Abstract
Primary sclerosing cholangitis (PSC) is a rare chronic cholestatic disease of the liver and bile ducts that is associated with inflammatory bowel disease, generally leads to end-stage liver disease, and is complicated by malignancies of the biliary tree and the large intestine. The pathogenesis of PSC remains enigmatic, making the development of targeted therapeutic strategies difficult. Immunosuppressive and antifibrotic therapeutic agents were ineffective or accompanied by major side effects. Ursodeoxycholic acid (UDCA) has consistently been shown to improve serum liver tests and might lower the risk of colon carcinoma and cholangiocarcinoma by yet unknown mechanisms. Whether “high dose” UDCA improves the long-term prognosis in PSC as suggested by small pilot trials remains to be demonstrated. The present overview discusses potential therapeutic options aside of targeted immunological therapies and UDCA. The C23 bile acid norUDCA has been shown to markedly improve biochemical and histological features in a mouse model of sclerosing cholangitis without any toxic effects. Studies in humans are eagerly being awaited. Nuclear receptors like the farnesoid-X receptor (FXR), pregnane-X receptor (PXR), vitamin D receptor (VDR), and peroxisome-proliferator-activator receptors (PPARs) have been shown to induce expression of diverse carriers and biotransformation enzymes of the intestinal and hepatic detoxification machinery and/or to modulate fibrogenesis. Pros and cons of respective receptor agonists for the future treatment of PSC are discussed in detail. In our view, the novel bile acid norUDCA and agonists of PPARs, VDR, and PXR appear particularly attractive for further studies in PSC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Primary sclerosing cholangitis (PSC) is a rare chronic cholestatic disorder of the liver and bile ducts that is characterized by fibrosing inflammation of the intra- and/or extrahepatic biliary tree generally leading to progressive bile duct obstruction, fibrosis, cirrhosis and end-stage liver disease [1]. Twice as many men as women are affected. PSC is diagnosed most frequently between ages 25 and 40 years. Criteria for the diagnosis of PSC include (1) a cholestatic serum enzyme pattern, (2) typical cholangiographic findings of bile duct stenoses and dilatations, (3) histologic findings compatible with PSC showing mild to moderate portal inflammation, and (4) exclusion of secondary causes of sclerosing cholangitis. The characteristic histological finding of an onion skin-like fibrosis around bile ductules in PSC is only found in a minority of conventional liver biopsies in patients with PSC as bile ducts with a diameter >100 μm are generally affected by the fibrosing inflammatory process. Secondary changes may rather predominate around smaller ductules. Concomitant inflammatory bowel disease, mainly ulcerative colitis (UC), is found in 70–90% of the patients and atypical perinuclear antineutrophil cytoplasmatic antibodies (pANCA) are detected in more than 70% of patients [1].
The pathogenesis of PSC remains enigmatic, making the development of targeted therapeutic strategies almost impossible [2, 3]. Adams and Ekstein provided the attractive hypothesis that PSC is mediated by long-lived gut-derived mucosal T cells that are normally restricted to the gut and that are recruited to the portal tracts of the liver by aberrantly expressed endothelial cell adhesion molecules (like the gut addressin MADCAM-1) and gut-specific chemokines (like CCL25) in individuals susceptible to PSC [4]. Modulation of tissue-specific lymphocyte homing appears as an attractive therapeutic approach in the future if this hypothesis can be confirmed by further studies. The present article does not address potential future targeted immunological approaches and refers to detailed expert reviews [2, 4].
Primary sclerosing cholangitis, like other chronic cholestatic liver diseases, is characterized by hepatic retention of potentially toxic substances normally excreted into bile, in particular hydrophobic bile acids, as a consequence of impaired hepatobiliary secretion and/or obstruction of bile flow [5, 6]. Elevated levels of bile acids in the hepatocyte [7] then can lead to cellular injury by hepatocyte apoptosis and necrosis and eventually to liver failure and the need for liver transplantation [8]. Therefore, bile acid homeostasis is tightly controlled. The proteins responsible for synthesis, metabolism, conjugation, and transport of bile acids are regulated in a coordinated fashion by nuclear hormone receptors including the farnesoid X receptor (FXR; NR1H4), the pregnane X receptor (PXR; NR1I2), the constitutive androgen receptor (CAR; NR1I3), the vitamin D receptor (VDR), and the peroxisome-proliferator-activator receptor γ (PPAR γ; NR1C1) [9, 10]. As the intrinsic adaptive responses to cholestasis tend to reduce hepatic concentration of bile acids but usually are not sufficient, pharmacological agents, which augment the adaptive responses may be beneficial. The nuclear receptors therefore have been proposed as potential targets for pharmacological treatment of cholestasis [6, 10–12].
Patients with PSC have an increased risk of developing carcinomas of the biliary tree (in the largest cohort studied (n = 604): 161-fold in comparison to a matched healthy Swedish population), pancreas (14-fold), and colon (10-fold) [13]. Both, genetic [14, 15] and environmental factors are discussed to contribute to carcinogenesis in this patient group. Among the tumors observed in PSC, colon carcinoma is by far the most frequent in the general population (5–6% lifetime risk) and also determines the prognosis of a considerable rate of patients with PSC and associated UC. Colorectal dysplasia/carcinoma has been reported to develop in up to 50% of PSC/UC patients during a 25-year follow-up [16] and has been shown to be a major cause of death in PSC patients after liver transplantation [17–19]. Seventy to ninety percent of patients with PSC suffer from inflammatory bowel disease, mainly UC, which itself is a risk factor for development of colorectal neoplasia. However, the presence of UC does not alone explain the increased risk of colon carcinoma in patients with PSC as patients with PSC and UC have a significantly higher risk to develop colon dysplasia/carcinoma when compared to patients with UC only (meta-analysis: odds ratio >4) [20]. In addition, the right colon is often affected in patients with PSC and UC, a finding less commonly described in UC only [21]. Rectal sparing and backwash ileitis are more frequent in patients with PSC and UC than in those with UC only leading to the assumption that UC in PSC might be a unique form of IBD [22]. A pathophysiological explanation for the increased risk of PSC patients to develop colonic dysplasia/malignancy has not yet been provided. Annual total colonoscopy with routine biopsies, however, is recommended in this group of patients for early detection of severe dysplasia and carcinoma.
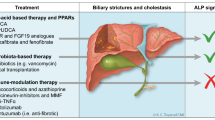
Previous therapeutic approaches
Numerous drugs have been evaluated for the treatment of PSC in randomized, controlled trials (e.g., colchicine, cyclosporine, methotrexate, d-penicillamine) and in pilot studies (e.g., budesonide, cladribin, etanercept, mycofenolate mofetil (MMF), nicotine, pentoxifylline, pirfenidone, prednisone, tacrolimus) and were mostly regarded as ineffective or were accompanied by major side effects during long-term treatment. None of these drugs is today recommended for monotherapy in PSC [1, 23].
