Abstract
A number of studies have investigated the association between tumor necrosis factor (TNF)-α gene polymorphisms and ischemic stroke susceptibility. However, results of different individual studies are often inconsistent. To provide a more robust evaluation of the association between polymorphisms of the TNF-α gene and ischemic stroke risk, we performed a systematic review with multivariate meta-analyses. PubMed, Embase, CNKI, and WanFang databases were searched up to December 20, 2014. Two reviewers independently extracted information and assessed quality of included studies after all the eligible studies were identified. Afterward, multivariate meta-analyses were performed using Stata 13. The estimation of polymorphisms and disease risk was presented by odds ratios (ORs) and corresponding 95 % confidence intervals (CIs). Forty-nine eligible case–control studies from 25 articles that explored the association between 10 TNF-α polymorphisms and ischemic stroke were indentified from aforementioned databases. The results of multivariate meta-analysis showed a significant association between −238G/A polymorphism (4760 patients and 4389 controls) and ischemic stroke risk in heterozygotes compared with wild genotype (AG vs. GG: OR 1.44, 95 % CI 1.11–1.87; AA vs. GG: OR 1.98, 95 % CI 0.73–5.40). No significant association of −308G/A, −857C/T, and −1031T/C polymorphisms was observed. The results of stratification analyses of −238G/A polymorphism showed that the AG genotype only increased the risk of ischemic stroke in Asians compared to GG genotype. No additional significant association was observed in this study. In conclusion, the present systematic review and meta-analysis support a prominent role of the TNF-α −238G/A polymorphism in the risk of ischemic stroke in Asian adults only, but do not support the role of −308G/A, −857C/T, −1031T/C, −244G/A, −367G/A, −646G/A, −806C/T, −863C/A, and +448G/A in the risk of ischemic stroke. The current evidence warrants further studies with high quality and large sample size to confirm.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ischemic stroke is a complex disease and pathologically based on atherosclerosis that caused by interplay or interaction of genetic effects and environmental factors, which is an increasing global and regional burden (Lopez et al. 2006). Researchers have suggested that inflammation had a predominant role in the development and rupture of atherosclerotic lesions, resulting in cardiovascular disease events (Packard and Libby 2008). The tumor necrosis factor (TNF)-α, one of the most typical pro-inflammatory cytokines, plays a vital role in inflammation and cell signaling (Bayley et al. 2004).
Many studies have investigated the association between TNF-α polymorphisms and ischemic stroke susceptibility. However, existing evidence is often inconsistent. In 2007, Pereira et al. (2007) performed a meta-analysis that investigated the TNF-α −308G/A polymorphism on the risk of ischemic stroke with eight case–control studies, and they suggested that the −308G/A polymorphism was a protective factor for ischemic stroke in Asians only. This is not in agreement with the subsequent meta-analysis performed by Gu et al. (2013b) with 13 studies, which suggested that −308G/A polymorphism was associated with the risk of juvenile ischemic stroke, and it was a protective factor for ischemic stroke in Asians and adult population. Afterward, Gu et al. (2013a) carried out another meta-analysis with seven studies for TNF-α −238G/A polymorphism, and they found that −238G/A polymorphism increased the risk of ischemic stroke in adults and Caucasians. Moreover, there are many other mutations identified in TNF-α, such as −857C/T and −1031T/C. In addition, certain more recent studies have since been published. Therefore, we performed this systematic review by multivariate meta-analysis to evaluate up-to-date estimates of the gene effect on ischemic stroke.
Methods
This study follows the Meta-analysis of Observational Studies in Epidemiology (MOOSE) statement (Stroup et al. 2000).
Literature Search
A comprehensive electronic search of PubMed, Embase, China National Knowledge Infrastructure, and WanFang databases was performed up to December 20, 2014. The following medical subject headings, terms, and text words were used in combination with each other: (“tumor necrosis factor” OR TNF) AND (polymorphism OR allele OR mutation) AND (“cerebrovascular disease” OR stroke OR “cerebrovascular disorder” OR “brain infarction” OR “ischemic stroke”). The search results were limited to humans. In addition, all references in the identified articles and recent reviews were retrieved manually for any further possible related studies.
Eligibility Criteria
Studies that met the following criteria were included in the present study: (1) Patients had magnetic resonance imaging or computer tomography confirmation of an ischemic stroke diagnosis; (2) the theme of study was to investigate the relationship between TNF-α polymorphisms and ischemic stroke susceptibility; (3) the study design was case–control or cohort; and (4) the study reported sufficient data for each genotypes in both case and control groups. No language restriction was implemented.
Studies were excluded if: (1) genotype data were not reported, in which case authors were contacted for these data where possible; (2) they contained overlapping data or duplicate publication; and (3) they included patients with other systemic diseases, such as sickle cell anemia.
