Abstract
It has been known that thyroid stimulating hormone (TSH) stimulates the growth or development of thyroid malignancy and higher serum TSH has association with both thyroid cancer incidence and advanced tumor stage. However, the role of TSH in high-risk features of well-differentiated thyroid cancer was not fully evaluated especially in Asian population. The purpose of our study is to evaluate the association of preoperative serum TSH levels with the advance of differentiated thyroid cancer and its high-risk clinicopathological features in Korean patients. We evaluated 554 patients retrospectively who underwent thyroidectomy and diagnosed as differentiated thyroid cancer during a 3-year period at Pusan National University Hospital. The preoperative TSH levels were significantly higher in the patients with extrathyroidal extension (P = 0.002) and those with lateral lymph node metastasis (P = 0.007). As the increase of the serum TSH concentration, there were significant rising trends in the prevalence of extrathyroidal extension (P = 0.009). In the patients with TSH ≥ 2.5 mIU/L, the prevalences of extrathyroidal extension (P = 0.006) and lateral lymph node metastasis (P = 0.024) were also significantly higher. Using multiple logistic regression, preoperative TSH level was a predictive factor for the presence of extrathyroidal extension (P = 0.008) and lateral lymph node metastasis (P = 0.025). Hashimoto’s thyroiditis itself was not associated with the status of extrathyroidal extension and lateral lymph node metastasis. In conclusion, preoperative TSH levels were associated with lateral lymph node matastasis, a novel finding, and extrathyroidal extension in well differentiated thyroid cancer and might be useful as a preoperative supplementary marker for determining the optimal extent of differentiated thyroid cancer surgery in Korean patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With the development of improved diagnostic and testing technologies, the incidence of thyroid cancers is increasing rapidly [1]. If treated appropriately, prognoses of patients with differentiated thyroid cancer are good in most cases. However, local or regional recurrences occur in around 5–20% of patients who have been operated on for differentiated thyroid cancers [2].
It has been shown that many genes and growth factors are involved with the development of thyroid cancer [3, 4]. But, it has been still understood that thyroid stimulating hormone (TSH) can also play an important role in the abnormal growth of thyrocytes. The fact that TSH can stimulate the growth of not only normal but also malignant thyroid tissues is the current basis on conducting postoperative TSH suppression therapy, which could reduce the rates of recurrence and improve the prognoses for differentiated thyroid cancer [5, 6]. TSH shows a trend to increase along with age [7], but also may be diverse in different individuals and population even within normal ranges.
Recently, some studies have been reported that TSH stimulates the growth or development of thyroid malignancy and higher serum TSH has association with both thyroid cancer incidence and advanced stage disease [8–13]. However, to the best of our knowledge, there was no study on the possible roles of preoperative TSH levels in the advance of differentiated thyroid cancer in Asian population, including Korean. According to the recent report [14], the time trend of incidence of thyroid cancer is different among different race/ethnicity groups, and there was a small degree of increase in the Asians compared with other races, including Hispanic and non-Hispanic whites. So we thought that it will be meaningful to evaluate the association of preoperative serum TSH levels and well differentiated thyroid cancer in Asian population additionally and to examine, if preoperative TSH levels may be associated with advanced tumor stage, what clinicopathologic high-risk cancer features, including extrathyroidal extention and lymph node metastasis, were related with TSH concentrations.
In this study, we attempted to elucidate correlations between preoperative TSH levels and postoperative clinicopathological features in differentiated thyroid cancer in Korean patients.
