Abstract
Various factors influence quality of life (QoL) in acromegaly. Whether disease control and treatment approach are related to QoL is still a matter of debate. The aim of the present study was to evaluate QoL in patients with acromegaly using the disease-specific Acromegaly Quality of Life Questionnaire in respect to disease activity, treatment modalities, and other factors. We studied 212 patients with acromegaly in a cross-sectional manner over a 6-year period in a single tertiary center. As a second step, seventy of the patients who were with active disease at baseline were followed up prospectively and 45 of them were in remission at re-evaluation. In regard to the cross-sectional group, active acromegaly independently predicted worse appearance scores. Prior radiotherapy and older age were independent negative predictors of all scales. Female gender negatively predicted all scales except the appearance domain. Longer duration of remission predicted worse personal relations scores in biochemically controlled patients. The use of somatostatin analog (SSA) was associated with worse personal relations scores, while higher IGF-1 index predicted worse appearance scores in patients with active acromegaly. In the prospective group, achievement of remission independently predicted improvement of the total scale. Lower corresponding baseline scores predicted improvement of the total, physical, and appearance scales, while the absence of hypopituitarism independently predicted improvement of the appearance scale. The use of SSA was associated with improvement of the total and appearance scores. In conclusion, QoL is a multifactorial issue that needs an individualized approach for detection and management.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acromegaly is a rare chronic disorder caused by pituitary adenoma in almost all cases. It manifests with facial and acral deformity and multiple systemic complications that lead to increased cardiovascular, respiratory, and neoplastic mortalities [1]. Apart from the physical changes, patients with acromegaly show some psychosocial alterations resulting altogether in decreased self-perception of well-being [2]. Achievement of disease control is expected to restore life expectancy to levels similar to the general population [1]. However, it is still debatable whether normalization of GH and IGF-1 levels is related to better quality of life (QoL) [3–11]. It seems that other factors, such as treatment approach, concomitant co-morbidities, disease duration, or even physical activity, could affect QoL [6, 7, 12–17].
The aim of the current study was to evaluate QoL in patients with acromegaly in a cross-sectional and prospective manner and assess the influence of biochemical disease control and treatment approach. We used Acromegaly Quality of Life (AcroQoL) Questionnaire—a disease-specific tool that has been developed by Webb and co-workers [18]. The questionnaire has shown a good consistency with generic tools and was successfully integrated in the clinical practice [3].
Patients and methods
Patients
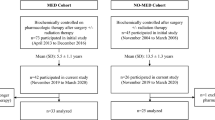
The study was performed in two stages. The first part was carried out in a cross-sectional manner—we investigated 212 patients with acromegaly at the Clinical Center of Endocrinology of the Medical University – Sofia, Bulgaria over a 6-year period of time (July 2007–July 2013). The study was approved by the local Ethic Committee. Exclusion criteria were severe cardiac disease, malignancies, documented psychiatric disorder, pregnancy, or lactation. All patients were older than 18 years. One hundred subjects had active acromegaly (26 of them were naïve), while the other 112 were biochemically controlled. Disease control was defined by basal GH < 2.5 μg/l and/or nadir of GH after OGTT < 1 μg/l and IGF-1 values within normal age-adjusted ranges [19]. Patients not conforming to these criteria were regarded as not controlled. The second stage was prospective follow-up of 70 patients who had active disease at baseline. They were re-evaluated during their regular follow-up stay at the hospital, and they were included in the study after being in remission for at least 6 months or after being treated for at least 6 months in the cases with uncontrolled disease. Sixteen patients were treatment naïve at baseline, of them 10 were operated, 4 were operated and received adjuvant SSA therapy, one was operated and received combination therapy with DA and SSA, and one received DA. One patient on primary DA therapy switched to SSA therapy. In the rest of the patients, the pharmacological therapy was adjuvant to surgery and/or radiotherapy: one was re-operated; 20 switched from DA to SSA therapy, 5 received DA; 7 received SSA; 5 on DA at baseline received combination therapy with SSA and DA; 8 had increase in the dose of DA or switched from Bromocriptine to Cabergoline; 4 on DA received SSA, followed by addition of Pegvisomant; 2 on SSA received Pegvisomant in addition; and in one patient, the dose of Pegvisomant was increased, one patient discontinued the DA therapy due to the effect of radiotherapy. Patients on Pegvisomant in combination with SSA were not included in the analysis of SSA influence on QoL. By July 2013, we had 45 patients with both safe GH values and IGF-1 values below the upper limit of age-adjusted reference ranges and 25 with persistent disease activity at re-evaluation.