Data Extraction and Quality Assessment
Two reviewers (Y-MN and HW) independently performed study selection and data extraction according to the prespecified eligible criteria. The inter-examiner consistency was detected by κ test (p = 0.97). The following data were extracted from each identified study: author, year of publication, study location, ethnicity and age of study subjects, number of sample size, phenotype of ischemic stroke, genotype distribution of each group, source of control, and other information for quality assessment. Any discrepancy was settled by consensus.
The quality assessment (Zeng et al. 2015) of included studies was performed independently by two authors (HW and CZ; p = 0.94 for κ test) according to the redefined criteria (Table 1) from the previous meta-analyses (Lu et al. 2014; Thakkinstian et al. 2005). Quality scores range from 0 to 11 points.
Statistical Analysis
First, the major allele frequencies of TNF-α polymorphisms in various racial groups (Asians and Caucasians) were estimated by random effects model inverse variance (I–V) method, as described by Thakkinstian et al. (2005). In addition, Hardy–Weinberg equilibrium (HWE) in controls in each study was detected by Chi-square test or Fisher’s exact test.
Second, the association between the gene effect (mutant alleles or genotypes) and ischemic stroke was estimated by odds ratios (ORs) and corresponding 95 % confidence intervals (CIs). Adding 0.5 (a continuity correction) to all cells of the contingency table was implemented in the case of a zero event (Friedrich et al. 2007). The between-study heterogeneity was assessed using Cochran’s Q statistic and I 2 metric (Higgins et al. 2003). Data were pooled using a random effects model with I–V method (to evaluate between-study variance—τ 2). Additionally, the present study also performed a more advanced method—the multivariate random effects meta-analysis—for estimating gene–disease associations (Bagos 2008). In this procedure, the two pooled logORs related to the risk allele, e.g., log(AG vs. GG) and log(AA vs. GG) for −308G/A, were modeled simultaneously as a bivariate response. Afterward, the ratio λ of the two logORs was calculated, e.g., λ = log(AG vs. GG)/log(AA vs. GG) for −308G/A. The genetic model of inheritance was inferred and quantified directly by the ratio λ (values of λ equal to 0, 0.5, and 1 correspond to the recessive, codominant, and dominant genetic model, respectively; if λ is <0 or >1, an overdominant model is suggested; i.e., a parsimonious approach) (Minelli et al. 2005a, b; Braliou et al. 2014), which could avoid multiple testing and the inflation of the type I error rate. Besides the finest genetic model, the remaining genetic models were also assessed. Sensitivity analysis was performed by including and excluding the study controls inconsistent in HWE. Subgroup analyses were implemented based on ethnicity and age of study subjects.
Funnel plot and Egger’s linear regression method were used to estimate possible publication bias (Egger et al. 1997). Cumulative meta-analyses were also conducted for the purpose of identifying a possible trend of the pooled estimate over years (“Proteus phenomenon”) (Bagos and Nikolopoulos 2009). All the statistical analyses were performed using Stata 13 (StataCorp). Results with a two-side p value <0.05 were considered statistically significant.
Results
Study Selection and Characteristics
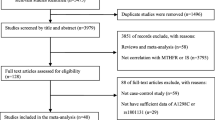
Figure 1 shows the results of literature search and selection. A total of 186 articles were retrieved with the comprehensive literature search, and finally 25 articles (Bai and Cheng 2004; Balding et al. 2004; Lee et al. 2004; Um and Kim 2004; Karahan et al. 2005; Rubattu et al. 2005; Harcos et al. 2006; Lalouschek et al. 2006; Llamas Sillero et al. 2007; Zhang et al. 2007; Li et al. 2009; Liu et al. 2009, 2012; Shi et al. 2009; Kim et al. 2010; Tong et al. 2010; Markoula et al. 2011; Munshi et al. 2011; Sultana et al. 2011; Szabo and Acsady 2011; Wu et al. 2011; Cui et al. 2012; Tuttolomondo et al. 2012; Gelfand et al. 2013; Ma 2012) (18 in English and seven in Chinese) of them were included in the present study according to the eligible criteria. Forty-nine eligible case–control studies from these 25 articles involve 23 studies of −308G/A (6220 patients and 6531 controls), 14 studies of −238G/A (4760 patients and 4389 controls), four studies of −857C/T (2589 patients and 2097 controls), three studies of −1031T/C (2416 patients and 1948 controls), one study (404 patients and 415 controls) of −244G/A and −367G/A, one study (67 patients and 70 controls) of −646G/A, −806C/T, −863C/A, and one study (525 patients and 500 controls) of +448G/A. If the number of studies was more than 3, we then pooled the gene effect for ischemic stroke; therefore, the −244G/A, −367G/A, −646G/A, −806C/T, −863C/A, and +448G/A polymorphisms were not pooled due to little data. The general characteristics of included studies are shown in Table 2.
