Abstract
Biliary epithelial cells (BECs) provide the first line of defense against lumenal microbes in the biliary system. BECs express a variety of pathogen recognition receptors and can activate several intracellular signaling cascades to initiate antimicrobial defenses, including production of several anti-microbial peptides, cytokines, chemokines, and adhesion molecules. BECs also secrete immunoglobulin A and interact with other cells through expression and release of adhesion molecules and immune mediators. Recently, several reports suggest a correlation between apoptosis and autoimmunity through ineffective clearance of self-antigens. Primary biliary cirrhosis (PBC) is a slowly progressive, autoimmune cholestatic liver disease characterized by highly specific antimitochondrial antibodies (AMAs) and the specific immune-mediated destruction of BECs. We have demonstrated that the AMA self-antigen, namely the E2 subunit of the pyruvate dehydrogenase complex, is detectable in its antigenically reactive form within apoptotic blebs from human intrahepatic biliary epithelial cells and activates innate immune responses. Primary sclerosing cholangitis (PSC) is a chronic cholestatic liver disease characterized by inflammation and the presence of concentric fibrosis of intrahepatic and/or extrahepatic bile ducts, eventually leading to cirrhosis. However, apoptosis does not appear to play a central role in PSC. Despite both diseases involving immune-mediated injury to bile ducts, apoptosis occurs more commonly overall in PBC where it likely plays a unique role.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The biliary system of the liver functions to deliver bile to the intestinal lumen. Biliary epithelial cells (BECs) form a continuous mucosal surface from the smallest biliary unit the bile ductule, through intralobular and septal bile ducts and finally to the large intrahepatic and extrahepatic bile ducts. Due to the exposure of the biliary tract to microbes, BECs are equipped to respond through several immunological pathways including a variety of pathogen pattern recognition receptors [1–3]. Activation of pathogen pattern recognition receptor-associated intracellular signaling cascades result in the expression of several anti-microbial peptide, cytokines/chemokines, adhesion molecules, and immunoglobulin A (IgA), initiating epithelial immune responses against microbial infection. However, a balance between inflammatory responses and tolerance is a key in mucosal environments.
Apoptosis, the major mechanism of programmed cell death, is essential to regulate and maintain tissue growth and homeostasis. Normally, apoptotic bodies are efficiently cleared by neighboring tissue cells or professional phagocytes without inciting an inflammatory reaction [4, 5]. However, several reports suggest a correlation between apoptosis and autoimmunity through an impairment of apoptosis or an ineffective removal of apoptotic bodies [6–8] leading to the release of intracellular components that are a potential source of autoantigenic stimulation [7, 9]. The presence of intact autoantigens within apoptotic bodies [10] and their ability to activate innate immunity through macrophage cytokine secretion [11] provide the strongest evidence linking apoptosis and autoimmunity [12].
Primary biliary cirrhosis (PBC) is an autoimmune liver disease characterized by progressive destruction of intrahepatic bile ducts with cholestasis, portal inflammation, and fibrosis. PBC may lead to cirrhosis and its complications, and eventually to liver transplantation or death. PBC is characterized by multi-lineage T and B cell responses against the E2 subunit of the pyruvate dehydrogenase complex (PDC-E2), which is contained in the mitochondria of all nucleated cells [13, 14]. However, a major unanswered question regarding the pathogenesis of PBC is the specific targeting of small BECs despite the presence of mitochondria in all nucleated cells. We reported that PDC-E2 is preserved in apoptotic bodies from human intrahepatic biliary epithelial cells (HiBECs) but not other epithelial cells during apoptosis [15, 16]. Furthermore, the triad of HiBEC apoptotic bodies, macrophages from patients with PBC, and antimitochondrial antibodies (AMAs) produce inflammatory cytokines and TNF-related apoptosis-inducing ligand (TRAIL) [17]. We have proposed that the unique apoptotic features of BECs allow the exposure of a potent intracellular autoantigen to the PBC-associated multi-lineage autoimmune response that leads to the tissue-specific autoimmune injury. Although genetic susceptibility and environmental factors have gained much recent attention, mounting evidence continues to suggest that BEC apoptosis plays an important role in PBC pathogenesis. Primary sclerosing cholangitis (PSC) is another liver disease likely of autoimmune etiology in which small as well as large bile ducts are destroyed and leads to biliary cirrhosis. However, based upon in situ staining, apoptosis is much more frequent in PBC compared with PSC [18]. This review summarizes the current understanding of the immunophysiology and apoptosis of BECs, as well as how they relate to PBC and PSC.
Basic Mechanism of Biliary Immunity
Toll-Like Receptors
Toll-like receptors (TLRs) are key responders to pathogen-associated molecular patterns (PAMPs) and are characterized by a variable leucine-rich extracellular domain and an intracellular toll/interleukin (IL)-1 receptor domain [19, 20]. The former domain responds to PAMPs, and the latter induces the production of antiviral cytokines and inflammatory cytokines/chemokines via intracellular transcription factors such as nuclear factor (NF)–kB, mitogen-activated protein kinases (MAPK), and interferon-regulatory factor-3 (IRF-3) followed by the initiation of inflammatory responses. Epithelial expression of TLRs is highly regulated, reflecting the specific microenvironment and function of each epithelial cell type. BECs express TLRs 1, 2, 3, 4, and 5, and signaling proteins myeloid differentiation factor 88 (MyD88), IL-1 receptor-associated kinase (IRAK-1), retinoic acid inducible gene-1 (Rig-1), and melanoma differentiation-associated gene 5 [21, 22]. Moreover, immunohistochemistry has confirmed that TLR1-TLR5, MyD88, and IRAK-1 are distributed diffusely in the intrahepatic biliary tree of normal human liver [21]. Upregulation of TLRs in BECs has been demonstrated in patients with PBC, PSC, and hepatolithiasis [23, 24]. In addition, BECs have also demonstrated responsiveness to the corresponding PAMPs. Lipopolysaccharide (LPS), a ligand of TLR4, binds to the surface of cultured BECs and induces the production of TNF-α mRNA in an NF–κB-dependent manner [25]. Stimulation of BEC with polyinosinic–polycytidylic acid (poly I:C), a ligand of TLR9, induces the activation of NF–κB and interferon regulatory factor (IRF3) and the production of interferon β1 (IFN-β1) and MxA as potent antiviral responses [26]. Therefore, BECs possess functional TLR signaling systems and participate in innate immunity.
Epithelial cells have also developed multiple strategies for negative regulation of TLR signaling that initiate events leading to resolution of the inflammatory responses. These strategies include the release of extracellular soluble decoy TLRs, interference of ligand–receptor interaction through transmembrane negative regulators, and activation of intracellular antagonists to downregulate TLR signaling [27]. Moreover, a function for some of these negative regulators has recently been elucidated in human BECs. Upregulation of interleukin-1 receptor-associated kinase M (IRAK-M), a negative regulator of TLRs signaling, was demonstrated in freshly isolated human BECs upon stimulation with TLR 2 and TLR 4 [28]. This study demonstrated endotoxin tolerance in the intrahepatic biliary epithelium and suggests that the expression of IRAK-M is crucial for LPS-induced tolerance in BECs. It is speculated that endotoxin tolerance is important in maintaining innate immune biliary homeostasis and that an impaired tolerance to LPS may be associated with the pathogenesis of biliary diseases.
