Abstract
Thyroid-stimulating hormone (TSH) is a growth factor affecting the initiation or progression of papillary thyroid cancer (PTC). However, the relationship between preoperative serum TSH and papillary thyroid microcarcinoma (PTMC) remains controversial. To investigate the relationship between preoperative serum TSH and tumor status of PTMC, a multicentered retrospective study was performed from January 2014 to December 2016. The cohort of this study consisted of 1997 patients who underwent thyroid surgery. Serum TSH concentrations were measured and PTMC was diagnosed based on the post-operation pathological report. Results showed that the preoperative serum TSH concentration was not related to age and gender but was positively associated with tumor size. Furthermore, higher TSH level was associated with extra-thyroidal extension and lymph node metastasis (LNM). These results indicated that TSH might not be involved in the development of PTMC but may be associated with PTMC progression. Preoperative serum TSH concentration should be considered as risk predictor for tumor progression in patients with PTMC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thyroid cancer is one of the most common malignancies of the endocrine system, which accounts for 1% of all human neoplasms [1]. Its annual incidence is estimated to be 0.5–10 per 100,000 persons worldwide [2]. However, in Chinese population, the incidence is 14.7 per 100,000 persons, well above the world average estimate. In 2015, a total of 201,000 new cases were diagnosed and around 75% (151,000) were women [3]. In recent years, the incidence of thyroid cancer continues to rise [4, 5] because of the increased use of imaging methods and early detection of tumors less than 1 cm, especially the increased detection of papillary thyroid microcarcinoma (PTMC) [6, 7]. Fortunately, the prognosis of PTMC is generally good because of its nature of being indolent and easily being monitored by neck ultrasonography [8]. Patients with PTMC are believed to have a low risk of recurrence (2.4%), and less than 1% of risk for distant metastasis. Although PTMC-associated recurrence and metastasis is low, the negative psychosocial and economic impact caused by this disease could be substantial and the quality of life for patients with PTMC would be compromised. Thus, accurate risk stratification is important to determine the patients who need more aggressive therapy.
Thyroid stimulating hormone (TSH) is a well-known growth factor for thyroid follicular cells, potentially affecting the initiation or progression of follicular-cell derived thyroid cancer [9]. Serum TSH also regulates thyroid cell differentiation and represents thyroid function sensitively [10]. Thus, it is used for evaluation of thyroid nodules. TSH suppression with levothyroxine is suggested as a therapeutic intervention for patients with thyroid cancer on the assumption that it can prevent the growth and spread of thyroid cancer cells [11]. Maintaining serum TSH in the subnormal-normal range was associated with better outcomes across all stages in patients with differentiated thyroid carcinoma (DTC) [12,13,14]. However, more aggressive TSH-suppressive treatment (TSH maintained below the lower limit of the reference range) is of little or no benefit to the vast majority of patients with DTC [9, 15]. In addition, several studies have reported that there is significant association between preoperative serum TSH levels and thyroid carcinoma status [1, 16, 17]. Even a slightly elevated preoperative TSH concentration increases the risk of thyroid cancers. For PMTC, an earlier investigation found no significant association between TSH levels and the progression of PTMC [18]. However, a recent study of 127 PTMCs found that tumor progression was significantly higher in the subgroup with the highest serum TSH levels (HR 3.55; 95% CI, 1.22–10.28) [6]. The true value of TSH in PTMC management is still debated. Furthermore, so far, the value of TSH in the prediction of malignancy of small thyroid nodules, which are commonly detected incidentally during ultrasound examinations, is still unclear. More evidence is required to illustrate the possible effect of TSH for PTMC.
In this study, we focus on the association between preoperative serum TSH levels and PTMC and investigate whether a relationship exists between preoperative serum TSH concentration and tumor size, extra-thyroidal extension, lymph node metastasis (LNM), and distant metastasis.