Major Allele Frequencies in Control Groups
−308G Allele
Twenty-three case–control studies from 19 articles (Bai and Cheng 2004; Balding et al. 2004; Lee et al. 2004; Um and Kim 2004; Karahan et al. 2005; Rubattu et al. 2005; Harcos et al. 2006; Lalouschek et al. 2006; Llamas Sillero et al. 2007; Zhang et al. 2007; Li et al. 2009; Kim et al. 2010; Tong et al. 2010; Sultana et al. 2011; Szabo and Acsady 2011; Cui et al. 2012; Tuttolomondo et al. 2012; Gelfand et al. 2013; Ma 2012) reported G allele frequencies, with 13 studies of Asian adults, one of Asian children, seven of Caucasian adults, and two of Caucasian children. Of these, six studies (Um and Kim 2004; Zhang et al. 2007; Li et al. 2009; Tong et al. 2010; Sultana et al. 2011; Ma 2012) in Asian adults were not consistent in HWE. The pooled frequency of G allele in Asian controls was 90.3 % (95 % CI 87.8–92.8 %) under random effects model with I–V method, with some evidence of heterogeneity between studies (I 2 = 91.6 %, p < 0.001, between-study variance τ 2 = 0.002). The pooled frequency among Caucasian controls was 85.3 % (95 % CI 80.5–90.0 %), with some between-study heterogeneity existed (I 2 = 97.6 %, p < 0.001, τ 2 = 0.005).
−238G Allele
Fourteen case–control studies from 11 articles (Lalouschek et al. 2006; Llamas Sillero et al. 2007; Li et al. 2009; Liu et al. 2009; Shi et al. 2009; Kim et al. 2010; Tong et al. 2010; Wu et al. 2011; Cui et al. 2012; Liu et al. 2012; Ma 2012) reported the frequency of −238G/A polymorphism, 11 studies of Asian adults, one of Asian children, and two of Caucasian adults. Three studies (Cui et al. 2012; Liu et al. 2012; Ma 2012) of Asian adults did not observe HWE in controls. There was moderate heterogeneity among the 12 Asian studies (I 2 = 47.6 %, p = 0.033, τ 2 < 0.001), and the pooled frequency was 96.9 % (95 % CI 96.2–97.5 %). The pooled frequency among Caucasian controls was 95.1 % (95 % CI 91.2–99.0 %) with some heterogeneity (I 2 = 90.9 %, p = 0.001, τ 2 = 0.0007).
−857T Allele
Four case–control studies from three articles (Shi et al. 2009; Markoula et al. 2011; Cui et al. 2012) reported the frequency of −857C/T polymorphism, two studies of Asian adults, one of Asian children, and one of Caucasian adults. All of them were observed HWE in controls. The pooled frequency of Asian studies was 82.1 % (95 % CI 79.8–84.4 %) with some heterogeneity (I 2 = 60.0 %, p = 0.082, τ 2 = 0.0002). The frequency of Caucasians was 74.6 % which was reported in one study only.
−1031C Allele
Three case–control studies from two articles (Shi et al. 2009; Cui et al. 2012) reported the frequency of −1031T/C polymorphism, two of Asian adults, and one of Asian children. The pooled frequency of Asian studies was 79.1 % (95 % CI 74.6–93.6 %) with some heterogeneity (I 2 = 88.8 %, p < 0.001, τ 2 = 0.0013).
Assessing Association Between Gene Polymorphism and Ischemic Stroke
TNF-α −308G/A
Twenty-three case–control studies from 19 articles (Bai and Cheng 2004; Balding et al. 2004; Lee et al. 2004; Um and Kim 2004; Karahan et al. 2005; Rubattu et al. 2005; Harcos et al. 2006; Lalouschek et al. 2006; Llamas Sillero et al. 2007; Zhang et al. 2007; Li et al. 2009; Kim et al. 2010; Tong et al. 2010; Sultana et al. 2011; Szabo and Acsady 2011; Cui et al. 2012; Tuttolomondo et al. 2012; Gelfand et al. 2013; Ma 2012) addressed the association between −308G/A polymorphism and ischemic stroke risk. The multivariate meta-analysis indicated that the overall gene effect was not significant (AG vs. GG: OR 0.86, 95 % CI 0.69–1.08; AA vs. GG: OR 0.79, 95 % CI 0.45–1.42; λ = 0.66 ranged from −0.60 to 1.91; Table 3). The univariate meta-analyses of per-allele contrast (A vs. G: OR 0.87, 95 % CI 0.70–1.08; I 2 = 79.4 %, p for heterogeneity = 0.000, τ 2 = 0.189), recessive genetic model (AA vs. AG + GG: OR 0.93, 95 % CI 0.54–1.60; I 2 = 47.8 %, p for heterogeneity = 0.807, τ 2 = 0.617), and dominant genetic model (AA + AG vs. GG: OR 0.84, 95 % CI 0.67–1.05; I 2 = 73.6 %, p for heterogeneity = 0.000, τ 2 = 0.180) also showed no statistical significance (Table 4).
