Abstract
Parkinson’s disease is the second most common neurodegenerative movement disorder; however, its etiology remains elusive. Nevertheless, in vivo observations have concluded that oxidative stress is one of the most common causes in the pathogenesis of Parkinson’s disease. It is known that mitochondria play a crucial role in reactive oxygen species-mediated pathways, and several gene products that associate with mitochondrial function are the subject of Parkinson’s disease research. The PTEN-induced kinase 1 (PINK1) protects cells from mitochondrial dysfunction and is linked to the autosomal recessive familial form of the disease. PINK1 is a key player in many signaling pathways engaged in mitophagy, apoptosis, or microglial inflammatory response and is induced by oxidative stress. Several proteins participate in mitochondrial networks, and they are associated with PINK1. The E3 ubiquitin ligase Parkin, the protease presenilin-associated rhomboid-like serine protease, the tyrosine kinase c-Abl, the protein kinase MARK2, the protease HtrA2, and the tumor necrosis factor receptor-associated protein 1 (TRAP1) provide different steps of control in protection against oxidative stress. Furthermore, environmental toxins, such as 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine, have been identified as contributors to parkinsonism by increasing oxidative stress in dopaminergic neurons. The present review discusses the mechanisms and effects of oxidative stress, the emerging concept of the impact of environmental toxins, and a possible neuroprotective role of the antioxidant astaxanthin in various neurodegenerative disorders with particular emphasis in Parkinson’s disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parkinson’s disease is the second most common neurodegenerative movement disorder with a median age of onset of 55 years and a prevalence of 3 % in people >80 years of age (Strickland and Bertoni 2004). The majority of these cases are identified as sporadic Parkinson’s disease, and only a small percentage are considered familial Parkinson’s disease. Phenotypically, it is characterized by tremor, rigidity, slowness of voluntary movement, and postural instability. Since Parkinson’s disease is characterized by various symptoms that are linked to different stages of its progression, the identification of this pathology at an early stage is not easy. The etiology is still unknown, but it is hypothesized that it may result from a complex interaction between environmental factors, genetic susceptibility, and aging (Reichmann 2011).
The motor symptoms of Parkinson’s disease result from the loss of dopaminergic neurons in the substantia nigra (SN) (Braak and Braak 2000). It is known that dopamine (DA) released from the neurons of the SN pars compacta (SNpc) into the striatum exerts a critical role in the modulation of basal ganglia activity (Graybiel 2005). Parkinson’s disease is also characterized by highly insoluble fibrillar aggregates of the protein alpha synuclein (α-syn), called Lewy bodies (LBs) and Lewy neurites (LNs), that accumulate in the neuronal cytoplasm or neuritic processes, respectively. These inclusions are rich in phosphorylated α-syn (p-α-syn), are often ubiquitinated (Fujiwara et al. 2002; Kuzuhara et al. 1988), and are widely distributed in the central nervous system (CNS), where they are associated with neuron loss (Wakabayashi et al. 2007). Despite these findings, current therapies of Parkinson’s disease are symptomatic, targeting mainly the lack of DA in the striatum with DA replacement strategies. Although these therapies provide symptomatic relief, they become more and more inefficient while the disease progresses.
Despite the fact that Parkinson’s disease has long been considered as a non-genetic disorder of sporadic origin, there have been identified some rare (<10 % of Parkinson’s disease cases) monogenic forms of Parkinson’s disease. This resulted in the identification of 16 “PARK” loci, with the genes PTEN-induced kinase 1 (PINK1 or PARK6), Parkin (PARK2), SNCA (PARK1/4), LRRK2 (PARK8), and DJ-1 (PARK7) being the most common (Crosiers et al. 2011; Sundal et al. 2012). It has been demonstrated that these genes also play a role in the much more common sporadic form of the disease; therefore, the knowledge of their biological function will contribute to the understanding of sporadic Parkinson’s disease since both share clinical and neuropathological features (Lesage and Brice 2012). Moreover, several cellular abnormalities displayed in sporadic Parkinson’s disease, such as mitochondrial and lysosomal dysfunction, oxidative stress, excitotoxicity, proteasomal stress, neuroinflammation, and protein aggregation, are also associated with mutations in the familial Parkinson’s disease genes (Yacoubian and Standaert 2009). More specifically, oxidative damage is very frequent in neurodegenerative disorders including Parkinson’s disease. The CNS is characterized by energy-demanding organs (brain and spinal cord); hence, persistent oxidative stress is a prominent factor in the pathogenesis of Parkinson’s disease (Ciccone et al. 2013).
Oxidative Stress in Parkinson’s Disease
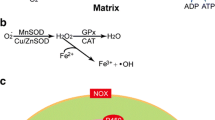
Oxidative stress can be defined as a condition in which the cellular antioxidant defense mechanisms are insufficient to keep the level of reactive oxygen species (ROS) below a toxic threshold (Shulman et al. 2011). This may be due to either an overproduction of reactive free radicals or to a failure of cell-buffering mechanisms (Yacoubian and Standaert 2009). ROS can damage all types of biomolecules, and oxidative damage of nucleic acids, lipids, and proteins can have deleterious effects (Dalle-Donne et al. 2003). ROS are produced by a number of different pathways, but all the initial free radical reactions require activation of molecular oxygen (Barnham et al. 2004). ROS are being continuously generated in vivo as a result of oxygen metabolism, with about 1–5 % of the oxygen consumed being converted to ROS (Deas et al. 2011). In addition, the generation of reactive nitrogen species (RNS) is due to nitric oxide synthase (NOS)-mediated conversion of arginine to citrulline (Barnham et al. 2004).
The occurrence of oxidative stress in Parkinson’s disease is supported by both postmortem studies and studies demonstrating the important role of oxidative stress and oxidizing toxins in neuronal degeneration of the DAergic nigral neurons (Gilgun-Sherki et al. 2001; Mythri et al. 2011). Early and profound loss of the antioxidant protein (protein-disulfide reductase) glutathione (GSH); a reduction in mitochondrial Complex I activity; increased oxidative damage of lipids, proteins, and DNA; augmented superoxide dismutase (SOD) activity; and elevated free iron levels in the SN of Parkinson’s disease patients have been documented (Blum et al. 2001; Mythri et al. 2011). Moreover, in vivo observations revealed that several markers of oxidative stress are altered in the cerebrospinal fluid (CSF) and blood samples of Parkinson’s disease patients (Ilic et al. 1998; Vinish et al. 2011).
An ever increasing number of studies associate oxidative stress with neurodegenerative disorders; therefore, it is crucial to understand why CNS exhibits increased susceptibility to oxidative stress (Fig. 1). First of all, it is noteworthy that the brain in particular is more vulnerable to oxidative stress and oxidative damage compared to other organs. For instance, the brain consumes more oxygen on a per weight basis under physiological conditions than any other organ. Secondly, the brain contains a relatively low level of antioxidants and free radical-scavenging enzymes compared to other tissues (Barnham et al. 2004; Mytilineou et al. 2002; Roberts et al. 2010) as well as a high amount of substances, such as phospholipids and unsaturated fatty acids (Cui et al. 2004), which are vulnerable to oxidative modifications (Barnham et al. 2004; Selley 1998). Furthermore, the vulnerability of neurons to oxidative damage, which accumulates in aging neurons, might also be due to their postmitotic nature (Crabtree and Zhang 2012).
Main causes of oxidative stress in Parkinson’s disease clustered in five groups by their functional similarity (marked in different color). Each group describes the general biological processes that may result in excessive oxidative stress, thus contributing to the pathogenesis of Parkinson’s disease. DA dopamine, mtDNA mitochondrial DNA, NM neuromelanin, PD Parkinson’s disease, ROS reactive oxygen species, SN substantia nigra, UPS ubiquitin–proteasome system
More specifically, the high concentration of DA in the nigrostriatal pathway is presumed to be essential for the high vulnerability of DAergic cells to oxidative stress. DA itself does not exert direct toxic effects (Lotharius and Brundin 2002), but toxic intermediates derived from its catabolism may contribute to the oxidative stress pathogenic pathway in Parkinson’s disease (Andersen 2004; Jenner 2003). Midbrain DAergic neurons are also prone to oxidative stress due to their low mitochondrial reserve compared to other neuronal populations (Feng and Maguire-Zeiss 2010).
A matter of concern is the role of Ca2+. Ca2+ stimulates DA synthesis and modulates the function of endoplasmic reticulum (ER) and mitochondria (Mosharov et al. 2009). SNpc DA neurons engage L-type Ca2+ channels to allow extracellular Ca2+ to enter the cytoplasm (Puopolo et al. 2007) and to maintain an adequate level of DA synthesis (Mosharov et al. 2009). This process requires L-type Ca2+ channels to be opened most of the time leading to a basal mitochondrial oxidant stress in SNpc DA neurons (Guzman et al. 2010). The unusual reliance of SNpc DA neurons on this type of Ca2+ channels is the key factor of Ca2+-mediated mitochondrial and ER stress, and it seems to be responsible for their selective vulnerability (Surmeier et al. 2011).