Materials and methods
Patients
This study was conducted at three medical centers, including Fudan University Shanghai Cancer center, Gansu Provincial Cancer Hospital, and the First Hospital of China Medical University, from January 2014 to December 2016. A total of 1997 patients who received thyroidectomy and had a histopathological diagnosis of PTMC were enrolled and reviewed retrospectively. Exclusion criteria were as follows: patients (i) with benign thyroid nodules detected by ultrasound scan before surgery but were accidently identified as PTMC by histopathology, (ii) with a history of thyroid surgery, (iii) with other malignant tumor simultaneously, (iv) aged less than 14 years, (v) without serum TSH concentration measures before surgery. This retrospective cohort study was approved by the local ethical committees. They are the Institutional Ethics Committee of Fudan University Shanghai Cancer Center (1706173–9), the Ethics Committee of Gansu Provincial Cancer Hospital (A201708020011), and the Institutional Ethics Committee of the first Affiliated Hospital of China Medical University (AF-SOP-07–1.1–01). The study was registered in Chinese Clinical Trial Registry (https://www.chictr.org.cn) (Registration Number: ChiCTR1800018108).
PTMC clinicopathological characteristics
Papillary thyroid carcinoma with the greatest tumor diameter of 10 mm or less was classified as PTMC. Information of all the patients with PTMC, including primary tumor size, the number of tumor foci, extrathyroidal extension, LNM, capsular and vascular invasion, and histological variants were recorded. The greatest tumor diameter in histopathological examination was accepted as tumor size. For multifocal tumors, the diameter of the greatest tumor focus was taken as the primary tumor. Staging was performed according to the eighth edition of TNM classification by the AJCC (American Joint Committee on Cancer 8th, 2018).
TSH detection
Serum TSH concentration was measured in all enrolled patients before surgery by immunochemiluminescent methods (IMMULITE 2500, Diagnostic Products Corp., Los Angeles, CA, USA and UniCel DXI800, Beckman Coulter, Brea, CA). The normal range was defined as 0.4–4 mU/L.
Statistical analysis
All variables (including baseline characteristics) are presented as numbers with percentages for categorical variables, mean ± SD for continuous variables. The Student’s t-test was used for comparing numerical variables. The chi-square test was used for comparing categorical variables. Kruskal-Wallis test was used to analyze the difference of tumor size across different preoperative serum TSH concentration groups. Spearman bivariate correlation analysis were used to identify the correlation between TSH and tumor size. Multivariable linear regression analysis was further performed to adjust for effect of TSH on tumor size (age, gender, hypothyroidism, hyperthyroidism, and Levothyroxine treatment). ROC curve was constructed to show the predictive value of preoperative serum TSH for extra-thyroidal extension, LNM, and distant metastasis in patients with PTMC. Statistical analyses were performed in SAS® 9.4. A P-value < 0.05 was accepted as statistical significance.
Results
Patient Characteristics
The baseline characteristics for all the PTMC patients (n = 1997) are presented in Table 1. Average age of patients was 44.6 ± 11.1 years and the median age at surgery was 44.4 years (range: 14.9–80.1, Q1–Q3: 36.2–52.4 years). Most patients were female (n = 1548, 77.5%) and the female to male ratio was 3.45: 1. The median baseline body mass index (BMI) was 23.4 Kg/m2. Among the 1997 patients, 12 (0.6%) with thyroiditis, 37 (1.9%) with hyperthyroidism and 8 (0.4%) with hypothyroidism. All patients had thyroid nodules diagnosed by ultrasound scan before surgery. Median size of thyroid nodules was 6 mm (Q1–Q3: 5.0–8.0 mm). Around 87.3% patients (1734) had normal preoperative serum TSH levels. The average levels of serum TSH was 2.55 ± 2.05 mU/L and the median value was 2.07 mU/L (range: 0–43.4 mU/L, Q1–Q3: 1.36–3.20 mU/L). Ten patients did not have TSH concentration measured before surgery and were thus excluded from further analysis, leaving a total of 1987 individuals (447 male and 1540 female patients) as the study population.
Figure 1 shows the demographics and PTMC prevalence by serum TSH level groups. The prevalence of PTMC was similar across different preoperative serum TSH levels (Fig. 1A). In addition, there was no significant difference in gender (Fig. 1B) and age (Fig. 1C) distribution across the serum TSH levels.