Hypopituitarism (deficiency of at least one anterior pituitary axis) was defined as low levels of one or more anterior pituitary hormones as well as decreased hormonal production of the relevant peripheral endocrine glands or the presence of substitution therapy. There were no new anterior pituitary deficiencies at re-evaluation.
Questionnaire
We used the AcroQoL questionnaire developed by Webb et al. [18] after cultural and linguistic adaptation in Bulgarian and approval from the original authors. It comprises of 22 questions divided into two scales—physical (PhS) (8 items) and psychological (PsS) (14 items). The psychological domain is further subdivided into two subscales—personal relations (PrS) and appearance (AS), each of them consisting of 7 items. Each item is scored in a 1–5 Likert scale as the maximum score is 110 (100 %), corresponding to best QoL, while the minimum score is 22 (0 %), corresponding to worse QoL.
Hormonal assays
Serum GH concentration was determined by a solid-phase two-site fluorometric assay based on a direct sandwich technique with two monoclonal antibodies directed against two different epitopes of the human GH molecule (Delfia; Perkin Elmer Life and Analytical Sciences, Wallac Oy, Finland). The sensitivity of this assay was <0.03 mIU/l. The intra- and interassay coefficients of variation were 3.9 and 5.0 %, respectively. We used conversion factor 3 for transformation in mass units [20].
Serum IGF-1 was measured with an immunoradiometric assay after acid–alcohol extraction (Immunotech; Beckman Coulter Co., France). Analytical sensitivity was <0.26 nmol/L. The intra- and interassay coefficients of variation were 6.3 and 6.8 %, respectively.
We used IGF-1 index (the ratio between the current IGF-1 value and the upper limit of normal for the corresponding age) to assess the influence of IGF-1 on QoL.
Statistics
Values are presented as mean ± SD (median; min–max) for continuous variables and as numbers (percentage) for categorical data. Normality of data distribution was evaluated by Kolmogorov–Smirnov’s test. Parametric Students’ t test was used to compare continuous data with normal distribution and non-parametric Mann–Whitney test to compare data with distribution that was not normal. We used the χ square method to analyze categorical data. Comparison between more than two groups was performed by ANOVA analysis. The influence of different factors on AcroQoL scores was assessed by linear regression in the cross-sectional group. We used logistic regression analyses to find factors predicting the presence or lack of improvement in the scores of the prospective group of patients. Significance level was set up at p < 0.05. All statistical analyses were performed by SPSS for Windows version 17.0 (SPSS, Inc.).
Results
Clinical and biochemical characteristics of acromegaly patients with active and controlled disease are presented in Table 1.
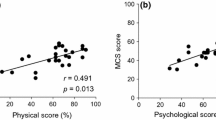
We have compared AcroQoL scores between genders in relation to the disease activity. There was no significant difference between scores of active and controlled patients of both genders. In patients with active disease, women had significantly lower scores of all scales compared to men, corresponding to lower QoL (Fig. 1 ).
In order to find factors with independent influence on the AcroQoL scores, we performed a linear regression analysis. In uncontrolled patients, after age and sex adjustment, the number of surgical interventions was associated with worse total score (TS) B = −6.9, p = 0.029; appearance score (AS) B = −7.7, p = 0.017; personal relations score (PrS) B = −8.3, p = 0.021; and psychological score (PsS) B = −8.0, p = 0.013. We performed a multivariate analysis including the following variables: age, gender, disease control, IGF-1 index (in the subgroups of active and controlled patients), GH value (in the subgroups of active and controlled patients), duration of active disease since diagnosis (duration of remission in the controlled group), prior radiotherapy, number of surgeries (1 or ≥2), dopamine agonist (DA) treatment, and somatostatin analog (SSA) treatment. Only variables with significant influence or borderline significance are shown in Table 2. In the model with IGF-1 index and GH, only IGF-1 index showed a borderline inverse influence on the appearance score—B = −3.98, p = 0.073. Arterial hypertension and diabetes mellitus were not included in the model as they did not show significant influence on either of the scores in a univariate analysis.
