Abstract
It is well established that both estrogen loss and type II diabetes mellitus (DMII) can impair bone metabolism, but whether estrogen loss exacerbates the effects of DMII is unclear. Therefore, we determined if ovariectomy (OVX) of rats on a long-term high-fat/sugar diet and injection of a low dose of streptozotocin (DMII) decreased bone mineral density (BMD) more than OVX or DMII alone. Bone insulin signaling is known to support bone metabolism; therefore, we also tested the hypothesis that OVX DMII rats (DOVX) would exhibit greater reductions in the expression of proteins important in insulin signaling, including IRS-1, IRS-2, and IGF-1. As hypothesized, BMD and plasma estrogen levels were decreased more in DOVX rats than in rats following OVX (NOVX) or DMII (DS) alone. IGF-1 expression was decreased in the liver, kidney, skeletal muscle, and bone of DOVX, DS, and NOVX rats; however, the decrease was larger and occurred sooner in DOVX rats. While IRS-1 and IRS-2 decreased in most groups in all tissues examined, the expression patterns differed in both a group- and tissue-dependent fashion. In conclusion, these data demonstrate that estrogen loss and DMII induced by a high-fat/sugar diet interact to produce osteoporosis and support the hypothesis that the bone loss may be mediated at least in part by concurrent decreases in the insulin signaling proteins in bone.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Type II diabetes mellitus (DMII) is due to impaired signaling secondary to the binding of insulin to its receptor. As a result, insulin-induced increases in the activation of signaling proteins, such as insulin receptor substrate (IRS)-1 and IRS-2, are attenuated in many tissues, including liver, skeletal muscle, kidney, and bone [1–4]. Thus, DMII can induce several serious consequences, in particular, osteoporosis [5–7]. Indeed, diabetes and osteoporosis are common and complex disorders that can be often associated especially in the middle-aged and elderly population, posing enormous financial burden on individuals and society as a whole. More concerning is that the prevalence of diabetes and osteoporosis is increasing [8–10].
Estrogen loss is another consequence of aging that also contributes to osteoporosis in both men and women. Interestingly, estrogen loss may increase bone resorption in part via decreases in the bone actions of insulin, and an insulin-related protein, insulin-like growth factor (IGF-1). Importantly, IGF-1 in vitro regulates various types of bone cells, and osteoblasts incubated with IGF-1 demonstrated enhanced differentiation and decreased apoptosis [11–13]. However, whether estrogen loss exacerbates the deleterious effects of DMII on bone via insulin and IGF-1 signaling pathways has not been previously investigated. To test this hypothesis, we determined if bone density was reduced more in ovariectomized (OVX) rats with DMII, due to consumption of a high-fat/sugar diet, than in rats following OVX or DMII alone. We also determined if the decreases in bone density were associated with parallel decreases in bone IRS-1, IRS-2, and IGF-1. To assess whether the interaction of OVX and DMII was specific to bone, we also quantified IRS-1, IRS-2, and IGF-1 in other tissues known to be influenced by insulin action, liver, skeletal muscle, and kidney.
Materials and methods
Experimental animal model
Female Wistar rats (Experimental Animal Center, Hebei Medical University) were studied beginning at 2.5–3 months of age. All experimental procedures were in compliance with the National Institutes of Health Guide for the Care and Use of Laboratory Animals. This study was reviewed and approved by the Institutional Animal Care and Use Committee at Hebei Medical University.
The animals were housed under standard laboratory conditions and maintained under controlled room temperature (22 ± 3 °C) and humidity with a daily cycle of 12 h of light and 12 h of dark. The experimental rats were randomly divided into four groups: normal sham group (NS, n = 24); normal ovariectomy group (NOVX, n = 26); type II diabetes sham group (DS, n = 24); and type II diabetes ovariectomy group (DOVX, n = 26). Rats in NS and NOVX groups were provided with regular diet (Experimental Animal Center, Hebei Medical University), while rats in the DS and DOVX groups were fed a high-sugar/fat diet for 8 weeks (regular diet plus 20 % sugar, 15 % lard, and 2.5 % cholesterol as kcal). After 8 weeks on these diets, DS and DOVX groups received an intraperitoneal injection of a low dose of streptozotocin (STZ; 30 mg/kg; Sigma); rats in the control groups were administered the vehicle (citrate buffer, pH 4.4; 0.25 mL/kg). The purpose of the STZ injection was to mimic later stage DMII, in which pancreatic insulin production becomes impaired. One week later, rats in the NOVX and DOVX groups underwent ovariectomy, while rats in the NS and DS groups were subjected to a sham operation, which was similar to the ovariectomy except that a small portion of abdominal fat was removed. The ovariectomy day was designated as time 0, and the rats were sacrificed 4, 8, and 12 weeks later. At this time, bone mineral density (BMD) of the spine at lumbar levels 3–6 was measured by dual energy X-ray absorptiometry (DEXA, Osteocore 3, France). The liver, skeletal muscle and kidney were individually perfused and collected in 4 % paraformaldehyde for immunohistochemistry. Part of the liver, skeletal muscle, kidney, and bone (femur, tibia, and humerus) were fresh-frozen in liquid nitrogen for RT-PCR.
