to WHO 2000 [3], were collected and all cases were further reclassified according to the 2010 WHO classification [6]. For all cases, slides were reviewed and differentiation, grade (as suggested by ENETs—mitotic count/10HPF and percentage of Ki-67 positive cells counting 2000 neoplastic cells), and stage (ENETs and UICC-2009) were re-evaluated.
Grading by mitotic count and Ki-67 immunohistochemistry
Mitotic count was performed on 50 HPF as suggested by ENETS [4, 5].
Proliferation index using Ki-67 antibodies was assessed on sections cut from one paraffin block of available tissue. In case of multiple NETs, Ki-67 was performed on the largest tumor.
From each selected paraffin block, 4-micron-thick sections were cut and mounted on appropriate slides (SuperFrost® Plus, Thermo Scientific, Braunschweig, Germany) in order to improve adherence. All sections were used for immunohistochemistry (IHC) within 1 month of cutting [12]. IHC was performed using the Ventana BenchMark® XT platform (Ventana Medical Systems, Arizona, USA) automated immunostaining device, according to the manufacturer’s protocol, using 3,3′-diaminobenzidine as chromogen.
Briefly, sections were deparaffinized and rehydrated. After epitope retrieval with a heat standard pretreatment (Thermopad 98–100 °C for 30′) sections were incubated with primary antibodies against Ki-67 (prediluted; Ventana Medical Systems, Arizona, USA) and immunoperoxidase reaction performed according to procedure. The slides were then counterstained with haematoxylin and cover-slipped.
Assessment of Ki-67 was expressed as a percentage by counting the number of positive tumor cells/2000 cells, in “hot spots” [4, 5]. To ease counting, microphotographs were taken at ×40 magnification in the area of highest Ki-67 labeling and color printed [13, 14]. If 2000 neoplastic cells were not reached on the first microphotograph, an adjacent field to the first one selected was photographed and cells counted.
Feasibility of reclassification
Feasibility was expressed in man-time (in minutes) and differed according to whether the specific task was performed by the laboratory technician or pathologist. A breakdown of the necessary steps which lead to case retrieval and to reclassification was performed and each step quantified. The following stages were necessary for case reclassification:
-
Case retrieval/80 cases
-
Slide retrieval/80 cases
-
Paraffin block retrieval/57 cases (in 23 cases Ki-67 had already been performed at original diagnosis)
-
Sections and immunohistochemistry/57 cases
-
Pathological reclassification/80 cases
-
Mean time per case.
Statistical analysis
Kaplan–Meier methodology was used to evaluate overall survival, stratified by original diagnosis and according to reclassified grade. All statistical tests were performed using SPSS, Inc., IL, USA.
Results
Clinico-pathologic characteristics
Mean age at diagnosis of the 80 reclassified patients was 61 years, F:M ratio was 1:1.1 and mean follow-up was 52 months (2–196).
The primary sites were as follows: stomach 6; duodenum 3; ileum 32; appendix 4; colon 5; pancreas 19; liver metastases from unknown primary 11. With regard to gastric neoplasms, 3 cases were WD and localized within the gastric body and associated with chronic atrophic gastritis, 1 case was WD, gastrin producing and localized in the gastric antrum and 2 cases were PD sporadic neuroendocrine carcinomas.
Morphology was WD in 74 cases while only 6 cases were PD. Grade was reclassified as follows: 45 cases (56 %) as G1; 28 cases (35 %) as G2; 7 cases (9 %) as G3. One pancreatic primary showed WD morphology but was G3 at Ki-67 evaluation (35 %). Stage at diagnosis was distributed as follows: stage I—14 cases (17.5 %); stage II—10 cases (12.5 %); stage III—24 cases (30 %); stage IV—32 cases (40 %).
Survival analysis
At the time of reclassification 53 out of 80 patients were alive.
Correlating differentiation with overall survival (OS), WD NETs had strikingly better outcome compared to PD neoplasms (p < 0.0001). According to WHO 2000 classification, OS at 5 years was as follows: WD tumor—100 %; WD carcinoma—78 %; PD carcinoma—0 %; p < 0.0001.
Differences in OS between G1, G2, and G3 (Fig. 1) were statistically significant (p < 0.0001) and, in particular, grade identified a subgroup of patients with WD lesions (G2) but less favorable clinical behavior (OS at 5 years: G1—89 %; G2—48 %; G3—0 %; G1 vs G2 p = 0.03).
One patient with a WD pancreatic primary at morphology but a Ki-67 of 35 % (G3) showed OS of 36 months. This length of survival is definitely longer compared to the other patients with PD G3 carcinomas (median OS 9; range 2–30 months).