Seventy patients were studied prospectively. All of them were with active disease at baseline, while at re-evaluation, 45 were in remission for at least 6 months. Females were 31 (68.9) versus 17 (68 %), p = 1.0 in the controlled and uncontrolled group, respectively. There was no significant difference at baseline between controlled and active patients in respect to age, GH values, IGF-1 index, time since diagnosis, number of patients with at least one anterior pituitary deficiency, number of surgical interventions, number of irradiated patients, number of patients under DA, SSA, combination of both drugs, or growth hormone receptor antagonist (GHRA) treatment. There was no significant difference in baseline scores of all scales as well. Clinical and biochemical characteristics at re-evaluation are presented in Table 3.
The mean individual change of scores (the difference between the scores at re-evaluation and baseline) was higher in controlled versus uncontrolled patients without reaching significance (Table 4).
We differentiated four groups in respect to the last treatment: operated patients without adjuvant pharmacological therapy, patients under DA therapy, subjects on SSA therapy, and treatment with the GHRA Pegvisomant. The mean individual change of scores was positive in operated patients and those under treatment with SSA, while patients under DA and Pegvisomant treatment had negative mean change of scores (Table 5). These observations, however, did not reach statistical significance. One patient was not included in any of the groups as remission was achieved due to radiotherapy. There was no significant difference between groups in respect to gender distribution, number of patients who reached remission, and IGF-1 index change. There was a significant difference in age (46.9 ± 10.0 vs. 57.6 ± 9.1 vs. 50.8 ± 11.4 vs. 43.0 ± 10.4, p = 0.017); time since diagnosis (2.9 ± 2.0 vs. 16.4 ± 8.4 vs. 12.6 ± 8.4 vs. 17.3 ± 7.8, p < 0.001) for surgery, DA, SSA, and Pegvisomant groups, respectively, and a trend toward a significant difference in the number of patients with hypopituitarism 0 versus 4 (28.6) versus 13 (35.1) versus 3 (42.9 %), p = 0.076 and prior radiotherapy 0 versus 5 (35.7) versus 12 (32.4) versus 1 (14.3), p = 0.09.
In logistic regression analysis after adjustment for age, achievement of remission, time since diagnosis, prior radiotherapy, the presence of hypopituitarism, and corresponding baseline score, treatment with SSA was a significant predictor of total score improvement OR 3.14 (95 % CI 1.035–9.515), p = 0.043 and appearance score improvement OR 4.16 (95 % CI 1.29–13.44), p = 0.017. After adjustment for the same variables, DA therapy or surgery without adjuvant medical therapy did not have significant influence on improvement of any of the scores. We performed a multivariate logistic regression analysis including all variables: age, gender, achievement of remission, corresponding baseline scores, time since diagnosis, radiotherapy, surgery as last treatment, application of DA, and application of SSA. Achievement of remission showed a tendency for improvement of the total score—OR 3.08 (0.94–10.1); p = 0.062. Table 6 shows the results after exclusion of 3 patients with IGF-1 values below the age-adjusted reference range where achievement of remission significantly predicted improvement of the total score OR 4.09 (1.17–14.2), p = 0.026. Variables without significant influence are not shown in the table. Normalization of either IGF-1 or GH was not significant predictor of improvement in either of the scores when these markers were used instead of achievement of remission in the model.
Discussion
Literature data concerning the association of QoL with biochemical disease control in subjects with acromegaly are controversial. A series of studies failed to show better AcroQoL scores in controlled versus uncontrolled patients [4–7]. Moreover, some teams reported even significantly higher scores in active versus controlled patients [10, 11]. Similar tendency was observed in male patients in our study, however, without reaching significance. On the contrary, other surveys showed better total, physical and PrS [8], or appearance score [9] in controlled versus uncontrolled patients. Furthermore, a number of longitudinal studies demonstrated improvement of QoL after treatment [3, 10, 13, 15, 21]. We also found higher, although non-significant, mean change of scores in controlled versus uncontrolled patients in our prospective group (Table 4). The difference between our study and the other published longitudinal surveys could be explained with the different baseline characteristics and combination of other factors influencing QoL in our patients.
Divergent results in regard to the correlation between biochemical parameters and QoL have been reported. Most cross-sectional [4, 5, 7, 22] or prospective studies [3, 10, 13, 15] do not show significant correlation between IGF-1/GH and AcroQoL scores. However, other research groups found a negative correlation between some scores and IGF-1 values [8, 9, 21]. Multivariate regression analysis demonstrated that the lack of disease control independently predicted worse appearance subscale with a trend toward worse psychological scale in our cross-sectional group. Higher IGF-1 levels tend to remain a predictor of worse appearance subscale in a model with IGF-1 index and GH values. It seems that it is not without significance how “active” a patient is as lower IGF-1 values predicted better appearance score in our active patients (Table 2). Active acromegaly is associated with soft tissue swelling, which could possibly explain the strongest influence of IGF-1 on the appearance scale in our study.