During the experiment, 4 rats died (1 NS and 3 DS), and 2 in the DOVX group were excluded because the FBG level did not meet the requirement.
Plasma measurements
Venous blood (tail vein) was collected before experimentation to measure fasting concentrations of blood glucose (FBG) (Roach blood glucose instrument). Intraocular angular vein blood (2.5–4 mL) was collected for measurement of fasting plasma insulin (FINS) by radioimmunoassay (3v-diagnostic Bioengineer, Shandong, China) and plasma estrogen by ELISA (Rat Estrogen/E ELISA Kit, 3v-Diagnostic Bioengineer, Shandong, China). The insulin sensitivity index (ISI) was calculated using the formula ln(1/FBG × FINS) [14].
Histology and immunohistochemistry
Paraffin-embedded liver, muscle and renal tissue sections (5-μm thick) were stained with haematoxylin and eosin to document changes in tissue and cell structure. Immunostaining was performed in these paraffin-embedded sections using the streptavidin–peroxidase (SP) method. Briefly, after antigen retrieval, the primary specific antibodies for IGF-1 (Goldbridge Biotechnology, Beijing, China; liver, 1:100; muscle, 1:150; kidney, 1:200), IRS-1 (Biosynthesis Biotechnology, Beijing, China; liver, 1:200; muscle, 1:200; kidney, 1:100), and IRS-2 (Biosynthesis Biotechnology, Beijing, China; liver, 1:100; muscle, 1:150; kidney, 1:150) were applied. In additional sections, the primary antibody was omitted and non-immunized goat serum was used for negative controls. After extensive rinsing, the biotinylated secondary antibody and SP complexes (Bio-high Technology, Hebei, China) were applied. Each section was examined on five randomly selected, optical fields by microscopy (400×).
Quantitation of immunoreactivity: yellow brown granules in the cytoplasm-identified positive cells. The immunohistochemical score (IHS) [15] was defined as the function of the percentage of positive cells and the staining intensity of positive cells as follows: A, the percentage of positive cells (no positive cells = 0, positive cells accounted for 1–10 % = 1, 11–50 % = 2, 51–80 % = 3, 81–100 % = 4); B, staining intensity of positive cells (negative = 0, weak positive = 1, moderately positive = 2, strong positive = 3), A multiplied by B is the IHS score.
Reverse transcriptase-polymerase chain reaction
Total RNA was extracted using TRIZOL (SBS Genetech Co., Ltd. Beijing, China) and was reverse transcribed into cDNA (Promega, USA). The levels of target gene mRNA transcripts determined by the polymerase chain reaction (PCR) using the cDNA as a template and specific primers (Generay Biotech Co., Ltd. Shanghai, China; Table 1). PCR of each sample was performed in duplicate at 94 °C for 5 min, and subjected to repeating cycles of 94 °C for 30 s, annealing for 30 s, and 72 °C for 50 s (MJ, USA). The PCR products were separated using 8 % polyacrylamide gel electrophoresis and analyzed using a bioimaging system (VILBER LOURMAT, France). Expression levels were quantified using Bandscan 5.0 software, normalized to β-actin.
Statistical analysis
All data were subjected to statistical analysis using SPSS 16.0. Data that characterized the DMII model are presented as median and range, and comparisons were performed using non parametric tests. Gene expression levels are expressed as mean ± standard deviation (SD). Statistical analysis was performed using one-way ANOVA. Between group differences were determined using the Newman–Keuls post hoc test. P values <0.05 were considered statistically significant.
Results
Characterization of the model
Compared to the control groups (NS, NOVX), prior to ovariectomy, the rats in the diabetic groups (DS, DOVX) exhibited significant increases in body weight and fasting serum glucose and insulin levels; the ISI was decreased in the diabetic rats (Table 2).
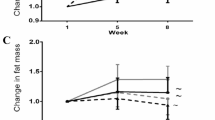
Twelve weeks after ovariectomy or sham ovariectomy, compared to the control groups (NS, NOVX), the rats in the diabetic groups (DS, DOVX) continued to exhibit significant increases in body weight, FBG and FINS; ISI was decreased in the diabetic rats (Table 3). Ovariectomy (NOVX, DOVX) decreased both BMD and estrogen levels compared to control groups (NS, DS). The DS group exhibited decreased bone density at 8 and 12 weeks, and also decreased estrogen level at 12 weeks, compared to the NS group (Fig. 1).