Sensitivity analyses were performed by excluding the six studies (Um and Kim 2004; Zhang et al. 2007; Li et al. 2009; Tong et al. 2010; Sultana et al. 2011; Ma 2012) in which the HWE was not observed, while the results of pooled ORs still presented robustness. Subgroup analyses based on age also did not show any association between the polymorphism and disease risk. However, we observed a decreased risk of disease in Caucasians in the dominant model (Tables 3 and 4); alternatively, this may be a spurious result. No publication bias was detected in all contrasts (Table 5). Furthermore, Proteus phenomenon was not observed in cumulative meta-analysis for the A versus G and the AA + AG versus GG contrasts, while for the AA versus AG + GG contrast a time trend was obvious (Table 5).
TNF-α −238/G/A
Fourteen case–control studies from 11 articles (Lalouschek et al. 2006; Llamas Sillero et al. 2007; Li et al. 2009; Liu et al. 2009; Shi et al. 2009; Kim et al. 2010; Tong et al. 2010; Wu et al. 2011; Cui et al. 2012; Liu et al. 2012; Ma 2012) reported the association between −238G/A polymorphism and ischemic stroke risk. The multivariate meta-analysis with random effects revealed an elevated risk in AG carriers but not in AA carriers, as compared to GG carriers (AG vs. GG: OR 1.44, 95 % CI 1.11–1.86; AA vs. GG: OR 1.98, 95 % CI 0.73–5.40) (Table 3). The estimated λ was 0.53 (95 % CI −0.19–1.25) close to 0.5, although the confidence interval was wide, a codominant genetic model could be expected. This suggests that the heterozygotes have about 44 % higher risk of having ischemic stroke than wild homozygotes. An elevated risk of ischemic stroke was also observed in the univariate meta-analyses of per-allele contrast (A vs. G: OR 1.62, 95 % CI 1.18–2.23; I 2 = 75.2 %, p for heterogeneity = 0.000, τ 2 = 0.231) and dominant genetic model (AA + AG vs. GG: OR 1.56, 95 % CI 1.16–2.10; I 2 = 65.5 %, p for heterogeneity = 0.000, τ 2 = 0.183), but not in the recessive genetic model (AA vs. AG + GG: OR 0.93, 95 % CI 0.54–1.60; I 2 = 47.8 %, p for heterogeneity = 0.807, τ 2 = 0.617) (Table 4).
The result of sensitivity analysis by excluding the three studies (Cui et al. 2012; Liu et al. 2012; Ma 2012) that did not observe HWE showed that the gene effect was robust. We performed subgroup analyses by ethnicity (Asians and Caucasians) and age (adults and children). The results of subgroup analyses showed that the significantly increased risk was observed in Asian adults only, except for per-allele contrast (even though we observed an increase in both Asians and Caucasians in per-allele contrast, it may be a spurious result) (Tables 3 and 4). No publication bias was assessed for all comparisons (Table 5). Furthermore, Proteus phenomenon was not observed in cumulative meta-analysis for A versus G, while for AA versus AG + GG and AA + AG versus GG a time trend was obvious (Table 5).
TNF-α −857C/T and −1031T/C
Four case–control studies from three articles (Shi et al. 2009; Markoula et al. 2011; Cui et al. 2012) addressed the association between −857C/T polymorphism and ischemic stroke risk. Nor did we detect any significant difference in the pooled ORs in both multivariate and univariate meta-analyses (Tables 3 and 4). Three case–control studies from two articles (Shi et al. 2009; Cui et al. 2012) examined the association between −1031T/C polymorphism and risk of ischemic stroke. We also did not observe any significant difference in the summary ORs in both multivariate and univariate meta-analyses (Tables 3 and 4).
Only one study (Lalouschek et al. 2006) addressed −244G/A and −367G/A polymorphism; one study (Shi et al. 2009) reported −646G/A, −806C/T, and −863C/A polymorphism; one study (Shi et al. 2009) identified +448G/A polymorphism. None of these studies achieved any significant difference.