Feasibility analysis
Feasibility of reclassification is shown in Fig. 2. The flow diagram represents the necessary steps for case selection and reclassification as well as times and personnel necessary (pathologist vs laboratory technician) for each step. If Ki-67 was already present in the Pathology slide archives, then time necessary for reclassification (approximately 45 min per case) was mostly dependent on the Pathologist looking at the slides and evaluating grade (mitotic index and Ki-67 rate). If, on the other hand, Ki-67 needed to be performed de novo, then necessary time lengthened to 64 min per case, of which approximately one half was pathologist’s time (38 min).
Flow diagram of the necessary steps for case selection and reclassification as well as times and personnel necessary (Pathologist—P vs Laboratory Technician—LT) for each step. The table shows total and single case mean time in minutes, distinguished for Pathologist and Laboratory Technician. *Cases in which Ki-67 was not already available
Conclusions
Our series confirms the importance of grade in prognostic stratification and underlines that reclassification is feasible, and may prove worthwhile in patient management (53 patients were alive and only 15 were disease free).
Reclassification is important as it permits the identification of a subgroup of G2 patients, previously classified as WD carcinomas according to WHO 2000 [3], who have a worse outcome compared to equal stage G1 tumors (also classified as WD carcinomas according to WHO 2000). Furthermore, within our cohort, a single patient with a G3 WD pancreatic tumor showed different clinical behavior with longer survival (36 months) compared to the median of G3 PD carcinomas (OS median 9 months). This is in line with emerging data on this subtype of WD G3 neoplasms [15] which will need further study in the future.
Currently, diverse treatment options, such as biological or target therapies and chemotherapies, are available for NETs and these therapies have proven their efficacy in recent studies on these neoplasms [11, 16, 17]. However, to date, there is still no standardized therapeutic sequence. The clinician therefore must have as much information as possible about tumor biology in order to choose the most appropriate treatment in individual patients. Indeed, it is not uncommon, given the long survival of patients, to choose a treatment based on pre-WHO 2010 histologic reports. Recent treatment algorithms, such as those proposed by the ESMO Guidelines [18], indicate grade as one of the variables to consider, for tailoring treatment.
The present study also highlights that reclassification is possible, even though there is a time and cost burden for Pathology which must be considered. Nevertheless, if we compare reclassification costs to treatment expenditure, accurate grading becomes fundamental and economically worthwhile. Benefits of reclassification also include the reduction in possible over or under-treatment of inadequately studied patients.
In conclusion, in consideration of the possible lengthy survival of these patients, retrospective reclassification, especially in cases which may not have been previously graded or staged, may influence the choice of therapeutic options, even in the future.
References
B.I. Gustafsson, M. Kidd, I.M. Modlin, Neuroendocrine tumors of the diffuse neuroendocrine system. Curr. Opin. Oncol. 20, 1–12 (2008)
I.M. Modlin, K. Oberg, D.C. Chung, R.T. Jensen, W.W. de Herder, R.V. Thakker, M. Caplin, G. Delle Fave, G.A. Kaltsas, E.P. Krenning, S.F. Moss, O. Nilsson, G. Rindi, R. Salazar, P. Ruszniewski, A. Sundin, Gastroenteropancreatic neuroendocrine tumours. Lancet Oncol. 9, 61–72 (2008)
C. Capella, E. Solcia, L.H. Sobin, in Pathology and genetics of tumours of the digestive system, ed. by S.R. Hamilton, L.A. Aaltonen (IARC Press, Lyon, 2000), pp. 77–82
G. Rindi, G. Klöppel, H. Alhman, M. Caplin, A. Couvelard, W.W. de Herder, B. Erikssson, A. Falchetti, M. Falconi, P. Komminoth, M. Körner, J.M. Lopes, A.M. McNicol, O. Nilsson, A. Perren, A. Scarpa, J.Y. Scoazec, B. Wiedenmann, all other Frascati Consensus Conference participants, European Neuroendocrine Tumor Society (ENETS), TNM staging of foregut (neuro)endocrine tumors: a consensus proposal including a grading system. Virchows Arch. 449, 395–401 (2006)