Effect of ovariectomy and a high-fat/sugar diet on bone mineral density (BMD, left 4 weeks, NS: vs NOVX (∆ P = 0.007), vs DOVX (∆ P < 0.001); DS: vs NOVX (*P = 0.021), vs DOVX (*P = 0.014); 8 weeks, NS: vs DS (∆ P = 0.037), vs NOVX (∆ P < 0.001), vs DOVX (∆ P < 0.001); DS: vs NOVX (*P = 0.02), vs DOVX (*P < 0.001); 12 weeks, NS: vs DS (∆ P = 0.022), vs NOVX (∆ P < 0.001), vs DOVX (∆ P < 0.001); DS: vs NOVX (*P = 0.027), vs DOVX (*P = 0.005) and estrogen (right, 4 weeks, NS: vs NOVX (∆ P = 0.004), vs DOVX (∆ P < 0.001); DS vs DOVX (*P < 0.001); NOVX vs DOVX (# P = 0.007); 8 weeks, NS: vs NOVX (∆ P = 0.015), vs DOVX (∆ P < 0.001); DS vs DOVX (*P < 0.001); NOVX vs DOVX (# P = 0.01); 12 weeks, NS: vs DS (∆ P = 0.015), vs NOVX (∆ P = 0.009), vs DOVX (∆ P < 0.001); DS vs DOVX (*P < 0.001); NOVX vs DOVX (# P = 0.024))
Histological changes of the diabetic groups
Microscopic inspection of the liver, skeletal muscle, and kidney also revealed significant histological changes in the diabetic group. In the non-diabetic groups, hepatocytes were neatly arranged with clearly defined nuclear structure; no inflammatory cells were observed. In contrast, in the diabetic groups, hepatic lobules exhibited architectural distortion, and steatosis was observed in individual hepatocytes. In the non-diabetic groups, skeletal muscle fascicles were nicely arranged and cells appeared normal; ultramicroscopic filaments were regularly arranged. In DS and DOVX groups, increased spacing between skeletal muscle fascicles was observed, and ultramicroscopic filaments were loosely and irregularly aligned. In the kidney, in contrast to the non-diabetic groups, the diabetic groups showed increased glomerular volume and dilated medullary loops (Fig. 2).
The mRNA expression levels of IGF-1, IRS-1, and IRS-2 in the bone, liver, skeletal muscle, and kidney of each group
In bone, with time, both ovariectomy (NOVX) and a high-fat/sugar diet (DS) alone decreased the mRNA levels of IGF-1, IRS-1, and IRS-2 compared to control rats (NS). However, the lowest levels were observed in DOVX rats. For IGF-1 and IRS-1, this interaction was observed as early as 8 weeks after ovariectomy.
In liver, muscle and kidney, IGF-1, IRS-1, and IRS-2 exhibited different expression patterns in response to changes in diet and hormonal status compared to bone. In liver, both ovariectomy and diet alone eventually decreased the mRNA levels of IGF-1, and even lower IGF-1 levels were observed in DOVX rats. On the other hand, the mRNA levels of IRS-1 and IRS-2 were not significantly altered by ovariectomy alone, although a high-fat/sugar diet alone decreased the IRS-1 and IRS-2 mRNA levels in liver. In addition, unlike bone, no interaction between gonadal hormone status and diet was observed in the suppression of IRS-1 and IRS-2.
In muscle and kidney, similarly to liver, ovariectomy and a high-fat/sugar diet alone reduced IGF-1 mRNA levels; an even greater suppression of IGF-1 was observed in DOVX rats after 12 weeks. Ovariectomy also decreased IRS-1 (kidney) and IRS-2 (muscle and kidney). Also like liver, a high-fat/sugar diet alone was sufficient to reduce IRS-1 (kidney) and IRS-2 (muscle and kidney). Finally, an interaction between diet and gonadal steroid status was detected in muscle and kidney for IRS-1 and IRS-2; however, the time course of this interaction was different compared to bone (Table 4; Fig. 3).