Furthermore, it is proposed that oxidative damage caused by excessive influx of Ca2+ could also be a consequence of overstimulation of ionotropic glutamate receptors (Nakamura and Lipton 2011). Glutamate is the major neurotransmitter in the CNS of mammals. Ionotropic glutamate receptors in the nervous system are represented by three classes: kainate, amino-3-hydroxy-5-methyl-4-isoxazole propionic acid (AMPA), and N-methyl-d-aspartate (NMDA). NMDA receptors (NMDARs) are widely expressed throughout the basal ganglia including SNpc (Johnson et al. 2009). Under physiological conditions, NMDARs can result in normal ROS and RNS production, which mediate normal signaling to support neuronal function and survival. However, under neurodegenerative conditions, overactivation of extrasynaptic NMDARs causes excessive influx of Ca2+ contributing to cell injury and death via oxidative stress, a process called excitotoxicity (Nakamura and Lipton 2010).
On the other hand, the nature of cells in which oxidative stress occurs in the SN in Parkinson’s disease is debated. It is not clear whether oxidative stress is a process that occurs in all DAergic cells, because those in the dorsal tier appear to be more resistant to degeneration than those found in ventral layers (Andersen 2004; Barnham et al. 2004; Jenner 2003). Additionally, the extent of change in parameters of oxidative stress has led to the notion that it must also take place in non-neuronal cells such as glial cells. Indeed, a decrease in glial cell GSH content has been demonstrated by immunohistochemistry in nigral tissue from Parkinson’s disease patients, and increased iron levels also occur within glia (Andersen 2004; Barnham et al. 2004; Jenner 2003; Pearce et al. 1997). This raises the important concept of a generalized oxidative stress occurring in the SN that affects both glial cells and neurons, perhaps because of a general metabolic failure (Fig. 1) (Andersen 2004).
In addition, it is important to note that the ROS-generating pathways are heavily dependent on the presence of metals such as copper and in particular iron, whose levels have been found to be elevated in the SN of Parkinson’s disease patients (Andersen 2004). The reason for this is not yet understood, but the fact is that during brain aging, a deregulation in total iron concentration may cause an increase in free iron within brain leading to oxidative damage. In this situation, neuromelanin (NM) can play a protective role by blocking reactive iron in a stable complex. NM is a dark-brown pigment that concentrates metal ions, such as iron, and thereby makes the nigrostriatal DAergic neurons appear dark colored. However, the role of NM has been debated for long time (Zecca et al. 2004). NM accumulates in the SNpc with age but in Parkinson’s disease patients, the NM levels are significantly reduced in DA neurons, while elevated in the extracellular space in the SNpc. Investigations show that the release of NM in the extracellular space is a result of damaged or dying neurons. Released NM induces mitochondrial activation, generates neuroinflammation, and leads to progressive degeneration of DA neurons (Zhang et al. 2013).
Furthermore, several of the genes linked to familial forms of Parkinson’s disease appear to be involved in the protection against or in the propagation of oxidative stress (Toulouse and Sullivan 2008; Yacoubian and Standaert 2009). In particular, subsequent studies have connected specific genetic defects with mitochondria and oxidative stress. Increased Parkinson’s disease risk has been linked to mutation in α-syn, Parkin, PINK1, DJ-1, and LRRK2 all of which have been related to mitochondria (Henchcliffe and Beal 2008). Impaired mitochondrial function is likely to increase oxidative stress, and the products of these Parkinson’s disease-associated genes have a crucial role in mitochondria under certain conditions (Henchcliffe and Beal 2008). Apart from that, many of the genetic loci linked to the familiar cases of Parkinson’s disease code for genes that affect the ubiquitin–proteasome system (UPS) (Olanow and McNaught 2006). The UPS is the main system through which the body removes superfluous proteins. Dysfunction of the UPS leads to accumulation of LB inclusions in the SNpc of Parkinson’s disease patients (Olanow and McNaught 2006).
Finally, mitochondrial DNA (mtDNA) alteration is implicated in Parkinson’s disease onset. High levels of somatic mtDNA mutations have been observed in SN neurons in Parkinson’s disease patients (Yan et al. 2013). MtDNA is vulnerable to oxidative stress; thus, an increase in ROS generation leads to a gradual accumulation of mtDNA mutations creating a positive feedback loop of increasing mutation and ROS production that is followed by eventual cell death (Yan et al. 2013).
Mitochondrial Dysfunction: Just Think PINK
We have discussed above the role of oxidative stress for Parkinson’s disease progression. Several postmortem studies performed on individuals with Parkinson’s disease have shown an increased level of lipids, proteins, and DNA oxidation, and a decreased concentration of GSH (Ciccone et al. 2013). Moreover, numerous studies have reported the involvement of mitochondria, neuroinflammation via activated microglia, and other ROS-mediated pathways in the pathogenesis of Parkinson’s disease (Varcin et al. 2012). Mitochondria play a pivotal role in eukaryotic metabolic processes by serving as cellular energy generators of ATP (Nicholls 2010), which are critical for cell survival and for normal cellular functions, as well as in mediating apoptosis and in determining their own autophagy called mitophagy (Novak 2012), an important control mechanism that clears damaged mitochondria. It seems that mitochondrial dysfunction is involved in Parkinson’s disease insurgence as well (Fig. 1) (Arduino et al. 2013).
PINK1 Regulatory Pathway Leading to Mitophagy: The Key Role of Parkin
The discovery of several inherited mutations in gene products that associate with mitochondrial function was crucial in Parkinson’s disease research. PINK1 is a mitochondria-targeted serine/threonine (Ser/Thr) kinase, which is linked to autosomal recessive familial form and early-onset Parkinson’s disease (Corti et al. 2011). PINK1 is present in different brain regions, in particular in SN, hippocampus, and Purkinje cells of cerebellum. It harbors a mitochondrial signal motif in the N-terminal domain and an autoregulatory region in the C-terminal domain. Several studies demonstrate that PINK1 is involved in mitochondrial metabolism and dynamics, ubiquitin-mediated protein degradation, and oxidative stress (Heeman et al. 2011). The subcellular localization of PINK1 is still debated but it seems that it is regulated by the mitochondrial membrane potential (∆Ψm). In healthy mitochondria, PINK1 is guided to the mitochondrial inner membrane through the general mitochondrial import machinery (Song et al. 2013), whereas in damaged mitochondria, the dissipation of ∆Ψm prevents PINK1 from reaching the inner membrane and as a consequence PINK1 remains localized to the outer mitochondrial membrane (Okatsu et al. 2012). The role of PINK1 in Parkinson’s disease progression is supported by the fact that PINK1 colocalizes with LBs (Zhou et al. 2008). Moreover, a study in primary neuronal cell lines from mice lacking PINK1 has shown typical symptoms of Parkinson’s disease, including mitochondrial impairment of DAergic neurons (Wood-Kaczmar et al. 2008). Compelling evidence indicates that the mutation of PINK1 is one of the principal causes of Parkinson’s disease insurgence (Marongiu et al. 2009).
In addition, PINK1 is known to regulate Parkinson’s disease-related protein Parkin (Corti et al. 2011). Parkin bears an N-terminal ubiquitin-like domain and a C-terminal RING finger region with E3 ubiquitin ligase activity (Shimura et al. 2000). Parkin plays an important role in controlling the amount of protein aggregates. Albeit Parkin can reduce ROS production, and the overexpression of mutant Parkin is linked to increased ROS generation. Postmortem studies performed in subjects affected by Parkinson’s disease demonstrate that Parkin colocalizes with LBs as well (Ciccone et al. 2013). In damaged mitochondria, PINK1 translocates to the outer membrane, where it recruits the E3 ubiquitin ligase Parkin from cytosol to mitochondria in order to initiate mitophagy (Fig. 2). This induces the ubiquitination of outer membrane proteins. In flies, Parkin accumulation and autophagy induction can cause an enrichment of impaired mitochondria in DAergic neurons and generate an excessive amount of ROS (Narendra et al. 2010).
Implication of mitochondrial dysfunction in the pathobiology of Parkinson’s disease. In damaged mitochondria, PARL cleaves PINK1 precursor and the mature PINK1 translocates from the inner to the outer membrane, where it recruits the E3 ubiquitin ligase Parkin from cytosol to mitochondria to induce mitophagy. MARK2 phosphorylates and activates the mature PINK1. During oxidative stress, however, cytoplasmic c-Abl moves to mitochondria and inactivates Parkin promoting the accumulation of misfolded proteins such as AIMP2 and FBP-1. C-Abl activates PKCδ leading to mitochondrial dysfunction and cell death as well. AIMP2 aminoacyl tRNA synthetase complex-interacting multifunctional protein 2, FBP-1 fructose-1,6-bisphosphatase 1, IMM inner mitochondrial membrane, IMS intermembrane space, MARK2 microtubule affinity-regulating kinase 2, OMM outer mitochondrial membrane, PARL presenilin-associated rhomboid-like serine protease, PINK1 PTEN-induced kinase 1, PKCδ protein kinase C delta
One important molecule that affects the proteolytic processing of PINK1 is the presenilin-associated rhomboid-like serine protease (PARL), the mammalian ortholog of mitochondrial protease Rhomboid-7 in flies (Deas et al. 2011). Normal PINK1 localization and stability require the catalytic activity of PARL. Consequently, PARL deficiency impairs Parkin recruitment to mitochondria, suggesting that PINK1 processing and localization are crucial in determining its interaction with Parkin (Greene et al. 2012). More than 50 mutations have been mapped throughout the kinase and C-terminal regulatory domains of PINK1 with various effects on protein stability implicating neuroprotective roles (Kumar et al. 2011; Rochet et al. 2012). Intramembrane proteolysis is a conserved mechanism that modulates various cellular processes. PARL cleaves human PINK1 within its conserved membrane anchor (Meissner et al. 2011), suggesting PINK1’s role in neurodegenerative disease. Mature PINK1 is then free to be released into the cytosol or into the mitochondrial intermembrane space (Fig. 2). Upon depolarization of the mitochondrial membrane potential, the import of PINK1 and its PARL-catalyzed processing are blocked, leading to the accumulation of the PINK1 precursor (Meissner et al. 2011). Targeting of this precursor to the outer mitochondrial membrane has been shown to trigger mitophagy (Okatsu et al. 2012). The PARL-catalyzed removal of the PINK1 signal sequence in the import pathway may act as a cellular checkpoint for mitochondrial integrity. Interestingly, Parkinson’s disease-causing mutations decrease the processing of PINK1 by PARL (Cookson and Bandmann 2010). When mitochondrial import is compromised by depolarization, PINK1 accumulates on the mitochondrial surface where it recruits the Parkinson’s disease-linked Parkin from cytosol, which in turn mediates the mitophagic destruction of mitochondria (Cookson and Bandmann 2010; Okatsu et al. 2012). The importance of PINK1 in mechanisms underlying neurodegeneration is demonstrated by the neuroprotective properties of Parkin in counteracting oxidative stress and improving mitochondrial function. The involvement of Parkin and PINK1 in mitochondrial dysfunction, oxidative injury, and impaired functioning of the ubiquitin–proteasome system has been investigated in light of Parkinson’s disease pathogenesis (Cookson and Bandmann 2010; Okatsu et al. 2012).
