Abstract
Adoptive cell therapy using CAR T cells has emerged as a novel treatment strategy with promising results against B cell malignancies; however, CAR T cells have not shown much success against solid malignancies. There are several obstacles which diminish the efficacy of CAR T cells, but the immunosuppressive tumor microenvironment (TME) of the tumor stands out as the most important factor. TME includes Tumor-Associated Stroma, Immunosuppressive cells and cytokines, tumor hypoxia and metabolism, and Immune Inhibitory Checkpoints which affect the CAR T cell efficacy and activity in solid tumors. A precise understanding of the TME could pave the way to engineer novel modifications of CAR T cells which can overcome the immunosuppressive TME. In this review, we will describe different sections of the TME and introduce novel approaches to improve the CAR T cells potential against solid tumors based on recent clinical and preclinical data. Also, we will provide new suggestions on how to modify CARs to augment of CAR T cells efficacy. Since there are also some challenges beyond the TME that are important for CAR function, we will also discuss and provide data about the improvement of CAR T cells trafficking and delivery to the tumor site and how to solve the problem of tumor antigen heterogeneity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
One of the latest advances approach in cancer immunotherapy is Adoptive cell therapy (ACT). Genetically engineering T cells to express chimeric antigen receptors (CAR T cells) have shown promising profits against hematological malignancies in clinical stage [1]. CAR is a genetically designed receptor composed of the extracellular domain (ScFv of tumor-specific antibody), hinge/spacer (derived from IgG4 or CD8), a transmembrane domain, and an intracellular domain (CD3ζ signaling domain with or without CD28 or 4-1BB co-stimulatory domains) [2, 3]. It is noteworthy that the CAR T cells proliferation, efficacy, persistence and, anti-tumor activity in tumor site are related to the level of CAR expression on T cells and increase by co-stimulatory domains [4, 5].
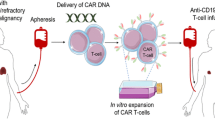
MHC-independency, along with prominent specificity of CAR, determines CAR T cell therapy as a promising method for the treatment of multiple cancers. Although CAR T cell therapy has created encouraging results in hematological cancers, clinical data regarding the potency of CAR T cells in solid tumors are disappointing. This is connected to the lack of appropriate solid tumor antigens for designing CARs, restricted the CAR T cells trafficking to the tumor environment, and immunosuppressive properties of solid cancer microenvironment (Fig. 1) [2, 6].
Immunosuppressive tumor microenvironment. a Physical barrier, including tumor stroma and extracellular matrix, that limits the penetration of the CAR T cells to the tumor. b Immunomodulatory cytokines (such as IL-10, IL-4, and TGF-β) and enzymes that hamper the function and proliferation of CAR T cells inside the TME. c Immunosuppressive cells (such as MDSCs, T-regs, TAMs) that suppress the function of engineered T cells by cell-cell contact and producing immunosuppressive cytokines. d Immune inhibitory checkpoints (such as CTLA-4, PD-1, LAG-3) that inhibit the cytotoxicity of CAR t cells by binding to their ligands (such as PD-L1, PD-L2) on tumor cells and immunosuppressive cells. E Products of hypoxia and aberrant metabolism of the tumor (such as ROS and IDO) which limits the proliferation and existence of the CAR T cells in the TME. Created by Esmaeilzadeh et al.
The tumor microenvironment (TME) has a major role in tumor proliferation, progression, and resistance to treatment by disturbing the antitumor function of the immune system [7]. The complex and heterogeneous microenvironment of the tumor affects the activation and function of the infiltrated effector T cells and thus, impairs the persistence, proliferation, and potential of the T cells [8]. This renders T cells exhausted and induces their anergy. It seems that a comprehensive understanding of the TME is necessary in order to alter the tumor microenvironment and induce more powerful immune responses. This takes the most important part to enhance the anti-tumor efficacy of CAR T cells against solid tumors [9, 10].
Here we aim to discuss the different characteristics of the tumor microenvironment that hamper maximal anti-tumor advantage of CAR T cells in solid tumors which are briefly described in Table 1. Other hurdles will also be noted briefly in the section named Challenges beyond tumor microenvironment. We also provide advanced data on how to reprogram the special properties of tumor microenvironment to improve the sensitivity of CAR T cells and expand its clinical benefit in several solid tumors based on recently published data (Fig. 2).
Novel approaches to improve efficacy of CAR T cells against the tumor microenvironment. a CAR T cells can be engineered against tumor-associated fibroblasts (FAP-CARs). In order ease the infiltration of the CAR T cells to the tumor stroma, they are engineered to produce heparanase (HPSE-CAR). b Overcoming the immune inhibitory checkpoints can be achieved by blocking immune checkpoints, using mAb, checkpoint inhibitors, and engineering checkpoint-knockout CAR T cells via CRISP-R/Cas9 system. c Hypoxia can be targeted via HIF-CAR. N-acetyl cysteine can also be applied to decrease the oxidative stress. Catalase-producing CAR T cells (CAT-CARs) can degrade the H2O2 which is present in high levels in tumor mircoenvironment. IDO inhibitors and RIAD-CARs are used to modulate tumor metabolism. e DN TGF-β CAR T cells lacks the receptor for TGF-β. TRUCK T cells can produce ILs such as IL-12, IL-15, and IL-18. 7 × 19 CAR contins the receptor for IL-7 and CCL19. 4/7 ICR CAR contains the IL-4 exodomain and is resistant to IL-4 induced immunosuppression. CD73 inhibitors diminish production of adeosine in tumor site. e There is need for novel strategies which could deprive the immunomodulatory effect of immunosuppressing cells in the TME. Created by Esmaeilzadeh et al
Tumor-Associated Stroma and Enzymes
Tumor-stroma has been identified as a significant factor of solid tumors which supports the initiation and persistence of the tumor [42]. Tumor-stroma is composed of vascular endothelial cells, connective tissue cells, immune cells, and tumor fibroblasts. Current CAR T cell therapeutic strategies have focused on targeting cancer cells; however, accumulating data have demonstrated that targeting tumor-stromal cells could help to increase the anti-tumor efficacy of the treatment, as well. Tumor-stromal cells named as cancer-associated stroma cells (CASCs) play a substantial role in the pathogenesis of solid tumor. One of the CASCs with a significant role is “cancer-associated fibroblast” (CAF) cell which plays an important role in the immunosuppressive function of the tumor microenvironment. CAFs exert their function especially by secreting several cytokines and chemokines such as SDF/CXCL12, “vascular endothelial growth factor” (VEGF), and other several growth factors. In this manner, CAFs help to promote tumor growth, metastasis, and angiogenesis. CAR T cell can target the one cell surface marker of the CAF cells which known as fibroblast activation protein (FAP), a member of the serine protease family. [43] According to these data, some groups have assessed the potency of anti-FAP CAR T cells and contrasting results have been achieved.