IGF-1, IRS-1, and IRS-2 mRNA expression levels in the bone, liver, muscle, and kidney of each group. Bone: the expression levels of IGF-1 and IRS-2 in NOVX and DOVX groups were lower than that in NS and DS groups, the expression of IRS-1 in NOVX, DOVX and DS groups were lower than that in NS group at 12 weeks. Liver: the expression levels of IGF-1 and IRS-1 in DS and DOVX groups were lower than that in NS group at 12 weeks, the expression level of IRS-2 in DS group was lower than that in NS and NOVX groups at 4 and 8 weeks. Muscle: the expression levels of IGF-1, IRS-1, and IRS-2 in DS and DOVX groups were lower than that in NS group. Kidney: IGF-1, IRS-1 and IRS-2 expression in NOVX, DS, and DOVX groups were lower than that in the NS group
Liver, skeletal muscle, and kidney IGF-1, IRS-1, and IRS-2 protein expression levels 12 weeks after ovariectomy
IGF-1, IRS-1, and IRS-2 were expressed in hepatocytes, skeletal muscle cells, and renal epithelial cells of each group. Similarly to mRNA levels, both ovariectomy and diet alone decreased the protein levels of IGF-1 in the liver, kidney, and skeletal muscle, and even lower IGF-1 levels were observed in DOVX rats at 12 weeks.
However, different patterns were observed for IRS-1 and IRS-2. In liver, although ovariectomy and a high-fat/sugar diet either alone or together decreased the expression of IRS-1, at 12 weeks the levels were not significantly different among these three treatment groups. For hepatic IRS-2, only DOVX rats exhibited decreased protein expression compared to with controls.
In skeletal muscle, ovariectomy alone did not alter IRS-1 or IRS-2. However, both DS and DOVX rats exhibited decreased IRS-1 and IRS-2 protein levels at 12 weeks, compared to NS and NOVX rats.
In the kidney, ovariectomy alone decreased only IRS-1, although a high-fat/sugar diet alone decreased the protein levels of both IRS-1 and IRS-2, compared to NS rats. Again, similarly to the mRNA levels, DOVX rats exhibited the lowest levels of IRS-1 and IRS-2 protein in kidney (Table 5; Fig. 4).
IGF-1, IRS-1, and IRS-2 protein expression levels in the liver, muscle and kidney (×400). Liver: the expression levels of IGF-1 and IRS-1 in NOVX, DS and DOVX groups were lower than that in NS groups at 12 weeks, IRS-2 in DOVX rats was lower than that in NS group. Muscle: the expression levels of IGF-1 and IRS-1 in DS and DOVX groups were lower than that in NS and NOVX groups at 12 weeks, the expression levels of IRS-2 in DS and DOVX groups were lower than that in NS group at 12 weeks. Kidney: the expression levels of IGF-1, IRS-1, and IRS-2 in DOVX and DS groups were lower than that in NS group at 12 weeks
Discussion
The purpose of this study was to test whether estrogen loss and type II diabetes interact via decreased insulin signaling proteins to produce osteoporosis. The major new findings are that (1) a high-fat/sugar diet associated with insulin resistance was sufficient to eventually decrease bone density and plasma estrogen levels; (2) bone density was reduced more in OVX rats with DMII than in rats following OVX or DMII alone; and (3) IGF-1, IRS-1, and IRS-2 were reduced by OVX and DMII in liver, skeletal muscle, kidney, and bone; however, the decreases were generally more rapid and profound in bone compared to the other tissues. Collectively, these data demonstrate that estrogen loss and insulin resistance induced by a high-fat/sugar diet interact to produce osteoporosis and support the hypothesis that the bone loss may be mediated at least in part by concurrent decreases in the insulin signaling proteins in bone.
Due to the high prevalence of diabetes worldwide, a number of diabetic animal models have been developed, of which rodent models are the most thoroughly described. These rodent models can be classified into two broad categories: (1) genetically induced spontaneous diabetes models, such as Zucker diabetic fatty (ZDF) rats [16, 17] and Goto–Kakizaki (G–K) rat, a model for non-obese type II diabetes [18, 19] and (2) experimentally induced nonspontaneous diabetes models. These models include: adult streptozotocin (STZ)/alloxan rat models, neonatal STZ/alloxan models, partial pancreatectomy models, long-term high-fat (HF) diet-fed models, and HF diet-fed STZ models [20]. In these models, the single dose STZ- or alloxan-induced diabetes mimics features of type 1 diabetes; however, a high dose of STZ/alloxan (90–120 mg/kg) is required. HF diet-induced DMII rats are similar to the earlier stages of obesity associated with insulin resistance, whereas the combination of a HF diet and a low dose of STZ is closely analogous to the later stages of the human DMII syndrome [21–24]. In this study, we used a high-fat/sugar diet coupled with a delayed low dose of STZ to induce this model of DMII (weight gain, elevated levels of insulin and glucose, followed by weight loss and lower insulin levels). The transition from insulin resistance to hyperglycemia in this situation would be analogous to the decline in compensatory hyperinsulinemia and development of hyperglycemia that likely occurs in human type II diabetes.