Current therapeutic approaches
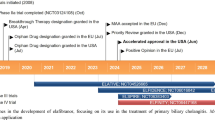
Ursodeoxycholic acid (UDCA) monotherapy is the only therapy in PSC for which improvement in serum liver tests has consistently been observed in placebo-controlled studies [24–29]. At doses of ≥ 20 mg/kg/d of UDCA, surrogate markers of prognosis like the Mayo risk score have been shown to be improved in small cohorts of patients, suggesting that “high dose UDCA” may represent an efficient treatment of PSC [29, 30]. However, a clear-cut survival benefit with UDCA treatment has not been shown in PSC, and no single study published so far fulfills the criteria of adequate sample size, adequate duration of follow-up, and/or adequate dose of UDCA treatment to be able to prove or disprove a survival benefit of UDCA in PSC. The largest trial from Scandinavia analyzed data from 198 patients being treated over 5 years with daily doses of 17–23 mg/kg. Unfortunately, this trial was underpowered (power analysis a priori: n = 346), and the biochemical response of patients was unexpectedly poor when compared to smaller randomized, controlled trials using comparable doses of UDCA [24, 26, 27, 29]. Data from a large randomized, long-term trial on “high-dose UDCA” in PSC supported by the NIH have to be awaited before a firmer conclusion on the efficacy of high-dose UDCA in PSC can be drawn.
On an interesting note, recent data suggest that UDCA treatment lowers the relative risk for PSC patients to develop hepatobiliary [31] and colonic dysplasia/carcinoma [32, 33] by yet unresolved mechanisms. Thus, UDCA treatment is considered as a treatment option in PSC by many experts, although adequate prospective, randomized, controlled studies on long-term outcome are still lacking.
The mechanisms and sites of action of UDCA in PSC and in cholestatic liver diseases in general are only in part resolved and await further elucidation [34]. Stimulation of impaired hepatocellular (and cholangiocellular) secretion, detoxification of bile, and antiapoptotic effects both in hepatocytes and cholangiocytes are considered to contribute to its beneficial, mainly posttranscriptional effects in various cholestatic disorders [9, 12, 34–36].
Future therapeutic approaches
Novel bile acids and (other) nuclear receptor agonists?
Nuclear receptor agonists have recently been considered as potential partners for combination therapy with UDCA in cholestatic liver diseases. Nuclear receptors, like the pregnane X receptor (PXR; in humans also called steroid and xenobiotic receptor, SXR), the vitamin D receptor (VDR), the farnesoid-X receptor (FXR), the constitutive androstane receptor (CAR), and the peroxisome proliferator-activated receptors (PPARs) control the expression of numerous genes in liver and intestine involved in uptake (“phase 0” of biotransformation), biotransformation/detoxification (phase 1, 2) and secretion (phase 3) of exogenous and endogenous agents. Some of these nuclear receptors (FXR, PXR, VDR) are activated, among others, by hydrophobic bile acids (e.g., chenodeoxycholic acid, lithocholic acid), whereas CAR is activated by bilirubin [12]. Among exogenous ligands of these receptors, rifampicin and certain corticosteroids (PXR), phenobarbital (CAR, PXR), fibrates (PPARα/γ), and vitamin D (VDR) are in regular clinical use for various indications, whereas others, like 6-ethyl-CDCA (FXR), await further clinical evaluation.
In PSC, PXR gene variants associated with a reduced PXR function had an increased risk of death or liver transplantation and a shorter median cumulative survival [37]. PXR −/− mice show more extensive liver damage after bile duct obstruction than their wild-type littermates [11]. These observations suggest that functional PXR is of critical importance under cholestatic conditions in man and mouse.
Impaired small intestinal detoxification capacity as cofactor of carcinogenesis in PSC?
The apical sodium bile acid transporter (ASBT, synonymous: IBAT) mediates uptake of bile acids from the intestinal lumen into the mucosa cells and is expressed not only in human ileocytes, but also at considerable levels in human duodenal mucosa [38]. Thus, bile acids may enter not only ileocytes, but also duodenal and jejunal cells at considerable amounts, and may activate nuclear receptors like FXR, PXR, and VDR, which stimulate induction of the small intestinal detoxification machinery. Induction of the intestinal detoxification machinery may, therefore, represent a so far unrecognized function of bile acids in the small intestine.
In cholestasis, a relative deficit of hydrophobic bile acids and bilirubin in the intestinal lumen together with downregulation of the ASBT in the upper intestine [38] may lead to impaired stimulation of expression of key detoxification enzymes and related transporters in the small intestine. As a consequence, colon mucosa cells as well as hepatocytes and cholangiocytes may be exposed to higher levels of potential exogenous co-carcinogens in cholestasis than under physiological conditions.
Ursodeoxycholic acid (UDCA) exerts anticholestatic effects and improves biliary secretion of bile acids and bilirubin glucuronides in PSC [39]. In man, UDCA is dehydroxylated to the potent PXR- and VDR-agonist lithocholic acid (LCA) by intestinal bacteria mainly in the colon [34]. Recent data indicate that UDCA markedly lowers the relative risk for PSC patients to develop colonic dysplasia and colon carcinoma [32, 33] by yet unresolved mechanisms.
We assume that cholestasis in patients with PSC and concomitant UC causes a relative deficit of hydrophobic bile acids and bilirubin glucuronides in the small and large intestinal lumen, which might lead to impaired expression of the PXR-, VDR-, FXR-, and CAR-triggered intestinal detoxification machinery and, thereby, impaired detoxification of putative carcinogens. Exposure of the right and left chronically inflamed (first hit) colon in UC to an enhanced load of putative carcinogens from the small intestine (second hit) may predispose patients with PSC to the development of colonic dysplasia and carcinoma more than patients with UC only (only first hit) [20] or patients with other cholestatic liver diseases without underlying colon inflammation (only second hit) [40].
“High-dose” UDCA and nuclear receptor agonists: activators of an impaired intestinal and hepatic detoxification capacity in PSC?
Ursodeoxycholic acid might upregulate intestinal expression of proteins involved in biotransformation phases 0, 1, 2, and 3 in patients with PSC and, thereby, reduce colon dysplasia/carcinoma risk by (a) reducing cholestasis and stimulating biliary secretion and intestinal content of endogenous bile acids and bilirubin and/or (b) inducing formation of the UDCA metabolite lithocholic acid (LCA), which is a potent PXR- and VDR-agonist.
The medical treatment of patients with PSC (and associated inflammatory bowel disease, mainly UC) should aim at both, effects on the liver and the intestinal tract to reverse (1) the cholestatic hepatobiliary disorder and its sequelae, and (2) the associated increased risk for malignant hepatobiliary and intestinal tumors. High-dose UDCA may become the first promising treatment strategy in PSC for the above-mentioned effects both on the hepatobiliary tract and the intestine. Derivatives of UDCA like its C23 analog, norUDCA, may even be more effective than UDCA as demonstrated in an experimental animal model of cholestasis [41], but studies in patients with cholestatic diseases like PSC are lacking so far.