Kakarla and colleagues engineered anti-FAP CAR T cells against A549 lung cancer model which reduced the progression of the tumor. They also reported that concomitant application of anti-FAP and anti-cancer cell CAR T cells would lead to an improved anti-tumor response [44].
In addition to FAP, there are also other targets in the tumor-stroma that can be targeted by CAR T cells. Heparan sulfate proteoglycan (HSPG) is an important part of the tumor stroma that inhibits aggregation and infiltration of the T cells to the tumor site. HSPG is degraded by heparanase enzyme (HPSE) which is produced by T cells. However, it is demonstrated that T cells lose the ability to produce HSPE within the CAR T cell manufacturing procedure. HPSE plays a significant role in trafficking and infiltration of the T cells to the tumor site and it proposed to enable CAR T cells to express the HPSE [45, 46]. In a study by Caruana and colleagues [13], inducing the expression of the HPSE by CAR T cells in human neuroblastoma xenograft model led to an improved degradation of the tumor extracellular matrix accompanied by enhanced the CAR T cells infiltration to the tumor microenvironment.
Clinical results regarding administration of the CAR T cells against stroma-specific targets such as HPSE and FAP are promising and beneficial; however, identifying and targeting CARs against new stroma targets could help to improve the anti-tumor immunity of CAR T cells.
Cytokines
The direct inhibition of immune-suppressing cytokines is the approach to increase the potency of CAR-directed therapy. TGF-β encompasses the ability to suppress the function of CD8+ T cells and modify CD4+ T cells toward the regulatory route. In 2002, a study demonstrated that designing a TGF-β receptor-negative engineered-T cell could improve the efficacy of immunotherapy [47]. In 2017, Mohammed et al. [17] studied the efficacy of “prostate stem cell antigen” (PSCA)-redirected CAR against prostate cancer. They modified the T cells by binding the IL-4 exodomain and IL-7 endodomain to each other, which known as 4/7 ICR CAR-PSCA were shown to have enhanced CAR T cells anti-tumor activity. In order to improve the efficacy of this approach, 4/7 ICR could also be combined with TRUCK T cells.
CAR T cells can be armed with the transgene which enables them to secrete anti-tumor cytokines such as IL-12, 15, 18, 21, and 7. The fourth generation of CAR T cells known as TRUCK-T cells (T-cells redirected for universal cytokine-mediated killing) contain the transgene to release specific cytokine inside the tumor site [6, 48,49,50]. Moreover, the most appropriate candidates seem to be IL-12 and IL-18 [51].
These considerations led to the production of TRUCK T cells combining the ability of cytokine production with CAR expression. Since IL-12 activates the patient’s immune system against tumor cells, it could also lead to the destruction of the antigen-negative tumor cells. Koneru et al. designed IL-12 secreting anti-MUC-16ecto CAR T cell for a phase I clinical trial against ovarian cancer. This study proved this approach to be highly safe and efficient against ovarian cancer [15].
In 2017, Chmielewski et al. [41] thought to improve anti-tumor immune response by inducing acute inflammatory environment through the inducible expression of IL-18 by CAR T cells. The immunosuppressive Dendritic Cells, T-regs, and M2 macrophages were reported to be decreased in number, while NKG2D+ NK cells and M1 macrophages were increased in the tumor site. All in all, IL-18 expressing TRUCK T cells were reported to sensitize lung and pancreatic tumors to immune reaction through altering the immunosuppressive TME.
IL-21 is another cytokine which can be used for developing TRUCK-T cells. In melanoma, IL-21 producing TRUCKs increased the function of TCD8+ cells in tumor site and elevated the memory CAR T cell survival. This was achieved by enhanced activation of the Wnt/β-catenin in T cell through the expression of the Lef1, Tcf7, and L-selectin genes [52].
IL-7 and IL-15 are potent stimulators of the proliferation and expansion of CD8+ T cells [53]. Also, genetically engineering CAR T cells to express IL-7Rα could improve the function and efficacy of CARs inside the solid tumor environment. Adachi et al. studied the anti-tumor activity of IL-7 and CCL19 (7 × 19 CAR-T cells) in an invivo mouse model. This study demonstrated that 7 × 19 CAR T cells prolonged mouse survival and had increased anti-tumor function. Also, 7 × 19 CAR T cells improved the DCs infiltration into the tumor microenvironment and thus improved the potential of the innate immune system against the tumor [18].
Hypoxia, Nutrient Deficiency, and Metabolism
Nutrient deficiency, hypoxia, and solid tumor metabolism are major hallmarks of the TME that hamper the efficacy and CAR T cells function.