The protein kinase microtubule affinity-regulating kinase 2 (MARK2) also plays key roles in several cellular processes underpinning neurodegenerative diseases (Gu et al. 2013). MARK2 phosphorylates the N-terminal Thr-313 and activates PINK1 (Matenia et al. 2012). Thr-313 is the primary phosphorylation site, mutated to a non-phosphorylatable residue in a frequent variant of Parkinson’s disease (Matenia et al. 2012). The importance of this PINK1 phosphorylation site is emphasized by the fact that the expression of the mutation of Thr-313 in PINK1 shows severe toxicity for cells (both CHO and neuronal cells) and leads to abnormal mitochondrial accumulations in the cell soma or degradation of mitochondria (Matenia et al. 2012). The mutation could also have effects on known PINK1 substrates like Omi/HtrA2 or TRAP-1 (Pridgeon et al. 2007). Both MARK2 and PINK1 colocalize with mitochondria, especially in axons and dendrites, and regulate their transport; therefore, MARK2 may be an upstream modulator of PINK1 that modulates mitochondrial trafficking in neuronal cells. Furthermore, it is suggested that this phosphorylation consequently enhances the binding and possibly the phosphorylation of Parkin by PINK1. As previously discussed, Parkin is recruited via PINK1 to defective mitochondria inducing their degradation by mitophagy. This effect seems to be also influenced by MARK2; thus, failure of this pathway results in the accumulation of mitochondria in the cell soma (Matenia et al. 2012). The MARK2–PINK1 cascade provides new insights into the control of mitochondrial trafficking in neurons. Alterations in mitochondrial homeostasis have been implicated as an important source of many neurodegenerative diseases; thus, suppression of PINK1 kinase activity and/or downregulation of PINK1 transcription contribute to Parkinson’s disease pathogenesis. Nonetheless, enhanced PINK1 kinase activity also induces neuronal cell death (Matenia et al. 2012). As a result, the importance of a tight regulation of PINK1 depending on MARK2 is crucial and failure of this balance contributes to the development of Parkinson’s disease (Matsuda et al. 2013).
Moreover, Parkin-induced mitophagy contributes to the mitochondrial control preventing neurodegeneration. However, oxidative and dopaminergic stress are thought to impair the function of Parkin through direct posttranslational modification (Imam et al. 2011). The exact mechanisms underlying impairment of Parkin function by these stressors remain elusive but an increase in c-Abl activity has been observed (Cao et al. 2001; Sun et al. 2000). The c-Abl tyrosine (Tyr) kinase is involved in diverse cellular activities depending on its subcellular localization. c-Abl can promote mitogenesis when located in cytoplasm, cell cycle arrest when activated in the nucleus, and upon translocation to the mitochondria can induce the loss of ∆Ψm, depletion of ATP, and apoptotic/necrotic cell death (Constance et al. 2012; Qi and Mochly-Rosen 2008). As mentioned before, oxidative DNA damage occurs to a higher extent in Parkinson’s disease individuals compared with age-matched controls (Alam et al. 1997). Studies conducted in vitro and in vivo indicate an association between c-Abl and Parkin. Specifically, compelling evidence suggests that c-Abl phosphorylates Parkin at Tyr-143 leading to the loss of Parkin function and disease progression in sporadic Parkinson’s disease (Imam et al. 2011). Activation of c-Abl and Parkin Tyr phosphorylation occurs after oxidative and dopaminergic stress both in vitro and in vivo, causing significant loss of Parkin’s E3 ubiquitin ligase activity and leading to the accumulation of neurotoxic aminoacyl tRNA synthetase complex-interacting multifunctional protein 2 (AIMP2) and fructose-1,6-bisphosphatase 1 (FBP-1), ultimately compromising Parkin’s protective function (Imam et al. 2011). The latter are two toxic substrates of Parkin detected in the striatum. Importantly, pharmacological inhibition of c-Abl by STI-571 enhances E3 ubiquitin ligase activity of Parkin and offers new therapeutic options for blocking Parkinson’s disease progression (Imam et al. 2011; Ko et al. 2010). In this manner, c-Abl can induce an alternative oxidative stress pathway via inhibiting the ubiquitin-mediated pathway by Parkin, and it can promote the accumulation of misfolded protein and toxic substrates (i.e., AIMP2 and FBP-1) (Fig. 2) (Gonfloni et al. 2012).
Moreover, c-Abl activity seems to have a role in Parkinson’s disease development by regulating the activation of protein kinase C delta (PKCδ). Studies have demonstrated that PKCδ, a prominent member of novel PKCs, plays a pro-apoptotic role in various cell types (Kanthasamy et al. 2003). In cell culture models of Parkinson’s disease, oxidative stress activates PKCδ through a caspase-3-dependent proteolytic cleavage that induces apoptotic cell death (Kanthasamy et al. 2003). Interestingly, proteolytic activation of PKCδ is regulated through phosphorylation of its Tyr residues. Evidence regarding a functional interaction between PKCδ and c-Abl has been provided following oxidative stress response (Sun et al. 2000). Indeed, in response to oxidative stress, cytoplasmic c-Abl moves to mitochondria, phosphorylates PKCδ on Tyr-311, and this modification amplifies apoptotic signals via activation of the mitochondrial apoptotic pathway and leads to mitochondrial dysfunction and cell death (Fig. 2) (Lu et al. 2007; Qi and Mochly-Rosen 2008).
The PINK1 Anti-apoptotic Pathway
Besides its role in mitophagy, PINK1’s cooperation with different molecules is involved in survival pathways to protect mitochondria against oxidative stress. First of all, PINK1 has been shown to phosphorylate TNF receptor-associated protein 1 (TRAP1), a mitochondrial chaperone of the heat-shock protein 90 (Hsp90) family also known as Hsp75, and thus to increase neuronal survival against oxidative stress or heat shock by preventing the release of cytochrome c (cyt c) and apoptosis (Fig. 3) (Pridgeon et al. 2007). TRAP1 may be a direct substrate for PINK1, which localizes primarily in the mitochondrial matrix and at extra mitochondrial sites. Upon induction of oxidative stress, PINK1 may regulate TRAP1 function constitutively (Bueler 2009). Phosphorylated TRAP1 is proposed to act as a chaperone to hamper protein misfolding and misassembly of respiratory complexes in mitochondria during oxidative stress (Plun-Favreau et al. 2007). Given that TRAP1 acts as a molecular chaperone in the clearance of misfolded proteins, it may lead to enhanced molecular quality control in mitochondria, therefore decreasing the demand for organelle quality control as a clearance mechanism for mitochondria overwhelmed by excessive protein misfolding (Costa et al. 2013).
The PINK1-dependent phosphorylation of HtrA2 increases its protease activity leading to enhanced survival against oxidative stress (Clausen et al. 2011). PINK1 serves as an adaptor in a trimeric complex, to bridge between p38 kinase and HtrA2 in order to prevent unwanted proteolysis of HtrA2 (Alnemri 2007). Furthermore, HtrA2 is not essential for all the protective functions of PINK1; thus, PARL seems to regulate HtrA2 via HAX1. HAX1 functions as a substrate of HtrA2 as well, reflecting a delicate balance between mitophagy and apoptosis. Finally, PINK1 phosphorylates and activates TRAP1 to inhibit the release of cyt c and apoptosis and hinder protein misfolding and misassembly of respiratory complexes. Cyt c cytochrome c, HAX1 HS1-associated protein X-1, HtrA2 high-temperature requirement A2 protease, IMM inner mitochondrial membrane, IMS intermembrane space, OMM outer mitochondrial membrane, PARL presenilin-associated rhomboid-like serine protease, PINK1 PTEN-induced kinase 1, TRAP1 TNF receptor-associated protein 1
Adding to the variety of survival functions of PINK1, its association with the mammalian high-temperature requirement A2 protease (HtrA2, also known as Omi) has been also investigated. HtrA2 belongs to a widely conserved family of serine proteases involved in various aspects of protein quality control and cell fate but it has received more attention than other HtrA family members because of its potential role in the regulation of apoptosis (Fig. 3) (Clausen et al. 2011). In healthy cells, HtrA2 resides in the intermembrane space of mitochondria. Apoptotic stimuli lead to HtrA2 release into the cytosol where it inactivates the caspase-inhibitory activity. HtrA2 proteolytic activity has also been suggested to ignite a caspase-independent cell death pathway (Fig. 3) (Alnemri 2007). Jones et al. (2003) revealed that the mnd2, a mouse model of neurodegeneration with features resembling Parkinson’s disease, results from a missense mutation that inactivates the proteolytic activity of HtrA2. Further analysis demonstrated that cells from these mice or from HtrA2 knockout mice exhibit a defective mitochondrial membrane potential that led to increased apoptosis, especially in striatal neurons and, consequently, to neurodegeneration (Martins et al. 2004). This supports the notion that HtrA2 functions primarily as a survival rather than a death protease.