TNM stage in different preoperative serum TSH levels
As shown in Table 2, there is no significant difference in TNM stage according to preoperative serum TSH concentration (p = 0.6039). In detail, when the serum TSH concentration was in the normal range (0.5 < TSH < 4 mIU/L), 1584(98.1%) patients were in T1, 12(0.7%) in T3, and 18 (1.1%) in T4 stage. Similarly, in the lowest TSH concentration (<0.5 mU/L) group, 72 (98.6%) patients were in T1, and one (1.4%) patient was in T3. And in the highest TSH concentration (≥4 mU/L) group, 295 (98.3%) patients were in T1, three patients (1%) were in T3, and two patients (0.7%) were in T4 stage. Meanwhile, most patients were in N0 stage. At the lowest, normal and highest TSH levels, there were 53 (72.6%), 1073 (66.5%), 216 (72.0%) patients in N0, and 20 (27.4%), 541(33.5%), 84 (28.0%) patients in N1 stage, respectively. Furthermore, 16 patients with stage T3b had extra-thyroidal extension invading only strap muscles. And in the patients with T4a, 14 patients had recurrent laryngeal nerve invasion, 4 patients had trachea invasion and two patients had esophagus invasion. Two patients with stage M1 had pulmonary metastasis.
Association between preoperative serum TSH concentration and tumor size
There was a significant difference in tumor size according to the serum TSH concentration (p = 0.0028). In the lowest TSH concentration, the mean tumor size was 6.1 ± 2.54 mm (range: 1–10 mm, Q1–Q3: 4.5–8.0 mm), while in the highest TSH groups, mean tumor size was 6.6 ± 2.22 mm (range: 1–10 mm, Q1–Q3: 5.0–8.0 mm). The average and median tumor size was the largest in the highest TSH concentration group (Table 3). In addition, the results of Spearman correlation analysis illustrated that preoperative serum TSH levels correlated with tumor size (R = 0.0674, P = 0.0030). After adjusting for age, gender, thyroid dysfunction and Levothyroxine treatment, this association was close to and significant (B = 0.0848, SE = 0.0251, 95% CI = 0.0355, 0.134, p = 0.0007).
The effect of TSH on extrathyroidal extension, LNM, and distant metastasis
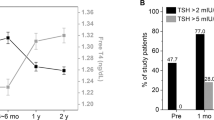
After surgery, 146 patients with extra-thyroidal extension were diagnosed by histopathology: 5 patients (6.9%) in the lowest TSH group, 98 patients (6.1%) in the normal TSH group, and 43 patients (14.3%) were in the highest TSH group. The proportion of extrathyroidal extension in patients with the highest TSH concentration was significantly higher than that in those with normal or lowest TSH concentration (p < 0.0001) (Fig. 2A). A total of 258 patients with LNM were verified by histopathology: 53 patients (17.7%) were in the highest TSH group and the proportion of LNM was significantly higher than that in patients with normal (197, 12.2%) and the lowest (8, 11.0%) TSH levels (p = 0.0402) (Fig. 2B). Two patients developed distant metastasis, and one (0.3%) in the highest TSH level group. However, the difference in distant metastasis prevalence across TSH levels was not statistically significant (p = 0.4498) (Fig. 2C).
Association of serum TSH concentration with PTMC metastasis. A Prevalence of lymph nodes metastasis increased in the higher TSH groups (P < 0.0001). B Prevalence of extrathyroidal invasion increased in the higher TSH groups (P = 0.0402). C Prevalence of distant metastasis increased in the higher TSH groups (P = 0.4498)
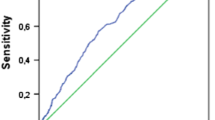
Furthermore, the predictive value of TSH to discriminate PTMC invasion and metastasis was determined by ROC analysis. The area under the curve (AUC) was 0.5814 (Youden index: 0.14) (Fig. 3D). A cut-off value of 2.22 mU/L for TSH had a sensitivity of 57% and a specificity of 57%. When only considering the extrathyroidal extension, the AUC was 0.6427 and Youden index was 0.24, and a cut-off value of 2.25 mU/L for TSH had a sensitivity of 66% and a specificity of 57% (Fig. 3A). And for distant metastasis, the AUC was 0.8372 and Youden index was 0.76, and a cut-off value of 3.28 mU/L for TSH had a sensitivity of 100% and a specificity of 76% (Fig. 3C). However, the results were not significant due to the small sample size.