In regard to our prospective study, the logistic regression analysis demonstrated that achievement of remission independently predicted global AcroQoL score improvement after exclusion of three patients with IGF-1 values below the lower age-adjusted reference level—OR 0.24 (0.07–0.85), p = 0.026 (Table 6). The impact of GH deficiency may be suggested as a possible explanation of this phenomenon which raises questions about aggressiveness of treatment in responders to the therapy and needs further investigation. As a whole, the comparative analyses could not show the role of the disease control on AcroQoL in a deliberate manner, which became evident only after regression analyses. The most reasonable explanation is the influence of other factors in addition to the biochemical markers.
Another factor related to QoL is disease duration. Longer duration of disease remission was related to worse PrS, with a tendency for worse total and psychological subscale scores (Table 2). Our results suggest that QoL progressively decreases with time despite biochemical control and independently from age probably due to the presence of irreversible changes. These results are not surprising, as even in remission, acromegaly is referred to as a chronic disease requiring regular follow-up and continuous medication use in most of the cases, which inevitably influences the self-perception of well-being. Similar relationship between PrS and disease duration was reported in several surveys [4, 7, 22].
In terms of therapeutic options, we demonstrated that radiotherapy had a serious negative impact on AcroQoL scores (Table 2). Radiotherapy was associated with worse QoL in a number of studies [5, 11, 16, 23]. Various explanations have been proposed. It could cause long-term neurocognitive dysfunction [24]. On the other hand, radiotherapy is usually applied in patients with aggressive course of disease, where surgical and pharmacological treatment options have been inefficient in establishing biochemical control. The subsequent long-term hormonal hypersecretion could be responsible for a higher degree of irreversible changes, especially in patients’ appearance and musculoskeletal system, possibly resulting in worse QoL [4, 23, 25]. Moreover, radiotherapy causes progressive increase in the proportion of patients with hypopituitarism, as well as in the number of deficient pituitary axes [26]. The lack of anterior pituitary deficiency predicted improvement of the appearance domain and had influence of borderline significance on the total score improvement in our prospective group (Table 6). Negative impact of hypopituitarism was shown on psychological and PrS by T’Sjoen et al.; however, no association was found by other research groups [4, 5, 9, 11, 22].
The impact of surgical and pharmacological treatment on QoL has been assessed by AcroQoL in several studies. No superiority of surgery over medical or other treatment modalities was demonstrated in some of them [4, 11, 15]. On the contrary, Matta et al. reported better appearance scores of uncontrolled surgically treated compared to medically treated patients [9]. We showed in a univariate regression analysis that the number of surgical interventions negatively influenced all scores, except the physical one. This observation, in analogy to radiotherapy, could possibly reflect the presence of more aggressive disease with more irrepairable damage due to longer hormonal hypersecretion.
In theory, the type of pharmacological therapy could also influence HRQoL, although the literature data are controversial. Some studies revealed that patients under SSA therapy were characterized by worse QoL despite achievement of remission [6, 14]. A possible explanation could be found in the theory of the so-called extra-hepatic acromegaly: persistence of GH over-expression in the extra-hepatic tissues in some SSA-treated patients in spite of the normalization of their serum IGF-1 levels [27]. In contrast, Mangupli et al. [15] showed improvement of the global AcroQoL score after application of Sandostatin LAR. Biermasz et al. found no significant difference between scores of patients with and without treatment with SSAs [4]. The application of Sandostatin LAR was related to worse PrS with a trend toward worse psychological and total scores only in uncontrolled but not in controlled patients from our cross-sectional group (Table 2). However, the application of SSA after adjustment for numerous variables predicted improvement of the total scale—OR 3.14 (95 % CI 1.035–9.515), p = 0.043 and the appearance scale OR 4.16 (95 % CI 1.29–13.44), p = 0.017 in our prospective group. We should discriminate between a momentary QoL, in the case of a cross-sectional study, and its change with time induced by various factors. Negative influence of SSA therapy on momentary QoL does not exclude the possibility of individual improvement from baseline at re-evaluation. Such discordance could also be explained by different combinations of baseline factors influencing QoL. When speculating over these results, we should take into consideration that we used the first logistic regression model to show the influence of SSA separately from the other treatment groups. However, the predictive role of their use was lost in the second model which included SSA treatment along with DA therapy and surgery. We could suggest that either SSA treatment does not have superiority over the other two approaches, or that the sensitivity of the model is compromised by the lower number of patients under DA therapy or surgery alone at the time of the last visit.