Anti-microbial Peptide
Defensins and cathelicidin are anti-microbial peptides belonging to the innate immune system [29]. They protect the mucosal barrier against bacteria, mycobacteria, fungi, and viruses via mechanisms such as the disruption of microbial membranes. However, they also participate in adaptive immunity through the recruitment of CD4+ T cells and immature dendritic cells [30]. Granulocytes express the highest density of defensins, however, cholangiocytes also produce these peptides in basal and diseased states [1, 29]. Defensins are divided into two major groups, α-defensins and β-defensins, based on their structure [31]. α-Defensins are particularly abundant in neutrophils and Paneth cells of the small intestine[31]. Of the six human β-defensins (hBD-1 to hBD-6) that have been identified, human β-defensin 1 (hBD-1) is diffusely expressed in the cytoplasm of normal BECs [31]. Moreover, because hBD-1 is constantly detectable in bile samples, hBD-1 is believed to play a role in the constitutive antimicrobial defense of the hepatobiliary system [1]. hBD-2 is undetected in normal BECs. However, hBD2 is induced by bacterial and viral infections and cytokines in the liver. Therefore, hBD-1 plays a constitutive role in biliary antimicrobial defense, while the expression of hBD-2 is induced in response to local infections and may play a role in additional antimicrobial defenses.
Cathelicidin is expressed in normal human BECs, as well as hepatocytes. Moreover, bile acids, including chenodeoxycholic acid and UCDA, enhance cathelicidin expression through the farnesoid X receptor and the vitamin D receptor [32].
Cytokines and Chemokines
HiBECs constitutively express IL-6, IL-8, and monocyte chemotactic protein-1 (MCP-1) [2, 33], which are important chemotactic agents for neutrophils, monocytes, and T cells. Treatment of HiBECs with PAMPs induces the production of IL-6 and MCP-1 via activation of transcription factors NF–kB and MAPK [2]. In addition, LPS induces expression and secretion of IL-12 and TNF-α in immortalized mouse BECs through activation of TLR4 [25]. Fractalkine is a chemokine with both chemoattractant and cell adhesive functions, and it is involved with its receptor CX3C chemokine receptor 1 (CX3CR1) in the chemoattraction and recruitment of intraepithelial lymphocytes. LPS induces the upregulation of fractalkine expression in cultured HiBECs, followed by the chemoattraction of CX3CR1-expressing mononuclear cells [34]. Shimoda et al. [35] demonstrated the significance of fractalkine and the precise mechanism of its production using populations of multiple intrahepatic cell types, including endothelial cells, liver sinusoidal endothelial cells, and BECs, to directly study the interaction of fractalkine producing cells with liver-infiltrating mononuclear cells. Endothelial cells produced large amounts of fractalkine upon stimulation by PAMPs. In contrast, liver sinusoidal endothelial cells produced no fractalkine. Moreover, TLR3-stimulated BECs produced fractalkine after direct contact with TLR4-stimulated autologous monocytes. These findings suggest that cytokines and chemokines secreted by BECs recruit and activate immune cells such as T cells, macrophages, and natural killer cells to protect against biliary infection [36].
Adhesion Molecules
Normal BECs express low levels of lymphocyte adhesion molecules such as intercellular adhesion molecule 1 (ICAM-1) and lymphocyte function-associated antigen 3 (LFA-3). However, previous study reports a lack of specific ICAM-1 immunohistochemical staining in normal livers [37]. ICAM-1 is critical for leukocyte migration to inflammatory sites. It binds to lymphocyte function-associated antigen-1 (LFA-1) and macrophage antigen-1 expressed on leukocytes such as neutrophils, macrophages, and lymphocytes [38]. BECs from patients with PBC exhibit increased expressions of ICAM-1, with a corresponding expression of LFA-1 on infiltrating lymphocytes [37]. The presence of the adhesion molecule LFA-3 on the surface of BECs allows their interaction with CD2 molecules expressed on cytotoxic T lymphocytes and natural killer cells [39]. T cells are also activated by CD40, a member of the TNF receptor superfamily, which is expressed on BECs [40]. The CD40–CD40L and CD2/CD58 complexes induce production of IL-12, which plays an important role in the cytotoxic response of BECs. CD40 and CD40L expression in BECs are increased, respectively, by stimulation with IFN-γ and activation of CD2 on T cells [40]. The increase in leukocyte adhesion molecules facilitates tissue-specific migration by the slowing down of leukocyte circulation near the damaged epithelium, encouraging trafficking to the target site.
Secretory IgA
BECs also transport protective immunoglobulins from the circulation into bile. The predominant immunoglobulin in bile is IgA, although IgM and IgG are present but at much lower levels. IgA could be protective for bile ducts by preventing bacterial infection or inhibiting bacterial toxins from interacting with BECs [41]. IgA is synthesized by plasma cells around bile ducts and secreted into bile after binding to the polymeric Ig receptor located on the basolateral membranes of BECs. Aagaard and colleagues demonstrated that natural IgA antibodies against a variety of intestinal bacteria are present in bile, and after inoculation of various antigens into the intestinal lumen or intestinal lymphoid tissues, a consequent secretion of specific IgA antibodies that protect from biliary tract infections is evident in the bile of experimental animals [42]. Additionally, IgA has been demonstrated to neutralize intracellular microbes and their products during its transit through mucosal epithelium. Immune complexes of IgA and foreign antigen in the lamina propria may also be transported to the lumen via secretory components, excreting pathogens to a proteolytic mucosal environment [43].
Biliary Immunity and Apoptosis
Apoptosis of Biliary Epithelial Cells
The decision of a cell to undergo apoptosis can be influenced by a wide variety of regulatory stimuli acting either as inhibitors or inducers of apoptosis. Apoptosis contributes to duct loss and is induced by signals such as activation of death receptors, immune-mediated injury, oxidative stress, infections, and toxins. Two main pathways of apoptosis regulation have been identified: termed the intrinsic and extrinsic pathways. The intrinsic pathway is characterized by mitochondria dysfunction or possibly by endoplasmic reticulum stress [44]. The extrinsic pathway is mediated either by cell surface receptors, including Fas and TNF-a receptor-1 (TNF-R1), or by perforin and granzyme B released from activated cytotoxic lymphocytes. Upon activation by Fas ligand (FasL) and TNF-a, both Fas, TNF-R1 recruit adaptor proteins, and aggregation of this complex initiates cleavage of procaspase 8 into its active form. TRAIL binds two death receptors (TRAIL-R1/death receptor 4 (DR4) and TRAIL-R2/death receptor 5 (DR5)) and has been demonstrated as a critical molecule in the extrinsic pathways[45, 46]. Cytotoxic lymphocytes express FasL and release granules containing granzyme B and perforin, which allows granzyme B to enter target cells. Granzyme B then directly cleaves critical cellular proteins and activates procaspases [47]. At the earliest stages of apoptosis, the phagocytes and the dying cells have to be in proximity, which is achieved through “find-me” signals; the phagocytes then specifically engage the dying cells, achieved via “eat-me” signals on dying cells and receptors for the “eat-me” signals on phagocytes; the phagocytes then physically engulf the dying cells through signaling induced by engulfment receptors and cytoskeletal reorganization. After internalization, actin is displaced from the phagosome, which matures by a series of fusion and fission events with components of the endocytic pathway [48, 49].