Diagnostic value of preoperative serum TSH concentration for extrathyroidal invasion, lymph node metastasis and distant metastasis. A ROC curve of preoperative serum TSH level for extrathyroidal invasion. B ROC curve of preoperative serum TSH level for lymph node metastasis. C ROC curve of preoperative serum TSH level for distant metastasis. D ROC curve of preoperative serum TSH level for diagnosis of PTMC invasion and metastasis
Discussion
TSH was once considered as an independent risk factor for different thyroid cancer regardless of the presence of thyroid nodules [19]. Previous clinical studies have demonstrated that elevated preoperative serum TSH concentrations are related to an increased risk of thyroid malignancy [16, 20]. Recently, Tam et al. also identified a positive association between preoperative serum TSH and pathological and aggressive features of PTC [1]. In the study, the authors found that serum TSH was higher in patients with malignant nodules compared to those with benign ones. And patients with aggressive variant PTC had higher serum TSH levels than those with nonaggressive PTC, which confirmed the association between serum TSH and thyroid cancer.
Over the past years, the incidence of thyroid cancer has been rising worldwide because of the increased detection of PTMC [4,5,6]. PTMCs exhibit significant differences in the mode of presentation from papillary tumors of larger size [21]. When compared with larger PTC, PTMC commonly exhibits a more benign behavior and has a more favorable prognosis [22]. However, the risk for extrathyroidal extension (31.9%), lymphatic invasion (19.2%), and lymph node metastasis (17.8%) should not be neglected [23]. Some authors suggested that there exists a subgroup of PTMCs that can be aggressive, requiring therapeutic management similar to that for larger tumors [17]. However, the selection of appropriate patients who need more aggressive therapy is difficult, due to lack of accurate risk stratification.
Although the association between the higher serum TSH and malignancy risk of thyroid nodules has been well established, the relationship of serum TSH concentration and the initiation and progression of PTMC has not been extensively analyzed. Haymart et al. has observed that an increased risk of cancer persisted with a higher TSH in patients with PTMCs until the TSH was ≥ 5.00 mU/L [16]. Similarly, Zafon et al. found that TSH level was the lowest among patients with benign lesions, intermediate among those with PTMC and the highest among those with DTC [17]. There seemingly exists an increment in tumor size as a function of increment in the TSH level in patients with PTMC [24]. However, some limitations should be noted when interpreting the results of these studies. For example, the sample sizes were very small in some studies, or patients with medullary thyroid carcinoma which is known to be unresponsive to TSH were chosen as a control group, or the diagnosis was based on cytological results in a considerable number of patients. Recently, Tam et al. observed patients with benign nodules (n = 969) had significantly lower TSH concentration compared to patients with PTMC (n = 384) and PTC (n = 279). Meanwhile, patients with PTMC and PTC had similar TSH levels [1]. In this study, we found that the average concentration of preoperative serum TSH was 2.55 ± 2.05 mU/L and the median value was 2.07mU/L in patients with PTMC, higher than that of patients with benign pathology reported in other studies (for example, 1.6 ± 0.1 mU/L in the study by Haymart et al. [16], 1.08 mU/L in the study by Shi et al. [21], and 0.98 mU/L in the study by Tam et al. [1]). But there was no significant difference in the prevalence of PTMC according to serum TSH concentration groups.
In addition, there was an association between preoperative serum TSH and more advanced cancer stage at diagnosis [16]. In a meta-analysis of 28 studies and 42032 subjects, the authors systematically assessed the association between serum TSH and thyroid cancer and found a correlation of TSH with higher disease grade even at normal TSH levels [25]. Similarly, Shi et al. showed that higher TSH was also associated with lymph node metastasis and advanced stage (III and IV). Serum TSH could be used as a predictive risk indicator for DTC. However, the use of serum TSH for risk prediction of DTC did not apply to microcarcinomas [21]. Likewise, Kim et al. did not find higher TSH levels in the advanced tumor stage in patients with PTMC during active surveillance [19]. In this study, no significant difference in TNM stage according to preoperative serum TSH concentration was observed.