Nuclear receptor agonists might complement the action of UDCA in the treatment of PSC by enhancing its anticholestatic effect at the site of the liver and by stimulating the small intestinal and hepatic detoxification machinery of biotransformation reactions phase 0 to 3. Therefore, various strategies including UDCA derivatives and agonists of the nuclear receptors FXR, PXR, VDR, and PPAR are discussed below for potential future medical therapy of patients with PSC.
UDCA derivatives
24-norUrsodeoxycholic acid (norUDCA) is the C23 homologue of the 3α,7β-dihydroxy C24 bile acid UDCA. In contrast to UDCA, norUDCA is barely amidated in liver cells and is mainly excreted into bile in its unconjugated and glucuronidated form. NorUDCA induces a bicarbonate-rich hypercholeresis mostly because of cholehepatic shunting of the unconjugated form [42]. In a mouse model of a sclerosing cholangitis-like bile duct inflammation, the mdr2 −/− mouse, norUDCA was more effective than UDCA in improving serum liver tests and markers of inflammation and fibrosis, and inducing bile acid-detoxifying enzymes and transporters [41]. The molecular mechanisms of action of norUDCA are under study at present. Pharmacokinetics of this bile acid was studied in humans in the past, and norUDCA was well tolerated [42]. In the near future, norUDCA awaits further evaluation in healthy individuals and in patients with cholestatic liver disease, in particular PSC.
Thus, norUDCA is a promising agent for evaluation for treatment of PSC.
FXR agonists
The nuclear hormone receptor farnesoid X receptor (FXR; NR1H4) is a bile acid-activated transcription factor that plays a critical role in bile acid homeostasis [43–45]. The hydrophobic bile acid chenodeoxycholic acid (CDCA) is the most potent natural activator of FXR, followed by deoxycholic acid (DCA) and lithocholic acid (LCA), whereas the hydrophilic bile acid, UDCA, appears to be only a weak agonist in man [44]. In the liver, activation of FXR reduces uptake of bile acids and other cholephiles via repression of Na+-taurocholate-cotransporting polypeptide (NTCP, SLC10A1) [46] and organic anion transporting protein (OATP1B1, SLCO1B1) [47] and downregulates bile acid synthesis via repression of the cytochrome P-450 enzymes CYP7A1 and CYP8B1 by an indirect mechanism involving nuclear receptor small heterodimer partner (SHP) [48]. On the other hand, FXR activates the canalicular secretion of bile acids and other constituents of bile via upregulation of the bile salt export pump (BSEP, ABCB11), the multidrug resistance-associated protein 2 (MRP2, ABCC2), the MDR3 P-glycoprotein (ABCB4), and the heteromeric organic solute transporter OSTα/OSTβ [12]. FXR also stimulates the metabolism of hydrophobic bile acids and other toxic compounds to more hydrophilic and less toxic metabolites via upregulation of CYP3A4, which is involved in phase I hydroxylation reactions, and the uridine diphosphate glucuronosyl transferases UGT2B4 and UGT2B7, which form more water-soluble glucuronides [49, 50]. In the small intestine, FXR negatively regulates the apical sodium-dependent bile salt transporter (ASBT, SCL10A2) and stimulates expression of the ileal bile acid-binding protein (I-BAPB) and the basolateral efflux bile salt transporter OSTα/OSTβ [51–54]. Thus, FXR functions as a bile acid sensor and reduces their body load by decreasing their biosynthesis, and increasing their metabolism and hepatic and intestinal elimination. Based on these observations, FXR ligands may offer a rational treatment option for cholestatic liver diseases such as PSC.
The potential beneficial effects of the potent and selective FXR agonist 6α-ethyl-chenodeoxycholic acid (6-ECDCA), a semisynthetic bile acid derivative of CDCA, have been studied in in vivo rat models of cholestasis induced by lithocholic acid (LCA) or 17α-ethynylestradiol (E217α). 6-ECDCA prevented bile flow impairment induced by both LCA and E217α and protected hepatocytes against acute necrosis caused by LCA [55, 56]. In vivo administration of 6-ECDCA led to enhanced expression of Shp, bsep, multidrug resistance-associated protein-2, and multidrug resistance protein-2, whereas it repressed cyp7a1, cyp8b1, and ntcp mRNA expression. These results were reproduced by another synthetic FXR ligand, the isoxazole GW4064 [56]. In primary cultures of human and rat hepatocytes, GW4064 treatment increased SHP expression and decreased CYP7A1 expression [57]. In bile duct ligation and α-naphthylisothiocyanate models of cholestasis, GW4064 treatment reduced markers of liver damage, inflammation, and bile duct proliferation and was associated with decreased expression of biosynthetic genes and increased expression of genes involved in bile acid transport [58]. Stimulation of the adaptive response to cholestasis by FXR agonists is likely to be beneficial in canalicular cholestasis, where secretory failure of the hepatocytes is the cause or in early partial/incomplete obstruction. In addition, an antifibrotic effect of FXR agonists has also been described [59].
However, upregulation of canalicular transporters by FXR ligands might be deleterious in advanced/complete obstruction. In support of this hypothesis, deletion of FXR in FXR knockout mice has been shown to reduce serum bile acids, biliary pressure, bile ductular proliferation, bile infarcts, and mortality in response to bile duct ligation, suggesting a benefit of FXR inhibition in obstructive cholestasis [60, 61]. Probable mechanisms for this protective effect include the downregulation of canalicular transporters, reducing biliary hydrostatic pressure, and the induction of basolateral Mrp4, facilitating “retrograde” secretion of bile acids and other potentially toxic cholephils into the systemic circulation for excretion by the kidney. Accordingly, FXR antagonists have also been proposed for the treatment of obstructive cholestasis [61]. A unifying concept has not yet evolved, and species differences make extrapolation to man difficult.
Thus, FXR agonists may not be, at present, the first candidate for evaluation for long-term treatment of PSC.
PXR agonists
The pregnane X receptor (PXR; NR1I2) (32), another ligand-activated member of the nuclear receptor superfamily, also has a crucial role in regulating the expression of many genes involved in detoxification and metabolism of bile acids [45, 62], including CYP3A4 and CYP7A1 [63, 64], SULT2A1 [65], UGT1A3 and UGT1A4 [66], MDR1 [67], MRP2 [68], and MRP3 [69]. Cholestatic PXR knockout mice exhibited more hepatic damage than wild-type mice both after bile duct ligation and cholic acid feeding, possibly because of impaired detoxification mechanisms and transport pathways [11, 61]. Activation of PXR may, therefore, be beneficial in cholestatic conditions. In line with this concept is the observation that the potent PXR ligand 5-pregnen-3β-ol-20-one-16α-carbonitrile (PCN) dramatically reduced (litho-)cholic acid-induced liver injury in wild-type mice, but not in PXR knockout mice [64, 70]. Hepatoprotection by PCN was associated with significant upregulation of the basolateral bile acid efflux transporter MRP3, emphasizing the importance of alternative excretory routes for toxic bile acids as a protective mechanism contributing to bile acid homeostasis in cholestasis [70].