We should also take into consideration some other factors which were strongly related to AcroQoL scores in our study. Men with active disease had significantly better scores of all scales compared to women in the cross-sectional group (Fig. 1). Female gender was found to be a negative independent predictor of QoL, especially in uncontrolled patients (Table 2). According to published data, men had better AcroQoL scores in several studies [3, 7, 22] but not in others [4, 5, 11]. An interesting observation of Psaras et al. was that concomitant diseases had different impact on males and females’ QoL in acromegaly [28]. Generally, there could be sex differences in disease perception and response to therapy [29], and further studies could probably shed more light on the issue.
Another significant factor influencing subjective perception of health was age. Older age predicted worse AcroQoL scores of all scales, except for the appearance score in controlled patients (Table 2). Negative influence of age on the appearance subscale has been reported [4], while no relation using AcroQoL has been found in other studies [3, 5, 7, 11, 22]. Age had borderline significance as a predictor of physical scale improvement from baseline in our prospective group (Table 6). Interestingly, baseline scores were negative predictors of improvement of the global, physical, and appearance scores, suggesting that patients with very good QoL are less likely to improve with time.
Our survey raises some issues that need further research. It would be interesting to study in more detail the factors behind the gender differences and gender-induced response to different treatment modalities. Probably such clues would be useful for elaborating sex-differentiated approach for improvement of QoL. Other studies have already shown that growth hormone deficiency in patients with cured acromegaly is associated with lower subjective perception of health [30]. However, patients on medical treatment are not evaluated with stimulation tests, and little is known about the effect of medical “over-treatment” on QoL. Another issue that arise questions is the negative relation between baseline scores and probability of improvement. Is the worsening of high baseline QoL really inevitable with time?
In conclusion, our study, which was based on a sample size large enough to ensure adequate power, confirmed the independent role of biochemical disease control for better appearance scale and improvement from baseline in the global scale, using AcroQoL. In addition, other independent factors, such as older age, prior irradiation, and female gender, showed negative influence on various scales of AcroQoL. Although application of SSA was related to worse QoL in the uncontrolled patients from the cross-sectional group, there was evidence for improvement from baseline at re-evaluation. Another interesting finding was the negative correlation between QoL and duration of remission in our patients. Given all our results, it seems that all factors are closely interrelated, which makes QoL a complex issue requiring individualized assessment.
References
O.M. Dekkers, N.R. Biermasz, A.M. Pereira, J.A. Romijn, J.P. Vandenbroucke, Mortality in acromegaly: a metaanalysis. J. Clin. Endocrinol. Metab. 93(1), 61–67 (2008). doi:10.1210/jc.2007-1191
A. Santos, E. Resmini, M.A. Martinez, C. Marti, J. Ybarra, S.M. Webb, Quality of life in patients with pituitary tumors. Curr. Opin. Endocrinol. Diabetes Obes. 16(4), 299–303 (2009). doi:10.1097/MED.0b013e32832cdec9
S.M. Webb, X. Badia, N.L. Surinach, Validity and clinical applicability of the acromegaly quality of life questionnaire, AcroQoL: a 6-month prospective study. Eur. J. Endocrinol. 155(2), 269–277 (2006). doi:10.1530/eje.1.02214