Although serum TSH did not correlate with the prevalence and TNM stage in PTMC patients, the positive association between serum TSH and tumor size was significant.
Consistently, previous observations by Haymart et al. [16] and Gerschpacher et al. [24] showed a similar positive correlation between the mean serum TSH concentration and tumor size. These findings supported the hypothesis that TSH might be involved in the progression of PTMC.
Furthermore, TSH may play a key role in extra-thyroidal extension and TNM. In a meta-analysis of 56 studies, Zheng et al. showed that higher serum TSH was significantly associated with tumor size and LNM [26]. Recently, Tam et al., showed that preoperative serum TSH was significantly higher in patients with LNM [1]. And Kim et al. further found that sustained increase in serum TSH levels was associated with progression of PTMC during active surveillance, and a cut-off point of serum TSH concentration for PTMC progression was 2.50 mU/L [6]. In this study, we also identified a significantly higher proportion of extra-thyroidal extension and LNM in patients with the highest preoperative serum TSH concentration compared with those with normal or the lowest TSH levels, which indicated an association between preoperative serum TSH levels and extra-thyroidal invasion, diffusion, and LNM in PTMC patients. Our analysis also identified the predictive value of TSH in discriminating PTMC invasion and metastasis, which suggested that serum TSH concentration before surgery may be useful for the prediction of PTMC progression.
Despite the association between serum TSH and PTMC development and progression is still controversial, this multicenter retrospective study with relatively larger sample size (n = 1987) identified a positive trend between preoperative serum TSH and tumor status. A higher serum TSH level might imply more aggressive process in patients with PTMC, including extra-thyroidal invasion, diffusion, and LNM. Therefore, maintaining a low-normal TSH concentration with levothyroxine treatment might be considered for patients with PTMC who received active surveillance.
References
A. Tam, D. Ozdemir, C. Aydın, N. Bestepe, S. Ulusoy, N. Sungu, R. Ersoy, B. Cakir, Association between preoperative thyrotrophin and clinicopathological and aggressive features of papillary thyroid cancer. Endocrine 59(3), 565–572 (2018). https://doi.org/10.1007/s12020-018-1523-6
M. Khan, N. Malik, K. Khan, M. Shahzad, Association of preoperative serum thyroid-stimulating hormone levels with thyroid cancer in patients with nodular thyroid disease. World J. Nucl. Med 16(3), 202–205 (2017). https://doi.org/10.4103/1450-1147.207277
W. Chen, R. Zheng, P.D. Baade, S. Zhang, H. Zeng, F. Bray, A. Jemal, X.Q. Yu, J. He, Cancer statistics in China, 2015. CA: a cancer J. clinicians 66(2), 115–132 (2016). https://doi.org/10.3322/caac.21338
L. Ellison, T. Bushnik, Changing trends in thyroid cancer incidence in Canada: a histologic examination, 1992 to 2016. Health Rep. 31(1), 15–25 (2020). https://doi.org/10.25318/82-003-x202000100002-eng
A. Powers, A. Marcadis, M. Lee, L. Morris, J. Marti, Changes in trends in thyroid cancer incidence in the United States, 1992 to 2016. JAMA 322(24), 2440–2441 (2019). https://doi.org/10.1001/jama.2019.18528
H. Kim, H. Jang, H. Ahn, S. Ahn, S. Park, Y. Oh, S. Hahn, J. Shin, J. Kim, J. Kim, J. Chung, T. Kim, S. Kim, High serum TSH level is associated with progression of papillary thyroid microcarcinoma during active surveillance. J. Clin. Endocrinol. Metab. 103(2), 446–451 (2018). https://doi.org/10.1210/jc.2017-01775
