Abstract
Heart type fatty acid binding protein (H-FABP) is a major cytoplasmic low-molecular weight protein and released into the circulation when the myocardium is injured. Previous studies have demonstrated that H-FABP is closely associated with acute coronary syndrome, hypertrophic and dilated cardiomyopathy, heart failure, stroke, obstructive sleep apnea syndrome, pulmonary embolism. The aim of this study was to investigate serum H-FABP value in the patients with metabolic syndrome (MetS). We measured serum H-FABP levels in 55 consecutive patients with MetS, and 73 age-matched control subjects by using a sandwich enzyme-linked immunosorbent assay. Serum H-FABP levels were significantly higher in patients with MetS than in control subjects 18.37 ± 13.0 and 7.9 ± 6.5 ng/ml, respectively, (P < 0.001). Serum H-FABP levels were significantly higher in patients with diabetic MetS than in without diabetic MetS, 24.0 ± 10.2 and 13.9 ± 12.6 ng/ml, respectively, (P: 0,003). There were statistically significant differences between patients without diabetic MetS and control subjects, 13.8 ± 12.6 and 7.9 ± 6.5 ng/ml, respectively, (P = 0.023). Patients with MetS have an increased risk of death from cardiovascular diseases. H-FABP seems to be a marker that will enable the detection of cardiac injury in the early asymptomatic period in patients with MetS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Insulin resistance, dyslipidemia, hypertension, and impairment of glucose homeostasis are closely linked to obesity, forming a cluster of abnormalities well known as metabolic syndrome (MetS) that is associated with increased atherosclerotic cardiovascular disease [1]. Although, major cardiovascular events are the first clinical manifestation of coronary artery disease in more than half of individuals, these acute coronary events occur after long preceding periods of subclinical disease development [2].
Heart type fatty acid binding protein (H-FABP), which is abundant in the cytosol of cardiomyocytes, transports fatty acids in cardiomyocytes. It is a powerful regulator of the mitochondrial beta-oxidative system [3]. It is undetectable in normal conditions but is released rapidly from cardiomyocytes into circulating blood after myocardial damage. Molecular size and intracellular location are also important factors determining the plasma kinetic release of cardiac biomarkers. Small cytoplasmic molecules H-FABP (15 kD) rise earlier (2–4 h) than bigger ones mainly associated with myofibrils as cardiac troponins (6–12 h) [4, 5]. Therefore, H-FABP has been used diagnostic marker for acute coronary syndromes. On the other hand, previous studies have demonstrated that serum level of H-FABP is increased in patients with hypertrophic and dilated cardiomyopathy, heart failure, stroke, obstructive sleep apnea syndrome, pulmonary embolism [5–11].
In the present study, we tested the hypothesis that serum H-FABP level is detectable in the circulation of patients with MetS, and may be associated with subclinical atherosclerosis.
Materials and methods
After getting approval of the Ethics Committee of Diskapi Education and Research Hospital, we studied 55 MetS (mean age 55 ± 9.0 years) patients and 73 age-matched healthy control subjects (mean age 50 ± 8.0 years). The patients had been referred to the Endocrinology and Metabolism Disease outpatient clinic at the Diskapi Education and Research Hospital.
MetS was defined according to the revised National Cholesterol Education Program Adult Treatment Panel III criteria [12]. The individual components were waist circumference 88 cm for women or 102 cm for men, glucose 100 mg/dl, blood pressure 130/80 or on medication for hypertension, high-density lipoprotein (HDL) <40 mg/dl (men) or <50 mg/dl (women), and triglycerides 150 mg/dl. The MetS patients were randomised as diabetic (n = 27) and nondiabetic (n = 28), respectively. All patients underwent a standard questionnaire, physical examination. Patients with the history of acute coronary syndrome, heart failure, pulmonary embolism, stroke, cardiomyopathy, renal, immunological diseases, or those who were on drugs due to disease, were excluded from the study. The control group was composed of volunteers who did not have a history of cardiological disease, acute coronary syndrome, heart failure, pulmonary embolism, stroke, cardiomyopathy, renal, immunological diseases, diabetes mellitus, and MetS.