Indeed, HtrA2 is indirectly phosphorylated and interacts with PINK1 as part of a signaling pathway (Fig. 3) (Plun-Favreau et al. 2007). The PINK1-dependent phosphorylation of HtrA2 augments its protease activity leading to enhanced survival against oxidative stress (Plun-Favreau et al. 2007, 2008). The HtrA2 is also phosphorylated upon activation of the p38 stress-activated protein kinase (SAPK) pathway, occurring in a PINK1-dependent manner (Plun-Favreau et al. 2007). Structural studies revealed that Ser-142 in the protease domain and Ser-400 in the PSD95/DLG1/ZO1 (PDZ) domain of HtrA2 are two potential phosphorylation sites for proline-directed Ser/Thr kinases. Point mutations in these regions of HtrA2 are a susceptibility factor for Parkinson’s disease. More specifically, PINK1 does not seem to be directly responsible for phosphorylating HtrA2 on Ser-142 upon activation of the p38 pathway; instead, it might serve as an adaptor in a trimeric complex to bridge between p38 kinase and HtrA2 (Fig. 3) (Alnemri 2007; Li et al. 2002). Furthermore, it appears that p38 and PINK1 operate upstream of HtrA2 in an external stress-sensing pathway to phosphorylate HtrA2 (Valente et al. 2004). As with many other proteases, the proteolytic activity of HtrA2 is tightly regulated to prevent unwanted proteolysis.
However, it has been shown in Drosophila that HtrA2 is not essential for all the protective functions of PINK1 (Tain et al. 2009; Yun et al. 2008). It is noteworthy that in Drosophila, the mitochondrial protease Rhomboid-7, equivalent to PARL in mammals, can physically interact with HtrA2, and that Rhomboid-7 is both necessary and sufficient to process one HtrA2 isoform in vitro and in vivo (Whitworth et al. 2008). In contrast, vertebrate PARL does not directly interact with HtrA2 and requires HS1-associated protein X-1 (HAX1), a B-cell leukemia-2 (Bcl-2) family protein not found in Drosophila (Fig. 3). Notably, it was first identified as a cleavage target of HtrA2 in the mnd2 mouse model. Degradation of HAX1 by HtrA2 was observed when cells were treated with various apoptotic inducers (Cilenti et al. 2004). It is important that HAX1 functions not only as a substrate of HtrA2, but also as a regulator of the mitochondrial import of HtrA2 through the presentation of HtrA2 to PARL. Collectively, these findings suggest that the interaction or balance between HAX1 and HtrA2 is crucial for both mitophagy and apoptosis. On the one hand, as an upstream modulator of HtrA2, HAX1 ensures the proper localization of functional HtrA2 to protect cells from stresses; on the other hand, as a specific substrate of HtrA2, HAX1 can be digested by HtrA2 to elicit mitophagy or to stimulate apoptosis when cells are ultimately sentenced to death (Li et al. 2010a, b).
PINK1 Participates in Microglial Inflammatory Response
Further to genetic background, environmental factors, such as environmental toxins or lifestyle factors, may have a role in Parkinson’s disease pathogenesis (Dawson et al. 2010). However, the most important “environmental” factor that regulates neuronal function and survival is glia (astrocytes and microglia). Accordingly, glia has recently been suggested as a turning point in the therapeutic strategy for Parkinson’s disease (Yin et al. 2010).
It is known that in response to brain injury, microglia and neurons die at injury sites (Jeong et al. 2010; Ji et al. 2007; Min et al. 2012), and that microglia in the penumbra region rapidly isolate these sites and produce cytokines such as interleukin (IL)-1β (IL-1β), which are not harmful to brain cells. It has been reported that the expression of pro-inflammatory cytokines increases in CSF and brain parenchyma of patients with Parkinson’s disease (Kim et al. 2013). Furthermore, inflammatory responses including microglia activation and expression of inflammatory cytokines increase in animal models of Parkinson’s disease (Beal 2003; Hald and Lotharius 2005). Studies have shown that brain inflammation is a risk factor for neurodegenerative diseases, including Parkinson’s disease (Whitton 2007), and anti-inflammatory drugs such as dexamethasone, ibuprofen, and rofecoxib display neuroprotective effects (Kurkowska-Jastrzebska et al. 2004). Specifically, it has been demonstrated that PINK1 deficiency augments the expression of pro-inflammatory cytokines such as tumor necrosis factor alpha (TNF-α), IL-1β, and IL-6 (Kim et al. 2013). Moreover, PINK1 knockout mice exhibit higher striatal levels of IL-1β, IL- 12, and IL-10 in response to lipopolysaccharide (Akundi et al. 2011). As explained previously, PINK1-deficient cells are vulnerable to apoptosis compared to wild-type cells (Valente et al. 2004). Therefore, it is critical to investigate the signaling pathway operating during brain inflammation.
The most important signaling pathways engaged in neurodegenerative disorders are the mitogen-activated protein kinase (MAPK) and the signal transducer and activator of transcription (STAT) signal transduction cascades (Pyo et al. 1998; Ryu et al. 2000). However, in a PINK1 knockout mouse model, the signaling pathways that increase inflammatory responses were slightly different. Kim et al. (2013) documented significant difference only in the activation pattern of STAT3. They observed a degradation of the nuclear factor kappa B (NF-κB) inhibitory protein inhibitory kappa B (IκB) due to STAT3 activation, which resulted in increased pro-inflammatory cytokines. It has been reported that STAT3 blocks NF-κB activation by preventing IκB phosphorylation and degradation (Yu et al. 2009). In addition, a recent study revealed that PINK1-mediated phosphorylation activates Parkin’s E3 ubiquitin ligase function and enhances Parkin-mediated ubiquitin signaling through the NF-κB pathway (Sha et al. 2010). Moreover, this study provided evidence that deregulation of the PINK1/Parkin/NF-κB cytoprotective pathway, which could be caused by PINK1 or Parkin mutations, is a common pathogenic mechanism leading to neurodegeneration in early-onset familial Parkinson’s disease (Sha et al. 2010).
The phosphoinositide-3 kinase (PI3K)/Akt signaling axis may be another factor regulating the inflammatory responses, independently of the STAT3 or IκB/NF-κB pathways. The importance of the PI3K/Akt pathway in inflammation has been documented in rheumatoid arthritis, multiple sclerosis, and asthma (Busse and Lemanske 2001; Camps et al. 2005; Sospedra and Martin 2005). Inhibiting PI3K augments TNF-α and IL-6 expression in macrophages (Medina et al. 2010). Because the PINK1 defect promotes brain inflammation in response to injury, the function of PINK1 may be more pertinent in injury states than in physiological states. Thus, a defect in PINK1 could exaggerate brain inflammation in the injured brain, increasing brain damage and resulting in DAergic neuronal death (Kim et al. 2013). Although PINK1 is involved in mitochondrial function, a recent report demonstrated that PINK1 has another action point in the cytoplasm (Murata et al. 2011). Specifically, phosphorylation of Akt at Ser-473 was enhanced by the overexpression of PINK1 independently of PI3K in SH-SY5Y cells, a cellular model of Parkinson’s disease. The Akt activation increased the protection of cells from various cytotoxic agents, including oxidative stress (Murata et al. 2011).
Environmental Toxins: The Paradigm of MPTP
The vast majority of Parkinson’s disease cases are a combination of genetic and environmental influences that may vary from person to person, and in this review, we briefly discuss the association of genetic susceptibility and aging with oxidative stress and inflammation as a risk factor. The emerging concept of the onset and progression of DAergic neuronal degeneration in vivo is that certain environmental agents act in cooperation with genetic factors (Yin et al. 2010). Hints that environmental toxins might play a role in the molecular pathology of Parkinson’s disease first appeared after the accidental administration of 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP) in a group of young drug users in the 70s, who eventually developed a clinical phenotype reminiscent of late-stage Parkinson’s disease, albeit in the absence of LBs pathology (Whitton 2007). It was the first proof that exposure to an environmental substance could produce parkinsonism in humans (Cui et al. 2004; Deas et al. 2009).