Hypoxia
Is an important characteristic of the TME caused by lack of vasculature and a high number of compressed tumor cells and tumor matrix. Since T cells need oxygen for proliferation and function, hypoxia boosts cancer metastasis and increases the resistance of the tumor to CAR T therapy. Utilization of the glycolysis pathway by tumor cells instead of oxidative phosphorylation, named as Warburg effect, leads to the production of lactate that increases the acidity of the tumor microenvironment. Low PH is a castrating factor of the T cell’s function. This also generates reactive oxygen species (ROS) causing oxidative stress that disrupts the anti-tumor activity of CAR T cells. In order to dominate this obstacle, CAR T cells were modified to secrete catalase (CAT-CAR), which is an antioxidant enzyme and degrades H2O2 in the TME. CAT-CARs were reported to have increased resilience against ROS by reducing the oxidative stress state inside the TME. These cells also reported maintaining the anti-tumor activity of CAR T cells in tumor local microenvironment [21, 54]. Another approach to reducing the mortality of T cells caused by tumor-induced metabolic stress could be the application of anti-oxidant factors. Scheffel and colleagues reported the decreased T cell death cell after application of N-acetyl cysteine (NAC) as an anti-oxidant agent [24]. This study could pave the way to engineering anti-oxidant producing CAR T cells or using anti-oxidant agents with CAR T cell therapy in order to overcome the oxidative stress caused by the tumor microenvironment.
Hypoxic microenvironment of the tumor leads to the production of a tumor-promoting protein named as Hypoxia Inducible Factor (HIF), which has a major role in tumor progression. HIF improves tumor angiogenesis, proliferation, invasion, metastasis, and growth [55]. HIF is highly produced in the hypoxic environment of multiple solid tumors. Sensitizing CAR T cells through the hypoxia could increase the accuracy of tumor targeting by CAR T cells. It was recently proposed to target hypoxia by fusing HIF to the CAR scaffold. Using this approach, CAR T cells were locally activated in the hypoxic TME which would prevent the CAR T cell activation in other normal tissues. This strategy led to the construction of the first model of self-decision making CARs that are only activated in the hypoxic TME of the tumor [56]. Targeting HIF could be a platform for designing the next generations of smarter self-decision making CARs against other molecules which are specific for tumor microenvironment.
Nutrient Starvation and Metabolism
Stands out as a key factor that reduces function and cytokine secretion of CAR T cells. Lack of specific nutrients such as glucose and amino acids that have an significant role in metabolism of T cell and lack of these agents could disturb its function. Tryptophan, lysine, and arginine are the most important amino acids required for T cell metabolism. Lack of tryptophan can induce autophagy response in T cells. Tumor cells and MDSCs produce “Indoleamine 2,3 dioxygenase” (IDO), the catalyst of tryptophan degradation, that finally leads to anergy of T cells along with aggregation of immunosuppressor T-regs [22]. Combination of CAR T cell and IDO-inhibitors could be considered as a new suggestion for the treatment of chemo-resistant tumors. Also, decreased bioavailability of arginine caused by arginase production by MDSCs leads to nutrient starvation with a similar effect on the function of CAR T cells [6].
Modification of the tumor microenvironment elements may emerge as a promising approach to enhance the function of CAR T cells. One of the immunosuppressive components is protein kinase-A (PKA) which can inhibit the activity of CAR T cells. “Regulatory subunit I anchoring disruptor” (RIAD) disrupts the PKA function and thus has been used to engineer RIAD-CARs targeting mesothelin. These CAR T cells exhibited increased progression and anti-tumor immunity. Also, the expression of RIAD enhanced chemotaxis in the microenvironment through increased expression of CXCR3 [23].
Also, extracellular adenosine, which is produced from extracellular ATP through the function of CD39 and CD73, is a metabolic immune checkpoint that can exert multiple immune-suppressing properties. Through its receptors, extracellular adenosine activates a number of immunoregulatory cells and cytokines. Also, since adenosine receptors are expressed on immune cells, it hampers the pro-inflammatory activities of multiple immune cells. Inhibition of adenosine function via multiple pathways has reported promising results in multiple studies [19, 57].
Two major strategies have been introduced for blocking the function of adenosine. The first one is to target CD73 with a mAb to inhibit the production of adenosine [19]. Another approach to block the activity of adenosine through direct blocking of its receptor, A2AR, via A2AR antagonists. In one study in 2017, Beavis and colleagues [33] studied the efficacy of anti-HER2 CAR T cells combined with anti-A2AR antagonist against melanoma tumor cells. The detailed information relating to this study has been described in the immune inhibitory section. Since this preclinical study demonstrated promising results, a clinical trial has been designed (NCT02655822) which focuses on the application of A2AR antagonists in multiple solid cancers.
Alteration of the tumor microenvironment metabolism and hypoxia can be a promising approach for CAR T cell efficacy enhancement.
Immunosuppressive Cells
The CAR T cell efficacy against solid tumors is partly restricted by immunomodulatory effects of some cellular elements of the TME. Regulatory T cells (T-regs), Tumor-Associated Macrophages (TAMs), Tumor-Associated Neutrophils (TANs), immature Dendritic Cells (iDCs), and Myeloid-Derived Suppressor Cells (MDSCs) are the most important immunosuppressor cells of the TME [58].
Myeloid-Derived Suppressor Cells (MDSCs)
Accumulating data have validated the important role of infiltrating MDSCs in tumor progression. The immunosuppressive characteristics of MDSCs are proven to be related to the IL-10, TGF-β, inducible Nitric Oxide Synthase (iNOS), arginine, cyclooxygenase-2 (COX-2), and Indolamine 2,3-dioxygenase (IDO) expression [1]. Also, MDSCs have the potential to induce the activation of T-regs. All these functions attribute the immunosuppressive functions of the MDSCs. Thus, it was proposed that CAR T cells function can increase through the suppressing or blocking the function of MDSCs.