Heart type fatty acid binding protein
The H-FABP quantitative test is based on a solid phase enzyme-linked immunosorbent assay. The assay system utilizes an affinity-purified goat anti-H-FABP antibody for solid phase (microtiter wells) immobilization and anti-H-FABP antibody of the same goat in the antibody–enzyme (horseradish peroxidase) conjugate solution. The test sample is allowed to react simultaneously with the antibodies, resulting in H-FABP molecules being sandwiched between the solid phase and enzyme-linked antibodies. After 60-min incubation at room temperature in an orbital shaker, the wells are washed with distilled water to remove unbound-labeled antibodies. A solution of tetramethylbenzidine (TMB) reagent is added and incubated for 20 min at room temperature, resulting in the development of a blue color. The color development is stopped with the addition of Stop solution, and the color is changed to yellow and measured spectrophotometrically at 450 nm. The concentration of H-FABP is proportional to the color intensity of the test sample. Coefficient of variation for the H-FABP assay was 7–8% for intra-assay and 9.3–12.6% for inter-assay.
Blood sample collections
A fasting venous blood sample was obtained for glucose (hexokinase method using Autoanalyser AU5200), triglycerides (glycerophosphate oxidase method using Autoanalyser AU5200), and HDL cholesterol (spectrophotometric method using Roche-Hitachi Modular P device) measurement.
Statistical analyses
Data analyses were performed with SPSS 15.0 for Windows. The continuous variables (age, body mass index, HDL-C, systolic blood pressure, diastolic blood pressure, fasting blood glucose, waist circumferences, triglyceride, blood urea nitrogen and creatinine) were presented as mean ± standard deviation (SD), whereas categorical variables (sex, history of diabetes mellitus, hypertension and hypertriglyceridemia) were presented as %. The Student’s t or Mann–Whitney tests were used in order to determine if there were any significant differences between groups. The Student’s t-test was used to compare and analyze differences in continuous variables that had a normal distribution (age, waist circumferences, HDL-C, body mass index). On the other hand, the variables without normal distribution (systolic blood pressure, diastolic blood pressure, fasting blood glucose, triglyceride, creatinine, blood urea nitrogene) were tested by Mann–Whitney test. Chi-square test was used to compare the sex distribution between MetS and control groups. Categorical variables with less than 5 cases (history of diabetes mellitus, hypertension, hypertriglyceridemia) were compared by Fisher’s Exact test. When there were more than two groups, the significance of the difference between groups in terms of continuous variables was investigated using the Kruskall–Wallis test and post hoc Mann–Whitney U test. The significance of a linear relation between the H-FABP and MetS components was evaluated by Spearman’s correlation test. P < 0.05 was accepted as statistically significant for the results.
Results
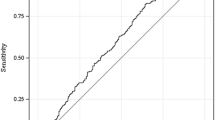
The demographic and biochemical features in patients with MetS and normal control subjects are shown in Table 1. Serum H-FABP levels were significantly elevated in MetS patients when compared with control subjects, respectively, (18.37 ± 13.0 ng/ml, 7.9 ± 6.5 ng/ml, P < 0.001). The patients with MetS were divided into two groups based on the presence or absence of diabetes mellitus (n = 27, n = 28). We compared serum H-FABP levels for both groups. Serum levels of H-FABP were higher in patients with diabetic MetS than in patients without diabetic MetS, respectively, (24.0 ± 10.2 ng/ml, 13.9 ± 12.6 ng/ml, P = 0,003) (Fig. 1). There were significant differences between nondiabetic MetS patients and control subjects, respectively, (13.8 ± 12.6 ng/ml, 7.9 ± 6.5 ng/ml, P = 0.023) (Fig. 2). A significant positive correlation was found between H-FABP and waist circumference, in the MetS subjects (r = 0.434, P = 0,001). No significant correlations were identified between H-FABP and the other of MetS parameters.