L. He, T. Zeng, L. Pu, S. Pan, W. Xia, L. Chen, Thyroid Hormones, Autoantibodies, Ultrasonography, and Clinical Parameters for Predicting Thyroid Cancer. Int. J. Endocrinol. 2016, 8215834 (2016). https://doi.org/10.1155/2016/8215834
S. Siddiqui, M. White, T. Antic, R. Grogan, P. Angelos, E. Kaplan, N. Cipriani, Clinical and Pathologic Predictors of Lymph Node Metastasis and Recurrence in Papillary Thyroid Microcarcinoma. Thyroid.: Off. J. Am. Thyroid. Assoc. 26(6), 807–815 (2016). https://doi.org/10.1089/thy.2015.0429
G. Grani, V. Ramundo, A. Verrienti, M. Sponziello, C. Durante, Thyroid hormone therapy in differentiated thyroid cancer. Endocrine 66(1), 43–50 (2019). https://doi.org/10.1007/s12020-019-02051-3
D. Kim, J. Park, Clinical implications of preoperative thyrotropin serum concentrations in patients who underwent thyroidectomy for nonfunctioning nodule(s). J. Korean Surgical Soc. 85(1), 15–19 (2013). https://doi.org/10.4174/jkss.2013.85.1.15
D. Cooper, TSH suppressive therapy: an overview of long-term clinical consequences. Hormones (Athens, Greece) 9(1), 57–59 (2010). https://doi.org/10.14310/horm.2002.1259
A. Carhill, D. Litofsky, D. Ross, J. Jonklaas, D. Cooper, J. Brierley, P. Ladenson, K. Ain, H. Fein, B. Haugen, J. Magner, M. Skarulis, D. Steward, M. Xing, H. Maxon, S. Sherman, Long-term outcomes following therapy in differentiated thyroid carcinoma: NTCTCS registry analysis 1987–2012. J. Clin. Endocrinol. Metab. 100(9), 3270–3279 (2015). https://doi.org/10.1210/jc.2015-1346
J. Jonklaas, N. Sarlis, D. Litofsky, K. Ain, S. Bigos, J. Brierley, D. Cooper, B. Haugen, P. Ladenson, J. Magner, J. Robbins, D. Ross, M. Skarulis, H. Maxon, S. Sherman, Outcomes of patients with differentiated thyroid carcinoma following initial therapy. Thyroid.: Off. J. Am. Thyroid. Assoc. 16(12), 1229–1242 (2006). https://doi.org/10.1089/thy.2006.16.1229
B. Haugen, E. Alexander, K. Bible, G. Doherty, S. Mandel, Y. Nikiforov, F. Pacini, G. Randolph, A. Sawka, M. Schlumberger, K. Schuff, S. Sherman, J. Sosa, D. Steward, R. Tuttle, L. Wartofsky, 2015 American thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The American Thyroid Association Guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid.: Off. J. Am. Thyroid. Assoc. 26(1), 1–133 (2016). https://doi.org/10.1089/thy.2015.0020
M. Haymart, N. Esfandiari, M. Stang, J. Sosa, Controversies in the management of low-risk differentiated thyroid cancer. Endocr. Rev. 38(4), 351–378 (2017). https://doi.org/10.1210/er.2017-00067
M. Haymart, D. Repplinger, G. Leverson, D. Elson, R. Sippel, J. Jaume, H. Chen, Higher serum thyroid stimulating hormone level in thyroid nodule patients is associated with greater risks of differentiated thyroid cancer and advanced tumor stage. J. Clin. Endocrinol. Metab. 93(3), 809–814 (2008). https://doi.org/10.1210/jc.2007-2215
C. Zafon, G. Obiols, J.A. Baena, J. Castellvi, B. Dalama, J. Mesa, Preoperative thyrotropin serum concentrations gradually increase from benign thyroid nodules to papillary thyroid microcarcinomas then to papillary thyroid cancers of larger size. J. thyroid Res. 2012, 530721 (2012). https://doi.org/10.1155/2012/530721
I. Sugitani, Y. Fujimoto, K. Yamada, Association between serum thyrotropin concentration and growth of asymptomatic papillary thyroid microcarcinoma. World J. Surg. 38(3), 673–678 (2014). https://doi.org/10.1007/s00268-013-2335-8
H.K. Kim, J. Yoon, S. Kim, J. Cho, S. Kweon, H. Kang, Higher TSH level is a risk factor for differentiated thyroid cancer. Clin. Endocrinol. 78(3), 472–477 (2013). https://doi.org/10.1111/cen.12027
K. Boelaert, J. Horacek, R. Holder, J. Watkinson, M. Sheppard, J. Franklyn, Serum thyrotropin concentration as a novel predictor of malignancy in thyroid nodules investigated by fine-needle aspiration. J. Clin. Endocrinol. Metab. 91(11), 4295–4301 (2006). https://doi.org/10.1210/jc.2006-0527