Since CXC15-CXCR2 signaling pathway has an essential role in the promotion and recruitment of MDSCs in TME, Wang et al. designed a study to assess the elimination of this pathway. It was demonstrated that blocking the CXC15-CXCR2 pathway decreases the number of MDSCs and improves the anti-tumor responses and survival in a prostate cancer model.
“All-trans retinoic acid” (ALTRA), the stimulator of the immature myeloid blasts that form MDSCs with major immunosuppressive properties in the TME, could be also recruited to suppress the function of the MDSCs. Utilization of ALTRA along with GD2-CAR T cells was reported to reduce the number and the activity of MDSCs in the pediatric sarcoma xenograft models [36].
Tumor-Associated Macrophages (TAMs)
TAMs are the M2 phenotype macrophages and have a significant role in the progression of the tumor by producing multiple cytokines such as IL-10. Also, TAMs produce multiple growth factors such as granulocyte-macrophage colony stimulating factor (GM-CSF) and vascular endothelial growth factor (VEGF) [59]. TAMs can promote the metastasis of the tumor by secreting matrix metalloproteinases (MMPs) such as MMP2 and MMP9 which can destruct the extracellular matrix and lead to metastasis [60]. TAMs have also reported inhibiting the function of CAR T cells by highly expression of PD-L1 [61]. This validates the importance of inhibiting the PD-1 immune checkpoint in the inhibition of tumor progression.
Regulatory T Cell (T-Regs)
Since T-regs are potential inhibitors of CD8+ T cells, they are accompanied with poor prognosis in patients. TME has reported being rich in T-reg number. T-regs disturb the T cells activity via downregulation of the CD80/CD86 signaling pathway, which is an important immune pathway and is associated with T cells activation [6]. They also accelerate the production of IDO-1 by DCs and produce adenosine [62]. T-regs can also limit the immune function of CARs by producing TGF-β and IL-10 [63]. MDSCs have the potential to induce the activation and function of T-regs, which highlights the importance of MDSC inhibition in controlling the progression of the tumor [6]. Also, IL-2, a cytokine with a proven effect on the proliferation and efficacy of CAR T cells, can quickly be taken up by T-regs and subsequently stimulate their proliferation [64].
Immature Dendritic Cell (iDC)
Dendritic Cells are a group of APCs that have an anti-tumor role inside the body. However, inside the tumor microenvironment, DCs exhibit pro-tumorigenic features and acquire immunosuppressive characteristics. These immunosuppressive DCs promote the progression of tumor cells and suppress the T cells function [65]. These concepts introduce inhibiting DCs as an appropriate strategy to elevate the potency of CAR T cell therapy in solid tumors.
Tumor-Associated Neutrophils (TAN)
TANs are a group of neutrophils and are distinct from peripheral blood neutrophils in terms of their surface proteins and their function. TANs exhibit tumor-promoting properties by multiple pathways such as hindering the function and activity of CD8+ T cells through arginase-1, promoting tumor angiogenesis via production of VEGF, and destructing the tumor stroma by MMP9 [66]. Targeting TANs could also be introduced as a promising approach for increasing the resistance of the CAR T cells to the immunosuppressive TME.
Immune Inhibitory Checkpoints
Inhibitory receptors expressed on T cell surface inhibit the transmission of antigen receptors, stimulate apoptosis, maintain peripheral tolerance and regulate immune responses [67]. Some of these receptor identified as immune checkpoint receptors include cytotoxic T lymphocyte antigen 4 (CTLA-4), B and T Lymphocyte Attenuators (BTLA), Programmed Death 1 (PD-1), Lymphocyte activation gene 3 (LAG3), T cell immunoglobulin and mucin-3 (TIM-3), adenosine 2A receptor (A2AR), and T cell immunoglobulin and ITIM domain (TIGIT) [68]. These checkpoint receptors are upregulated via the reaction of their ligands on the tumor cells surface or “antigen presenting cells” (APC). This reaction results in the suppression of the function of the T cells in the tumor site. Recent studies demonstrate targeting inhibitory checkpoint receptors as one of the most important strategies for the solid tumors treatment [69]. Some of these immune checkpoints receptors and their mechanisms are described below.
-
1.
CTLA4 (cytotoxic T lymphocyte antigen 4) is an inhibitory checkpoint which is expressed on activated T cells [70].CTLA4 bind to its ligand B7.1 (CD80) and B7.2 (CD86) at the APC surface with higher affinity than CD28 [71]. In tumor cells, due to a decrease in the level of intrinsic immunity and absence of CD28, CTLA4 is upregulated and inhibits T cells activity [72]. In addition, CTLA4 causes the down-regulation of CD4+ T cells and enhances the immunosuppressive function of the T-regs [25]. Thus, blocking CTLA-4 leads to an increase in T CD4+ function and inhibition of the immunosuppressive activity of T-reg [73]. According to accumulating data, blocking CTLA4 via monoclonal antibodies in combination with CAR T cell therapy could suppress the inhibitory effect of CTLA-4 and improve the anti-tumor efficacy. Also, genetical modifying CARs, specifically via CRISP-R/Cas9 system, in order to eliminate the CTLA-4 could be a promising approach for further studies [26].
-
2.
PD1 (Programmed Death 1) is a negative regulator receptor that is expressed on activated T cells, which reduces T cell function and proliferation [74]. Also, PD1 is expressed on T-regs and increases its immunosuppressive response in the tumor microenvironment [75]. The ligands for PD-1 are known as a PD-L1 (B7-H1) and PD-L2 (B7-DC) [76]. PD-L1 is highly expressed on tumor cells in various solid tumors [77].
Some clinical trials have designed CAR-T cells that produce CTLA-4 and PD-1 antibodies in various solid tumors, including, MUC1+ solid tumors (NCT03179007), EGFR+ solid tumors (NCT03182816), Mesothelin+ solid tumors (NCT03182803), EGFR family+ lung, liver and stomach cancer (NCT02862028), and Glioblastoma Multiform (NCT03170141).