Human PXR agonists include lithocholic acid, rifampicin, statins, dexamethasone and other corticosteroids, phenobarbital, and St. John wort [12], The antibiotic rifampicin is a potent human PXR activator that is also being used to treat pruritus in cholestatic patients. Rifampicin has been reported to improve serum liver tests in PBC [71, 72]. In patients with otherwise healthy gallstones, who are undergoing cholecystectomy, rifampicin-induced upregulation of UGT1A1 and MRP2 facilitating bilirubin elimination and increased CYP3A4 expression facilitating detoxification of bile acids [73]. Consistent with this, Dilger et al. showed that in patients with early-stage PBC and healthy controls, rifampicin markedly induced CYP3A metabolism as assessed by pharmacokinetic profiling of budesonide and its phase 1 metabolites in plasma and urine and urinary 6β-hydroxy cortisol [74]. The therapeutic bile acid UDCA had no relevant effect on CYP3A metabolic activity [73, 74], but increased expression of the hepatocyte transporters BSEP, MDR3, and MRP4 by posttranscriptional mechanisms [73]. These complementary effects on transcriptional regulation of hepatobiliary enzymes and transporters suggest that the combined use of both agents might have synergistic beneficial effects in patients with non-obstructive cholestasis. Rifampicin was reported to be safe in cholestatic liver disease during short-term use for up to 2 weeks [75]. However, after use for more than 4 weeks, severe hepatotoxicity has been reported in up to 13% of patients with cholestatic disorders [72]. Thus, use of rifampicin for treatment of a chronic cholestatic liver disease like PSC, although conceptually attractive, may be limited by its rate of hepatotoxicity during long-term administration in cholestatic disorders.
Combined treatment with UDCA and the PXR agonist atorvastatin at doses up to 40 mg daily [76] did not beneficially affect serum liver tests but worsened serum alkaline phosphatase activity when compared to UDCA alone [77] in patients with early stage primary biliary cirrhosis who incompletely responded to UDCA monotherapy. This yet unexplained finding makes statins less attractive for future therapeutic evaluations in cholestatic disorders.
The corticosteroid dexamethasone is a potent PXR and glucocorticoid receptor (GR) agonist, but is not a treatment option for patients with PSC: the high rate of systemic side effects including induction of osteoporosis during long-term treatment prohibits use of dexamethasone in PSC. In addition, GR agonists have not been shown to be effective in most patients with PSC [1, 23]. Still, the effect of GR agonists may need to be better defined for subgroups particularly at young age and early stages of disease [78].
Budesonide is a potent corticosteroid with a high first-pass effect of about 90%. Budesonide is a PXR- [79] and GR-agonist, which might—in addition to its well-known anti-inflammatory action in the intestine [80] and the liver [74, 81–84]—lead to induction of expression of key detoxification enzymes and transporters in the small intestine and the liver [79, 85]. It might, thereby, at doses high enough to be an effective anti-inflammatory and inducing agent, but lower than those known to induce bone loss in cholestatic patients with early stage disease [82, 83] be an effective combination partner of UDCA. Short-term treatment of PSC with budesonide and UDCA over a period of 8 weeks did not reveal a significant additional beneficial effect of budesonide on serum liver tests compared to UDCA only [86]. Treatment for 1 year revealed an improvement of serum liver tests (alkaline phosphatase, AST) and of inflammatory activity around the bile ducts, but an increase of serum bilirubin in a heterogeneous group of PSC patients [87], Thus, the PXR/GR agonist budesonide may deserve reevaluation at moderate doses in a well-defined subgroup of patients with early-stage PSC and accompanying UC.
VDR agonists
The Vitamin D receptor (VDR, NR 1I1), a type 1 nuclear receptor, is commonly found in the intestine, bone, and kidney of mammals. In response to its natural ligand 1,25-dihydroxyvitamin D3 (1,25(OH)2D3), VDR forms a complex with its heterodimer partner Retinoid X Receptor (RXR) and activates VDR response elements (VDREs) present in the regulatory region of target genes. Apart from the classical involvement of VDR in the regulation of genes required for calcium homeostasis and bone mineralization, VDR is also able to self-regulate its own transcription via a complex feedback mechanism involving the cytochrome P450 (CYP) genes. The CYP27B1 enzyme converts 25-hydroxyvitamin D (25(OH)D3) into 1,25(OH)2D3 via hydroxylation of carbon chains. Activation of VDR by 1,25(OH)2D3, leads to the repression of CYP27B1 expression and thus a reduction in the VDR [88]. The VDR further activates CYP24A1, an enzyme whose role it is to inactivate 1,25(OH)2D3, thereby resulting in a further reduction in VDR expression [89, 90].
Recent in silico data has shown VDR to regulate over 27,000 genes in humans [91]. A growing number of genes involved in bile formation, drug transport, and drug metabolizing enzymes have been associated with regulation by VDR. The apical sodium-dependent bile acid transporter (ASBT) is responsible for bile acid absorption in the distal ileum [92, 93]. In the presence of 1,25(OH)2D3, VDR was shown to activate rat ASBT leading to increased transport of taurocholate through the ileum [94].
The multidrug resistance-associated protein 3 (MRP3) mediates the basolateral efflux of organic anions and xenobiotic compounds in liver and intestine. Functional studies revealed VDR regulation of Mrp3 in the colon of mice exposed to vitamin D3 in addition to the secondary bile acid, LCA [95]. LCA, at high concentrations, is associated with colon cancer [96]. Several mechanisms exist to detoxify LCA including its sulfation via the sulfotransferase enzyme SULT2A [97]. On an interesting note, increased activation of Mrp3 is associated with increased expression of Sult2a in mice, suggesting a key role for VDR in LCA detoxification [95]. This is further supported by the VDR-mediated regulation of CYP3A genes [98]. CYP3A enzymes are involved in the catabolism of LCA in the intestine and liver. CYP3A4 and CYP3A11 are induced by VDR in the presence of LCA [98]. Indeed, competitive binding assays revealed LCA to be a direct ligand of VDR and in fact a more potent ligand for VDR than for the nuclear receptors FXR and PXR [98].
A second bile acid and drug sulfating enzyme, SULT2A1, is also regulated by VDR [99]. Most abundantly expressed in the intestine and liver, in vitro studies revealed a VDR-mediated activation of SULT2A1 in the presence of 1,25(OH)2D3 [99]. Whereas this study was carried out using the human hepatic cell line HepG2, several studies have shown VDR expression to be extremely low in human liver [100]. Thus, whereas intestinal SULT2A1 activation by the VDR is plausible, the induction of SULT2A1 in the liver remains controversial.