There is controversial evidence concerning the expression of programmed-death (PD) ligands in BECs of biliary diseases. PD molecules are expressed on leukocytes, induce apoptosis in the leukocyte, and may be another method of limiting the immune response [50, 51]. Death receptor 5 (DR5) is constitutively expressed by BECs in normal conditions and is significantly upregulated in BECs of some biliary diseases, which may result in their apoptosis via ligation by TRAIL expressed by activated cytotoxic lymphocytes [46]. Stimulation of BEC with poly I:C induced the activation of NF–κB and IRF-3, followed by the production of antiviral IFN-β1 and also enhanced apoptosis via production of TRAIL [26]. The expression of TRAIL by diseased BECs in PBC and PSC may be an attempt by BECs to control the inflammatory responses in these diseases by targeting DR5-expressing leukocytes [46]. The induction of apoptosis in BECs by leukocytes is also important for the clearance of pathogens and may play a role in the induction of BECs damage in biliary diseases. CD40 binds to the CD40L found on leukocytes such as T cells, B cells, and macrophages. In the case of PBC, infiltrating macrophages and T cells express CD40L, with a more pronounced expression on macrophages [52]. In the same study, cultured cholangiocytes demonstrated constitutive expression of CD40, Fas, and FasL. Ligation of CD40 increased FasL expression and led to a three- to fourfold increase in Fas-dependent apoptosis of cultured BECs, suggesting that the binding of CD40 on BECs by inflammatory leukocytes causes apoptosis and perhaps, the clearance of infectious agents. Thus, apoptosis is an important mechanism in the control of immune responses and may contribute to biliary diseases.
Apoptosis and Autoimmunity
The clearance of apoptotic cells is a highly regulated process, essential to avoid the outflow of intracellular contents and to limit the immunological response against generated antigens. Indeed, the most significant difference between the phagocytosis of pathogens and the uptake of apoptotic cells has traditionally been considered the immune response: A pro-inflammatory reaction is often induced after the phagocytosis of necrotic cells, whereas the secretion of anti-inflammatory cytokines follows the engulfment of apoptotic cells [53–55]. The formation of apoptotic bodies and fragments is essential during apoptosis to limit the escape of intracellular content and to preclude any ensuing immunological responses against intracellular autoantigens with inflammatory reactions [54, 56]. Nevertheless, apoptotic bodies and fragments can, under some circumstances, constitute a major source of immunogens in autoimmune diseases that involve the targeting of ubiquitous autoantigens [57]. Although autoantigens have no common cellular distribution or function that distinguishes them from other molecules, a high percentage of autoantigens are specifically cleaved by caspases [58, 59] and become concentrated in cytoplasmic surface blebs or apoptotic bodies during apoptosis [10, 57]. Apoptotic cells engulfed by antigen-presenting dendritic cells (DC) are suggested to serve as a source of self-antigens for the induction of peripheral self-tolerance in normal conditions [60, 61]. Moreover, apoptotic cells are able to promote maturation of DCs by upregulating costimulatory molecules and inducing proinflammatory cytokine release, while functioning as endogenous adjuvants for the induction of specific T cell responses [62]. Further evidence supporting the presentation of neo-antigens derived from apoptotic cells by DCs has been reported [63–65].
Association with Immunophysiology and Apoptosis in Biliary Disease
Primary Biliary Cirrhosis
PBC is a female-predominant, organ-specific autoimmune disease characterized by destruction of intrahepatic small bile duct BECs [66]. The serological hallmark of PBC is the presence of AMAs directed against PDC-E2 located in the inner membrane of mitochondria [14, 67, 68]. In addition, it has been reported that 23% and 57% patients with PBC also produce autoantibodies against two other 2-oxo acid dehydrogenase enzymes, the E2 subunit of the oxo-glutarate dehydrogenase complex (OGDC-E2) and the E2 subunit of the branched chain 2-oxo acid dehydrogenase complex (BCOADC-E2), respectively[13, 69–71]. Furthermore, patients with PBC who are negative for AMAs do not have autoantibodies against PDC-E2, OGDC-E2, or BCOADC-E2 but often have autoantibodies to nuclear autoantigens [70, 72–75].
Epidemiologic studies have shown that having a first-degree relative with PBC, a history of urinary tract infections, a history of smoking, or use of hormone replacement therapies increased the risk of PBC [76, 77]. More recently, genome-wide case–control association studies in PBC have identified a significant association with interleukin-12A (IL-12A), interleukin-12 receptor, beta2 subunit (IL-12RB2), and signal transducer and activator of transcription 4 (STAT4) polymorphisms [78, 79]. The IL-12A polymorphism is also associated with celiac disease [80] and multiple sclerosis [81], and the STAT4 polymorphism is also found in patients with systemic lupus erythematosus and rheumatoid arthritis [82]. The association of these pleiotropic immune function-related genes in PBC and other autoimmune diseases illustrates that multiple genes are shared between clinically distinct but immune-related diseases, and that the immune-mediated pathogenesis of PBC may be secondary to the breaking of tolerance to the PDC-E2 epitope by environmental factors such as xenobiotics [83].
Immune Response in PBC
CD4+ and CD8+ T cells and innate responses have all been demonstrated in PBC patients and proposed as possible etiologies for the biliary injury of PBC[84]. PDC-E2-specific autoreactive CD4+ and CD8+ T cells have been identified in peripheral blood from patients of PBC. Furthermore, PDC-E2-specific autoreactive CD4+ T cells are 100- to 150-fold higher and CD8+ T cells are ten- to 15-fold higher in the liver compared with peripheral blood in PBC patients [85–89]. Notably, the frequency of CD4+CD45RO+ memory T cells are higher in PBC patients compared with normal controls [37, 38], and T cell clones with PDC-E2 specificity derived from PBC patients were all CD4+CD45RO+ T cell [39]. In addition to the memory CD4+ T cells, memory CD8+ T cells are increased in a mouse model of PBC [40]. Although both CD4+ and CD8+ T cells are present within portal tract infiltrates, there is a growing body of data that suggest a more direct role of cytotoxic CD8+ T cells in the biliary destruction pathway [90–92]. Compared with healthy controls, PBC patients had an increased frequency of CD8+ effector memory T cells (CD8highTEM cells), characterized as CD45ROhighCD57+CD8high T cells and respond specifically to the major histocompatibility class I epitope of PDC-E2. Histologically, CD8+CD57+ T cells accumulate around the portal area supporting their role in the progressive destruction of BECs [93].