N.R. Biermasz, S.W. van Thiel, A.M. Pereira, H.C. Hoftijzer, A.M. van Hemert, J.W. Smit, J.A. Romijn, F. Roelfsema, Decreased quality of life in patients with acromegaly despite long-term cure of growth hormone excess. J. Clin. Endocrinol. Metab. 89(11), 5369–5376 (2004). doi:10.1210/jc.2004-0669
S.V. Rowles, L. Prieto, X. Badia, S.M. Shalet, S.M. Webb, P.J. Trainer, Quality of life (QOL) in patients with acromegaly is severely impaired: use of a novel measure of QOL: acromegaly quality of life questionnaire. J. Clin. Endocrinol. Metab. 90(6), 3337–3341 (2005). doi:10.1210/jc.2004-1565
S.C. Hua, Y.H. Yan, T.C. Chang, Associations of remission status and lanreotide treatment with quality of life in patients with treated acromegaly. Eur. J. Endocrinol. 155(6), 831–837 (2006). doi:10.1530/eje.1.02292
G. T’Sjoen, M. Bex, D. Maiter, B. Velkeniers, R. Abs, Health-related quality of life in acromegalic subjects: data from AcroBel, the Belgian registry on acromegaly. Eur. J. Endocrinol. 157(4), 411–417 (2007). doi:10.1530/EJE-07-0356
R. Trepp, R. Everts, C. Stettler, S. Fischli, S. Allemann, S.M. Webb, E.R. Christ, Assessment of quality of life in patients with uncontrolled vs. controlled acromegaly using the Acromegaly Quality of Life questionnaire (AcroQoL). Clin. Endocrinol. (Oxf) 63(1), 103–110 (2005). doi:10.1111/j.1365-2265.2005.02307.x
M.P. Matta, E. Couture, L. Cazals, D. Vezzosi, A. Bennet, P. Caron, Impaired quality of life of patients with acromegaly: control of GH/IGF-I excess improves psychological subscale appearance. Eur. J. Endocrinol. 158(3), 305–310 (2008). doi:10.1530/EJE-07-0697
C. Sardella, M. Lombardi, G. Rossi, C. Cosci, S. Brogioni, I. Scattina, S.M. Webb, M. Gasperi, E. Martino, F. Bogazzi, Short- and long-term changes of quality of life in patients with acromegaly: results from a prospective study. J. Endocrinol. Invest. 33(1), 20–25 (2010)
H. Kepicoglu, E. Hatipoglu, I. Bulut, E. Darici, N. Hizli, P. Kadioglu, Impact of treatment satisfaction on quality of life of patients with acromegaly. Pituitary (2013). doi:10.1007/s11102-013-0544-7
N.R. Biermasz, A.M. Pereira, J.W. Smit, J.A. Romijn, F. Roelfsema, Morbidity after long-term remission for acromegaly: persisting joint-related complaints cause reduced quality of life. J. Clin. Endocrinol. Metab. 90(5), 2731–2739 (2005). doi:10.1210/jc.2004-2297
S.J. Neggers, M.O. van Aken, W.W. de Herder, R.A. Feelders, J.A. Janssen, X. Badia, S.M. Webb, A.J. van der Lely, Quality of life in acromegalic patients during long-term somatostatin analog treatment with and without pegvisomant. J. Clin. Endocrinol. Metab. 93(10), 3853–3859 (2008). doi:10.1210/jc.2008-0669
M.R. Postma, R.T. Netea-Maier, G. van den Berg, J. Homan, W.J. Sluiter, M.A. Wagenmakers, A.C. van den Bergh, B.H. Wolffenbuttel, A.R. Hermus, A.P. van Beek, Quality of life is impaired in association with the need for prolonged postoperative therapy by somatostatin analogs in patients with acromegaly. Eur. J. Endocrinol. 166(4), 585–592 (2012). doi:10.1530/EJE-11-0853
R. Mangupli, P. Camperos, S.M. Webb, Biochemical and quality of life responses to octreotide-LAR in acromegaly. Pituitary (2013). doi:10.1007/s11102-013-0533-x
A.A. van der Klaauw, N.R. Biermasz, H.C. Hoftijzer, A.M. Pereira, J.A. Romijn, Previous radiotherapy negatively influences quality of life during 4 years of follow-up in patients cured from acromegaly. Clin. Endocrinol. (Oxf) 69(1), 123–128 (2008). doi:10.1111/j.1365-2265.2007.03169.x
E. Hatipoglu, N. Topsakal, O.E. Atilgan, N. Alcalar, A.F. Camliguney, M. Niyazoglu, H.B. Cotuk, P. Kadioglu, Impact of exercise on quality of life and body-self perception of patients with acromegaly. Pituitary 17(1), 38–43 (2014). doi:10.1007/s11102-013-0463-7