Discussion
Our systematic review summarized the available evidence to date regarding the association between TNF-α and the risk of ischemic stroke. The results from meta-analysis suggest that the TNF-α −238G/A polymorphism is likely to be associated with the risk of ischemic stroke. Meta-analysis performed separately for Caucasian and Asian studies showed that −238G/A heterozygotes presented an elevated risk of ischemic stroke compared with wild homozygotes in Asian adults, but no association in Caucasians was revealed. No significant association was observed for other TNF-α polymorphisms analyzed.
The parsimonious approach suggested that the finest genetic model for TNF-α −238G/A polymorphism was codominant model. Therefore, the TNF-α −238 AG heterozygotes present a roughly 1.44-fold higher risk of developing ischemic stroke compared with GG wild homozygotes. However, subgroup analyses showed that the AG genotype carriers presented an elevated risk of 1.41-fold for developing ischemic stroke in Asian adults only. It is ambiguous why the association of this mutation differs in different ethnicity, even though the major frequency of G allele was similar in different races (96.9 % in Asians and 95.1 % in Caucasians). However, it may be due to the limited quantity of included studies of Caucasians (only two studies). Our results are strengthened by the fact that there were significant differences in per-allele contrast and dominant genetic model. Moreover, meta-analysis of −308G/A polymorphism showed that A allele carriers (AA + AG) presented a decreased risk of ischemic stroke in Caucasians; however, this may be a spurious result that the parsimonious approach suggested an insignificant overall gene effect and nonexistence of the finest genetic model of inheritance for the −308G/A polymorphism.
The present meta-analysis differs from the previous meta-analyses analyzing the association between the TNF-α polymorphisms and ischemic stroke risk (Pereira et al. 2007; Gu et al. 2013a, b). Pereira et al. (2007) performed a meta-analysis that investigated the effect of TNF-α −308G/A polymorphism on the risk of ischemic stroke with eight case–control studies in 2007, and they suggested that the −308G/A polymorphism was a protective factor for ischemic stroke in Asians only. Latterly Gu et al. (2013b) conducted a meta-analysis with 13 studies and suggested that −308G/A polymorphism was associated with the risk of juvenile ischemic stroke, and it was a protective factor for ischemic stroke in Asians and adult population. However, our meta-analysis with 23 case–control studies from 19 articles demonstrated that the TNF-α −308G/A polymorphism was not associated with ischemic stroke risk. Afterward, Gu et al. (2013a) carried out a meta-analysis with seven studies and indicated that −238G/A polymorphism increased the risk of ischemic stroke in adults and Caucasians. But in the present meta-analysis with 14 case–control studies from 11 articles, we suggest that −238G/A heterozygotes (AG) presented an elevated risk of ischemic stroke compared with wild homozygotes (GG) in Asian adults only. Compared to the previous meta-analyses, our study was a systematic review and meta-analysis that so far most comprehensively and systematically evaluated the association between 10 TNF-α polymorphisms and risk of ischemic stroke. Moreover, we had a higher statistical power to detect the gene effect than previous meta-analyses (Pereira et al. 2007; Gu et al. 2013a, b) with a larger sample size by including more Chinese studies. Most importantly, the previous meta-analyses used bivariate meta-analysis which does not consider the within-study pairwise correlation of genotype contrast, and a biological justification for the choice of genetic model is not available (Bagos 2008; Minelli et al. 2005b). Therefore, we believe that this systematic review with multivariate meta-analyses will help researchers to better understand the association between the TNF-α polymorphisms and risk of ischemic stroke and also indicates further study fields.
Like any meta-analytic study, the present study also should be viewed with caution because of certain inherent limitations. First, confounding factors and heterogeneity may have distorted the result of meta-analysis. In addition, meta-analyses are prone to potential biases not only the publication bias. Although our meta-analyses did not observe any publication bias by funnel plot and Egger’s linear regression method, we still cannot eliminate the possibility of these biases. Second, the haplotype analyses could not be performed due to little information in the eligible studies, and results may be spurious as effected by the haplotype gene effect. Third, this meta-analysis identified data from Asians and Caucasians; hence, the results of our study are only applicable to these two ethnicities. Fourth, except −308G/A and −238G/A polymorphisms, the sample size was too small and the statistical power was too low for the other polymorphisms in TNF-α. In addition, the minor allele frequencies of −308A and −238A were quite small in both Asians and Caucasians; therefore, large sample size was needed to better detect the true gene effect of disease. Finally, perhaps one of the most important pitfalls of the included studies in the meta-analysis may be the study design, which was unmatched case–control for most studies. Indeed, the case–control design leads results prone to survival bias and underestimates gene effect of disease.