Apoptosis in PBC
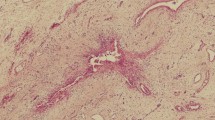
It is clear that mitochondrial proteins are present in all nucleated cells, yet the autoimmune attack is directed with high specificity to BECs. Notably, there are qualitative differences between the metabolic processing of PDC-E2 during apoptosis of BECs compared with other epithelial cells. We confirmed by immunoblotting that seven mitochondrial and four nuclear proteins were present in naive, untreated cultures of HiBECs, human bronchial epithelial cells (BrEPCs), human mammary epithelial cells (MaEPCs), and keratinocytes [16]. Of interest, PDC-E2 was detectable in its antigenically reactive form within apoptotic blebs from HiBECs, but it was not detected in apoptotic blebs from the three other epithelial cell lines [15, 16]. It is reasoned that absence of glutathiolation may contribute to this unique feature of the BEC [94]. Furthermore, we demonstrated that other mitochondrial inner membrane proteins including OGDC-E2, BCOADC-E2, 2,4-dienoyl coenzyme A reductase 1 (DECR1), and ubiquiol cytochrome c reductase complex core protein II (UQCR2) remain intact in apoptotic blebs from HiBECs. In addition to mitochondrial inner membrane enzymes, Sjogren’s syndrome antigen A (SSA/Ro) and glycoprotein 210 kD (gp210), which are nuclear antigens, are detectable in apoptotic blebs from HiBECs (Fig. 1) [16]. Furthermore, we tested the ability of apoptotic blebs from HiBECs to induce cytokine production from mature monocyte-derived macrophage from either patients with PBC or controls in the presence or absence of AMA. We demonstrated that only the unique triad of HiBEC apoptotic blebs, macrophage from PBC patients, and AMA produces inflammatory cytokines and TRAIL [17]. Our observations may help close several remaining gaps in the understanding of PBC including the mechanisms that lead to the selective destruction of small intrahepatic bile ducts. We posit that PDC-E2 in the apoptotic blebs is recognized by circulating AMAs, and the resulting immune complexes stimulate macrophages from subjects with a susceptible genetic background. This event leads to a localized burst of inflammatory cytokines, and the ensuing inflammation is associated with increased apoptosis of surrounding cells, including BECs, and perpetuation of local inflammation with chronic damage to the biliary tract (Fig. 2). Although much work remains to be done in this area, recent findings suggest that BEC apoptosis may be of considerable importance for understanding PBC and that the BEC is more than simply an innocent victim of an immune attack. Rather, it attracts an immune attack by virtue of the unique biochemical mechanisms by which it handles PDC-E2.
Presence of mitochondrial inner membrane enzymes and nuclear antigens in apoptotic bodies of various cell types undergoing apoptosis. Mitochondrial inner membrane enzymes; PDC-E2, OGDC-E2, DECR1, BCOADC-E2, UQCR2, COX-IV, and ATPB. Nuclear antigens; SSA/Ro, SSB/La, Sp100, and gp210. All 11 autoantigens are present in naive, unmanipulated cultures of human primary epithelial cells. PDC-E2, OGDC-E2, and DECR1 are detected in apoptotic bleb from HiBECs only
Schema of pathogenic model in PBC. During the apoptosis of BECs, PDC-E2 remains intact because of its lack of glutathiolation in apoptotic blebs. The PDC-E2 present in the apoptotic blebs would be recognized by circulating AMA, and the immune complex would then stimulate the innate immune system in a subject with a susceptible genetic background
Several studies have investigated apoptosis of BECs specifically in PBC. There is increased DNA fragmentation, implying increased apoptosis, in the BEC of patients with PBC when compared with normal controls [95–97]. Fas, FasL, perforin, granzyme B, and TRAIL expressed significantly greater levels on BECs of patients with PBC [46, 96, 98]. In addition, the upregulation of WAF1 and p53 related to biliary apoptosis is found in BECs of PBC [99]. TdT-mediated deoxyuridine triphosphate nick-end labeling (TUNEL) staining has also shown significantly greater apoptosis of BECs in PBC compared with PSC even when controlled for similar degrees of inflammation [18, 46, 96, 99] (Table 1). These findings suggest that intrinsic pathways induce apoptosis of BECs in PBC and that apoptosis of BECs occurs more commonly in PBC than PSC.
Therapy for PBC
UDCA is well known to be a beneficial agent for the treatment of PBC. Especially in early-stage PBC, a substantial proportion of patients have a favorable outcome with UDCA treatment [100]. Long-term treatment with UDCA in PBC patients improves biochemical liver tests, delays histologic progression, and prolongs survival without liver transplantation [101, 102]. However, the mechanisms of UDCA action have not been fully clarified. It has been postulated that the inherently greater hydrophilic nature of UDCA prevents hepatocytes and BEC damage by replacing more hepatotoxic hydrophobic bile acids [103]. Several studies demonstrated that, both in vivo and in vitro, UDCA can reduce apoptosis in BEC, hepatocytes, and non-liver tissues [95, 97, 104]. UDCA reduces serum levels of both solubilized FasL and TNF-α in patients with PBC. Also, UDCA reduces not only the mitochondrial MPT in isolated mitochondria but also interferes with alternate and upstream molecular targets such as the E2F-1/Mdm-2/p53 pathway [104, 105]. Reduction of apoptosis in BEC may play a role in the therapeutic response to UDCA in PBC.
Primary Sclerosing Cholangitis
PSC is a chronic inflammatory large duct cholangiopathy that induces fibrosis and dilatations of the intrahepatic and extrahepatic bile ducts, leading to the formation of multifocal bile duct strictures [106]. PSC is a male-predominant disease and is strongly associated with inflammatory bowel disease [106, 107]. Additionally, there is an increased risk of cholangiocarcinoma and gallbladder carcinoma. Histological changes show concentric periductal fibrosis (onion skinning) with progression to stricturing of large bile ducts and obliteration of small bile ducts. Although it has been reported that 50% to 80% and 7% to 77% patients with PSC produce autoantibodies against pANCA and ANA, respectively, they have no role in the routine diagnosis of PSC [108].
Immune Response in PSC
CD4+ T cells predominate in the portal infiltrate, and CD8+ T cells predominate in the lobular infiltrate in the liver of patients with PSC [109]. There is a greater percentage of γδ+ T cells in peripheral blood of patients with PSC compared with healthy controls. The infiltrating T cells express the IL-2 receptor and CD45RO, suggesting that they have an activated memory phenotype [110]. Chemokines and their receptors have specific roles in PSC. Hepatic inflammation upregulates mucosal addressin cell adhesion molecule-1 (MAdCAM1) and CCL25, the CCR9 ligand, and increases recruitment of mucosal T cells. CCR9+ liver-infiltrating lymphocytes appear to be specifically increased in PSC compared with PBC. Although the frequency of CCR9+ lymphocytes is not increased in peripheral blood, approximately 20% of lymphocytes from PSC livers express CCR9 compared with <2% in normal livers or PBC [111]. α4β7 and CCR9 expression is functionally relevant because MAdCAM1 and CCL25, which are absent from normal liver, are present on hepatic endothelium in liver diseases associated with colitis and α4β7+CCR9+ lymphocytes from livers of patients with PSC bind MAdCAM1 and respond to CCL25 in adhesion and migration assays [78].