S.M. Webb, L. Prieto, X. Badia, M. Albareda, M. Catala, S. Gaztambide, T. Lucas, C. Paramo, A. Pico, A. Lucas, I. Halperin, G. Obiols, R. Astorga, Acromegaly Quality of Life Questionnaire (ACROQOL) a new health-related quality of life questionnaire for patients with acromegaly: development and psychometric properties. Clin. Endocrinol. (Oxf) 57(2), 251–258 (2002)
A. Giustina, A. Barkan, F.F. Casanueva, F. Cavagnini, L. Frohman, K. Ho, J. Veldhuis, J. Wass, K. Von Werder, S. Melmed, Criteria for cure of acromegaly: a consensus statement. J. Clin. Endocrinol. Metab. 85(2), 526–529 (2000)
M.C. Sheppard, Growth hormone assay standardization: an important clinical advance. Clin. Endocrinol. (Oxf) 66(2), 157–161 (2007). doi:10.1111/j.1365-2265.2007.02703.x
A.N. Paisley, S.V. Rowles, M.E. Roberts, S.M. Webb, X. Badia, L. Prieto, S.M. Shalet, P.J. Trainer, Treatment of acromegaly improves quality of life, measured by AcroQol. Clin. Endocrinol. (Oxf) 67(3), 358–362 (2007). doi:10.1111/j.1365-2265.2007.02891.x
P. Anagnostis, Z.A. Efstathiadou, M. Charizopoulou, D. Selalmatzidou, E. Karathanasi, M. Poulasouchidou, M. Kita, Psychological profile and quality of life in patients with acromegaly in Greece. Is there any difference with other chronic diseases? Endocrine (2014). doi:10.1007/s12020-014-0166-5
M.J. Wassenaar, N.R. Biermasz, M. Kloppenburg, A.A. van der Klaauw, J. Tiemensma, J.W. Smit, A.M. Pereira, F. Roelfsema, H.M. Kroon, J.A. Romijn, Clinical osteoarthritis predicts physical and psychological QoL in acromegaly patients. Growth Horm IGF Res. 20(3), 226–233 (2010). doi:10.1016/j.ghir.2010.02.003
B.J. Spiegler, E. Bouffet, M.L. Greenberg, J.T. Rutka, D.J. Mabbott, Change in neurocognitive functioning after treatment with cranial radiation in childhood. J. Clin. Oncol. 22(4), 706–713 (2004). doi:10.1200/JCO.2004.05.186
A. Miller, H. Doll, J. David, J. Wass, Impact of musculoskeletal disease on quality of life in long-standing acromegaly. Eur. J. Endocrinol. 158(5), 587–593 (2008). doi:10.1530/EJE-07-0838
P.J. Jenkins, P. Bates, M.N. Carson, P.M. Stewart, J.A. Wass, Conventional pituitary irradiation is effective in lowering serum growth hormone and insulin-like growth factor-I in patients with acromegaly. J. Clin. Endocrinol. Metab. 91(4), 1239–1245 (2006). doi:10.1210/jc.2005-1616
S.J. Neggers, J.J. Kopchick, J.O. Jorgensen, A.J. van der Lely, Hypothesis: extra-hepatic acromegaly: a new paradigm? Eur. J. Endocrinol. 164(1), 11–16 (2011). doi:10.1530/EJE-10-0969
T. Psaras, J. Honegger, B. Gallwitz, M. Milian, Are there gender-specific differences concerning quality of life in treated acromegalic patients? Exp. Clin. Endocrinol. Diabetes 119(5), 300–305 (2011). doi:10.1055/s-0030-1267912
A.P. Arnold, Promoting the understanding of sex differences to enhance equity and excellence in biomedical science. Biol. Sex Differ. 1(1), 1 (2010). doi:10.1186/2042-6410-1-1
T. Wexler, L. Gunnell, Z. Omer, K. Kuhlthau, C. Beauregard, G. Graham, A.L. Utz, B. Biller, L. Nachtigall, J. Loeffler, B. Swearingen, A. Klibanski, K.K. Miller, Growth hormone deficiency is associated with decreased quality of life in patients with prior acromegaly. J. Clin. Endocrinol. Metab. 94(7), 2471–2477 (2009). doi:10.1210/jc.2008-2671
Acknowledgments
This work has been supported by the National Science Fund, Ministry of Education, Youth and Science, Grant No. DO02-356/31.12.2008.
Conflict of interest
The authors declare that there is no conflict of interest that would prejudice the impartiality of the reported scientific work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vandeva, S., Yaneva, M., Natchev, E. et al. Disease control and treatment modalities have impact on quality of life in acromegaly evaluated by Acromegaly Quality of Life (AcroQoL) Questionnaire. Endocrine 49, 774–782 (2015). https://doi.org/10.1007/s12020-014-0521-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-014-0521-6