While it is well established that DMI can reduce BMD, in patients with DMII, a normal, reduced or increased BMD has been observed in comparison with that of healthy controls [25–27]. Nevertheless, several clinical studies consistently demonstrated that DMII is associated with an increased risk of fractures even in the presence of high BMD [28–31]. In addition, Hamann et al. [32] found that in insulin-resistant DMII rats, trabecular and lumbar spine BMD were lower than in non-diabetic rats, and bone quality also decreased in streptozotocin-induced DMII [33]. Our results support these earlier findings, since we found that DMII alone time dependently decreased BMD.
Menopause, due to reduced estrogen levels, also decreases BMD. In support, we found that OVX rats exhibited markedly reduced BMD compared to normal female rats. However, whether estrogen loss exacerbates the deleterious effects of DMII has received only limited attention. For example, postmenopausal women with DMII exhibited larger holes in the trabecular bone at the distal radius as compared to controls [34]. In our study, after 12 weeks, the lumbar BMD of OVX rats with DMII was lower than OVX or DMII alone. This change in bone was associated with rather dramatic histological pathology in other tissues, including muscle, kidney and liver.
Although OVX with DMII decreased BMD and induced osteopenia and osteoporosis, the exact underlying mechanism is still elusive. It is well-known bone is continually being remodeled, depending on the balance between bone formation by osteoblasts and resorption by osteoclasts. A shift in this balance, causing a predominance of bone resorption over bone formation, results in bone loss such as that seen in osteoporosis. Postmenopausal women with DMII had lower levels of bone formation markers as compared to controls [35, 36], and it is widely accepted that hyperglycemia has direct and indirect deleterious effects on osteoblast function and bone formation; therefore, suppressed osteoblastogenesis may underlie the low bone mass in DMII.
Insulin resistance may be one potential contributor to reduced BMD in DMII, since hyperinsulinemia can be associated with low BMD [37]. In addition, the important role of insulin signaling in the maintenance of normal bone metabolism has been demonstrated using knockout mice. Small bone size, low BMD, and osteoporosis were reported in IGF-1 and IGF-1 receptor knockout mice [38], and cultured osteoblasts from IRS-2 −/− mice showed reduced differentiation and matrix synthesis compared with wild-type osteoblasts [39]. Moreover, IRS-1 deficiency in osteoblasts impairs osteoblast proliferation, differentiation, and support of osteoclastogenesis, resulting in low turnover osteopenia. Finally, nuclear insulin signaling may play an important role in the transcription control, differentiation, and growth of osteoblast cells, since both insulin and IGF-1 have been shown to be anabolic agents in osteoblasts and bone development primarily through the activation of Akt and ERK signaling pathways [40]. Therefore, the reductions in bone insulin signaling proteins observed in this study may have reduced osteoblast bone formation and explain the reductions in BMD observed in OVX rats with DMII.
Similar to previous studies [41–44], we found that DMII alone decreases IGF-1, IRS-1, and IRS-2 in the liver, skeletal muscle, and kidney. In some tissues, OVX alone was sufficient to decrease IRS-1 or IRS-2. However, the falls in these insulin signaling proteins generally occurred either sooner or more dramatically in bone. Several hormones and other factors (e.g., free fatty acids) have been identified as contributors to the development of insulin resistance [45–49]. Therefore, the differential timing and degree of suppression of insulin signaling proteins in liver, kidney, and skeletal muscle compared to bone could be due to either the actions of different mediators or to an enhanced sensitivity of bone to the same insulin resistance-inducing factors [50–52]. Future experiments are required to differentiate among these possibilities.
In conclusion, we have demonstrated that combined OVX and DMII decreased BMD more than OVX or DMII alone. The concurrent profound effect of OVX and DMII to decrease insulin signaling proteins in bone relative to other tissues suggests that these pathways may contribute to the severe osteoporosis that is produced.