Taken together, VDR may represent a promising therapeutic target in early-stage PSC considering potential improvement of mainly intestinal detoxification capacity by administration of VDR agonists.
PPAR agonists
Peroxisome proliferator-activated receptors (PPARs) are transcription factors that are activated by various ligands, heterodimerize with retinoid X receptors, and bind to peroxisome proliferator response elements in the promoter regions of their respective target genes. Three PPAR genotypes (α, β, γ/δ) have been described and all of them are expressed in the vasculature and inflammatory cells [101].
PPARα is also expressed in the liver and has been implicated in the beta oxidation of fatty acids and in lipid metabolism. PPARα is activated by natural ligands such as fatty acids and fibrates, a class of drugs that are commonly used to lower lipids [102]. On an interesting note, bezafibrate has been shown to have additional beneficial effects on cholestatic liver enzymes (aP, γ-GT) in patients with primary biliary cirrhosis (PBC) already receiving UDCA monotherapy, although these trials are rather small [103–105]. How can these clinical observations be explained?
PPARα agonists decrease IL-1-induced CRP expression in primary human hepatocytes and induction of plasma CRP levels by IL-1 in human CRP-expressing transgenic mice [106, 107]. In these human CRP transgenic mice, PPARα activation also reduced basal plasma CRP levels even in the absence of an inflammatory stimulus. Thus, fibrates might attenuate the inflammation of bile ducts via PPARα activation in PBC as its major mechanism of action. As PSC is characterized by chronic inflammation of the small and large bile ducts, which ultimately causes the typical bile duct strictures leading to cirrhosis, fibrates or novel PPARα agonists might be an attractive treatment option in addition to UDCA also, or even more so for PSC patients.
Fenofibrate has recently been shown to suppress tumor growth by inhibition of angiogenesis, which makes this drug even more interesting as a potential treatment option in PSC, as PSC is associated with a greatly increased tumor risk as outlined earlier [108]. Moreover, PPARα activates transcription of the human ASBT (SLC10A2) gene [109].
PPARγ is important in the regulation of glucose metabolism and cell growth processes and is known to inhibit the production of proinflammatory cytokines [110]. Pharmacologically, PPARγ is targeted by thiazolidinediones, which are used in the treatment of diabetes mellitus. Pioglitazone has also been shown to improve metabolic parameters and histology in patients with non-alcoholic steatohepatitis [111]. On an interesting note, PPARγ protein is ubiquitously expressed in intrahepatic biliary epithelium of PBC patients, but is reduced in damaged bile ducts [112]. Thus, PPARγ might be important to maintain homeostasis in the intrahepatic biliary epithelium.
Fickert et al. recently hypothesized that PSC might represent the “arteriosclerosis of the bile duct” initiated by toxic biliary lipids and demonstrated puzzling similarities of molecular pathomechanisms involved in these vascular and biliary entities [113]. As outlined in this provocative hypothesis paper, exposure to abnormal luminal lipid composition, ultimately resulting in lipid oxidation, might be critically involved in both conditions.
Taken together, these concepts could stimulate research on the role of PPAR agonists in the treatment of PSC.
References
LaRusso NF, Shneider BL, Black D et al (2006) Primary sclerosing cholangitis: summary of a workshop. Hepatology 44(3):746–764
O’Mahony CA, Vierling JM (2006) Etiopathogenesis of primary sclerosing cholangitis. Semin Liver Dis 26(1):3–21
Worthington J, Cullen S, Chapman R (2005) Immunopathogenesis of primary sclerosing cholangitis. Clin Rev Allergy Immunol 28(2):93–103
Adams DH, Eksteen B (2006) Aberrant homing of mucosal T cells and extra-intestinal manifestations of inflammatory bowel disease. Nat Rev Immunol 6(3):244–251
Trauner M, Meier PJ, Boyer JL (1998) Molecular pathogenesis of cholestasis. N Engl J Med 339(17):1217–1227
Paumgartner G (2006) Medical treatment of cholestatic liver diseases: from pathobiology to pharmacological targets. World J Gastroenterol 12(28):4445–4451
Fischer S, Beuers U, Spengler U, Zwiebel FM, Koebe HG (1996) Hepatic levels of bile acids in end-stage chronic cholestatic liver disease. Clin Chim Acta 251(2):173–186
Beuers U, Boyer JL, Paumgartner G (1998) Ursodeoxycholic acid in cholestasis: potential mechanisms of action and therapeutic applications. Hepatology 28(6):1449–1453
Trauner M, Boyer JL (2003) Bile salt transporters: molecular characterization, function, and regulation. Physiol Rev 83(2):633–671
Boyer JL (2007) New perspectives for the treatment of cholestasis: lessons from basic science applied clinically. J Hepatol 46(3):365–371
Stedman CA, Liddle C, Coulter SA et al (2005) Nuclear receptors constitutive androstane receptor and pregnane X receptor ameliorate cholestatic liver injury. Proc Natl Acad Sci U S A 102(6):2063–2068
Zollner G, Marschall HU, Wagner M, Trauner M (2006) Role of nuclear receptors in the adaptive response to bile acids and cholestasis: pathogenetic and therapeutic considerations. Mol Pharm 3(3):231–251
Bergquist A, Ekbom A, Olsson R et al (2002) Hepatic and extrahepatic malignancies in primary sclerosing cholangitis. J Hepatol 36(3):321–327
Melum E, Karlsen TH, Schrumpf E et al (2008) Cholangiocarcinoma in primary sclerosing cholangitis is associated with NKG2D polymorphisms. Hepatology 47(1):90–96
Karlsen TH, Schrumpf E, Boberg KM (2007) Genetic epidemiology of primary sclerosing cholangitis. World J Gastroenterol 13(41):5421–5431
Broome U, Lofberg R, Veress B, Eriksson LS (1995) Primary sclerosing cholangitis and ulcerative colitis: evidence for increased neoplastic potential. Hepatology 22(5):1404–1408
Vera A, Gunson BK, Ussatoff V et al (2003) Colorectal cancer in patients with inflammatory bowel disease after liver transplantation for primary sclerosing cholangitis. Transplantation 75(12):1983–1988