In conclusion, the present systematic review and meta-analysis support a prominent role of the TNF-α −238G/A polymorphism in the risk of ischemic stroke in Asian adults only, but do not support the role of −308G/A, −857C/T, −1031T/C, −244G/A, −367G/A, −646G/A, −806C/T, −863C/A, and +448G/A in the risk of ischemic stroke. The current evidence warrants further studies with high quality and large sample size to confirm.
References
Bagos, P. G. (2008). A unification of multivariate methods for meta-analysis of genetic association studies. Statistical Applications in Genetics and Molecular Biology,. doi:10.2202/1544-6115.1408.
Bagos, P. G., & Nikolopoulos, G. K. (2009). Generalized least squares for assessing trends in cumulative meta-analysis with applications in genetic epidemiology. Journal of Clinical Epidemiology, 62(10), 1037–1044. doi:10.1016/j.jclinepi.2008.12.008.
Bai, X. G., & Cheng, Z. J. (2004). Correlation between tumor necrosis factor alpha gene polymorphisms and cerebral infarction. Yi Xue Xin Zhi, 14(2), 111–113.
Balding, J., Livingstone, W. J., Pittock, S. J., Mynett-Johnson, L., Ahern, T., Hodgson, A., et al. (2004). The IL-6 G-174C polymorphism may be associated with ischaemic stroke in patients without a history of hypertension. Irish Journal of Medical Science, 173(4), 200–203.
Bayley, J. P., Ottenhoff, T. H., & Verweij, C. L. (2004). Is there a future for TNF promoter polymorphisms? Genes and Immunity, 5(5), 315–329. doi:10.1038/sj.gene.6364055.
Braliou, G. G., Grigoriadou, A. M., Kontou, P. I., & Bagos, P. G. (2014). The role of genetic polymorphisms of the Renin–Angiotensin system in renal diseases: A meta-analysis. Computational and Structural Biotechnology Journal, 10(16), 1–7. doi:10.1016/j.csbj.2014.05.006.
Cui, G., Wang, H., Li, R., Zhang, L., Li, Z., Wang, Y., et al. (2012). Polymorphism of tumor necrosis factor alpha (TNF-alpha) gene promoter, circulating TNF-alpha level, and cardiovascular risk factor for ischemic stroke. Journal of Neuroinflammation, 9, 235. doi:10.1186/1742-2094-9-235.
Egger, M., Davey Smith, G., Schneider, M., & Minder, C. (1997). Bias in meta-analysis detected by a simple, graphical test. BMJ, 315(7109), 629–634.
Friedrich, J. O., Adhikari, N. K., & Beyene, J. (2007). Inclusion of zero total event trials in meta-analyses maintains analytic consistency and incorporates all available data. BMC Medical Research Methodology, 7, 5. doi:10.1186/1471-2288-7-5.
Gelfand, A. A., Croen, L. A., Torres, A. R., & Wu, Y. W. (2013). Genetic risk factors for perinatal arterial ischemic stroke. Pediatric Neurology, 48(1), 36–41. doi:10.1016/j.pediatrneurol.2012.09.016.
Gu, L., Su, L., Wu, G., Chen, Q., Yan, Y., Xie, J., et al. (2013a). Association between TNF-delta 238G/A polymorphisms and the risk of ischemic stroke. International Journal of Neuroscience, 123(1), 1–6. doi:10.3109/00207454.2012.725118.
Gu, L., Wu, G., Long, J., Su, L., Yan, Y., Chen, Q., et al. (2013b). The role of TNF-alpha 308G > A polymorphism in the risk for ischemic stroke. The American Journal of the Medical Sciences, 345(3), 227–233. doi:10.1097/MAJ.0b013e31825f92da.
Harcos, P., Laki, J., Kiszel, P., Szeplaki, Z., Szolnoki, Z., Kovacs, M., et al. (2006). Decreased frequency of the TNF2 allele of TNF-alpha −308 promoter polymorphism is associated with lacunar infarction. Cytokine, 33(2), 100–105. doi:10.1016/j.cyto.2005.12.006.
Higgins, J. P., Thompson, S. G., Deeks, J. J., & Altman, D. G. (2003). Measuring inconsistency in meta-analyses. BMJ, 327(7414), 557–560. doi:10.1136/bmj.327.7414.557.
Karahan, Z. C., Deda, G., Sipahi, T., Elhan, A. H., & Akar, N. (2005). TNF-alpha −308G/A and IL-6 −174 G/C polymorphisms in the Turkish pediatric stroke patients. Thrombosis Research, 115(5), 393–398. doi:10.1016/j.thromres.2004.09.008.
Kim, O. J., Lee, J. H., Choi, J. K., Oh, S. H., Hong, S. H., Oh, D., et al. (2010). Association between tumor necrosis factor-alpha (−308G– > A and −238G– > A) polymorphisms and homocysteine levels in patients with ischemic strokes and silent brain infarctions. Cerebrovascular Diseases, 30(5), 483–490. doi:10.1159/000319023.