Apoptosis of Biliary Epithelial Cells in PSC
Histologically, TRAIL expression in BECs has been noted to be significantly greater in both PSC and PBC patients compared with healthy controls and patients with biliary stones, although DR5 expression was not significantly different between PSC, PBC, or controls [46]. However, Fas has been shown to be lower in the BEC of PSC when compared with PBC [112]. TUNEL staining score was significantly higher in BECs from PBC than PSC and control group. Furthermore, it was significantly higher in BECs from PBC than PSC in the presence of similar degrees of inflammation [18]. TUNEL staining may identified not only the apoptotic nuclei but also the nuclei in the necrotic tissues; the staining of necrotic cells could be explained either by the activation of an apoptotic pathway in damaged cells or by the degradation of DNA by lysosomal enzymes [113]. Though TUNEL staining may not indicate the exact frequency of apoptotic cells, it is a reliable parameter of comparison between PBC, PSC, and normal control. This difference of apoptosis suggests that BEC apoptosis may be of considerable importance for understanding PBC and suggests different pathogenic mechanisms for bile duct injury in PSC.
Conclusion
Biliary immunity is speculated to be associated with the pathogenesis of biliary diseases as well as the defense against microbial infection. The clearance of apoptotic cells is considered as a multipurpose process that is critical to the maintenance of tolerance. The presence of intact autoantigens within apoptotic bodies and the activation of innate immunity through macrophage cytokine secretion provide a link between apoptosis and autoimmunity. The roles of genetic susceptibility and environmental factors that modify the autoantigen motif and contribute to the breakdown of tolerance may lead to further understanding of the unique immunophysiology of BEC during apoptosis and the pathogenesis of autoimmune biliary diseases.
Abbreviations
- AMAs:
-
Antimitochondrial antibodies
- ANA:
-
Anti-nuclear antibody
- BCOADC-E2:
-
The E2 subunit of the branched chain 2-oxo acid dehydrogenase complex
- BECs:
-
Biliary epithelial cells
- BrEPCs:
-
Human bronchial epithelial cells
- CX3CR1:
-
CX3C chemokine receptor 1
- DC:
-
Dendritic cells
- DECR1:
-
2,4-Dienoyl coenzyme A reductase 1
- DR:
-
Death receptor
- FasL:
-
Fas ligand
- gp210:
-
Glycoprotein 210 kD
- hBD:
-
Human β-defensin
- HiBECs:
-
Human intrahepatic biliary epithelial cells
- ICAM-1:
-
Intercellular adhesion molecule 1
- IFN-β1:
-
Interferon β1
- IgA:
-
Immunoglobulin A
- IL-12A:
-
Interleukin-12A
- IL-12RB2:
-
Interleukin-12 receptor beta2 subunit
- IRAK-1:
-
IL-1 receptor-associated kinase
- IRAK-M:
-
Interleukin-1 receptor-associated kinase M
- IRF-3:
-
Interferon-regulatory factor-3
- LFA-1:
-
Lymphocyte function-associated antigen-1
- LFA-3:
-
Lymphocyte function-associated antigen 3
- LPS:
-
Lipopolysaccharide
- MAdCAM1:
-
Mucosal addressin cell adhesion molecule-1
- MaEPCs:
-
Human mammary epithelial cells
- MAPK:
-
Mitogen-activated protein kinases
- MCP-1:
-
Monocyte chemotactic protein-1
- MDA-5:
-
Melanoma differentiation associated gene 5
- MPT:
-
Mitochondrial membrane permeability transition
- MxA:
-
Myxovirus resistance protein A
- MyD88:
-
Myeloid differentiation factor 88
- (NF)–kB:
-
Nuclear factor
- OGDC-E2:
-
The E2 subunit of the oxo-glutarate dehydrogenase complex
- PAMPs:
-
Pathogen-associated molecular patterns
- pANCA:
-
Perinuclear anti-neutrophil cytoplasmic antibody
- PBC:
-
Primary biliary cirrhosis
- PDC-E2:
-
The E2 subunit of the pyruvate dehydrogenase complex
- poly I:C:
-
Polyinosinic–polycytidylic acid
- PSC:
-
Primary sclerosing cholangitis
- Rig-1:
-
Retinoic acid inducible gene-1
- STAT4:
-
Signal transducer and activator of transcription 4
- SSA/Ro:
-
Sjogren’s syndrome antigen A
- TRAIL:
-
TNF-related apoptosis-inducing ligand
- TLRs:
-
Toll-like receptors
- TNF-R1:
-
TNF-α receptor-1
- TUNEL:
-
TdT-mediated deoxyuridine triphosphate nick-end labeling
- UCDA:
-
Ursodeoxycholic acid
- UQCR2:
-
Ubiquiol cytochrome c reductase complex core protein II
References
Harada K, Ohba K, Ozaki S et al (2004) Peptide antibiotic human beta-defensin-1 and -2 contribute to antimicrobial defense of the intrahepatic biliary tree. Hepatology 40:925–932
Yokoyama T, Komori A, Nakamura M et al (2006) Human intrahepatic biliary epithelial cells function in innate immunity by producing IL-6 and IL-8 via the TLR4-NF-kappaB and -MAPK signaling pathways. Liver Int 26:467–476
Chen XM, O’Hara SP, Nelson JB et al (2005) Multiple TLRs are expressed in human cholangiocytes and mediate host epithelial defense responses to Cryptosporidium parvum via activation of NF-kappaB. J Immunol 175:7447–7456
Savill J, Dransfield I, Gregory C, Haslett C (2002) A blast from the past: clearance of apoptotic cells regulates immune responses. Nat Rev Immunol 2:965–975
Ravichandran KS, Lorenz U (2007) Engulfment of apoptotic cells: signals for a good meal. Nat Rev Immunol 7:964–974
Lleo A, Invernizzi P, Selmi C et al (2007) Autophagy: highlighting a novel player in the autoimmunity scenario. J Autoimmun 29:61–68
Salunga TL, Cui ZG, Shimoda S et al (2007) Oxidative stress-induced apoptosis of bile duct cells in primary biliary cirrhosis. J Autoimmun 29:78–86
Allina J, Hu B, Sullivan DM et al (2006) T cell targeting and phagocytosis of apoptotic biliary epithelial cells in primary biliary cirrhosis. J Autoimmun 27:232–241
Torok NJ (2007) Apoptotic cell death takes its toll. Hepatology 46:1323–1325
Schiller M, Bekeredjian-Ding I, Heyder P, Blank N, Ho AD, Lorenz HM (2008) Autoantigens are translocated into small apoptotic bodies during early stages of apoptosis. Cell Death Differ 15:183–191
Lucas M, Stuart LM, Savill J, Lacy-Hulbert A (2003) Apoptotic cells and innate immune stimuli combine to regulate macrophage cytokine secretion. J Immunol 171:2610–2615