Discussion
The present study confirms that the increased serum levels of H-FABP are detected in patients with MetS, and for the first time, demonstrates that elevated circulating serum levels of H-FABP may provide important prognostic information in patients with MetS.
H-FABP is a 15 kDa protein that mediates the passage of the fatty acids from the plasma membrane to sites of lipid synthesis. It was reported that H-FABP is a potent inducer of cardiac myocyte hypertrophy, stimulating an increase in cell surface area, protein synthesis, and c-jun expression [13]. H-FABP has been introduced as a new specific serum bio-marker for acute myocardial infarction [14, 15]. H-FABP is more specific for heart muscle than are other types of fatty acid binding protein [16, 17]. Nakata et al. [18] demonstrated that serum H-FABP can be early diagnostic and prognostic bio-chemical marker, particularly within the first 6 h from the onset of chest symptoms, in acute coronary syndrome. Arimoto et al. [19] demonstrated that serum H-FABP levels are increased in heart failure patients, are related to the severity of heart failure, and may be novel independent prognostic information irrespective of functional class. Tambara et al. [20] reported that pericardial fluid levels of H-FABP reflected myocardial ischemia within 24 h of their measurements, and may be secreted into the interstitial space, associated with severe myocardial ischemia.
Alhadi et al. [21] concluded that H-FABP is a sensitive marker for the detection of acute myocardial infarction, but is not 100% cardiac-specific, because of its presence in tissues outside the heart. In renal failure and skeletal muscle disease, it has limited diagnostic value.
In our study, serum H-FABP levels were significantly elevated in MetS patients when compared with control subjects (18.3 ± 13.0 and 7.9 ± 6.5 ng/ml, respectively, P < 0.001). Our findings also suggest that an elevated circulating level of H-FABP is not only a highly sensitive and specific marker of myocardial damage, but also an important prognostic determinant in patients with MetS. However, an elevated circulating level of H-FABP can reflect early identification of subclinical atherosclerosis in patients with MetS.
Alexander et al. [22] have reported that MetS with diabetes is associated with the highest prevalence of coronary heart disease compared with MetS without diabetes in ≥50 years of age. Iglseder et al. [23] demonstrated that the effect of MetS on early atherosclerosis is more pronounced in women than in men because of the strong link between MetS and type 2 diabetes.
In our study, serum H-FABP levels were significantly elevated in patients with diabetic MetS when compared in patients without diabetic MetS (24.0 ± 10.2 ng/ml and 13.9 ± 12.6 ng/ml, respectively, P = 0.003). These data suggest that an elevated level of H-FABP can identify those with diabetic MetS who are at increased risk of atherosclerotic cardiovascular events, and patients with diabetic MetS may warrant more aggressive therapy. Moreover, a significant positive correlation was found between H-FABP and waist circumference, in the MetS subjects (r = 0.434, P = 0.001). This suggests that the components of MetS and type 2 diabetes can affect serum H-FABP levels.
Screening for subclinical atherosclerosis using new imaging technologies or novel biomarkers could help to further risk-stratify patients with MetS. In particular, noninvasive imaging of carotid intima-media thickness (CIMT) and coronary artery calcium (CAC) scoring seem to have promising prognostic value in identifying patients at high risk [24–27].
In conclusion, as far as we are aware, the present study is the first case–control study in which significant alteration in serum H-FABP levels were detected in patients with MetS. H-FABP may be used as a diagnostic serum marker in patients with MetS to determine subclinical atherosclerosis. Further studies are required to investigate the relation between the value of H-FABP and the development of cardiac dysfunction in patients with MetS in the long term period.