References
M. Prasannarong, K. Vichaiwong, V. Saengsirisuwan, Calorie restriction prevents the development of insulin resistance and impaired insulin signaling in skeletal muscle of ovariectomized rats. Biochim. Biophys. Acta 1822, 1051–1061 (2012)
D. Unal, S. Aksak, Z. Halici, O. Sengul, B. Polat, B. Unal, M. Halici, Effects of diabetes mellitus on the rat liver during the postmenopausal period. J. Mol. Histol. 42, 273–287 (2011)
H. Chang-Quan, D. Bi-Rong, H. Ping, L. Zhen-Chan, Insufficient renal 1-alpha hydroxylase and bone homeostasis in aged rats with insulin resistance or type 2 diabetes mellitus. J. Bone. Miner. Metab. 26, 561–568 (2008)
S. Elis, H.W. Courtland, Y. Wu, J.C. Fritton, H. Sun, C.J. Rosen, S. Yakar, Elevated serum IGF-1 levels synergize PTH action on the skeleton only when the tissue IGF-1 axis is intact. J. Bone. Miner. Res. 25, 2051–2058 (2010)
R. Blakytny, M. Spraul, E.B. Jude, Review: the diabetic bone: a cellular and molecular perspective. Int. J. Low. Extrem. Wounds 10, 16–32 (2011)
T.D. Rachner, S. Khosla, L.C. Hofbauer, Osteoporosis: now and the future. Lancet 377, 1276–1287 (2011)
G. Mazziotti, J. Bilezikian, E. Canalis, D. Cocchi, A. Giustina, New understanding and treatments for osteoporosis. Endocrine 41, 58–69 (2012)
F.J. de Paula, M.C. Horowitz, C.J. Rosen, Novel insights into the relationship between diabetes and osteoporosis. Diabetes Metab. Res. Rev. 26, 622–630 (2010)
S. Kurra, E. Siris, Diabetes and bone health: the relationship between diabetes and osteoporosis-associated fractures. Diabetes Metab. Res. Rev. 27, 430–435 (2011)
C. Torti, G. Mazziotti, P.A. Soldini, E. Focà, R. Maroldi, D. Gotti, G. Carosi, A. Giustina, High prevalence of radiological vertebral fractures in HIV-infected males. Endocrine 41, 512–517 (2012)
S. Perrini, A. Natalicchio, L. Laviola, A. Cignarelli, M. Melchiorre, F. De Stefano, C. Caccioppoli, A. Leonardini, S. Martemucci, G. Belsanti, S. Miccoli, A. Ciampolillo, A. Corrado, F.P. Cantatore, R. Giorgino, F. Giorgino, Abnormalities of insulin-like growth factor-I signaling and impaired cell proliferation in osteoblasts from subjects with osteoporosis. Endocrinology 149, 1302–1313 (2008)
A. Giustina, G. Mazziotti, E. Canalis, Growth hormone, insulin-like growth factors, and the skeleton. Endocr. Rev. 29, 535–559 (2008)
J. Paccou, J. Dewailly, B. Cortet, Reduced levels of serum IGF-1 is related to the presence of osteoporotic fractures in male idiopathic osteoporosis. Joint Bone Spine 79, 78–82 (2012)
J. Vangipurapu, A. Stančáková, T. Kuulasmaa, P. Soininen, A.J. Kangas, M. Ala-Korpela, J. Kuusisto, M. Laakso, Association between liver insulin resistance and cardiovascular risk factors. J. Intern. Med. (2012). doi:10.1111/j.1365-2796.2012.02540.x
R.A. Soslow, A.J. Dannenberg, D. Rush, B.M. Woerner, K.N. Khan, J. Masferrer, A.T. Koki, COX-2 is expressed in human pulmonary, colonic, and mammary tumors. Cancer 89, 2637–2645 (2000)
R.R. Bosch, S.W. Janssen, P.N. Span, A. Olthaar, S.E. van Emst-de Vries, P.H. Willems, J.M.G. Martens, A.R. Hermus, C.C. Sweep, Exploring levels of hexosamine biosynthesis pathway intermediates and protein kinase C isoforms in muscle and fat tissue of Zucker diabetic fatty rats. Endocrine 20, 247–252 (2003)
M. Mansour, D. White, C. Wernette, J. Dennis, Y.X. Tao, R. Collins, L. Parker, E. Morrison, Pancreatic neuronal melanocortin-4 receptor modulates serum insulin levels independent of leptin receptor. Endocrine 37, 220–230 (2010)
M.H. Giroix, K. Louchami, Y.A. Carpentier, A. Sener, W.J. Malaisse, Fatty acid pattern of pancreatic islet lipids in Goto–Kakizaki rats. Endocrine 37, 173–179 (2010)
M. Matsushita, K. Tamura, S. Osada, H. Kogo, Effect of troglitazone on the excess testosterone and LH secretion in thyroidectomized, insulin-resistant, type 2 diabetic Goto–Kakizaki rats. Endocrine 27, 301–305 (2005)