In addition to MPTP, other environmental toxins have been identified as contributors to DAergic neuronal cell death and parkinsonism, supporting further the link between environmental exposure to pesticides and a risk of developing Parkinson’s disease (Shulman et al. 2011). Four individual pesticides were found to increase the risk of Parkinson’s disease such as dieldrin, maneb (MN), paraquat (PQ), and rotenone (Horowitz and Greenamyre 2010), with the latter two behaving as mitochondrial toxins in a mode similar to MPTP (Shulman et al. 2011). In rural environments where workers were coexposed to PQ and MN, several studies have clearly shown a marked increase in Parkinson’s type neurodegeneration (Gollamudi et al. 2012). Unraveling the signaling pathways following exposure to these toxins may offer a potential therapeutic approach in the pathology of Parkinson’s disease.
MPTP was subsequently identified as a potent neurotoxin that can readily cross the blood–brain barrier and is metabolized in astrocytes to 4-phenyl-2,3-dihydropyridinium ion (MPP+). The latter is a powerful mitochondrial Complex I inhibitor that causes abnormal energy metabolism and increased ROS production, and is then selectively transported into DAergic neurons via dopamine transporter (DAT), ultimately leading to cell death via mitochondrial impairment (Horowitz and Greenamyre 2010). In normal conditions, MPP+ generates several ROS (Esposito et al. 2002), resulting in lipid peroxidation, DNA fragmentation, mitochondrial harm, lactate dehydrogenase (LDH) leakage, GSH depletion, reduction of Na+/K+-ATPase and catalase activities, increase in caspase-3 activity, and eventually cell death (Chan et al. 2009; Harish et al. 2010). Consequently, the MPTP model constitutes the best-characterized toxin paradigm for Parkinson’s disease, clearly reflecting most of its clinical and pathological hallmarks (Langston et al. 1984; Li et al. 2010a, b).
As analyzed beforehand, in the striatum bordering the subventricular zone (SVZ) of Parkinson’s disease experimental models, glia exhibits remarkable morphological and functional changes, including the expression of an array of pro-inflammatory cytokines and chemokines as well as production of ROS (Gao et al. 2008; Hirsch and Hunot 2009; Marchetti and Abbracchio 2005). Of special interest, MPTP-dependent inflammatory mechanisms are recognized to contribute to nigrostriatal DAergic degeneration and self-repair (L’Episcopo et al. 2010). During the last decade, many investigators have attempted to illuminate the mechanisms underlying the so-called SVZ stem cell niche, which includes neuronal progenitors cells (NPCs) and surrounding glia. Wnt/β-catenin signaling is a vital pathway regulating self-renewal and differentiation of neural stem cells (Logan and Nusse 2004). Stabilized β-catenin, a chief transcriptional regulator, can enter the nucleus and associate with T-cell factor/lymphoid enhancer-binding factor (TCF/LEF) transcription factors, leading to the expression of Wnt-target genes involved in cell survival, proliferation, and differentiation. A volume of data suggests a role for this pathway in adult neurogenesis, providing a novel therapeutic approach in many neurodegenerative diseases, such as Parkinson’s disease (Kuwabara et al. 2009; Munji et al. 2011; Wexler et al. 2008; Zhang et al. 2011). Because Wnt/β-catenin signaling controls the expression of diverse target genes, deregulation of this signaling cascade is involved in various neurodegenerative disorders (Inestrosa and Arenas 2010; Kim et al. 2011; L’Episcopo et al. 2011a; Shruster et al. 2011).
In Parkinson’s disease, the Wnt/β-catenin pathway plays also a fundamental role in the generation, survival, and protection of midbrain DAergic neurons (Inestrosa and Arenas 2010; L’Episcopo et al. 2011a; Prakash et al. 2006). Interestingly, in response to nigrostriatal injury, reactive astrocytes express Wnt1 and protect DAergic neurons against different neurotoxic insults via the potentiation of Wnt/β-catenin signaling (L’Episcopo et al. 2011a, b). The exogenous MPTP leads to the induction of the caspase-3-dependent apoptotic pathway in a dose-dependent fashion (L’Episcopo et al. 2012). However, exogenous manipulation of Wnt/β-catenin signaling in primary mesencephalic neurons exerts potent neuroprotective effects against oxidative stress and MPTP-induced DAergic cell death in vitro and in vivo (L’Episcopo et al. 2011a, b). Additional studies are necessary to address the significance and implications of Wnt/β-catenin signaling disruption in conditions associated with exacerbated inflammation, neurodegeneration, and impaired neurogenesis such as Parkinson’s disease.
Last but not least, several studies lately have focused on the discovery of supplements that can enhance the amount of the daily antioxidant intake. Astaxanthin (3,3′-dihydroxy-β,β-carotene-4,4′-dioneastaxanthin; ATX), a non-provitamin A carotenoid found in the red pigment of shrimp, crab, salmon, and asteroidean, seems to have neuroprotective effects in a dose-dependent manner following MPP+-induced oxidative damage (Ye et al. 2013), thus providing a promising candidate for chemoprevention and chemotherapy strategies for Parkinson’s disease. Naguib (2000) using rats fed on natural ATX found that ATX crossed the blood–brain barrier in mammals, extending its antioxidant benefits into the brain. As a result, a number of in vitro and in vivo studies of ATX have demonstrated its antioxidant and neuroprotective effects, with the antioxidant properties of ATX being 100–1,000 times more effective than vitamin E (Liu et al. 2009). ATX, as an exogenous environmental agent, may diminish the Parkinson’s disease phenotype and offer a valuable curative tool for the treatment for other progressive neurodegenerative diseases as well.
Conclusion and Future Perspectives
Parkinson’s disease is a multivariate disorder caused by genetic background and environmental factors. Many studies try to tackle different aspects of the disease in order to elucidate the mechanisms underpinning its pathogenesis. Signaling networks comprised of multiple layers of interacting proteins are an imperative key in this direction. Activation of most cell signaling circuits is modulated by feedback control, and disease conditions are often caused by the loss of this control. A comprehensive understanding of the complexities of signaling networks is required to design effective therapies without inducing off-target effects. In neurodegenerative disorders, the temporal and spatial de-organization of signaling complexes can cause a system failure ending in neuronal loss. Protein aggregation and organelle malfunction are hallmarks of many late-onset neurodegenerative diseases. Mitochondrial damage and dysfunction are indeed linked to neurodegeneration in a gamut of animal models.
Many therapeutic regimens have been proposed to reduce the symptoms of Parkinson’s disease. Clearance of misfolded proteins and damaged organelles may be considered an effective recovery strategy for stressed neuronal cells. In addition, the genetic “repair” of mutated proteins that participate in this process may lead to positive results. The ex vivo replacement of damaged neurons by endogenous stem cells of SVZ is another therapeutic strategy. Lately, antioxidants have been considered as agents of great importance toward the prevention of oxidative stress in diverse diseases such as cancer or neurodegenerative disorders.
In summary, this review focused on the complex interaction and complementary interrelationship between oxidative stress and Parkinson’s disease. To this end, the possible effect of the Parkinson’s disease-related gene PINK1 in the oxidative stress pathogenic pathway and its role against oxidative stress by preventing mitophagy, apoptosis, or the microglial inflammatory response were discussed. The effect of environmental toxins, such as MPTP, in nigrostriatal DAergic degeneration strengthens the notion that oxidative stress is central to the pathways leading to the development of Parkinson’s disease.
Abbreviations
- AIMP2:
-
Aminoacyl tRNA synthetase complex-interacting multifunctional protein 2
- AMPA:
-
Amino-3-hydroxy-5-methyl-4-isoxazole propionic acid
- α-syn:
-
Alpha synuclein
- ATX:
-
3,3′-Dihydroxy-β,β-carotene-4,4′-dioneastaxanthin
- Bcl-2:
-
B cell leukemia-2
- CSF:
-
Cerebrospinal fluid
- CNS:
-
Central nervous system
- Cyt c:
-
Cytochrome c
- DA:
-
Dopamine
- DAT:
-
Dopamine transporter
- ER:
-
Endoplasmic reticulum
- ERK:
-
Extracellular signal-regulated kinase
- FBP-1:
-
Fructose-1,6-bisphosphatase 1
- GSH:
-
Glutathione
- HAX1:
-
HS1-associated protein X-1
- Hsp:
-
Heat-shock protein
- HtrA2:
-
High-temperature requirement A2 protease
- IκB:
-
Inhibitory kappa B
- IL:
-
Interleukin
- IMM:
-
Inner mitochondrial membrane
- IMS:
-
Intermembrane space
- JNK:
-
c-Jun N-terminal kinase
- LBs:
-
Lewy bodies
- LDH:
-
Lactate dehydrogenase
- LNs:
-
Lewy neurites
- MAPK:
-
Mitogen-activated protein kinase
- MARK2:
-
Microtubule affinity-regulating kinase 2
- MN:
-
Maneb
- MPP+:
-
4-Phenyl-2,3-dihydropyridinium ion
- MPTP:
-
1-Methyl-4-phenyl-1,2,3,6-tetrahydropyridine
- mtDNA:
-
Mitochondrial DNA
- NF-κB:
-
Nuclear factor kappa B
- NM:
-
Neuromelanin
- NMDA:
-
N-methyl-d-aspartate
- NMDAR:
-
NMDA receptor
- NOS:
-
Nitric oxide synthase
- NPCs:
-
Neuronal progenitor cells
- OMM:
-
Outer mitochondrial membrane
- RNS:
-
Reactive nitrogen species
- ROS:
-
Reactive oxygen species
- PARL:
-
Presenilin-associated rhomboid-like serine protease
- p-α-syn:
-
Phosphorylated α-syn
- PDZ:
-
Postsynaptic density protein (PSD95)/Drosophila disc large tumor suppressor (Dlg1)/zonula occludens-1 protein (Zo-1)
- PI3K:
-
Phosphoinositide-3 kinase
- PINK1:
-
PTEN-induced kinase 1
- PKCδ:
-
Protein kinase C delta
- PQ:
-
Paraquat
- SAPK:
-
Stress-activated protein kinase
- SN:
-
Substantia nigra
- SNpc:
-
Substantia nigra pars compacta
- SOD:
-
Superoxide dismutase
- STAT:
-
Signal transducer and activator of transcription
- SVZ:
-
Subventricular zone
- TCF/LEF:
-
T-cell factor/lymphoid enhancer-binding factor
- TNF-α:
-
Tumor necrosis factor alpha
- TRAP1:
-
TNF receptor-associated protein
- UPS:
-
Ubiquitin–proteasome system
- ∆Ψm:
-
Mitochondrial membrane potential
References
Akundi, R. S., et al. (2011). Increased mitochondrial calcium sensitivity and abnormal expression of innate immunity genes precede dopaminergic defects in Pink1-deficient mice. PLoS ONE, 6(1), e16038.