Abbreviations
- BMI:
-
Body mass index
- CVD:
-
Cardiovascular disease
- HDL-C:
-
High-density lipoprotein cholesterol
- TG:
-
Triglycerides
- CIMT:
-
Carotis intima-media thickness
- H-FABP:
-
Heart type fatty acid binding protein
- CAC:
-
Coronary artery calcium
- MetS:
-
Metabolic syndrome
References
S.M. Grundy, Obesity, metabolic syndrome, and cardiovascular disease. J. Clin. Endocrinol. Metab. 89, 2595–2600 (2004)
P. Schoenhagen, S.E. Nissen, Identification of the metabolic syndrome and imaging of subclinical coronary artery disease: early markers of cardiovascular risk. J. Cardiovasc. Nurs. 21, 291–297 (2006)
N.C. Fournier, M.A. Richard, Role of fatty acid-binding protein in cardiac fatty acid oxidation. Mol. Cell. Biochem. 98, 149–159 (1990)
M.M. Pelsers, W.T. Hermens, J.F. Glatz, Fatty acid-binding proteins as plasma markers of tissue injury. Clin. Chim. Acta 352, 15–35 (2005)
D. Nagahara, T. Nakata, A. Hashimoto, T. Takahashi, M. Kyuma, M. Hase, K. Tsuchihashi, K. Shimamoto, Early positive biomarker in relation to myocardial necrosis and impaired fatty acid metabolism in patients presenting with acute chest pain at an emergency room. Circ. J. 70, 419–425 (2006)
T. Arimoto, Y. Takeishi, T. Niizeki, N. Nozaki, O. Hirono, T. Watanabe, J. Nitobe, Y. Tsunoda, S. Suzuki, Y. Koyama, T. Kitahara, A. Okada, K. Takahashi, I. Kubota, Cardiac sympathetic denervation and ongoing myocardial damage for prognosis in early stages of heart failure. J. Card. Fail. 13, 34–41 (2007)
T. Niizeki, Y. Takeishi, N. Takabatake, Y. Shibata, T. Konta, T. Kato, S. Kawata, I. Kubota, Circulating levels of heart-type fatty acid-binding protein in a general Japanese population: effects of age, gender, and physiologic characteristics. Circ. J. 71, 1452–1457 (2007)
K. Komamura, T. Sasaki, A. Hanatani, J. Kim, K. Hashimura, Y. Ishida, Y. Ohkaru, K. Asayama, T. Tanaka, A. Ogai, T. Nakatani, S. Kitamura, K. Kangawa, K. Miyatake, M. Kitakaze, Heart-type fatty acid binding protein is a novel prognostic marker in patients with non-ischaemic dilated cardiomyopathy. Heart 92, 615–628 (2006)
M.T. Wunderlich, T. Hanhoff, M. Goertler, F. Spener, J.F. Glatz, C.W. Wallesch, M.M. Pelsers, Release of brain-type and heart-type fatty acid-binding proteins in serum after acute ischaemic stroke. J. Neurol. 252, 718–724 (2005)
B. Renaud, A. Ngako, Heart-type fatty acid-binding proteins (H-FABP): a reliable tool for initial risk stratification of pulmonary embolism? Eur. Heart J. 28, 146–157 (2007)
B. Oktay, E. Akbal, H. Firat, S. Ardic, R. Akdemir, M. Kizilgun, Evaluation of the relationship between heart type fatty acid binding protein levels and the risk of cardiac damage in patients with obstructive sleep apnea syndrome. Sleep Breath 12, 223–228 (2008)
S.M. Grundy, J.I. Cleeman, S.R. Daniels, K.A. Donato, R.H. Eckel, B.A. Franklin, D.J. Gordon, R.M. Krauss, P.J. Savage, S.C. Smith Jr, J.A. Spertus, F. Costa, Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute scientific statement. Circulation 112, 2735–2752 (2005)
P.B. Burton, C.E. Hogben, C.L. Joannou, A.G. Clark, J.J. Hsuan, N.F. Totty, C. Sorensen, R.W. Evans, M.J. Tynan, Heart Fatty acid binding protein is a novel regulator of cardiac myocyte hyperthyrophy. Biochem. Biophys. Res. Commun. 305, 1822–1828 (1994)
T. Tanaka, Y. Hirota, K. Sohmiya, S. Nishimura, K. Kawamura, Serum and urinary human heart fatty acid-binding protein in acute myocardial infarction. Clin. Biochem. 24, 195–201 (1991)