M.S. Islam, T. Loots du, Experimental rodent models of type 2 diabetes: a review. Methods Find. Exp. Clin. Pharmacol. 31, 249–261 (2009)
M. Yu, W. Zhou, Y. Song, F. Yu, D. Li, S. Na, G. Zou, M. Zhai, C. Xie, Development of mesenchymal stem cell-implant complexes by cultured cells sheet enhances osseointegration in type 2 diabetic rat model. Bone 49, 387–394 (2011)
K. Srinivasan, B. Viswanad, L. Asrat, C.L. Kaul, P. Ramarao, Combination of high-fat diet-fed and low-dose streptozotocin-treated rat: a model for type 2 diabetes and pharmacological screening. Pharmacol. Res. 52, 313–320 (2005)
M.J. Reed, K. Meszaros, L.J. Entes, M.D. Claypool, J.G. Pinkett, T.M. Gadbois, G.M. Reaven, A new rat model of type 2 diabetes: the fat-fed, streptozotocin-treated rat. Metabolism 49, 1390–1394 (2000)
W. Sun, Y. Bi, H. Liang, M. Cai, X. Chen, Y. Zhu, M. Li, F. Xu, Q. Yu, X. He, J. Ye, J. Weng, Inhibition of obesity-induced hepatic ER stress by early insulin therapy in obese diabetic rats. Endocrine 39, 235–241 (2011)
D. Merlotti, L. Gennari, F. Dotta, D. Lauro, R. Nuti, Mechanisms of impaired bone strength in type 1 and 2 diabetes. Nutr. Metab. Cardiovasc. Dis. 20, 683–690 (2010)
R.A. Kayal, J. Alblowi, E. McKenzie, N. Krothapalli, L. Silkman, L. Gerstenfeld, T.A. Einhorn, D.T. Graves, Diabetes causes the accelerated loss of cartilage during fracture repair which is reversed by insulin treatment. Bone 44, 357–363 (2009)
A. Montagnani, S. Gonnelli, M. Alessandri, R. Nuti, Osteoporosis and risk of fracture in patients with diabetes: an update. Aging Clin. Exp. Res. 23, 84–90 (2011)
J.M. Pritchard, L.M. Giangregorio, S.A. Atkinson, K.A. Beattie, D. Inglis, G. Ioannidis, Z. Punthakee, J.D. Adachi, A. Papaioannou, Adults with type 2 diabetes mellitus (DM) have an elevated fracture risk despite normal areal bone mineral density (aBMD). Arthr. Care Res. (Hoboken) 64, 83–91 (2012)
T. Mancini, G. Mazziotti, M. Doga, R. Carpinteri, N. Simetovic, P.P. Vescovi, A. Giustina, Vertebral fractures in males with type 2 diabetes treated with rosiglitazone. Bone 45, 784–788 (2009)
G. Mazziotti, M. Gola, A. Bianchi, T. Porcelli, A. Giampietro, V. Cimino, M. Doga, C. Gazzaruso, L. De Marinis, A. Giustina, Influence of diabetes mellitus on vertebral fractures in men with acromegaly. Endocrine 40, 102–108 (2011)
A. Shu, M.T. Yin, E. Stein, S. Cremers, E. Dworakowski, R. Ives, M.R. Rubin, Bone structure and turnover in type 2 diabetes mellitus. Osteoporos. Int. 23, 635–641 (2012)
C. Hamann, C. Goettsch, J. Mettelsiefen, V. Henkenjohann, M. Rauner, U. Hempel, R. Bernhardt, N. Fratzl-Zelman, P. Roschger, S. Rammelt, K.P. Günther, L.C. Hofbauer, Delayed bone regeneration and low bone mass in a rat model of insulin-resistant type 2 diabetes mellitus is due to impaired osteoblast function. Am. J. Physiol. Endocrinol. Metab. 301, E1220–E1228 (2011)
N. Erdal, S. Gürgül, S. Kavak, A. Yildiz, M. Emre, Deterioration of bone quality by streptozotocin (STZ)-induced type 2 diabetes mellitus in rats. Biol. Trace Elem. Res. 140, 342–353 (2011)
S. Chakreeyarat, S. Saetung, L.O. Chailurkit, S. Rattanasiri, S. Ditbanjong, N. Chitrapazt, S. Jaovisidha, B. Ongphiphadhanakul, Elevated vitamin D status in postmenopausal women on thiazolidinediones for type 2 diabetes. Endocrine 39, 278–282 (2011)
M. Yamamoto, T. Yamaguchi, K. Nawata, M. Yamauchi, T. Sugimoto, Decreased PTH levels accompanied by low bone formation are associated with vertebral fractures in postmenopausal women with type 2 diabetes. J. Clin. Endocrinol. Metab. 97, 1277–1284 (2012)
L. Sauque-Reyna, M.A. Salcedo-Parra, P.R. Sánchez-Vargas, J.D. Flores-Helguera, C. Badillo-Sánchez, A. Reza-Albarrán, M. Rodríguez-Morán, F. Guerrero-Romero, Bone mineral density in patients with type 2 diabetes. Rev. Invest. Clin. 63, 162–169 (2011)