Another method has shown that the engineered CAR T cell, by expressing a dominant negative receptor of PD-1 (DNR), can bind to PDL1 of the tumor cells surface as a decoy receptor and prevent their inhibitory signaling. This method of treating mesothelioma and prostate cancer has shown more advantages including permanent efficacy, long half-life, low toxicity, long-term tumor replace, and high potential in limiting of the inhibitory function of checkpoints [78]. It is also possible to eliminate the PD-1 in engineered CAR T cells through CRISP- R/Cas9 genome editing strategy [28].
-
3.
LAG-3 (Lymphocyte Activation Gene-3 or CD233) is an inhibitory checkpoint molecule [79]. Its ligand, known as MHC II, is expressed on tumor epithelial cells, tumor infiltration DCs, and macrophages [80]. In addition, LSECtin, a member of the DC-SIGN family, is another ligand for LAG-3 that is expressed on liver cancer, melanoma, and many tumors [81]. This inhibitory checkpoint has a significant role in T cell suppression and its anergy. Also, it is up-regulated on T-regs and enhances its immunosuppressive function [82]. Zhang et al. [83] engineered LAG-3 knockout CAR T cells with CRISP-R/Cas9 has shown over a 70% increase in anti-tumor immunity [84].
-
4.
TIM3 (T cell immunoglobulin and mucin-3) is an inhibitory checkpoint membrane protein. [85]. Galactin-9 is a well-known ligand that is expressed by tumor cells. By binding to TIM3, Galactin-9 leads to suppression of TH1 and TIL function, induces apoptosis and MDSCs in the tumor microenvironment [86]. In order to overcome TIM3, the CAR T cell can be co-administrated with the anti-TIM3 antibody. Studies have been reported that co-expression of PD1 and TIM3 can be targeted via dual blockade of them using CAR T cell. This leads to the significant increase in the synergic anti-tumor function of T cells and the immune response progression in the tumor microenvironment [87].
-
5.
BTLA (B and T Lymphocyte Attenuators or CD272) is known as an inhibitory receptor. Its ligand, identified as HVEM (Herpes Virus Entry Mediator), is expressed on tumor-related endothelial cells [88]. Some studies have demonstrated that the interaction between BTLA and HVEM decreases T cell cytokine excretion and proliferation in tumor site, especially in melanoma [89]. BTLA and PD1 are co-expressed on exhausted T cells in tumor microenvironment. It has been reported that double blockade of PD1 and BTLA leads to enhancement of T cell proliferation and efficacy [32]. In order to suppress the BTLA immune inhibitory function, a combination of anti-BTLA monoclonal antibody and engineered CAR T cell therapy could be beneficial.
-
6.
TIGIT (T cell Immunoglobulin and Immunotyrosine inhibitory motif (ITIM) domain) is another inhibitory receptor. This checkpoint binds to two ligands include CD155/PVR (poliovirus receptor) and CD112 (PVRL2) that are expressed on APCs, T cells, and tumor cells [90]. The interaction of TIGIT with its ligands induces the secretion of IL-10 and decreases IL-12 production from DCs [91], reduces the release of IFN-γ from T cell and NK cell [90], inhibits T cell proliferation and function, and also suppresses the differentiation of T cells to TH1 and TH17 [92]. Some studies have reported the overexpression of TIGIT in multiple cancers to include endometrial carcinoma [93], lung squamous cell carcinoma [94], colorectal cancer [95], breast cancer [96], kidney-renal clear cell carcinoma [97], and Melanoma [98]. In this study, we suggest the CAR T cells be designed against this receptor to improve their efficacy.
-
7.
A2AR (adenosine 2A receptor) is an inhibitory receptor that is expressed on activated T cell and inhibits its anti-tumor response by interaction with adenosine, a molecule that is produced from extracellular ATP by CD39 and CD73 ectoenzymes [99]. By binding to its receptor, adenosine exerts its immunosuppressive role in tumor hypoxic microenvironment through activation of multiple immunoregulatory cellular components and molecules. These steps finally result in T cell anergy, tumor progression, and therapy-resistance [100]. Studies have reported that targeting this receptor by specific CAR T cell can enhance T cell anti-tumor function by decreasing T-reg activity in solid tumor [20].
Challenges beyond Tumor Microenvironment
CAR T Cells Trafficking to the Solid Tumor Site
Another important obstacle that confines the CAR T cell therapy success against solid tumors is the CAR T cell insufficient migration and permeation to the solid tumor microenvironment. Studies have shown that improving the infiltration of the CAR T cells to the tumor site could enhance the anti-tumor immunity and lead to better clinical outcomes [101]. The chemokines produced by solid tumors need to match the receptors on T cells for appropriate penetration of the CAR T cells. The absence of coordination between chemokines and receptors, named as Chemokine/receptor mismatch, has shown to be a major underlying cause of inadequate CAR T cell penetration to the tumor microenvironment. Scientists proposed modifying CAR T cells to express the specific cytokine receptors to improve the migration and infiltration of the CAR T cells to TME.
One example is the genetical modification of the CAR T cells to express CXCR-2, which has shown to improve the migration of the CAR T cells to the xenograft models of neuroblastoma and mesothelioma tumors [102]. Also, NKG2D CAR T cells modified to express CXCR3 reported eradicating ID8 ovarian tumor line cells [103]. The other approach is to alter tumor cells in order to express chemokines which have receptors on the surface of T cells. This can be achieved by employing oncolytic viruses. Examples of this approach include injecting oncolytic adenovirus to the neuroblastoma tumor cells in order to secrete RANTES and IL-15, which resulted in improved infiltration and migration of the T cells to the tumor stroma [14]. In another preclinical study, NK-92 cell line was modified with EGFR-CAR and oncolytic herpes simplex virus. This study was conducted on brain metastatic model which exhibited encouraging results [2]. It is noteworthy that other approaches for chemokine transport, such as cellular transports, may also be beneficial and effective.