Nagata S, Hanayama R, Kawane K (2010) Autoimmunity and the clearance of dead cells. Cell 140:619–630
Kaplan MM, Gershwin ME (2005) Primary biliary cirrhosis. N Engl J Med 353:1261–1273
Gershwin ME, Mackay IR, Sturgess A, Coppel RL (1987) Identification and specificity of a cDNA encoding the 70 kd mitochondrial antigen recognized in primary biliary cirrhosis. J Immunol 138:3525–3531
Lleo A, Selmi C, Invernizzi P et al (2009) Apotopes and the biliary specificity of primary biliary cirrhosis. Hepatology 49:871–879
Rong G, Zhong R, Lleo A et al (2011) Epithelial cell specificity and apotope recognition by serum autoantibodies in primary biliary cirrhosis. Hepatology 54:196–203
Lleo A, Bowlus CL, Yang GX et al (2010) Biliary apotopes and anti-mitochondrial antibodies activate innate immune responses in primary biliary cirrhosis. Hepatology 52:987–998
Tinmouth J, Lee M, Wanless IR, Tsui FW, Inman R, Heathcote EJ (2002) Apoptosis of biliary epithelial cells in primary biliary cirrhosis and primary sclerosing cholangitis. Liver 22:228–234
Anderson KV (2000) Toll signaling pathways in the innate immune response. Curr Opin Immunol 12:13–19
Kaisho T, Akira S (2002) Toll-like receptors as adjuvant receptors. Biochim Biophys Acta 1589:1–13
Harada K, Isse K, Nakanuma Y (2006) Interferon gamma accelerates NF-kappaB activation of biliary epithelial cells induced by Toll-like receptor and ligand interaction. J Clin Pathol 59:184–190
Takeda K, Kaisho T, Akira S (2003) Toll-like receptors. Annu Rev Immunol 21:335–376
Wang AP, Migita K, Ito M et al (2005) Hepatic expression of toll-like receptor 4 in primary biliary cirrhosis. J Autoimmun 25:85–91
Karrar A, Broome U, Sodergren T et al (2007) Biliary epithelial cell antibodies link adaptive and innate immune responses in primary sclerosing cholangitis. Gastroenterology 132:1504–1514
Harada K, Ohira S, Isse K et al (2003) Lipopolysaccharide activates nuclear factor-kappaB through toll-like receptors and related molecules in cultured biliary epithelial cells. Lab Invest 83:1657–1667
Harada K, Sato Y, Itatsu K et al (2007) Innate immune response to double-stranded RNA in biliary epithelial cells is associated with the pathogenesis of biliary atresia. Hepatology 46:1146–1154
Chen XM, O’Hara SP, LaRusso NF (2008) The immunobiology of cholangiocytes. Immunol Cell Biol 86:497–505
Harada K, Isse K, Sato Y, Ozaki S, Nakanuma Y (2006) Endotoxin tolerance in human intrahepatic biliary epithelial cells is induced by upregulation of IRAK-M. Liver Int 26:935–942
Fellermann K, Stange EF (2001) Defensins—innate immunity at the epithelial frontier. Eur J Gastroenterol Hepatol 13:771–776
Taylor K, Barran PE, Dorin JR (2008) Structure–activity relationships in beta-defensin peptides. Biopolymers 90:1–7
Yang D, Liu ZH, Tewary P, Chen Q, de la Rosa G, Oppenheim JJ (2007) Defensin participation in innate and adaptive immunity. Curr Pharm Des 13:3131–3139
D’Aldebert E, Biyeyeme Bi Mve MJ, Mergey M et al (2009) Bile salts control the antimicrobial peptide cathelicidin through nuclear receptors in the human biliary epithelium. Gastroenterology 136:1435–1443
Morland CM, Fear J, McNab G, Joplin R, Adams DH (1997) Promotion of leukocyte transendothelial cell migration by chemokines derived from human biliary epithelial cells in vitro. Proc Assoc Am Physicians 109:372–382
Isse K, Harada K, Zen Y et al (2005) Fractalkine and CX3CR1 are involved in the recruitment of intraepithelial lymphocytes of intrahepatic bile ducts. Hepatology 41:506–516
Shimoda S, Harada K, Niiro H et al (2010) CX3CL1 (fractalkine): a signpost for biliary inflammation in primary biliary cirrhosis. Hepatology 51:567–575
Selmi C, Mackay IR, Gershwin ME (2007) The immunological milieu of the liver. Semin Liver Dis 27:129–139
Yokomori H, Oda M, Ogi M et al (2005) Expression of adhesion molecules on mature cholangiocytes in canal of Hering and bile ductules in wedge biopsy samples of primary biliary cirrhosis. World J Gastroenterol 11:4382–4389
Yang L, Froio RM, Sciuto TE, Dvorak AM, Alon R, Luscinskas FW (2005) ICAM-1 regulates neutrophil adhesion and transcellular migration of TNF-alpha-activated vascular endothelium under flow. Blood 106:584–592
Leon MP, Bassendine MF, Gibbs P, Thick M, Kirby JA (1997) Immunogenicity of biliary epithelium: study of the adhesive interaction with lymphocytes. Gastroenterology 112:968–977
Cruickshank SM, Southgate J, Selby PJ, Trejdosiewicz LK (1998) Expression and cytokine regulation of immune recognition elements by normal human biliary epithelial and established liver cell lines in vitro. J Hepatol 29:550–558
Adams DH, Afford SC (2002) The role of cholangiocytes in the development of chronic inflammatory liver disease. Front Biosci 7:e276–e285
Aagaard BD, Heyworth MF, Oesterle AL, Jones AL, Way LW (1996) Intestinal immunisation with Escherichia coli protects rats against Escherichia coli induced cholangitis. Gut 39:136–140
Mostov KE (1994) Transepithelial transport of immunoglobulins. Annu Rev Immunol 12:63–84
Nakagawa T, Zhu H, Morishima N et al (2000) Caspase-12 mediates endoplasmic-reticulum-specific apoptosis and cytotoxicity by amyloid-beta. Nature 403:98–103
Ashkenazi A (2002) Targeting death and decoy receptors of the tumour-necrosis factor superfamily. Nat Rev Cancer 2:420–430
Takeda K, Kojima Y, Ikejima K et al (2008) Death receptor 5 mediated-apoptosis contributes to cholestatic liver disease. Proc Natl Acad Sci U S A 105:10895–10900
Bai J, Odin JA (2003) Apoptosis and the liver: relation to autoimmunity and related conditions. Autoimmun Rev 2:36–42
Lleo A, Selmi C, Invernizzi P, Podda M, Gershwin ME (2008) The consequences of apoptosis in autoimmunity. J Autoimmun 31:257–262
Ravichandran KS (2011) Beginnings of a good apoptotic meal: the find-me and eat-me signaling pathways. Immunity 35:445–455