Patients and methods
Between January 2006 and December 2008, total 867 patients underwent thyroid surgery at Pusan National University Hospital. Of these, 618 patients were found to have primary thyroid cancer after surgery. All thyroid surgeries were performed by two surgeons during this 3-year time period. Of the 618 cases of thyroid surgeries, unilateral lobectomy was performed only in 14 cases, and total thyroidectomy was done in 604 patients. Papillary thyroid carcinoma accounted for 97.2% of all thyroid malignancies (601 of 618). Follicular thyroid cancer (nine cases) or Hürthle cell cancer (one case) comprised 1.6% of thyroid malignancies (10 of 618). The remaining 1.1% of thyroid cancers (seven of 618) were anaplastic thyroid cancer (five cases), and medullary thyroid cancer (two cases). Undifferentiated carcinoma and medullary carcinoma were considered unlikely to be TSH responsive and excluded in this analysis. 32 of 618 patients were also excluded because antithyroid drugs or levothyroxine were prescribed before checking of preoperative TSH levels. In addition, adequate preoperative serum TSH measurement was not available in 25 patients. Finally, 554 patients with differentiated thyroid cancer were eligible for analysis in our study. Of these, total thyroidectomy was performed in 540 (97.5%) patients. Central compartment neck dissection was routinely performed during total thyroidectomy and selective neck dissection (159 of 540, 28.7%) was done for patients with clinically overt or ultrasound detected metastatic cervical lymph nodes. Preoperative assessment for lateral cervical lymph node metastasis included high-resolution ultrasonography, computed tomography, and fine-needle aspiration cytologic investigations. Pathologic Hashimoto’s thyroiditis was defined as the presence of diffuse plasma and lymphocytic cell infiltration, oxyphilic cells, and the formation of lymphoid follicles and reactive germinal centers. However, peritumoral inflammatory response was not considered as Hashimoto’s thyroiditis.
TSH level was checked within 3 months before surgery and was determined by immunoradiometric assay using the commercial kit (Coat-A-Count, TSH IRMA, DPC, USA). The analytical sensitivity of the assay for TSH is 0.03 mIU/L and the intra-assay coefficients of variation ranged from 1.9 to 5.8%. Normal reference ranges for TSH were 0.4–5.0 mIU/L. We divided the patients into two groups as a cut-off value of 2.5 mIU/L of TSH level for the analyses, because more than 95% of normal individuals have TSH levels below 2.5 mIU/L, and TSH values greater than 2.5 mIU/L could be predictive of evolution into “high TSH level” [15, 16] even within normal ranges. As previous study [12], we also used the 45 of age as a cut-off because it has been known that general prognoses were worse in patients ≥45 years versus <45 years [17].
Informed consent was obtained from each participant at the time of surgery. The retrospective review protocol was approved by the Institutional Review Board at Pusan National University Hospital.
Statistical analysis
Statistical analyses were performed with SPSS version 12.0 (SPSS, Chicago, IL, USA). Serum TSH value did not show normal distribution, so it was reported as median and range. Age, tumor size, and serum TSH were evaluated as continuous variables. Independent two-sample t-test was used to compare two independent groups. Pearson’s χ2 test was done to analyze categorical data as appropriate. Factors related to extrathyroidal extension and lateral lymph node metastasis were conducted with multivariate logistic regression analyses. Multivariate models for extrathyroidal extension were adjusted for age, gender, tumor size, lymphovascular invasion, multifocality, Hashimoto’s thyroiditis, TSH as independent variables. In multivariate analyses for lateral lymph node metastasis, extrathyroidal extension was added as an independent variable. P < 0.05 was considered statistically significant.
Results
Clinicopathologic characteristics of patients
The cohort included 86 men and 468 women with age ranging from 12 to 80 years (47.9 ± 12.5). The mean tumor size was 1.28 ± 1.05 cm and the mean preoperative TSH level was 1.96 (range 0.001–10.8) mIU/L. Of the total 554 cohort cases, pathological extrathyroidal extension, lymphovascular invasion, and Hashimoto’s thyroiditis comprised 57.8% (320 of 554), 8.1% (45 of 554), and 7.2% (40 of 554), respectively. Lymph node metastasis and distant metastasis were identified in 54.5% (302 of 554) and 1.8% (10 of 554), respectively. With regard to lymph node metastasis, only central lymph node involvement comprised 34.3% (190 of 554), while lateral lymph node involvement comprised 20.2% (112 of 554). 190 patients (34.3%) had multifocality on tissue pathology and patients with tumor size >4 cm were 3.1% (17 of 554) (Table 1).