Other hurdles such as physical barriers may also bring about the limited infiltration of the CAR T cells. As mentioned in the Stroma section of this article, breaking the tumor stroma may also enhance the CAR T cell penetration to the tumor microenvironment. Based on this hypothesis, CAR T cells by expression of heparanase to breakdown the physical barrier of the microenvironment to facilitate the penetration of the CAR T cells into the tumor microenvironment [13]. Also, concomitantly targeting tumor vasculature and tumor antigens can accelerate the infusion of CAR T cells through the destruction of the tumor blood vessel endothelial cells. Chinnasamy et al. designed CAR T cells that simultaneously targeted VEGFR-2 and B-16 melanoma in mice which resulted in improved infiltration of the T cells into the tumor site [104].
Another strategy is to engineer self-decision making CAR T cells that are able to selectively migrate to the tumor site which has been comprehensively discussed above [56].
In order to augment the CAR T cells availability in the tumor site, regional injection of the CAR T cells to the solid tumor has been studied. Adusumilli et al. reported local administration of CAR T cells increased the trafficking and anti-tumor efficacy as well as inhibition of tumor growth [105]. Regional and local delivery of CAR T cells to the solid tumor have been discussed in further sections of the article.
Heterogeneity of Solid Tumor Antigens
Antigen heterogeneity of solid tumor is one of the hurdles that restrict the CAR T cell therapy success against the solid tumor. One of the important reasons for the variability of clinical results between hematologic malignancies and solid tumors is the homogeneous expression of target antigens by hematologic malignant cells, while solid tumor cells are highly heterogeneous regarding antigen expression. This leads to the failure of cancer cell recognition by T cells and thus can result in reduced the efficacy of CAR T therapy against solid tumors. Since Tumor Associated Antigens (TAAs) are the most employed targets for engineering CAR against solid tumors, the variability of the TAA expression by different cells of the tumor represents a major obstacle. In addition, CAR T cells function may disturb in the tumor site because of the different levels of the antigen expression in different sites of the tumor. This characteristic of tumor cells makes it difficult to find specific cancer cell antigens which are highly and specifically expressed by cancer cells but not by other normal tissue cells [53]. In addition, there are few Tumor-Specific Antigens (TSAs) which would be specifically and particularly expressed by tumor cells, not by normal tissue cells.
Since CAR T cells are not capable of eradicating target-negative tumor cells, one possible solution can be the administration of armored CAR T cells with the potential for cytokine production. Since IL-12 can induce both innate and adaptive immune responses, IL-12-armored CAR T cells would exhibit immunity against both antigen-positive and antigen-negative tumor cells. In a study, CEA-CAR T cells were armored with IL-12 transgene and were reported to eradicate both CEA-positive and CEA-negative solid tumor cells [106]. Another possible solution may be targeting CSCs which have proven to be present in most solid tumors with a major role in tumor progression and relapse. CSCs carry antigens which are believed to be cancer-specific antigens at least in the early stages of tumor progression and thus can be an appropriate candidate to be targeted by CAR T cells. One example of tumor stem cell targeting by CAR is the Prostate Stem Cell Antigen (PSCA)-redirected CAR T cell therapy against prostate cancer [107]. Recognition of new cancer stem cell antigens could provide new promising targets for designing CAR T cells against solid tumors.
In addition, in order to the cognition of different tumor cells by CAR T cells, it might be helpful to engineer CARs against two or even multiple antigens. Dual-CAR is an example of this method which can target two antigens at the same time. Recently in 2018, compound CAR T cells have shown impressing results against hematologic cancers [108] and can be considered as a promising strategy against solid tumors as well. Using this approach would increase the precise recognition and eradication of heterogeneous solid tumor cells. Also, improving CAR-engineering technologies could help to design multi-target CARs which would show more specific targeting of the tumor cells.
Application of multiple antigen-directed CARs could decrease the rate of on-target, off-tumor toxicity caused by inappropriate cytotoxicity of CAR T cells against normal cells.
CAR T Cell Delivery in Solid Tumors
There are several approaches in which CAR T cells can be transmitted into the tumor site. The most important strategies include the intravenous, also named as systemic delivery, and the local administration, named as regional delivery. Regional delivery approaches include intrapleural, intraperitoneal, intracavitary, and intratumoral injection of CAR T cells.
Some studies have shown the application of intravenous delivery to have promising results in hematologic malignancies and solid tumors such as ovarian cancer [109], metastatic neuroblastoma [110], colon cancer [111], malignant pleural mesothelioma [112], sarcoma [113], metastatic renal cell carcinoma [114], prostate cancer [4], metastatic colorectal cancer [115], progressive glioblastoma [116], and pancreatic cancer [117]. Currently, several clinical trials have assessed the capability of regional delivery of CAR T cells for solid tumor treatment. In one study, Adusumilli and colleagues reported that local delivery of CAR T cell leads to high anti-tumor efficacy with lower T cell doses, partially because of CD4+ cells activation [105]. Also, this delivery method enhanced T cell persistence, expansion, and effector cell differentiation [118]. In addition, local injection of CAR T cell has the ability to prevent the CAR T cells to enter the blood circulation and migrate to other tissues. This will also reduce the systemic side effects of CAR T cell therapy. However, the limitation of regional delivery is its dependence on delivery techniques in compare with systemic delivery. This approach is complex and requires operational supplies and procedures. It can also increase the risks associated with the device include obstruction, defect, and infection. Also, to achieve improved efficacy, it is necessary for the CAR T cells to traffic to distant sites and penetrates to solid tumors. This obstacle is also solved via regional delivery [119].
In one study in 2015, Brown et al. used local administration of CAR T cell targeting IL13aR2 to treat recurrent Glioblastoma in phase I clinical trial. The results reported the anti-tumor response and no adverse effects [120].