Loftus EV Jr, Aguilar HI, Sandborn WJ et al (1998) Risk of colorectal neoplasia in patients with primary sclerosing cholangitis and ulcerative colitis following orthotopic liver transplantation. Hepatology 27(3):685–690
Narumi S, Roberts JP, Emond JC, Lake J, Ascher NL (1995) Liver transplantation for sclerosing cholangitis. Hepatology 22(2):451–457
Soetikno RM, Lin OS, Heidenreich PA, Young HS, Blackstone MO (2002) Increased risk of colorectal neoplasia in patients with primary sclerosing cholangitis and ulcerative colitis: a meta-analysis. Gastrointest Endosc 56(1):48–54
Lindberg BU, Broome U, Persson B (2001) Proximal colorectal dysplasia or cancer in ulcerative colitis. The impact of primary sclerosing cholangitis and sulfasalazine: results from a 20-year surveillance study. Dis Colon Rectum 44(1):77–85
Loftus EV Jr, Harewood GC, Loftus CG et al (2005) PSC-IBD: a unique form of inflammatory bowel disease associated with primary sclerosing cholangitis. Gut 54(1):91–96
Cullen SN, Chapman RW (2006) The medical management of primary sclerosing cholangitis. Semin Liver Dis 26(1):52–61
Beuers U, Spengler U, Kruis W et al (1992) Ursodeoxycholic acid for treatment of primary sclerosing cholangitis: a placebo-controlled trial. Hepatology 16(3):707–714
Stiehl A, Walker S, Stiehl L, Rudolph G, Hofmann WJ, Theilmann L (1994) Effect of ursodeoxycholic acid on liver and bile duct disease in primary sclerosing cholangitis. A 3-year pilot study with a placebo-controlled study period. J Hepatol 20(1):57–64
Lindor KD (1997) Ursodiol for primary sclerosing cholangitis. Mayo Primary Sclerosing Cholangitis-Ursodeoxycholic Acid Study Group. N Engl J Med 336(10):691–695
Mitchell SA, Bansi DS, Hunt N, Von Bergmann K, Fleming KA, Chapman RW (2001) A preliminary trial of high-dose ursodeoxycholic acid in primary sclerosing cholangitis. Gastroenterology 121(4):900–907
Olsson R, Boberg KM, de Muckadell OS et al (2005) High-dose ursodeoxycholic acid in primary sclerosing cholangitis: a 5-year multicenter, randomized, controlled study. Gastroenterology 129(5):1464–1472
Cullen SN, Rust C, Fleming K, Edwards C, Beuers U, Chapman R (2008) High dose ursodeoxycholic acid for the treatment of primary sclerosing cholangitis is safe and effective. J Hepatol 48(5):792–800
Harnois DM, Angulo P, Jorgensen RA, Larusso NF, Lindor KD (2001) High-dose ursodeoxycholic acid as a therapy for patients with primary sclerosing cholangitis. Am J Gastroenterol 96(5):1558–1562
Brandsaeter B, Isoniemi H, Broome U et al (2004) Liver transplantation for primary sclerosing cholangitis; predictors and consequences of hepatobiliary malignancy. J Hepatol 40(5):815–822
Pardi DS, Loftus EV Jr., Kremers WK, Keach J, Lindor KD (2003) Ursodeoxycholic acid as a chemopreventive agent in patients with ulcerative colitis and primary sclerosing cholangitis. Gastroenterology 124(4):889–893
Tung BY, Emond MJ, Haggitt RC et al (2001) Ursodiol use is associated with lower prevalence of colonic neoplasia in patients with ulcerative colitis and primary sclerosing cholangitis. Ann Intern Med 134(2):89–95
Beuers U (2006) Drug insight: Mechanisms and sites of action of ursodeoxycholic acid in cholestasis. Nature Clin Pract Gastroenterol Hepatol 3(6):318–328
Paumgartner G, Beuers U (2002) Ursodeoxycholic acid in cholestatic liver disease: mechanisms of action and therapeutic use revisited. Hepatology 36(3):525–531
Lazaridis KN, Gores GJ, Lindor KD (2001) Ursodeoxycholic acid ‘mechanisms of action and clinical use in hepatobiliary disorders’. J Hepatol 35(1):134–146
Karlsen TH, Lie BA, Frey Froslie K et al (2006) Polymorphisms in the steroid and xenobiotic receptor gene influence survival in primary sclerosing cholangitis. Gastroenterology 131(3):781–787
Hruz P, Zimmermann C, Gutmann H et al (2006) Adaptive regulation of the ileal apical sodium dependent bile acid transporter (ASBT) in patients with obstructive cholestasis. Gut 55(3):395–402
Stiehl A, Rudolph G, Sauer P, Theilmann L (1995) Biliary secretion of bile acids and lipids in primary sclerosing cholangitis. Influence of cholestasis and effect of ursodeoxycholic acid treatment. J Hepatol 23(3):283–289
Serfaty L, De Leusse A, Rosmorduc O et al (2003) Ursodeoxycholic acid therapy and the risk of colorectal adenoma in patients with primary biliary cirrhosis: an observational study. Hepatology 38(1):203–209
Fickert P, Wagner M, Marschall HU et al (2006) 24-norUrsodeoxycholic acid is superior to ursodeoxycholic acid in the treatment of sclerosing cholangitis in Mdr2 (Abcb4) knockout mice. Gastroenterology 130(2):465–481
Hofmann AF, Zakko SF, Lira M et al (2005) Novel biotransformation and physiological properties of norursodeoxycholic acid in humans. Hepatology 42(6):1391–1398
Makishima M, Okamoto AY, Repa JJ et al (1999) Identification of a nuclear receptor for bile acids. Science 284(5418):1362–1365
Parks DJ, Blanchard SG, Bledsoe RK et al (1999) Bile acids: natural ligands for an orphan nuclear receptor. Science 284(5418):1365–1368
Paumgartner G, Pusl T (2008) Medical treatment of cholestatic liver disease. Clin Liver Dis 12(1):53–80
Eloranta JJ, Jung D, Kullak-Ublick GA (2006) The human Na + -taurocholate cotransporting polypeptide gene is activated by glucocorticoid receptor and peroxisome proliferator-activated receptor-gamma coactivator-1alpha, and suppressed by bile acids via a small heterodimer partner-dependent mechanism. Mol Endocrinol 20(1):65–79
Jung D, Kullak-Ublick GA (2003) Hepatocyte nuclear factor 1 alpha: a key mediator of the effect of bile acids on gene expression. Hepatology 37(3):622–631
Eloranta JJ, Kullak-Ublick GA (2005) Coordinate transcriptional regulation of bile acid homeostasis and drug metabolism. Arch Biochem Biophys 433(2):397–412
Barbier O, Torra IP, Sirvent A et al (2003) FXR induces the UGT2B4 enzyme in hepatocytes: a potential mechanism of negative feedback control of FXR activity. Gastroenterology 124(7):1926–1940
Gnerre C, Blattler S, Kaufmann MR, Looser R, Meyer UA (2004) Regulation of CYP3A4 by the bile acid receptor FXR: evidence for functional binding sites in the CYP3A4 gene. Pharmacogenetics 14(10):635–645