Lalouschek, W., Schillinger, M., Hsieh, K., Endler, G., Greisenegger, S., Marculescu, R., et al. (2006). Polymorphisms of the inflammatory system and risk of ischemic cerebrovascular events. Clinical Chemical Laboratory Medicine, 44(8), 918–923. doi:10.1515/CCLM.2006.165.
Lee, B. C., Ahn, S. Y., Doo, H. K., Yim, S. V., Lee, H. J., Jin, S. Y., et al. (2004). Susceptibility for ischemic stroke in Korean population is associated with polymorphisms of the interleukin-1 receptor antagonist and tumor necrosis factor-alpha genes, but not the interleukin-1beta gene. Neuroscience Letters, 357(1), 33–36. doi:10.1016/j.neulet.2003.12.041.
Li, S. M., Chen, Y. C., & Chen, S. Q. (2009). Relationship of TNFα-238 and TNFα-308 polymorphisms with atherosclerosis cerebral infarction. Zhonghua Sheng Wu Yi Xue Gong Cheng Za Zhi, 15(2), 98–102.
Liu, Z. W., Li, J. C., Li, S. M., & Chen, S. Q. (2009). Study on TNFα − 238G/A polymorphisnis in patients with cerebral infarction. Jie Pou Xue Yan Jiu, 31(4), 259–262.
Liu, D. F., Zhang, B. Q., Zhang, Z. Y., Chen, H., Zhao, Y. T., Zhang, C. X., et al. (2012). The association between IL-6 −572C/G and TNF-α − 238G/A polymorphism and Han patients with cerebral infarction in Tangshan. Zhong Guo Nao Nian Xue Za Zhi, 32(24), 5397–5398.
Llamas Sillero, P., de Velasco, Fernandez, Casarrubios, J., Garcia-Raso, A., Meseguer Gancedo, E., Santos Montero, A. B., & Tomas Martinez, J. F. (2007). Polymorphism −238 G/A of tumor necrosis factor alpha gene promoter is a genetic risk factor for ischemic cerebrovascular disease. Journal of Molecular Neuroscience, 32(2), 108–110.
Lopez, A. D., Mathers, C. D., Ezzati, M., Jamison, D. T., & Murray, C. J. (2006). Global and regional burden of disease and risk factors, 2001: Systematic analysis of population health data. The Lancet, 367(9524), 1747–1757. doi:10.1016/S0140-6736(06)68770-9.
Lu, X. C., Yu, W., Tao, Y., Zhao, P. L., Li, K., Tang, L. J., et al. (2014). Contribution of transforming growth factor alpha polymorphisms to nonsyndromic orofacial clefts: A HuGE review and meta-analysis. American Journal of Epidemiology, 179(3), 267–281. doi:10.1093/aje/kwt262.
Ma, X. L. (2012). IL-1 and TNF and gene polymorphisms and the risk of cerebral infarction. Zhong Guo Shi Yong Shen Jing Ji Bing Za Zhi, 15(6), 33–35.
Markoula, S., Chatzikyriakidou, A., Giannopoulos, S., Odysseas, K., Markou, S., Vemmos, K., et al. (2011). Association of TNF-857C > T, TNFRSF1A36A > G, and TNFRSF1B676T > G polymorphisms with ischemic stroke in a Greek population. Stroke Research and Treatment, 2011, 920584. doi:10.4061/2011/920584.
Minelli, C., Thompson, J. R., Abrams, K. R., & Lambert, P. C. (2005a). Bayesian implementation of a genetic model-free approach to the meta-analysis of genetic association studies. Statistics in Medicine, 24(24), 3845–3861. doi:10.1002/sim.2393.
Minelli, C., Thompson, J. R., Abrams, K. R., Thakkinstian, A., & Attia, J. (2005b). The choice of a genetic model in the meta-analysis of molecular association studies. Interntional Journal of Epidemiology, 34(6), 1319–1328. doi:10.1093/ije/dyi169.
Munshi, A., Rajeshwar, K., Kaul, S., Al-Hazzani, A., Alshatwi, A. A., Shafi, G., et al. (2011). Association of tumor necrosis factor-alpha and matrix metalloproteinase-3 gene variants with stroke. European Journal of Neurology, 18(8), 1053–1059. doi:10.1111/j.1468-1331.2010.03334.x.
Packard, R. R., & Libby, P. (2008). Inflammation in atherosclerosis: from vascular biology to biomarker discovery and risk prediction. Clinical Chemistry, 54(1), 24–38. doi:10.1373/clinchem.2007.097360.