TSH levels according to the clinicopathologic features
As shown in Table 1, the preoperative TSH level was higher in the patients with advanced tumor stages (stage III/IV) compared to those with stage I and II disease. The preoperative TSH level in the patients with extrathyroidal extension was higher compared with those without extrathyroidal extension (1.73 vs. 1.30 mIU/L, P = 0.002). Although, there was no significant difference in the preoperative TSH level between the presence and absence of lymph node metastasis, the TSH level was significantly higher in the patients with lateral lymph node metastasis compared with those without nodal metastasis and those with central lymph node metastasis (P = 0.007, P = 0.015, respectively). The preoperative TSH level was higher in the patients with ≥45 years (350 of 554, 63.1%) compared with those <45 years (1.65 vs. 1.44 mIU/L, P = 0.054). The patients coexisting with Hashimoto’s thyroiditis on surgical pathologic finding represented also higher TSH level. There were no significant differences in preoperative levels according to gender, pathologic tumor size, multifocalilty, lymphovascular invasion, and distant metastasis.
Prevalence of extrathyroidal extension and lateral lymph node metastasis according to the TSH levels and tumor size
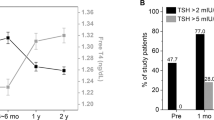
We subdivided total patients into four groups of serum TSH ranges (<0.40, 0.40–2.49, 2.50–4.99, ≥5.00) and examined the prevalence of extrathyroidal extension. As the increase of the serum TSH concentration, there were significant rising trends in the prevalence of extrathyroidal extension (46.2, 55.1, 69.1, 65.7%, P = 0.009) (Fig. 1).
In the patients with TSH ≥ 2.5 mIU/L, a higher prevalence in extrathyroidal extension was noted compared to those with TSH < 2.5 mIU/L (68.2 vs. 54.6%, P = 0.006). Moreover, there were significant increase in the presence of lateral lymph node metastasis in the patients with TSH ≥ 2.5 mIU/L compared to those with TSH < 2.5 mIU/L (28.7 vs. 17.6%, P = 0.024). The mean age was also increased in the group with TSH ≥ 2.5 mIU/L (Table 2).
Furthermore, we divided the patients into two groups according to the tumor size as cut-off of 2 cm, a classification point of T1 and T2 in thyroid cancer staging [16], and performed further analyses (≤2 cm, [471 of 554] vs. >2 cm, [83 of 554]). In cases of ≤2 cm of tumor size, the presences of extrathyroidal extention (P = 0.024) and later lymph node metastasis (P = 0.030) were also significantly increased in the group with TSH > 2.5 mIU/L. These findings were also observed similarly in cases of >2 cm of tumor size (Table 3).
TSH levels according to the tumor stages
According to the American Joint Committee on Cancer (AJCC)/International Union Against Cancer (UICC) pathologic tumor-node-metastasis (TNM) classification [17], there were 290 patients with stage I (52.3%), 8 with stage II (1.4%), 183 with stage III (33.0%), and 73 with stage IV disease (13.2%).
We evaluated the association of serum TSH concentrations with the advance of the tumor stage in patients with age ≥ 45 years. As the advance of the tumor stage, serum TSH concentrations were significantly increased (Fig. 2a). The TSH level was significantly higher in the patients with stage III and stage IV relative to those with stage I and II disease (1.79 vs. 1.19 mIU/L, P < 0.001) (Fig. 2b).