Regional delivery of CAR T cells can be a promising method for the treatment of solid tumors. However, more novel strategies are required to study and increase the efficacy of this approach against solid tumors.
Novel Strategies to Enhance the Safety, Efficacy, and Feasibility of CAR-T Cell Therapy in Solid Tumors
To date, several studies have demonstrated the CAR-T cell therapy success in hematological malignancies; however, solid tumors have not achieved much success due to the complex structure and inhibitory obstacles. Accordingly, various strategies have been proposed to target these barriers by CAR-T cells. Therefore, new strategies include gene modification and combinational therapy enhance the efficacy, feasibility, and safety of CAR-T cell therapy in the solid tumor which are discussed here (Fig. 3).
Schematic of various chimeric antigen receptor (CAR). a Split signal CARs. The two split structures of the CAR-T cell are assembled and activated in the presence of a small molecule. b Universal ectodomain CAR. Biotin Binding Immune Receptor with modified extracellular avidin and FITC-specific CAR which increases T cell’s flexibility to target the various and multiple TAA. c SUPRA CAR. The zipFv is composed of a ScFv and leucine zipper that recognition and bind to TAA, which can attach to the leucine zipper of zipCAR that composed of signaling motif. d Physiological CAR. CAR-T cells that ligand/receptor as the extracellular domain that is connected to CD3z signaling domain. e TRUCK. 4th generation of CAR T cells which is engineered to release transgenic material such as cytokine and enzyme in tumor sites. f Tandem CAR. The CAR that contains two distinct ScFvs and one costimulatory domain. g Dual CAR. This CAR structure’s is comprised of the Two CARs specific and contains two costimulatory domains. Created by Esmaeilzadeh et al
CAR T Cell Gene Modification
There are several methods for editing the genome such as CRISPR-Cas9 nucleases, homing endonucleases, zinc finger nucleases, meganucleases, and Transcription activator-like effector nuclease (TALENs) that are successfully used in the design of the transgenic CAR-T cells. The applications of this strategy are used to overcome the inhibitory tumor microenvironment and also increase the specificity of CAR-T cells [121].
Inhibitory Tumor Microenvironment
Tumor microenvironment includes multiple cytokines and inhibitory checkpoints such as TGF-β, PD-L1, and CTLA-4 that inhibit the maximal efficacy of CAR T cells. Some studies have modified CAR T cells using the CRISPR/Cas9 system which is discussed in the cytokine and immune inhibitory checkpoint sections.
Enhancement of CAR-T Cell Specificity
One of the important barriers of CAR T cell therapy is the antigen heterogeneity of solid tumors. Tumor antigen heterogeneity is caused by expression of different antigens as well as distinct levels of antigen expression at different sites of a tumor. Various studies have reported that CAR T cells redirected against one tumor antigen possess lower specificity and efficacy in comparison with dual-CAR T cell. Thereupon, scientists have presented novel theories for engineering flexible CAR T cells by targeting multiple antigens on solid tumors. This strategy could overcome the immune escape of tumor cells and “on target-off tumor” effect of CAR-T cells [3].
Split Signal CARs
Split signal CAR is the other precision controlled CAR-T cell. Wu et al. designed the split construct CAR which exerted its function in the presence of the small molecule. After binding of ScFv to the tumor antigen, this small molecule connects the tumor antigen binding domain to the signaling domain of the CAR. This complex activates the CAR T cell and leads to response to tumor antigen [122].
Universal Ectodomain CAR-T Cell
Universal ectodomain CAR-T cell includes a novel generation of CAR that consists an anti-FITC ScFv as the extracellular domain. Fluorescein isothiocyanate (FITC) is a safely fluochrome use in the body that easily conjugate to its Ab. This anti-FITC ScFv can recognize the FITC-labeled monoclonal Ab which is specific for a target tumor antigen. After binding of anti-FITC ScFv to the FITC, the intracellular domain of the T cell including CD28, CD3z and, 4-1BB is activated.
Anti-tumor mAbs labeled with FITC such as anti-Her2 (trastuzumab), anti-CD20 (rituximab), and anti-EGFR (cetuximab) are fused to the anti-FITC CAR. This connection includes a specific linkage between the anti-FITC CAR and FITC-labeled Ab. This CAR-T cell was reported to increase the T cell proliferation, cytokine release, and tumors lysis. Accordingly, this strategy can be used to target different types of TAAs for cancer treatment [123].
Another type of Universal CAR T cell is produced using biotin-avidin and biotinylated molecules for enhancing CAR T cell specificity. In this approach, biotinylated antigen-specific molecules such as tumor-specific ligands, ScFv, and the monoclonal antibody are used for tumor target recognition. Since avidin has high sensitivity for binding to biotin, this complex binds to the avidin and its attached to its receptor named as Biotin-Binding Immune Receptor (BBIR). This receptor on CAR-T cell can bind to tumor cells that are pre-labeled with biotinylated molecules. Consequently, the intracellular domain of the T cell is activated. Altogether, this method increases the T cell’s flexibility to target various TAAs [123, 124].
Physiological CAR-T Cell
Psychological CAR is another genetically engineered CAR T cell which includes ligand/receptor as the extracellular antigen recognition domain instead of ScFv. Similar to ScFv, the ligand/receptor is connected to the CD3z signaling domain [125]. This strategy has demonstrated promising responses in solid tumors which led to tumor regression. The example of ligand/receptor-based CAR is the production of IL-13-zetakine CAR T cell against glioblastoma multiform [126]. Also, CD27-receptor [127], VEGF (ligand for VEGFR2) [128], heregulin (ligand for Her3/4) [129], NKG2D receptor [130] and NKp30 (receptor for B7-H6) [131] are other examples of physiological CAR T cells.