Pereira, T. V., Rudnicki, M., Franco, R. F., Pereira, A. C., & Krieger, J. E. (2007). Effect of the G-308A polymorphism of the tumor necrosis factor alpha gene on the risk of ischemic heart disease and ischemic stroke: A meta-analysis. American Heart Journal, 153(5), 821–830. doi:10.1016/j.ahj.2007.02.031.
Rubattu, S., Speranza, R., Ferrari, M., Evangelista, A., Beccia, M., Stanzione, R., et al. (2005). A role of TNF-alpha gene variant on juvenile ischemic stroke: A case-control study. European Journal of Neurology, 12(12), 989–993. doi:10.1111/j.1468-1331.2005.01136.x.
Shi, K. L., He, B., Wang, J. J., & Zou, L. P. (2009). Role of TNF-alpha gene variation in idiopathic childhood ischemic stroke: A case-control study. Journal of Child Neurology, 24(1), 25–29. doi:10.1177/0883073808321046.
Stroup, D. F., Berlin, J. A., Morton, S. C., Olkin, I., Williamson, G. D., Rennie, D., et al. (2000). Meta-analysis of observational studies in epidemiology: A proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA, 283(15), 2008–2012.
Sultana, S., Kolla, V. K., Jeedigunta, Y., Penagaluru, P. K., Joshi, S., Rani, P. U., et al. (2011). Tumour necrosis factor alpha and interleukin 10 gene polymorphisms and the risk of ischemic stroke in south Indian population. Journal of Genetics, 90(2), 361–364.
Szabo, G. V., & Acsady, G. (2011). Tumornecrosis-factor-alpha 308 GA polymorphism in atherosclerotic patients. Pathology and Oncology Research, 17(4), 853–857. doi:10.1007/s12253-011-9393-8.
Thakkinstian, A., McEvoy, M., Minelli, C., Gibson, P., Hancox, B., Duffy, D., et al. (2005). Systematic review and meta-analysis of the association between {beta}2-adrenoceptor polymorphisms and asthma: a HuGE review. American Journal of Epidemiology, 162(3), 201–211. doi:10.1093/aje/kwi184.
Tong, Y., Geng, Y., Xu, J., Wang, Z., Zhang, Y., Lin, L., et al. (2010). The role of functional polymorphisms of the TNF-alpha gene promoter in the risk of ischemic stroke in Chinese Han and Uyghur populations: Two case-control studies. Clinica Chimica Acta, 411(17–18), 1291–1295. doi:10.1016/j.cca.2010.05.007.
Tuttolomondo, A., Di Raimondo, D., Forte, G. I., Casuccio, A., Vaccarino, L., Scola, L., et al. (2012). Single nucleotide polymorphisms (SNPs) of pro-inflammatory/anti-inflammatory and thrombotic/fibrinolytic genes in patients with acute ischemic stroke in relation to TOAST subtype. Cytokine, 58(3), 398–405. doi:10.1016/j.cyto.2012.02.012.
Um, J. Y., & Kim, H. M. (2004). Tumor necrosis factor alpha gene polymorphism is associated with cerebral infarction. Brain Research. Molecular Brain Research, 122(1), 99–102. doi:10.1016/j.molbrainres.2003.11.019.
Wu, K., Li, G. J., Wang, Z., Jin, S. J., & Fu, S. G. (2011). Association study of TNFα-238 G/A polymorphism in senior Han patients with cerebral infarction in Hainan. Zhonghua Lao Nian Xin Nao Xue Guan Bing Za Zhi, 13(11), 1011–1012.
Zeng, X., Zhang, Y., Kwong, J. S., Zhang, C., Li, S., Sun, F., et al. (2015). The methodological quality assessment tools for pre-clinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: A systematic review. Journal of Evidence-Based Medicine,. doi:10.1111/jebm.12141.
Zhang, G. Z., Pan, S. Y., Lu, B. X., & Li, W. (2007). Correlation between tumor necrosis factor alpha and beta gene polymorphisms and cerebral infarction. Zhong Guo Xian Dai Yi Xue Za Zhi, 17(7), 813–816.
Acknowledgments
We gratefully acknowledged the support of the subjects who participated in this study. This study was partly supported by Foundation of Ministry of Education of Hubei Province (D20142102) and Foundation of Taihe Hospital (2013PY02, 2013JJXM011). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. No additional external funding received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Yu-Ming Niu, Hong Weng, and Chao Zhang have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Niu, YM., Weng, H., Zhang, C. et al. Systematic Review by Multivariate Meta-analyses on the Possible Role of Tumor Necrosis Factor-α Gene Polymorphisms in Association with Ischemic Stroke. Neuromol Med 17, 373–384 (2015). https://doi.org/10.1007/s12017-015-8365-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12017-015-8365-7