Oikawa T, Takahashi H, Ishikawa T et al (2007) Intrahepatic expression of the co-stimulatory molecules programmed death-1, and its ligands in autoimmune liver disease. Pathol Int 57:485–492
Mataki N, Kikuchi K, Kawai T et al (2007) Expression of PD-1, PD-L1, and PD-L2 in the liver in autoimmune liver diseases. Am J Gastroenterol 102:302–312
Afford SC, Ahmed-Choudhury J, Randhawa S et al (2001) CD40 activation-induced, Fas-dependent apoptosis and NF-kappaB/AP-1 signaling in human intrahepatic biliary epithelial cells. FASEB J 15:2345–2354
Voll RE, Herrmann M, Roth EA, Stach C, Kalden JR, Girkontaite I (1997) Immunosuppressive effects of apoptotic cells. Nature 390:350–351
Huynh ML, Fadok VA, Henson PM (2002) Phosphatidylserine-dependent ingestion of apoptotic cells promotes TGF-beta1 secretion and the resolution of inflammation. J Clin Invest 109:41–50
Fadok VA, Bratton DL, Konowal A, Freed PW, Westcott JY, Henson PM (1998) Macrophages that have ingested apoptotic cells in vitro inhibit proinflammatory cytokine production through autocrine/paracrine mechanisms involving TGF-beta, PGE2, and PAF. J Clin Invest 101:890–898
Henson PM (2005) Dampening inflammation. Nat Immunol 6:1179–1181
Casciola-Rosen LA, Anhalt G, Rosen A (1994) Autoantigens targeted in systemic lupus erythematosus are clustered in two populations of surface structures on apoptotic keratinocytes. J Exp Med 179:1317–1330
Casiano CA, Martin SJ, Green DR, Tan EM (1996) Selective cleavage of nuclear autoantigens during CD95 (Fas/APO-1)-mediated T cell apoptosis. J Exp Med 184:765–770
Casciola-Rosen LA, Anhalt GJ, Rosen A (1995) DNA-dependent protein kinase is one of a subset of autoantigens specifically cleaved early during apoptosis. J Exp Med 182:1625–1634
Huang FP, Platt N, Wykes M et al (2000) A discrete subpopulation of dendritic cells transports apoptotic intestinal epithelial cells to T cell areas of mesenteric lymph nodes. J Exp Med 191:435–444
Sauter B, Albert ML, Francisco L, Larsson M, Somersan S, Bhardwaj N (2000) Consequences of cell death: exposure to necrotic tumor cells, but not primary tissue cells or apoptotic cells, induces the maturation of immunostimulatory dendritic cells. J Exp Med 191:423–434
Johansson U, Walther-Jallow L, Smed-Sorensen A, Spetz AL (2007) Triggering of dendritic cell responses after exposure to activated, but not resting, apoptotic PBMCs. J Immunol 179:1711–1720
Rovere P, Manfredi AA, Vallinoto C et al (1998) Dendritic cells preferentially internalize apoptotic cells opsonized by anti-beta2-glycoprotein I antibodies. J Autoimmun 11:403–411
Frisoni L, McPhie L, Colonna L et al (2005) Nuclear autoantigen translocation and autoantibody opsonization lead to increased dendritic cell phagocytosis and presentation of nuclear antigens: a novel pathogenic pathway for autoimmunity? J Immunol 175:2692–2701
Tzeng TC, Suen JL, Chiang BL (2006) Dendritic cells pulsed with apoptotic cells activate self-reactive T-cells of lupus mice both in vitro and in vivo. Rheumatology (Oxford) 45:1230–1237
Gershwin ME, Mackay IR (2008) The causes of primary biliary cirrhosis: convenient and inconvenient truths. Hepatology 47:737–745
Mao TK, Davis PA, Odin JA, Coppel RL, Gershwin ME (2004) Sidechain biology and the immunogenicity of PDC-E2, the major autoantigen of primary biliary cirrhosis. Hepatology 40:1241–1248
Moteki S, Leung PS, Coppel RL et al (1996) Use of a designer triple expression hybrid clone for three different lipoyl domain for the detection of antimitochondrial autoantibodies. Hepatology 24:97–103
Moteki S, Leung PS, Dickson ER et al (1996) Epitope mapping and reactivity of autoantibodies to the E2 component of 2-oxoglutarate dehydrogenase complex in primary biliary cirrhosis using recombinant 2-oxoglutarate dehydrogenase complex. Hepatology 23:436–444
Miyakawa H, Tanaka A, Kikuchi K et al (2001) Detection of antimitochondrial autoantibodies in immunofluorescent AMA-negative patients with primary biliary cirrhosis using recombinant autoantigens. Hepatology 34:243–248
Oertelt S, Rieger R, Selmi C et al (2007) A sensitive bead assay for antimitochondrial antibodies: chipping away at AMA-negative primary biliary cirrhosis. Hepatology 45:659–665
Muratori P, Muratori L, Ferrari R et al (2003) Characterization and clinical impact of antinuclear antibodies in primary biliary cirrhosis. Am J Gastroenterol 98:431–437
Liu H, Norman GL, Shums Z et al (2010) PBC screen: an IgG/IgA dual isotype ELISA detecting multiple mitochondrial and nuclear autoantibodies specific for primary biliary cirrhosis. J Autoimmun 35:436–442
Agmon-Levin N, Shapira Y, Selmi C et al (2010) A comprehensive evaluation of serum autoantibodies in primary biliary cirrhosis. J Autoimmun 34:55–58
Hu CJ, Zhang FC, Li YZ, Zhang X (2010) Primary biliary cirrhosis: what do autoantibodies tell us? World J Gastroenterol 16:3616–3629
Gershwin ME, Selmi C, Worman HJ et al (2005) Risk factors and comorbidities in primary biliary cirrhosis: a controlled interview-based study of 1032 patients. Hepatology 42:1194–1202
Selmi C, Gershwin ME, Lindor KD et al (2007) Quality of life and everyday activities in patients with primary biliary cirrhosis. Hepatology 46:1836–1843
Hirschfield GM, Liu X, Xu C et al (2009) Primary biliary cirrhosis associated with HLA, IL12A, and IL12RB2 variants. N Engl J Med 360:2544–2555
Liu X, Invernizzi P, Lu Y et al (2010) Genome-wide meta-analyses identify three loci associated with primary biliary cirrhosis. Nat Genet 42:658–660
Hunt KA, Zhernakova A, Turner G et al (2008) Newly identified genetic risk variants for celiac disease related to the immune response. Nat Genet 40:395–402
International Multiple Sclerosis Genetics Consortium (IMSGC) (2010) IL12A, MPHOSPH9/CDK2AP1 and RGS1 are novel multiple sclerosis susceptibility loci. Genes Immun 11:397–405
Remmers EF, Plenge RM, Lee AT et al. (2007) STAT4 and the risk of rheumatoid arthritis and systemic lupus erythematosus. N Engl J Med 357:977–986.