Alam, Z. I., et al. (1997). Oxidative DNA damage in the parkinsonian brain: an apparent selective increase in 8-hydroxyguanine levels in substantia nigra. Journal of Neurochemistry, 69(3), 1196–1203.
Alnemri, E. S. (2007). HtrA2 and Parkinson’s disease: Think PINK? Nature Cell Biology, 9(11), 1227–1229.
Andersen, J. K. (2004). Oxidative stress in neurodegeneration: Cause or consequence? Nature Medicine, 10(Suppl), S18–S25.
Arduino, D. M., Esteves, A. R., & Cardoso, S. M. (2013). Mitochondria drive autophagy pathology via microtubule disassembly: A new hypothesis for Parkinson disease. Autophagy, 9(1), 112–114.
Barnham, K. J., Masters, C. L., & Bush, A. I. (2004). Neurodegenerative diseases and oxidative stress. Nature Reviews Drug Discovery, 3(3), 205–214.
Beal, M. F. (2003). Mitochondria, oxidative damage, and inflammation in Parkinson’s disease. Annals of the New York Academy of Sciences, 991, 120–131.
Blum, D., et al. (2001). Molecular pathways involved in the neurotoxicity of 6-OHDA, dopamine and MPTP: Contribution to the apoptotic theory in Parkinson’s disease. Progress in Neurobiology, 65(2), 135–172.
Braak, H., & Braak, E. (2000). Pathoanatomy of Parkinson’s disease. Journal of Neurology, 247(Suppl 2), II3–II10.
Bueler, H. (2009). Impaired mitochondrial dynamics and function in the pathogenesis of Parkinson’s disease. Experimental Neurology, 218(2), 235–246.
Busse, W. W., & Lemanske, R. F., Jr. (2001). Asthma. New England Journal of Medicine, 344(5), 350–362.
Camps, M., et al. (2005). Blockade of PI3Kgamma suppresses joint inflammation and damage in mouse models of rheumatoid arthritis. Nature Medicine, 11(9), 936–943.
Cao, C., et al. (2001). The ARG tyrosine kinase interacts with Siva-1 in the apoptotic response to oxidative stress. Journal of Biological Chemistry, 276(15), 11465–11468.
Chan, K. C., Mong, M. C., & Yin, M. C. (2009). Antioxidative and anti-inflammatory neuroprotective effects of astaxanthin and canthaxanthin in nerve growth factor differentiated PC12 cells. Journal of Food Science, 74(7), H225–H231.
Ciccone, S., et al. (2013). Parkinson’s disease: A complex interplay of mitochondrial DNA alterations and oxidative stress. International Journal of Molecular Sciences, 14(2), 2388–2409.
Cilenti, L., et al. (2004). Regulation of HAX-1 anti-apoptotic protein by Omi/HtrA2 protease during cell death. Journal of Biological Chemistry, 279(48), 50295–50301.
Clausen, T., et al. (2011). HTRA proteases: Regulated proteolysis in protein quality control. Nature Reviews Molecular Cell Biology, 12, 152–162.
Constance, J., Despres, S., Nishida, A., & Lim, C. (2012). Selective targeting of c-Abl via a cryptic mitochondrial targeting signal activated by cellular redox status in leukemic and breast cancer cells. Pharmaceutical Research, 29(8), 2317–2328.
Cookson, M. R., & Bandmann, O. (2010). Parkinson’s disease: Insights from pathways. Human Molecular Genetics, 19(R1), R21–R27.
Corti, O., Lesage, S., & Brice, A. (2011). What genetics tells us about the causes and mechanisms of Parkinson’s disease. Physiological Reviews, 91(4), 1161–1218.
Costa, A. C., Loh, S. H. Y., & Martins, M. (2013). Drosophila Trap1 protects against mitochondrial dysfunction in a PINK1/parkin model of Parkinson’s disease. Cell Death Disease, 4, e467; doi:10.1038/cddis.2012.205.
Crabtree, D. M., & Zhang, J. (2012). Genetically engineered mouse models of Parkinson’s disease. Brain Research Bulletin, 88(1), 13–32.
Crosiers, D., et al. (2011). Parkinson disease: Insights in clinical, genetic and pathological features of monogenic disease subtypes. Journal of Chemical Neuroanatomy, 42(2), 131–141.
Cui, K., et al. (2004). Role of oxidative stress in neurodegeneration: Recent developments in assay methods for oxidative stress and nutraceutical antioxidants. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 28(5), 771–799.
Dalle-Donne, I., et al. (2003). Protein carbonylation in human diseases. Trends in Molecular Medicine, 9(4), 169–176.
Dawson, T. M., Ko, H. S., & Dawson, V. L. (2010). Genetic animal models of Parkinson’s disease. Neuron, 66(5), 646–661.
Deas, E., Plun-Favreau, H., & Wood, N. W. (2009). PINK1 function in health and disease. EMBO Mol Med, 1(3), 152–165.
Deas, E., et al. (2011). PINK1 cleavage at position A103 by the mitochondrial protease PARL. Human Molecular Genetics, 20(5), 867–879.
Esposito, E., et al. (2002). A review of specific dietary antioxidants and the effects on biochemical mechanisms related to neurodegenerative processes. Neurobiology of Aging, 23(5), 719–735.
Feng, L. R., & Maguire-Zeiss, K. A. (2010). Gene therapy in Parkinson’s disease: Rationale and current status. CNS Drugs, 24(3), 177–192.
Fujiwara, H., et al. (2002). Alpha-Synuclein is phosphorylated in synucleinopathy lesions. Nature Cell Biology, 4(2), 160–164.
Gao, H. M., et al. (2008). Neuroinflammation and oxidation/nitration of alpha-synuclein linked to dopaminergic neurodegeneration. Journal of Neuroscience, 28(30), 7687–7698.
Gilgun-Sherki, Y., Melamed, E., & Offen, D. (2001). Oxidative stress induced-neurodegenerative diseases: The need for antioxidants that penetrate the blood brain barrier. Neuropharmacology, 40(8), 959–975.
Gollamudi, S., et al. (2012). Concordant signaling pathways produced by pesticide exposure in mice correspond to pathways identified in human Parkinson’s disease. PLoS ONE, 7(5), e36191.
Gonfloni, S., et al. (2012). Oxidative stress, DNA damage, and c-Abl signaling: At the crossroad in neurodegenerative diseases? International Journal of Cell Biology, 2012, 683097.
Graybiel, A. M. (2005). The basal ganglia: Learning new tricks and loving it. Current Opinion in Neurobiology, 15(6), 638–644.
Greene, A. W., et al. (2012). Mitochondrial processing peptidase regulates PINK1 processing, import and Parkin recruitment. EMBO Reports, 13(4), 378–385.
Gu, G. J., et al. (2013). Elevated MARK2-dependent phosphorylation of Tau in Alzheimer’s disease. Journal of Alzheimer’s Disease, 33(3), 699–713.
Guzman, J. N., et al. (2010). Oxidant stress evoked by pacemaking in dopaminergic neurons is attenuated by DJ-1. Nature, 468(7324), 696–700.
Hald, A., & Lotharius, J. (2005). Oxidative stress and inflammation in Parkinson’s disease: Is there a causal link? Experimental Neurology, 193(2), 279–290.
Harish, G., et al. (2010). Bioconjugates of curcumin display improved protection against glutathione depletion mediated oxidative stress in a dopaminergic neuronal cell line: Implications for Parkinson’s disease. Bioorganic & Medicinal Chemistry, 18(7), 2631–2638.
Heeman, B., et al. (2011). Depletion of PINK1 affects mitochondrial metabolism, calcium homeostasis and energy maintenance. Journal of Cell Science, 24(Pt 7), 1115–1125.
Henchcliffe, C., & Beal, M. F. (2008). Mitochondrial biology and oxidative stress in Parkinson disease pathogenesis. Nature Clinical Practice Neurology, 4(11), 600–609.
Hirsch, E. C., & Hunot, S. (2009). Neuroinflammation in Parkinson’s disease: A target for neuroprotection? Lancet Neurology, 8(4), 382–397.
Horowitz, M. P., & Greenamyre, J. T. (2010). Gene-environment interactions in Parkinson’s disease: The importance of animal modeling. Clinical Pharmacology and Therapeutics, 88(4), 467–474.