Prognostic factors for extrathyroidal extension and lateral lymph node metastasis
Multivariate logistic regression analyses showed that the existences of lymphovascular invasion (P < 0.001), multifocality (P < 0.001), and TSH ≥ 2.5 mIU/L (P = 0.006) were predictive factors of the presence of extrathyroidal extension. In the point of lateral lymph node involvement, lymphovascular invasion (P < 0.001), tumor size > 2 cm (P < 0.001), the presences of extrathyroidal extension (P < 0.001), multifocality (P = 0.035) and TSH ≥ 2.5 mIU/L (P = 0.022) were predictive factors. Pathological Hashimoto’s thyroiditis was not significantly associated with the presences of extrathyroidal extension (P = 0.236) and lateral lymph node metastasis (P = 0.395) in our data (Table 4).
Discussion
Recently, several studies reported that TSH is associated with the incidence of thyroid cancers regardless of age and is also related with advanced stages, supporting the role of TSH in differentiated thyroid cancers [8–13]. However, there was no study on these correlations in the Asian population. In this study, we demonstrated that high preoperative TSH levels were significantly correlated with extrathyroidal extension, lateral lymph node metastasis, and advanced TNM stage and a predictive factor for extrathyroidal extension and lateral lymph node involvement in Korean patients with differentiated thyroid cancers. In consistent with previous findings [12, 13], the mean preoperative TSH levels were also higher in the patients with stage III and IV compared to those with stage I and II in both analyses with total patients and patients with ≥45 years of age in our study.
The risk of death in relation to the degree of extrathyroidal extension was reported to be 2.9–7.7 times more and it was also reported to be 5–17 times increased in a study by Cady et al., showing that the degree of infiltration was a powerful prognostic factor [18, 19]. Similar to the previous studies that reported the relationship between high TSH level and extrathyroidal extension [11, 12], TSH levels were also significantly higher in patients with extrathyroidal extension, suggesting preoperative TSH value is one of the prognostic factors that could predict the prevalence of extrathyroidal extension in our study. Furthermore, we showed that the prevalence of extrathyroidal extension was significantly increased as the rise of TSH levels.
Although there is no agreed opinion on the prognostic value of lymph node metastasis [20], it is known that lymph node metastases are found in 20–50% of diagnoses and central lymph node involvements are reported in approximately 30% in T1 or T2 lesions in the case of papillary thyroid carcinomas [21, 22]. In addition, lymph node metastases found at the time of diagnosis is an independent risk of tumor recurrence and some authors suggested that central lymph node dissections will reduce the risk of recurrence and enhance survival [23–25]. Based on these evidences, our hospital conducted central compartment neck dissections in almost all thyroid papillary carcinoma patients. Although prophylactic lateral lymph node dissections are not generally recommended, lateral lymph node dissections reduced the risks of recurrence and mortality in patients with clinically or US-detected lymph node metastasis [26, 27]. While Haymart et al. could not identify the effect of TSH on lymph node metastases [11, 12], Fiore et al. showed that TSH values in patients with neck node metastasis were significantly higher than those without neck node metastasis [13]. We also evaluated the association of preoperative TSH levels with lymph node metastasis through routine operative surveillance of lymph node involvement. In this study, there was no significant difference in mean TSH level in relation to central lymph node metastasis. However, as a novel finding, incidences of lateral lymph node metastases were more increased significantly in patients with high preoperative TSH levels. In addition, lateral lymph node metastases were found in 68.4%, especially in cases with tumor size >2 cm and TSH ≥2.5 mIU/L. Hence, we think that the preoperative neck ultrasonography should be performed to detect lateral lymph node enlargement in all subjects with elevated preoperative TSH levels even within the normal range. We believe that these results relating to TSH in our study are reliable because operations were conducted by two surgeons having the same opinion about thyroid operation method including neck dissection in a relatively short period of 3 years.
The scope and extent of initial surgeries and the decision for post-operative radioiodine therapy in the treatment of papillary thyroid carcinomas remain controversial, especially in the case of T1 tumors (less than 2 cm). In this study, the frequencies of extrathyroidal extension and lateral lymph node metastases were significantly higher in the group with TSH ≥ 2.5 compared to the group with TSH < 2.5 in T1 tumors with sizes less than 2 cm. As a result, preoperative TSH level may represent a considerable prognostic factor for advanced stage in small tumors with sizes less than 2 cm.