G. Rindi, G. Klöppel, A. Couvelard, P. Komminoth, M. Körner, J.M. Lopes, A.M. McNicol, O. Nilsson, A. Perren, A. Scarpa, J.Y. Scoazec, B. Wiedenmann, TNM staging of midgut and hindgut (neuro) endocrine tumors: a consensus proposal including a grading system. Virchows Arch. 451, 757–762 (2007)
F.T. Bosman, F. Carneiro, R.H. Hruban, N.D. Theise (eds.), WHO classification of tumours of the digestive system (IARC Press, Lyon, 2010), pp. 13–14
L. Sobin, M. Gospodarowicz, C. Wittekind (eds.), UICC/AJCC TNM classification of malignant tumours, 7th edn. (Wiley, New York, 2009)
U.F. Pape, H. Jann, J. Mueller-Nordhorn, A. Bockelbrink, U. Berndt, S.N. Willich, M. Koch, C. Röcken, G. Rindi, B. Wiedenmann, Prognostic relevance of a novel TNM classification system for upper gastroenteropancreatic neuroendocrine tumors. Cancer 113, 256–265 (2008)
H. Jann, S. Roll, A. Couvelard, O. Hentic, M. Pavel, J. Mueller-Nordhorn, M. Koch, C. Roecken, G. Rindi, P. Ruszniewski, B. Wiedenmann, U.F. Pape, Neuroendocrine tumors of midgut and hindgut origin: tumor-node-metastasis classification determines clinical outcome. Cancer 117, 3332–3341 (2011)
J. Strosberg, A. Nasir, D. Coppola, M. Wick, L. Kvols, Correlation between grade and prognosis in metastatic gastroenteropancreatic neuroendocrine tumors. Human Pathol. 40, 1262–1268 (2009)
J.C. Yao, M.H. Shah, T. Ito, C.L. Bohas, E.M. Wolin, Cutsem E. Van, T.J. Hobday, T. Okusaka, J. Capdevila, E.G. de Vries, P. Tomassetti, M.E. Pavel, S. Hoosen, T. Haas, J. Lincy, D. Lebwohl, K. Öberg, RAD001 in Advanced Neuroendocrine Tumors, Third Trial (RADIANT-3) Study Group, Everolimus for advanced pancreatic neuroendocrine tumors. N. Engl. J. Med. 10(364), 514–523 (2011)
F. Grillo, S. Pigozzi, P. Ceriolo, P. Calamaro, R. Fiocca, L. Mastracci, Factors affecting immunoreactivity in long-term storage of formalin-fixed paraffin-embedded tissue sections. Histochem. Cell Biol. 144(1), 93–99 (2015)
V. Adsay, Ki67 labeling index in neuroendocrine tumors of the gastrointestinal and pancreatobiliary tract: to count or not to count is not the question, but rather how to count. Am. J. Surg. Pathol. 36, 1743–1746 (2012)
M.D. Reid, P. Bagci, N. Ohike, B. Saka, I. Erbarut Seven, N. Dursun, S. Balci, H. Gucer, K.T. Jang, T. Tajiri, O. Basturk, S.Y. Kong, M. Goodman, G. Akkas, V. Adsay, Calculation of the Ki67 index in pancreatic neuroendocrine tumors: a comparative analysis of four counting methodologies. Modern Pathol. 28, 686–694 (2015)
O. Basturk, Z. Yang, L.H. Tang, R.H. Hruban, V. Adsay, C.M. McCall, A.M. Krasinskas, K.T. Jang, W.L. Frankel, S. Balci, C. Sigel, D.S. Klimstra, The high-grade (WHO G3) pancreatic neuroendocrine tumor category is morphologically and biologically heterogenous and includes both well differentiated and poorly differentiated neoplasms. Am. J. Surg. Pathol. 39, 683–690 (2015)
E. Raymond, L. Dahan, J.L. Raoul, Y.J. Bang, I. Borbath, C. Lombard-Bohas, J. Valle, P. Metrakos, D. Smith, A. Vinik, J.S. Chen, D. Hörsch, P. Hammel, B. Wiedenmann, E. Van Cutsem, S. Patyna, D.R. Lu, C. Blanckmeister, R. Chao, P. Ruszniewski, Sunitinib malate for the treatment of pancreatic neuroendocrine tumors. N. Engl. J. Med. 10(364), 501–513 (2011)
J.R. Strosberg, R.L. Fine, J. Choi, A. Nasir, D. Coppola, D.T. Chen, J. Helm, L. Kvols, First-line chemotherapy with capecitabine and temozolomide in patients with metastatic pancreatic endocrine carcinomas. Cancer 15(117), 268–275 (2011)
K. Öberg, U. Knigge, D. Kwekkeboom, A. Perren, ESMO Guidelines Working Group, Neuroendocrine gastro-entero-pancreatic tumors: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 23 Suppl 7, vii124–vii130 (2012)
Acknowledgments
This work was supported by a University of Genoa Research Grant 2011 awarded to Dr. Grillo.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they do not have any conflicts of interest.
Additional information
Federica Grillo and Manuela Albertelli have contributed equally.
Rights and permissions
About this article
Cite this article
Grillo, F., Albertelli, M., Annunziata, F. et al. Twenty years of gastroenteropancreatic neuroendocrine tumors: is reclassification worthwhile and feasible?. Endocrine 53, 58–62 (2016). https://doi.org/10.1007/s12020-015-0734-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-015-0734-3