L. Shi, Y. Li, H. Guan, C. Li, L. Shi, Z. Shan, W. Teng, Usefulness of serum thyrotropin for risk prediction of differentiated thyroid cancers does not apply to microcarcinomas: results of 1,870 Chinese patients with thyroid nodules. Endocr. J. 59(11), 973–980 (2012). https://doi.org/10.1507/endocrj.ej12-0154
M. Jeon, W. Kim, K. Chung, J. Baek, W. Kim, Y. Shong, Active surveillance of papillary thyroid microcarcinoma: where do we stand? Eur. thyroid J. 8(6), 298–306 (2019). https://doi.org/10.1159/000503064
D. Lim, K. Baek, Y. Lee, W. Park, M. Kim, M. Kang, H. Jeon, J. Lee, C.B. Yun, K. Lee, H. Son, S. Kang, Clinical, histopathological, and molecular characteristics of papillary thyroid microcarcinoma. Thyroid.: Off. J. Am. Thyroid. Assoc. 17(9), 883–888 (2007). https://doi.org/10.1089/thy.2007.0001
M. Gerschpacher, C. Göbl, C. Anderwald, A. Gessl, M. Krebs, Thyrotropin serum concentrations in patients with papillary thyroid microcancers. Thyroid.: Off. J. Am. Thyroid. Assoc. 20(4), 389–392 (2010). https://doi.org/10.1089/thy.2009.0139
D.S. McLeod, K.F. Watters, A.D. Carpenter, P.W. Ladenson, D.S. Cooper, E.L. Ding, Thyrotropin and thyroid cancer diagnosis: a systematic review and dose-response meta-analysis. J. Clin. Endocrinol. Metab. 97(8), 2682–2692 (2012). https://doi.org/10.1210/jc.2012-1083
J. Zheng, C. Li, W. Lu, C. Wang, Z. Ai, Quantitative assessment of preoperative serum thyrotropin level and thyroid cancer. Oncotarget 7(23), 34918–34929 (2016). https://doi.org/10.18632/oncotarget.9201
Acknowledgements
We thank Ms. Haili Cao and Ms. Yuanyuan Zhao (Gansu Provincial cancer hospital, China), for their expert technical assistance and administrative support. A special thank goes to Ying Liu, Meifang Ruan, and Chen Zhang, for their expert statistical analysis and support. The appreciation also goes to the anonymous peer reviewers for providing constructive comments that strengthened the presentation of this work.
Author information
Authors and Affiliations
Contributions
Z.Y.W., J.W., and H.X.G. conceived and designed this study. An.N., Wu Y.Y.W., and J.W. performed the study. A.M. and T.W. performed data analysis and interpretation. A.M. and J.W. wrote the manuscript. All authors have read and approved the final version of the manuscript.
Funding
This research was supported by Merk Serono Co., Ltd, China (an affiliate of Merck KGaA Darmstadt, Germany), Gansu provincial Science and Technology Project (20YF3FA021), Gansu Health Project (GSWSKY-2017-13, GSWSKY-2018-05, and GSWSKY-2018-66), and Lanzhou Science and Technology Development Guiding Plan Project (2018-ZD-39). The sponsor has no role in this study design, implementation, data analysis, and manuscript drafting.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. This article does not contain any animal studies performed by any of the authors.
Consent to participate
The patients provided written informed consent for disclosing clinical and imaging data.
Ethics approval
All procedures were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. And the study was approved by the local ethical committees.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Aihong Mao, Ning An
Rights and permissions
About this article
Cite this article
Mao, A., An, N., Wang, J. et al. Association between preoperative serum TSH and tumor status in patients with papillary thyroid microcarcinoma. Endocrine 73, 617–624 (2021). https://doi.org/10.1007/s12020-021-02690-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-021-02690-5