Ilic, T., et al. (1998). Oxidative stress and Parkinson’s disease. Vojnosanitetski Pregled., 55(5), 463–468.
Imam, S. Z., et al. (2011). Novel regulation of parkin function through c-Abl-mediated tyrosine phosphorylation: Implications for Parkinson’s disease. Journal of Neuroscience, 31(1), 157–163.
Inestrosa, N. C., & Arenas, E. (2010). Emerging roles of Wnts in the adult nervous system. Nature Reviews Neuroscience, 11(2), 77–86.
Jenner, P. (2003). Oxidative stress in Parkinson’s disease. Annals of Neurology, 53(Suppl 3), S26–S36.
Jeong, H. K., et al. (2010). Inflammatory responses are not sufficient to cause delayed neuronal death in ATP-induced acute brain injury. PLoS ONE, 10, e13756.
Ji, K. A., et al. (2007). Resident microglia die and infiltrated neutrophils and monocytes become major inflammatory cells in lipopolysaccharide-injected brain. Glia, 55(15), 1577–1588.
Johnson, K. A., Conn, P. J., & Niswender, C. M. (2009). Glutamate receptors as therapeutic targets for Parkinson’s disease. CNS & Neurological Disorders: Drug Targets, 8(6), 475–491.
Jones, J. M., et al. (2003). Loss of Omi mitochondrial protease activity causes the neuromuscular disorder of mnd2 mutant mice. Nature, 425(6959), 721–727.
Kanthasamy, A. G., et al. (2003). Proteolytic activation of proapoptotic kinase PKCdelta is regulated by overexpression of Bcl-2: Implications for oxidative stress and environmental factors in Parkinson’s disease. Annals of the New York Academy of Sciences, 1010, 683–686.
Kim, H. et al. (2011). Downregulation of Wnt/beta-catenin signaling causes degeneration of hippocampal neurons in vivo. Neurobiology of Aging, 32(12), 2316 e1–e15.
Kim, J., et al. (2013). PINK1 deficiency enhances inflammatory cytokine release from acutely prepared brain slices. Experimental Neurobiology, 22(1), 38–44.
Ko, H. S., et al. (2010). Phosphorylation by the c-Abl protein tyrosine kinase inhibits parkin’s ubiquitination and protective function. Proceedings of National Academic Science USA, 107(38), 16691–16696.
Kumar, K. R., Djarmati-Westenberger, A., & Grunewald, A. (2011). Genetics of Parkinson’s disease. Seminars in Neurology, 31(5), 433–440.
Kurkowska-Jastrzebska, I., et al. (2004). Dexamethasone protects against dopaminergic neurons damage in a mouse model of Parkinson’s disease. International Immunopharmacology, 4(10–11), 1307–1318.
Kuwabara, T., et al. (2009). Wnt-mediated activation of NeuroD1 and retro-elements during adult neurogenesis. Nature Neuroscience, 12(9), 1097–1105.
Kuzuhara, S., et al. (1988). Lewy bodies are ubiquitinated. A light and electron microscopic immunocytochemical study. Acta Neuropathologica, 75(4), 345–353.
L’Episcopo, F., et al. (2010). Glia as a turning point in the therapeutic strategy of Parkinson’s disease. CNS & Neurological Disorders: Drug Targets, 9(3), 349–372.
L’Episcopo, F., et al. (2011a). Reactive astrocytes and Wnt/beta-catenin signaling link nigrostriatal injury to repair in 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine model of Parkinson’s disease. Neurobiology of Diseases, 41(2), 508–527.
L’Episcopo, F., et al. (2011b). A Wnt1 regulated Frizzled-1/beta-Catenin signaling pathway as a candidate regulatory circuit controlling mesencephalic dopaminergic neuron-astrocyte crosstalk: Therapeutical relevance for neuron survival and neuroprotection. Molecular Neurodegeneration, 6, 49.
L’Episcopo, F., et al. (2012). Plasticity of subventricular zone neuroprogenitors in MPTP (1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine) mouse model of Parkinson’s disease involves cross talk between inflammatory and Wnt/beta-catenin signaling pathways: Functional consequences for neuroprotection and repair. Journal of Neuroscience, 32(6), 2062–2085.
Langston, J. W., et al. (1984). 1-Methyl-4-phenylpyridinium ion (MPP +): Identification of a metabolite of MPTP, a toxin selective to the substantia nigra. Neuroscience Letters, 48(1), 87–92.
Lesage, S., & Brice, A. (2012). Role of Mendelian genes in “sporadic” Parkinson’s disease. Parkinsonism & Related Disorders, 18(Suppl 1), S66–S70.
Li, W., et al. (2002). Structural insights into the pro-apoptotic function of mitochondrial serine protease HtrA2/Omi. Natural Structural Biology, 9(6), 436–441.
Li, B., et al. (2010a). Omi/HtrA2 is a positive regulator of autophagy that facilitates the degradation of mutant proteins involved in neurodegenerative diseases. Cell Death and Differentiation, 17, 1773–1784.
Li, X., et al. (2010b). Tetrahydroxystilbene glucoside attenuates MPP + -induced apoptosis in PC12 cells by inhibiting ROS generation and modulating JNK activation. Neuroscience Letters, 483(1), 1–5.
Liu, X., et al. (2009). Astaxanthin inhibits reactive oxygen species-mediated cellular toxicity in dopaminergic SH-SY5Y cells via mitochondria-targeted protective mechanism. Brain Research, 1254, 18–27.
Logan, C. Y., & Nusse, R. (2004). The Wnt signaling pathway in development and disease. Annual Review of Cell and Developmental Biology, 20, 781–810.
Lotharius, J., & Brundin, P. (2002). Pathogenesis of Parkinson’s disease: Dopamine, vesicles and alpha-synuclein. Nature Reviews Neuroscience, 3(12), 932–942.
Lu, W., et al. (2007). The phosphorylation of tyrosine 332 is necessary for the caspase 3-dependent cleavage of PKCdelta and the regulation of cell apoptosis. Cellular Signalling, 19(10), 2165–2173.
Marchetti, B., & Abbracchio, M. P. (2005). To be or not to be (inflamed)—is that the question in anti-inflammatory drug therapy of neurodegenerative disorders? Trends in Pharmacological Sciences, 26(10), 517–525.
Marongiu, R., et al. (2009). Mutant Pink1 induces mitochondrial dysfunction in a neuronal cell model of Parkinson’s disease by disturbing calcium flux. Journal of Neurochemistry, 108(6), 1561–1574.
Martins, L. M., et al. (2004). Neuroprotective role of the Reaper-related serine protease HtrA2/Omi revealed by targeted deletion in mice. Molecular and Cellular Biology, 24(22), 9848–9862.
Matenia, D., et al. (2012). Microtubule affinity-regulating kinase 2 (MARK2) turns on phosphatase and tensin homolog (PTEN)-induced kinase 1 (PINK1) at Thr-313, a mutation site in Parkinson disease: Effects on mitochondrial transport. Journal of Biological Chemistry, 287(11), 8174–8186.
Matsuda, S., Kitagishi, Y., & Kobayashi, M. (2013). Function and characteristics of PINK1 in mitochondria. Oxidative Medicine and Cellular Longevity, 2013, 601587.
Medina, E. A., Morris, I. R., & Berton, M. T. (2010). Phosphatidylinositol 3-kinase activation attenuates the TLR2-mediated macrophage proinflammatory cytokine response to Francisella tularensis live vaccine strain. The Journal of Immunology, 185(12), 7562–7572.
Meissner, C., et al. (2011). The mitochondrial intramembrane protease PARL cleaves human Pink1 to regulate Pink1 trafficking. Journal of Neurochemistry, 117(5), 856–867.
Min, K. J., et al. (2012). Spatial and temporal correlation in progressive degeneration of neurons and astrocytes in contusion-induced spinal cord injury. Journal of Neuroinflammation, 9, 100.
Mosharov, E. V., et al. (2009). Interplay between cytosolic dopamine, calcium, and alpha-synuclein causes selective death of substantia nigra neurons. Neuron, 62(2), 218–229.
Munji, R. N., et al. (2011). Wnt signaling regulates neuronal differentiation of cortical intermediate progenitors. Journal of Neuroscience, 31(5), 1676–1687.
Murata, H., et al. (2011). A new cytosolic pathway from a Parkinson disease-associated kinase, BRPK/PINK1. Activation of Akt via mTORC2. Journal of Biological Chemistry, 286(9), 7182–7189.
Mythri, R. B., et al. (2011). Evaluation of markers of oxidative stress, antioxidant function and astrocytic proliferation in the striatum and frontal cortex of Parkinson’s disease brains. Neurochemical Research, 36(8), 1452–1463.
Mytilineou, C., Kramer, B. C., & Yabut, J. A. (2002). Glutathione depletion and oxidative stress. Parkinsonism & Related Disorders, 8(6), 385–387.
Naguib, Y. M. (2000). Antioxidant activities of astaxanthin and related carotenoids. Journal of Agriculture and Food Chemistry, 48(4), 1150–1154.
Nakamura, T., & Lipton, S. A. (2010). Preventing Ca2+-mediated nitrosative stress in neurodegenerative diseases: Possible pharmacological strategies. Cell Calcium, 47(2), 190–197.
Nakamura, T., & Lipton, S. A. (2011). Redox modulation by S-nitrosylation contributes to protein misfolding, mitochondrial dynamics, and neuronal synaptic damage in neurodegenerative diseases. Cell Death and Differentiation, 18(9), 1478–1486.