Grober J, Zaghini I, Fujii H et al (1999) Identification of a bile acid-responsive element in the human ileal bile acid-binding protein gene. Involvement of the farnesoid X receptor/9-cis-retinoic acid receptor heterodimer. J Biol Chem 274(42):29749–29754
Cariou B, Staels B (2006) The expanding role of the bile acid receptor FXR in the small intestine. J Hepatol 44(6):1213–1215
Landrier JF, Eloranta JJ, Vavricka SR, Kullak-Ublick GA (2006) The nuclear receptor for bile acids, FXR, transactivates human organic solute transporter-alpha and -beta genes. Am J Physiol Gastrointest Liver Physiol 290(3):G476–485
Neimark E, Chen F, Li X, Shneider BL (2004) Bile acid-induced negative feedback regulation of the human ileal bile acid transporter. Hepatology 40(1):149–156
Pellicciari R, Fiorucci S, Camaioni E et al (2002) 6alpha-ethyl-chenodeoxycholic acid (6-ECDCA), a potent and selective FXR agonist endowed with anticholestatic activity. J Med Chem 45(17):3569–3572
Fiorucci S, Clerici C, Antonelli E et al (2005) Protective effects of 6-ethyl chenodeoxycholic acid, a farnesoid X receptor ligand, in estrogen-induced cholestasis. J Pharmacol Exp Ther 313(2):604–612
Goodwin B, Jones SA, Price RR et al (2000) A regulatory cascade of the nuclear receptors FXR, SHP-1, and LRH-1 represses bile acid biosynthesis. Mol Cell 6(3):517–526
Liu Y, Binz J, Numerick MJ et al (2003) Hepatoprotection by the farnesoid X receptor agonist GW4064 in rat models of intra- and extrahepatic cholestasis. J Clin Invest 112(11):1678–1687
Fiorucci S, Antonelli E, Rizzo G et al (2004) The nuclear receptor SHP mediates inhibition of hepatic stellate cells by FXR and protects against liver fibrosis. Gastroenterology 127(5):1497–1512
Wagner M, Fickert P, Zollner G et al (2003) Role of farnesoid X receptor in determining hepatic ABC transporter expression and liver injury in bile duct-ligated mice. Gastroenterology 125(3):825–838
Stedman C, Liddle C, Coulter S et al (2006) Benefit of farnesoid X receptor inhibition in obstructive cholestasis. Proc Natl Acad Sci U S A 103(30):11323–11328
Kliewer SA, Willson TM (2002) Regulation of xenobiotic and bile acid metabolism by the nuclear pregnane X receptor. J Lipid Res 43(3):359–364
Bertilsson G, Heidrich J, Svensson K et al (1998) Identification of a human nuclear receptor defines a new signaling pathway for CYP3A induction. Proc Natl Acad Sci U S A 95(21):12208–12213
Staudinger JL, Goodwin B, Jones SA et al (2001) The nuclear receptor PXR is a lithocholic acid sensor that protects against liver toxicity. Proc Natl Acad Sci U S A 98(6):3369–3374
Fang HL, Strom SC, Ellis E et al (2007) Positive and negative regulation of human hepatic hydroxysteroid sulfotransferase (SULT2A1) gene transcription by rifampicin: roles of hepatocyte nuclear factor 4alpha and pregnane X receptor. J Pharmacol Exp Ther 323(2):586–598
Gardner-Stephen D, Heydel JM, Goyal A et al (2004) Human PXR variants and their differential effects on the regulation of human UDP-glucuronosyltransferase gene expression. Drug Metab Dispos 32(3):340–347
Geick A, Eichelbaum M, Burk O (2001) Nuclear receptor response elements mediate induction of intestinal MDR1 by rifampin. J Biol Chem 276(18):14581–14587
Kast HR, Goodwin B, Tarr PT et al (2002) Regulation of multidrug resistance-associated protein 2 (ABCC2) by the nuclear receptors pregnane X receptor, farnesoid X-activated receptor, and constitutive androstane receptor. J Biol Chem 277(4):2908–2915
Teng S, Jekerle V, Piquette-Miller M (2003) Induction of ABCC3 (MRP3) by pregnane X receptor activators. Drug Metab Dispos 31(11):1296–1299
Teng S, Piquette-Miller M (2007) Hepatoprotective role of PXR activation and MRP3 in cholic acid-induced cholestasis. Br J Pharmacol 151(3):367–376
Bachs L, Pares A, Elena M, Piera C, Rodes J (1989) Comparison of rifampicin with phenobarbitone for treatment of pruritus in biliary cirrhosis. Lancet 1(8638):574–576
Bachs L, Pares A, Elena M, Piera C, Rodes J (1992) Effects of long-term rifampicin administration in primary biliary cirrhosis. Gastroenterology 102(6):2077–2080
Marschall HU, Wagner M, Zollner G et al (2005) Complementary stimulation of hepatobiliary transport and detoxification systems by rifampicin and ursodeoxycholic acid in humans. Gastroenterology 129(2):476–485
Dilger K, Denk A, Heeg MH, Beuers U (2005) No relevant effect of ursodeoxycholic acid on cytochrome P450 3A metabolism in primary biliary cirrhosis. Hepatology 41(3):595–602
Khurana S, Singh P (2006) Rifampin is safe for treatment of pruritus due to chronic cholestasis: a meta-analysis of prospective randomized-controlled trials. Liver Int 26(8):943–948
Wagner M, Halilbasic E, Marschall HU et al (2005) CAR and PXR agonists stimulate hepatic bile acid and bilirubin detoxification and elimination pathways in mice. Hepatology 42(2):420–430
Stojakovic T, Putz-Bankuti C, Fauler G et al (2007) Atorvastatin in patients with primary biliary cirrhosis and incomplete biochemical response to ursodeoxycholic acid. Hepatology 46(3):776–784
Boberg KM, Egeland T, Schrumpf E (2003) Long-term effect of corticosteroid treatment in primary sclerosing cholangitis patients. Scand J Gastroenterol 38(9):991–995
Maier A, Zimmermann C, Beglinger C, Drewe J, Gutmann H (2007) Effects of budesonide on P-glycoprotein expression in intestinal cell lines. Br J Pharmacol 150(3):361–368
Sandborn WJ, Feagan BG, Lichtenstein GR (2007) Medical management of mild to moderate Crohn’s disease: evidence-based treatment algorithms for induction and maintenance of remission. Aliment Pharmacol Ther 26(7):987–1003
Wiegand J, Schuler A, Kanzler S et al (2005) Budesonide in previously untreated autoimmune hepatitis. Liver Int 25(5):927–934
Leuschner M, Maier KP, Schlichting J et al (1999) Oral budesonide and ursodeoxycholic acid for treatment of primary biliary cirrhosis: results of a prospective double-blind trial. Gastroenterology 117(4):918–925