S. Arikan, A. Tuzcu, M. Bahceci, S. Ozmen, D. Gokalp, Insulin resistance in type 2 diabetes mellitus may be related to bone mineral density. J. Clin. Densitom. 15, 186–190 (2012)
N. Ogata, H. Kawaguchi, Involvement of insulin and IGF-1 signaling molecules in bone metabolism. Clin. Calcium 18, 614–622 (2008)
T. Akune, N. Ogata, K. Hoshi, N. Kubota, Y. Terauchi, K. Tobe, H. Takagi, Y. Azuma, T. Kadowaki, K. Nakamura, H. Kawaguchi, Insulin receptor substrate-2 maintains predominance of anabolic function over catabolic function of osteoblasts. J. Cell. Biol. 159, 147–156 (2002)
W. Zhang, X. Shen, C. Wan, Q. Zhao, L. Zhang, Q. Zhou, L. Deng, Effects of insulin and insulin-like growth factor 1 on osteoblast proliferation and differentiation: differential signalling via Akt and ERK. Cell. Biochem. Funct. 30, 297–302 (2012)
M. Cipok, S. Aga-Mizrachi, A. Bak, T. Feurstein, R. Steinhart, C. Brodie, S.R. Sampson, Protein kinase Calpha regulates insulin receptor signaling in skeletal muscle. Biochem. Biophys. Res. Commun. 345, 817–824 (2006)
M.K. Diamond-Stanic, E.M. Marchionne, Critical role of the transient activation of p38 MAPK in the etiology of skeletal muscle insulin resistance induced by low-level in vitro oxidant stress. Biochem. Biophys. Res. Commun. 405, 439–444 (2011)
Y. Segev, R. Eshet, O. Yakir, N. Haim, M. Phillip, D. Landau, Systemic and renal growth hormone-IGF1 axis involvement in a mouse model of type 2 diabetes. Diabetologia 50, 1327–1334 (2007)
J.L. Bailey, B. Zheng, Z. Hu, S.R. Price, W.E. Mitch, Chronic kidney disease causes defects in signaling through the insulin receptor substrate/phosphatidylinositol 3-kinase/Akt pathway: implications for muscle atrophy. J. Am. Soc. Nephrol. 17, 1388–1394 (2006)
V.T. Samuel, G.I. Shulman, Mechanisms for insulin resistance: common threads and missing links. Cell 148, 852–871 (2012)
Y. Zhang, B. Zhou, F. Zhang, J. Wu, Y. Hu, Y. Liu, Q. Zhai, Amyloid-β induces hepatic insulin resistance by activating JAK2/STAT3/SOCS-1 signaling pathway. Diabetes 61, 1434–1443 (2012)
O.T. Hardy, M.P. Czech, S. Corvera, What causes the insulin resistance underlying obesity? Curr. Opin. Endocrinol. Diabetes Obes. 19, 81–87 (2012)
A.R. Martins, R.T. Nachbar, R. Gorjao, M.A. Vinolo, W.T. Festuccia, R.H. Lambertucci, M.F. Cury-Boaventura, L.R. Silveira, R. Curi, S.M. Hirabara, Mechanisms underlying skeletal muscle insulin resistance induced by fatty acids: importance of the mitochondrial function. Lipids Health Dis. 11, 30 (2012)
S.S. Moon, Y.S. Lee, S.W. Kim, Association of nonalcoholic fatty liver disease with low bone mass in postmenopausal women. Endocrine (2012). doi:10.1007/s12020-012-9639-6
D.C. Leitman, S. Paruthiyil, C. Yuan, C.B. Herber, M. Olshansky, M. Tagliaferri, I. Cohen, T.P. Speed, Tissue-specific regulation of genes by estrogen receptors. Semin. Reprod. Med. 30, 14–22 (2012)
A. Margoni, L. Fotis, A.G. Papavassiliou, The transforming growth factor-beta/bone morphogenetic protein signalling pathway in adipogenesis. Int. J. Biochem. Cell. Biol. 44, 475–479 (2012)
P. Magni, E. Dozio, E. Galliera, M. Ruscica, M.M. Corsi, Molecular aspects of adipokine-bone interactions. Curr. Mol. Med. 10, 522–532 (2010)
Acknowledgments
We thank Professor Virginia L. Brooks for editing the language (Department of Physiology and Pharmacology, Oregon Health & Science University, Portland, Oregon 97239, USA. brooksv@ohsu.edu). This study was financially supported by Hebei Natural Science Foundation (C2009001179).
Conflict of interest
None of the authors has any conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Li, B., Wang, Y., Liu, Y. et al. Altered gene expression involved in insulin signaling pathway in type II diabetic osteoporosis rats model. Endocrine 43, 136–146 (2013). https://doi.org/10.1007/s12020-012-9757-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-012-9757-1