Amano K, Leung PS, Rieger R et al (2005) Chemical xenobiotics and mitochondrial autoantigens in primary biliary cirrhosis: identification of antibodies against a common environmental, cosmetic, and food additive, 2-octynoic acid. J Immunol 174:5874–5883
Lindor KD, Gershwin ME, Poupon R, Kaplan M, Bergasa NV, Heathcote EJ (2009) Primary biliary cirrhosis. Hepatology 50:291–308
Kita H, Lian ZX, Van de Water J et al (2002) Identification of HLA-A2-restricted CD8(+) cytotoxic T cell responses in primary biliary cirrhosis: T cell activation is augmented by immune complexes cross-presented by dendritic cells. J Exp Med 195:113–123
Shimoda S, Nakamura M, Ishibashi H, Hayashida K, Niho Y (1995) HLA DRB4 0101-restricted immunodominant T cell autoepitope of pyruvate dehydrogenase complex in primary biliary cirrhosis: evidence of molecular mimicry in human autoimmune diseases. J Exp Med 181:1835–1845
Van de Water J, Ansari A, Prindiville T et al (1995) Heterogeneity of autoreactive T cell clones specific for the E2 component of the pyruvate dehydrogenase complex in primary biliary cirrhosis. J Exp Med 181:723–733
Kita H, Matsumura S, He XS et al (2002) Quantitative and functional analysis of PDC-E2-specific autoreactive cytotoxic T lymphocytes in primary biliary cirrhosis. J Clin Invest 109:1231–1240
Shimoda S, Van de Water J, Ansari A et al (1998) Identification and precursor frequency analysis of a common T cell epitope motif in mitochondrial autoantigens in primary biliary cirrhosis. J Clin Invest 102:1831–1840
Yang GX, Lian ZX, Chuang YH et al (2008) Adoptive transfer of CD8(+) T cells from transforming growth factor beta receptor type II (dominant negative form) induces autoimmune cholangitis in mice. Hepatology 47:1974–1982
Ueno Y, Ambrosini YM, Moritoki Y, Ridgway WM, Gershwin ME (2010) Murine models of autoimmune cholangitis. Curr Opin Gastroenterol 26:274–279
Wakabayashi K, Lian ZX, Moritoki Y et al (2006) IL-2 receptor alpha(-/-) mice and the development of primary biliary cirrhosis. Hepatology 44:1240–1249
Tsuda M, Ambrosini YM, Zhang W et al (2011) Fine phenotypic and functional characterization of effector cluster of differentiation 8 positive T cells in human patients with primary biliary cirrhosis. Hepatology 54:1293–1302
Odin JA, Huebert RC, Casciola-Rosen L, LaRusso NF, Rosen A (2001) Bcl-2-dependent oxidation of pyruvate dehydrogenase-E2, a primary biliary cirrhosis autoantigen, during apoptosis. J Clin Invest 108:223–232
Koga H, Sakisaka S, Ohishi M, Sata M, Tanikawa K (1997) Nuclear DNA fragmentation and expression of Bcl-2 in primary biliary cirrhosis. Hepatology 25:1077–1084
Harada K, Ozaki S, Gershwin ME, Nakanuma Y (1997) Enhanced apoptosis relates to bile duct loss in primary biliary cirrhosis. Hepatology 26:1399–1405
Sakisaka S, Koga H, Sasatomi K, Mimura Y, Kawaguchi T, Tanikawa K (1997) Biliary secretion of endotoxin and pathogenesis of primary biliary cirrhosis. Yale J Biol Med 70:403–408
Harada K, Kono N, Tsuneyama K, Nakanuma Y (1998) Cell-kinetic study of proliferating bile ductules in various hepatobiliary diseases. Liver 18:277–284
Harada K, Furubo S, Ozaki S, Hiramatsu K, Sudo Y, Nakanuma Y (2001) Increased expression of WAF1 in intrahepatic bile ducts in primary biliary cirrhosis relates to apoptosis. J Hepatol 34:500–506
Poupon RE, Lindor KD, Pares A, Chazouilleres O, Poupon R, Heathcote EJ (2003) Combined analysis of the effect of treatment with ursodeoxycholic acid on histologic progression in primary biliary cirrhosis. J Hepatol 39:12–16
Corpechot C, Carrat F, Bahr A, Chretien Y, Poupon RE, Poupon R (2005) The effect of ursodeoxycholic acid therapy on the natural course of primary biliary cirrhosis. Gastroenterology 128:297–303
Poupon RE, Balkau B, Eschwege E, Poupon R (1991) A multicenter, controlled trial of ursodiol for the treatment of primary biliary cirrhosis. UDCA-PBC Study Group. N Engl J Med 324:1548–1554
Podda M, Ghezzi C, Battezzati PM et al (1989) Effect of different doses of ursodeoxycholic acid in chronic liver disease. Dig Dis Sci 34:59S–65S
Rodrigues CM, Fan G, Ma X, Kren BT, Steer CJ (1998) A novel role for ursodeoxycholic acid in inhibiting apoptosis by modulating mitochondrial membrane perturbation. J Clin Invest 101:2790–2799
Amaral JD, Castro RE, Sola S, Steer CJ, Rodrigues CM (2007) p53 is a key molecular target of ursodeoxycholic acid in regulating apoptosis. J Biol Chem 282:34250–34259
Chapman R, Fevery J, Kalloo A et al (2010) Diagnosis and management of primary sclerosing cholangitis. Hepatology 51:660–678
Fausa O, Schrumpf E, Elgjo K (1991) Relationship of inflammatory bowel disease and primary sclerosing cholangitis. Semin Liver Dis 11:31–39
Hov JR, Boberg KM, Karlsen TH (2008) Autoantibodies in primary sclerosing cholangitis. World J Gastroenterol 14:3781–3791
Aron JH, Bowlus CL (2009) The immunobiology of primary sclerosing cholangitis. Semin Immunopathol 31:383–397
Martins EB, Graham AK, Chapman RW, Fleming KA (1996) Elevation of gamma delta T lymphocytes in peripheral blood and livers of patients with primary sclerosing cholangitis and other autoimmune liver diseases. Hepatology 23:988–993
Eksteen B, Grant AJ, Miles A et al (2004) Hepatic endothelial CCL25 mediates the recruitment of CCR9+ gut-homing lymphocytes to the liver in primary sclerosing cholangitis. J Exp Med 200:1511–1517
Dienes HP, Lohse AW, Gerken G et al (1997) Bile duct epithelia as target cells in primary biliary cirrhosis and primary sclerosing cholangitis. Virchows Arch 431:119–124
Ansari B, Coates PJ, Greenstein BD, Hall PA (1993) In situ end-labelling detects DNA strand breaks in apoptosis and other physiological and pathological states. J Pathol 170:1–8
Kaserer K et al (1998) Characterization of the inflammatory infiltrate autoimmune cholangitis. A morphological and immunhistochemical study. Virchows Arch 432(3):217–222
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kawata, K., Kobayashi, Y., Gershwin, M.E. et al. The Immunophysiology and Apoptosis of Biliary Epithelial Cells: Primary Biliary Cirrhosis and Primary Sclerosing Cholangitis. Clinic Rev Allerg Immunol 43, 230–241 (2012). https://doi.org/10.1007/s12016-012-8324-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12016-012-8324-0