Rautiainen H, Karkkainen P, Karvonen AL et al (2005) Budesonide combined with UDCA to improve liver histology in primary biliary cirrhosis: a three-year randomized trial. Hepatology 41(4):747–752
Hempfling W, Grunhage F, Dilger K, Reichel C, Beuers U, Sauerbruch T (2003) Pharmacokinetics and pharmacodynamic action of budesonide in early- and late-stage primary biliary cirrhosis. Hepatology 38(1):196–202
Jung D, Fantin AC, Scheurer U, Fried M, Kullak-Ublick GA (2004) Human ileal bile acid transporter gene ASBT (SLC10A2) is transactivated by the glucocorticoid receptor. Gut 53(1):78–84
van Hoogstraten HJ, Vleggaar FP, Boland GJ et al (2000) Budesonide or prednisone in combination with ursodeoxycholic acid in primary sclerosing cholangitis: a randomized double-blind pilot study. Belgian–Dutch PSC Study Group. Am J Gastroenterol 95(8):2015–2022
Angulo P, Batts KP, Jorgensen RA, LaRusso NA, Lindor KD (2000) Oral budesonide in the treatment of primary sclerosing cholangitis. Am J Gastroenterol 95(9):2333–2337
Lechner D, Kallay E, Cross HS (2007) 1alpha,25-dihydroxyvitamin D3 downregulates CYP27B1 and induces CYP24A1 in colon cells. Mol Cell Endocrinol 263(1–2):55–64
Kim MS, Fujiki R, Kitagawa H, Kato S (2007) 1alpha,25(OH)2D3-induced DNA methylation suppresses the human CYP27B1 gene. Mol Cell Endocrinol 265–266:168–173
Turunen MM, Dunlop TW, Carlberg C, Vaisanen S (2007) Selective use of multiple vitamin D response elements underlies the 1 alpha,25-dihydroxyvitamin D3-mediated negative regulation of the human CYP27B1 gene. Nucleic Acids Res 35(8):2734–2747
Wang TT, Tavera-Mendoza LE, Laperriere D et al (2005) Large-scale in silico and microarray-based identification of direct 1,25-dihydroxyvitamin D3 target genes. Mol Endocrinol 19(11):2685–2695
Shneider BL (2001) Intestinal bile acid transport: biology, physiology, and pathophysiology. J Pediatr Gastroenterol Nutr 32(4):407–417
Craddock AL, Love MW, Daniel RW et al (1998) Expression and transport properties of the human ileal and renal sodium-dependent bile acid transporter. Am J Physiol 274(1 Pt 1):G157–169
Chen X, Chen F, Liu S et al (2006) Transactivation of rat apical sodium-dependent bile acid transporter and increased bile acid transport by 1alpha,25-dihydroxyvitamin D3 via the vitamin D receptor. Mol Pharmacol 69(6):1913–1923
McCarthy TC, Li X, Sinal CJ (2005) Vitamin D receptor-dependent regulation of colon multidrug resistance-associated protein 3 gene expression by bile acids. J Biol Chem 280(24):23232–23242
Kozoni V, Tsioulias G, Shiff S, Rigas B (2000) The effect of lithocholic acid on proliferation and apoptosis during the early stages of colon carcinogenesis: differential effect on apoptosis in the presence of a colon carcinogen. Carcinogenesis 21(5):999–1005
Miyata M, Matsuda Y, Tsuchiya H et al (2006) Chenodeoxycholic acid-mediated activation of the farnesoid X receptor negatively regulates hydroxysteroid sulfotransferase. Drug Metab Pharmacokinet 21(4):315–323
Makishima M, Lu TT, Xie W et al (2002) Vitamin D receptor as an intestinal bile acid sensor. Science 296(5571):1313–1316
Song CS, Echchgadda I, Seo YK et al (2006) An essential role of the CAAT/enhancer binding protein-alpha in the vitamin D-induced expression of the human steroid/bile acid-sulfotransferase (SULT2A1). Mol Endocrinol 20(4):795–808
Gascon-Barre M, Demers C, Mirshahi A, Neron S, Zalzal S, Nanci A (2003) The normal liver harbors the vitamin D nuclear receptor in nonparenchymal and biliary epithelial cells. Hepatology 37(5):1034–1042
Desvergne B, Wahli W (1999) Peroxisome proliferator-activated receptors: nuclear control of metabolism. Endocr Rev 20(5):649–688
Zandbergen F, Plutzky J (2007) PPARalpha in atherosclerosis and inflammation. Biochim Biophys Acta 1771(8):972–982
Itakura J, Izumi N, Nishimura Y et al (2004) Prospective randomized crossover trial of combination therapy with bezafibrate and UDCA for primary biliary cirrhosis. Hepatol Res 29(4):216–222
Dohmen K, Mizuta T, Nakamuta M, Shimohashi N, Ishibashi H, Yamamoto K (2004) Fenofibrate for patients with asymptomatic primary biliary cirrhosis. World J Gastroenterol 10(6):894–898
Iwasaki S, Akisawa N, Saibara T, Onishi S (2007) Fibrate for treatment of primary biliary cirrhosis. Hepatol Res 37(Suppl 3):S515–S517
Kleemann R, Verschuren L, de Rooij BJ et al (2004) Evidence for anti-inflammatory activity of statins and PPARalpha activators in human C-reactive protein transgenic mice in vivo and in cultured human hepatocytes in vitro. Blood 103(11):4188–4194
Kleemann R, Gervois PP, Verschuren L, Staels B, Princen HM, Kooistra T (2003) Fibrates down-regulate IL-1-stimulated C-reactive protein gene expression in hepatocytes by reducing nuclear p50-NFkappa B-C/EBP-beta complex formation. Blood 101(2):545–551
Panigrahy D, Kaipainen A, Huang S, et al (2008) PPAR{alpha} agonist fenofibrate suppresses tumor growth through direct and indirect angiogenesis inhibition. PNAS 105:985–990
Jung D, Fried M, Kullak-Ublick GA (2002) Human apical sodium-dependent bile salt transporter (SLC10A2) gene is regulated by the peroxisome proliferator-activated receptor alpha. J Biol Chem 277(34):30559–30566
Heikkinen S, Auwerx J, Argmann CA (2007) PPARgamma in human and mouse physiology. Biochim Biophys Acta 1771(8):999–1013
Belfort R, Harrison SA, Brown K et al (2006) A placebo-controlled trial of pioglitazone in subjects with nonalcoholic steatohepatitis. N Engl J Med 355(22):2297–2307
Harada K, Isse K, Kamihira T, Shimoda S, Nakanuma Y (2005) Th1 cytokine-induced downregulation of PPARgamma in human biliary cells relates to cholangitis in primary biliary cirrhosis. Hepatology 41(6):1329–1338
Fickert P, Moustafa T, Trauner M (2007) Primary sclerosing cholangitis—the arteriosclerosis of the bile duct? Lipids Health Dis 6:3
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Beuers, U., Kullak-Ublick, G.A., Pusl, T. et al. Medical Treatment of Primary Sclerosing Cholangitis: A Role for Novel Bile Acids and other (post-)Transcriptional Modulators?. Clinic Rev Allerg Immunol 36, 52–61 (2009). https://doi.org/10.1007/s12016-008-8085-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12016-008-8085-y