It is considered that patients with Hashimoto’s thyroiditis have higher risks for the incidence of thyroid papillary carcinomas compared to patients without hashimoto’s thyroiditis [28, 29]. In our study, the existence of pathological Hashimoto’s thyroiditis itself did not show any significant correlations with extrathyroidal extension and lateral lymph node metastases, thus increase in TSH level rather than the morbidity of the Hashimoto’s thyroiditis itself may be associated with the risk factors in the advance of tumor stages. This finding is also consistent with the study of Fiore et al. [13] showing that the frequency of papillary thyroid cancer was not significantly different between thyroid auto-antibodies (TAb) positive and TAb negative patients and may be an another result, which supports that thyroid autoimmunity does not play a significant role in the advance of thyroid cancer. The prevalence of papillary thyroid cancer was very high (97.2%) in our analyses and the possible reason is that Busan is very iodine-sufficient region because it is located near the East Sea of Asia and most people living our city take plenty of sea foods.
Our study did have several limitations. First, the study was not based on longitudinal observations but was conducted under a cross-sectional design and some preoperative data including thyroid auto-antibodies or thyroid scan were not obtained. Therefore, patients with transient thyroid dysfunctions, especially in those with below or above normal ranges of preoperative TSH levels, might be included in our data. But, patients who had been previously diagnosed with hypothyroidism or Graves’ disease were excluded in our study. Second, we could not elucidate the association with distant metastasis (1.8%) and tumor size > 4 cm (3.1%) because of very low cases in our data. Lastly, even if high TSH level is related to advanced stages, it is unknown whether it will directly affect overall prognosis of thyroid cancers such as tumor recurrences and survival.
In conclusion, although high preoperative TSH level is not considered an important prognostic factor for differentiated thyroid cancer patients, increased preoperative TSH levels may be also correlated with advanced cancer stages and its high-risk features including extrathyroidal extension and lateral lymph node metastases in Korean population. As a result, TSH could be considered as a supplementary marker when determining the scope of required treatment before operation.
References
N.C. Hodgson, J. Button, C.C. Solorzano, Ann. Surg. Oncol. 11, 1093–1097 (2004)
M.J. Schlumberger, N. Engl. J. Med. 338, 297–306 (1998)
M. Derwahl, M. Broecker, Z. Kraiem, J. Clin. Endocrinol. Metab. 84, 829–834 (1998)
E.L. Mazzaferri, Endocr. Pract. 6, 221–225 (2000)
B. Biondi, S. Filetti, M. Schlumberger, Nat. Clin. Pract. Endocrinol. Metab. 1, 32–40 (2005)
J. Jonklaas, N.J. Sarlis, D. Litofsky, K.B. Ain, S.T. Bigos, J.D. Brierley, D.S. Cooper, B.R. Haugen, P.W. Ladenson, J. Magner, J. Robbins, D.S. Ross, M. Skarulis, H.R. Maxon, S.I. Sherman, Thyroid 16, 1229–1242 (2006)
M.I. Surks, J.G. Hollowell, J. Clin. Endocrinol. Metab. 92, 4575–4582 (2007)