J.F. Glatz, A.H. Kleine, F.A. van Nieuwenhoven, W.T. Hermens, M.P. van Dieijen-Visser, G.J. van der Vusse, Fatty acid-binding protein as a plasma marker fort he estimation of myocardial infarct size in humans. Br. Heart J. 71, 135–140 (1994)
K. Yoshimoto, T. Tanaka, K. Somiya, R. Tsuji, F. Okamoto, K. Kawamura, Y. Ohkaru, K. Asayama, H. Ishii, Human heart-type cytoplasmic fatty acid-binding protein as an indicator of acute myocardial infarction. Heart Vessels 10, 304–309 (1995)
F. Okamoto, K. Sohmiya, Y. Ohkaru, K. Kawamura, K. Asayama, H. Kimura, S. Nishimura, H. Ishii, N. Sunahara, T. Tanaka, Human heart-type cytoplasmic fatty acid-bindingprotein (H-FABP) for the diagnosis of acute myocardial infarction. Clinical evaluation of H-FABP in comparison with myoglobin and creatine kinase isoenzyme MB. Clin. Chem. Lab. Med. 38, 231–238 (2000)
T. Nakata, A. Hashimoto, M. Hase, K. Tsuchihashi, K. Shimamoto, Human heart-type fatty acid-binding protein as an early diagnostic and prognostic marker in acute coronary syndrome. Cardiology 99, 96–104 (2003)
T. Arimoto, Y. Takeishi, R. Shiga, A. Fukui, H. Tachibana, N. Nozaki, O. Hirono, J. Nitobe, T. Miyamoto, B.D. Hoit, I. Kubota, Prognostic value of elevated circulating heart-type fatty acid binding protein in patients with congestive heart failure. J. Card. Fail. 11, 56–60 (2005)
K. Tambara, M. Fujita, S. Miyamoto, K. Doi, K. Nishimura, M. Komeda, Pericardial fluid level of heart-type cytoplasmic fatty acid-binding protein (H-FABP) is an indicator of severe myocardial ischemia. Int. J. Cardiol. 93, 281–284 (2004)
K. Alhadi, K.A. Fox, Do we need additional markers of myocytenecrosis: the potential value of heart fatty-acid-binding protein. QJM 97, 187–198 (2004)
C.M. Alexander, P.B. Landsman, S.M. Teutsch, S.M. Haffner, Third National Health and Nutrition Examination Survey (NHANES III); National Cholesterol Education Program (NCEP). NCEP-defined metabolic syndrome, diabetes, and prevalence of coronary heart disease among NHANES III participants age 50 years and older. Diabetes 52, 1210–1214 (2003)
B. Iglseder, P. Cip, L. Malaimare, G. Ladurner, B. Paulweber, The metabolic syndrome is a stronger risk factor for early carotid atherosclerosis in women than in men. Stroke 36, 1212–1217 (2005)
A.I. Del Sol, K.G. Moons, M. Hollander, A. Hofman, P.J. Koudstaal, D.E. Grobbee, M.M. Breteler, J.C. Witteman, M.L. Bots, Is carotid intima-media thickness useful in cardiovascular disease risk assessment? The Rotterdam Study. Stroke 32, 1532–1538 (2001)
J.A. Hoff, M.L. Daviglus, E.V. Chomka, A.J. Krainik, A. Sevrukow, G.T. Kondos, Conventional coronary artery disease risk factors and coronary artery calcium detected by electron beam tomography in 30.908 healthy individuals. Ann. Epidemiol. 13, 163–169 (2003)
M.J. Budoff, K.M. Gul, Expert review on coronary calcium. Vasc. Health Risk Manag. 4, 315–324 (2008)
A. Adolphe, L.S. Cook, X. Huang, A cross-sectional study of intima-media thickness, ethnicity, metabolic syndrome, and cardiovascular risk in 2268 study participants. Mayo Clin. Proc. 84, 221–228 (2009)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Akbal, E., Özbek, M., Güneş, F. et al. Serum heart type fatty acid binding protein levels in metabolic syndrome. Endocr 36, 433–437 (2009). https://doi.org/10.1007/s12020-009-9243-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-009-9243-6