Narendra, D. P., et al. (2010). PINK1 is selectively stabilized on impaired mitochondria to activate Parkin. PLoS Biology, 8(1), e1000298.
Nicholls, D. G. (2010). Mitochondrial ion circuits. Essays in Biochemistry, 47, 25–35.
Novak, I. (2012). Mitophagy: A complex mechanism of mitochondrial removal. Antioxidants & Redox Signaling, 17(5), 794–802.
Okatsu, K., et al. (2012). PINK1 autophosphorylation upon membrane potential dissipation is essential for Parkin recruitment to damaged mitochondria. Nature Communications, 3, 1016.
Olanow, C. W., & McNaught, K. S. (2006). Ubiquitin–proteasome system and Parkinson’s disease. Movement Disorders, 21(11), 1806–1823.
Pearce, R. K., et al. (1997). Alterations in the distribution of glutathione in the substantia nigra in Parkinson’s disease. Journal of Neural Transmission, 104(6–7), 661–677.
Plun-Favreau, H., et al. (2007). The mitochondrial protease HtrA2 is regulated by Parkinson’s disease-associated kinase PINK1. Nature Cell Biology, 9(11), 1243–1252.
Plun-Favreau, H., et al. (2008). What have PINK1 and HtrA2 genes told us about the role of mitochondria in Parkinson’s disease? Annals of the New York Academy of Sciences, 1147, 30–36.
Prakash, N., et al. (2006). A Wnt1-regulated genetic network controls the identity and fate of midbrain-dopaminergic progenitors in vivo. Development, 133(1), 89–98.
Pridgeon, J. W., et al. (2007). PINK1 protects against oxidative stress by phosphorylating mitochondrial chaperone TRAP1. PLoS Biology, 5(7), e172.
Puopolo, M., Raviola, E., & Bean, B. P. (2007). Roles of subthreshold calcium current and sodium current in spontaneous firing of mouse midbrain dopamine neurons. Journal of Neuroscience, 27(3), 645–656.
Pyo, H., et al. (1998). Mitogen-activated protein kinases activated by lipopolysaccharide and beta-amyloid in cultured rat microglia. NeuroReport, 9(5), 871–874.
Qi, X., & Mochly-Rosen, D. (2008). The PKCdelta-Abl complex communicates ER stress to the mitochondria—an essential step in subsequent apoptosis. Journal of Cell Science, 121(6), 804–813.
Reichmann, H. (2011). View point: Etiology in Parkinson’s disease. Dual hit or spreading intoxication. Journal of the Neurological Sciences, 310(1–2), 9–11.
Roberts, R. A., et al. (2010). Toxicological and pathophysiological roles of reactive oxygen and nitrogen species. Toxicology, 276(2), 85–94.
Rochet, J. C., Hay, B. A., & Guo, M. (2012). Molecular insights into Parkinson’s disease. Progress in Molecular Biology and Translational Science, 107, 125–188.
Ryu, J., et al. (2000). Thrombin induces NO release from cultured rat microglia via protein kinase C, mitogen-activated protein kinase, and NF-kappa B. Journal of Biological Chemistry, 275(39), 29955–29959.
Selley, M. L. (1998). (E)-4-hydroxy-2-nonenal may be involved in the pathogenesis of Parkinson’s disease. Free Radical Biology & Medicine, 25(2), 169–174.
Sha, D., Chin, L. S., & Li, L. (2010). Phosphorylation of parkin by Parkinson disease-linked kinase PINK1 activates parkin E3 ligase function and NF-kB signaling. Human Molecular Genetics, 19(2), 352–363.
Shimura, H., et al. (2000). Familial Parkinson disease gene product, parkin, is a ubiquitin-protein ligase. Nature Genetics, 25(3), 302–305.
Shruster, A., et al. (2011). Wnt signaling pathway overcomes the disruption of neuronal differentiation of neural progenitor cells induced by oligomeric amyloid beta-peptide. Journal of Neurochemistry, 116(4), 522–529.
Shulman, J. M., De Jager, P. L., & Feany, M. B. (2011). Parkinson’s disease: Genetics and pathogenesis. Annual Review of Pathology: Mechanisms of Disease, 6, 193–222.
Song, S., et al. (2013). Characterization of phosphatase and tensin homolog (PTEN)-induced putative kinase 1 (PINK1) mutations associated with Parkinson’s disease in mammalian cells and Drosophila. Journal of Biological Chemistry, 288(8), 5660–5672.
Sospedra, M., & Martin, R. (2005). Immunology of multiple sclerosis. Annual Review of Immunology, 23, 683–747.
Strickland, D., & Bertoni, J. M. (2004). Parkinson’s prevalence estimated by a state registry. Movement Disorders, 19(3), 318–323.
Sun, X., et al. (2000). Interaction between protein kinase C delta and the c-Abl tyrosine kinase in the cellular response to oxidative stress. Journal of Biological Chemistry, 275(11), 7470–7473.
Sundal, C., et al. (2012). Autosomal dominant Parkinson’s disease. Parkinsonism & Related Disorders, 18(Suppl 1), S7–S10.
Surmeier, D. J., et al. (2011). The role of calcium and mitochondrial oxidant stress in the loss of substantia nigra pars compacta dopaminergic neurons in Parkinson’s disease. Neuroscience, 198, 221–231.
Tain, L. S., et al. (2009). Drosophila HtrA2 is dispensable for apoptosis but acts downstream of PINK1 independently from Parkin. Cell Death and Differentiation, 16(8), 1118–1125.
Toulouse, A., & Sullivan, A. M. (2008). Progress in Parkinson’s disease-where do we stand? Progress in Neurobiology, 85(4), 376–392.
Valente, E. M., et al. (2004). Hereditary early-onset Parkinson’s disease caused by mutations in PINK1. Science, 304(5674), 1158–1160.
Varcin, M., et al. (2012). Oxidative stress in genetic mouse models of Parkinson’s disease. Oxidative Medicine and Cellular Longevity, 2012, 624925.
Vinish, M., Anand, A., & Prabhakar, S. (2011). Altered oxidative stress levels in Indian Parkinson’s disease patients with PARK2 mutations. Acta Biochimica Polonica, 58(2), 165–169.
Wakabayashi, K., et al. (2007). The Lewy body in Parkinson’s disease: Molecules implicated in the formation and degradation of alpha-synuclein aggregates. Neuropathology, 27(5), 494–506.
Wexler, E. M., Geschwind, D. H., & Palmer, T. D. (2008). Lithium regulates adult hippocampal progenitor development through canonical Wnt pathway activation. Molecular Psychiatry, 13(3), 285–292.
Whitton, P. S. (2007). Inflammation as a causative factor in the aetiology of Parkinson’s disease. British Journal of Pharmacology, 150(8), 963–976.
Whitworth, A. J., et al. (2008). Rhomboid-7 and HtrA2/Omi act in a common pathway with the Parkinson’s disease factors Pink1 and Parkin. Disease Models & Mechanisms, 1(2–3), 168–174.
Wood-Kaczmar, A., et al. (2008). PINK1 is necessary for long term survival and mitochondrial function in human dopaminergic neurons. PLoS ONE, 3(6), e2455.
Yacoubian, T. A., & Standaert, D. G. (2009). Targets for neuroprotection in Parkinson’s disease. Biochimica et Biophysica Acta, 1792(7), 676–687.
Yan, M. H., Wang, X., & Zhu, X. (2013). Mitochondrial defects and oxidative stress in Alzheimer disease and Parkinson disease. Free Radical Biology & Medicine, 62, 90–101.
Ye, Q., et al. (2013). Astaxanthin suppresses MPP+ -induced oxidative damage in PC12 cells through a Sp1/NR1 signaling pathway. Marine Drugs, 11(4), 1019–1034.
Yin, L., et al. (2010). Terminal differentiation of chronic myelogenous leukemia cells is induced by targeting of the MUC1-C oncoprotein. Cancer Biology & Therapy, 10(5), 483–491.
Yu, H., Pardoll, D., & Jove, R. (2009). STATs in cancer inflammation and immunity: A leading role for STAT3. Nature Reviews Cancer, 9(11), 798–809.
Yun, J., et al. (2008). Loss-of-function analysis suggests that Omi/HtrA2 is not an essential component of the PINK1/PARKIN pathway in vivo. Journal of Neuroscience, 28(53), 14500–14510.
Zecca, L., et al. (2004). The role of iron and copper molecules in the neuronal vulnerability of locus coeruleus and substantia nigra during aging. Proceedings of National Academic Science USA, 101(26), 9843–9848.
Zhang, L., et al. (2011). The Wnt/beta-catenin signaling pathway in the adult neurogenesis. European Journal of Neuroscience, 33(1), 1–8.
Zhang, W., et al. (2013). Human neuromelanin: An endogenous microglial activator for dopaminergic neuron death. Frontiers in Bioscience (Elite Edition), 5, 1–11.
Zhou, C., et al. (2008). The kinase domain of mitochondrial PINK1 faces the cytoplasm. Proceedings of National Academic Science USA, 105(33), 12022–12027.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gaki, G.S., Papavassiliou, A.G. Oxidative Stress-Induced Signaling Pathways Implicated in the Pathogenesis of Parkinson’s Disease. Neuromol Med 16, 217–230 (2014). https://doi.org/10.1007/s12017-014-8294-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12017-014-8294-x