K. Boelaert, J. Horacek, R.L. Holder, J.C. Watkinson, M.C. Sheppard, J.A. Franklyn, J. Clin. Endocrinol. Metab. 91, 4295–4301 (2006)
J. Jonklaas, H. Nsouli-Maktabi, S.J. Soldin, Thyroid 18, 943–952 (2008)
S.A. Polyzos, M. Kita, Z. Efstathiadou, P. Poulakos, A. Slavakis, D. Sofianou, N. Flaris, M. Leontsini, A. Kourtis, A. Avramidis, J. Cancer Res. Clin. Oncol. 134, 953–960 (2008)
M.R. Haymart, D.J. Repplinger, G.E. Leverson, D.F. Elson, R.S. Sippel, J.C. Jaume, H. Chen, J. Clin. Endocrinol. Metab. 93, 809–814 (2008)
M.R. Haymart, S.L. Glinberg, J. Liu, R.S. Sippel, J.C. Jaume, H. Chen, Clin. Endocrinol. (Oxf.) 71, 434–439 (2009)
E. Fiore, T. Rago, M.A. Provenzale, M. Scutari, C. Ugolini, F. Basolo, G. Di Coscio, P. Berti, L. Grasso, R. Elisei, A. Pinchera, P. Vitti, Endocr. Relat. Cancer 16, 1251–1260 (2009)
G.P. Yu, J.C. Li, D. Branovan, S. McCormick, S.P. Schantz, Thyroid 20, 465–473 (2010)
Z. Baloch, P. Carayon, B. Conte-Devolx, L.M. Demers, U. Feldt-Rasmussen, J.F. Henry, V.A. LiVosli, P. Niccoli-Sire, R. John, J. Ruj, P.P. Smyth, C.A. Spencer, J.R. Stockigt, Thyroid 13, 3–126 (2003)
M.P.J. Vanderpump, W.M.G. Tunbridge, J.M. French, D. Appleton, D. Bates, F. Clark, J. Grimley Evans, D.M. Hasan, H. Rodgers, F. Tunbridge, E.T. Young, Clin. Endocrinol. (Oxf.) 43, 55–68 (1995)
American Joint Committee on Cancer, in AJCC cancer staging handbook, 6th edn (Springer, New York, 2002), pp 89–98
I.D. Hay, E.J. Bergstralh, J.R. Goellner, J.R. Ebersold, C.S. Grant, Surgery 114, 1050–1057 (1993)
B. Cady, R. Rossi, Surgery 104, 947–953 (1988)
D.S. Dean, I.D. Hay, J Moffitt Cancer Center 7, 229–238 (2000)
Y. Ito, T. Uruno, K. Nakano, Y. Takamura, A. Miya, K. Kobayashi, T. Yokozawa, F. Matsuzuka, S. Kuma, K. Kuma, A. Miyauchi, Thyroid 13, 381–387 (2003)
G. Pellegriti, C. Scollo, G. Lumera, C. Regalbuto, R. Vigneri, A. Belfiore, J. Clin. Endocrinol. Metab. 89, 3713–3737 (2004)
A. Jukkola, R. Bloigu, T. Ebeling, P. Salmela, G. Blanco, Endocr. Relat. Cancer 11, 571–579 (2004)
J.A. Pereira, J. Jimeno, J. Miquel, M. Iglesias, A. Munne, J.J. Sancho, A. Sitges-Serra, Surgery 138, 1095–1100 (2005)
M.L. Urken, Endocr. Pract. 16, 1–29 (2010)
Y. Ito, C. Tomoda, T. Uruno, Y. Takamura, A. Miya, K. Kobayashi, F. Matsuzuka, K. Kuma, A. Miyauchi, World J. Surg. 28, 498–501 (2004)
M.A. Kouvaraki, S.E. Shapiro, B.D. Fornage, B.S. Edeiken-Monro, S.I. Sherman, R. Vassilopoulou-Sellin, J.E. Lee, D.B. Evans, Surgery 134, 946–954 (2003)
C. Cipolla, L. Sandonato, G. Graceffa, S. Fricano, A. Torcivia, S. Vieni, S. Latteri, M.A. Latteri, Am. Surg. 71, 874–878 (2005)
O. Kurukahvecioglu, F. Taneri, O. Yuksel, A. Aydin, E. Tezel, E. Onuk, Adv. Ther. 24, 510–516 (2007)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, S.S., Lee, B.J., Lee, J.C. et al. Preoperative serum thyroid stimulating hormone levels in well-differentiated thyroid carcinoma is a predictive factor for lateral lymph node metastasis as well as extrathyroidal extension in Korean patients: a single-center experience. Endocr 39, 259–265 (2011). https://doi.org/10.1007/s12020-010-9430-5
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-010-9430-5