Supra Car
Split, universal, and programmable CARs (SUPRA CARs) are the novel generation of CAR T cells. SUPRA CARs, in comparison with conventional CARs, are more safe, flexible, and programmable. Also, they possess increased efficacy and specificity. Furthermore, they have enhanced the potential to activate T cells with higher-sensitivity responses to various tumor antigens. They can also make changes in targets without re-engineering the T cells, monitor various pathways of signaling in T cell and some other cells, prevent cytokine release syndrome by controlling the secretion of cytokines, overcome tumor-immune escape, and reduce CAR T cell over-activity [132, 133]. Anti-tumor specific ScFv adaptor molecule (zipFv) and Universal receptor on T cell (zipCAR) are SUPRA CAR system components. The zipFv is composed of a ScFv and leucine zipper. ZipCAR includes the signaling motif (CD3z, CD28, and 4-1BB) and a leucine zipper. Different types of zipFv can be designed to recognize different tumor antigens. Leucine zipper of zipFv can attach to the leucine zipper of zipCAR and activate the T cell, subsequently [132].
SUPRA CAR system can distinguish and respond to various tumor antigens without requiring CAR genetic engineering for each tumor antigen. A SUPRA CAR produced using primary CD8+ T cell containing one zipCAR. This SUPRA CAR was reported to regress the K562 myelogenous leukemia tumor cells by binding to three distinct zipFvs. This led the SUPRA CAR T cells to target a-Axl, Mesothelin, and Her2 concomitantly and thus could regress the leukemia progression [132].
Tandem CAR-T Cell (Tan-CAR)
Another strategy to increase CAR-T cell efficacy and specificity is to use Tan-CAR. Tan-CARs can increase the accuracy of tumor cell targeting and decline the “on target-off tumor” toxicity by targeting two different antigens on the surface of the tumor cell. Concomitant identification of both antigens by Tandem CAR leads to an increased level of safety, specificity, and efficacy in comparison with conventional CAR. An example tandem CAR which was targeting Glioblastoma is using HER2+/IL-13Rα2 Tan-CAR [134, 135].
Dual CAR T Cell
Dual CAR is similar to Tan-CAR regarding the concept of targeting two tumor antigen; however, they differ in the number of the costimulatory domains they consistent. Detailed information of dual CAR T cell is discussed in Heterogeneity of solid tumor antigens section [136, 137].
TRUCK Cell
“T cells Redirected for Universal Cytokine Killing” (TRUCK T cells) are CAR-T cells with the potential to release cytokines like IL-12,1 L-15,1 L-18 and IL-2. TRUCK cells have exhibited increased penetration to the tumor site and enhanced toxicity against tumor cells. TRUCK cells are discussed in the section of Cytokines.
Combinational Therapy with CAR T Cell
In order to enhance the effectiveness of CAR T cell therapy in solid tumors, it could be beneficial to combine CAR-T cell therapy with other therapeutic methods. Some of these combinatorial therapies including chemotherapy, radiotherapy, checkpoint inhibitors, targeted therapies, oncolytic viruses, and chemokine therapies are described in Table 2.
Concluding Remarks
Adoptive cell therapy with CAR T cells has shown impressive results, especially against B cell hematological malignancies. Although there is a long way for CAR T cells to beat solid tumors, some clinical trials have shown promising results. In a study published in 2016 [150], IL13Rα2 CAR T cells were reported to cause complete remission by the transient response (7.5 months) in a patient with multifocal Glioblastoma. All the central nervous system tumors exhibited regression after infusion of IL13Rα2 CAR T cells. CAR T cell therapy against solid tumors include multiple challenges of which the suppressive microenvironment seems to be the most prominent obstacle. Characterizing the special attributes of the immunosuppressive microenvironment has provided new insights into how to promote the function of CAR T cells against solid tumors. The immunosuppressive microenvironment of the solid tumor includes multiple barriers that limit the efficacy of CAR T cell therapy. The tumor stroma reduces the penetration of the CAR T cells to the tumor site. Also, multiple immunosuppressive cytokines which are released by tumor cells and other immunomodulatory cells attribute to suppress the CAR T cells function. Hypoxia, specific tumor microenvironment metabolism, immune inhibitory checkpoints, and immunosuppressive cells play an important role in hampering the anti-tumor potential of the CAR T cells against the solid tumor. In order to overcome these hurdles and improve the CAR T cell therapy efficacy, multiple strategies have been proposed: blockade of immune inhibitory checkpoints, targeting the tumor stroma by CAR T cells, inhibiting immunosuppressive cytokines, sensitizing CAR T cells against hypoxia, and other novel strategies are among the recent innovations to beat the immunosuppressive microenvironment of the solid tumor. Also, combination therapy using CAR T cells in combination with other therapeutic strategies can provide a promising approach against solid tumors. However, in order to optimize the efficacy of CAR T cell therapy in solid tumors, more novel strategies are indispensable to rearrange and improve the structure of CAR. Finally, it is noteworthy that CAR T cell therapy is in its improving stages to overcome obstacles against solid tumors.
References
Xia, A.-L., Wang, X.-C., Lu, Y.-J., Lu, X.-J., & Sun, B. (2017). Chimeric-antigen receptor T (CAR-T) cell therapy for solid tumors: Challenges and opportunities. Oncotarget., 8(52), 90521.
Chen, X., Han, J., Chu, J., Zhang, L., Zhang, J., Chen, C., et al. (2016). A combinational therapy of EGFR-CAR NK cells and oncolytic herpes simplex virus 1 for breast cancer brain metastases. Oncotarget., 7(19), 27764.
Elahi, R., Khosh, E., Tahmasebi, S., & Esmaeilzadeh, A. (2018). Immune cell hacking: Challenges and clinical approaches to create smarter generations of chimeric antigen receptor T cells. Frontiers in Immunology, 9. https://doi.org/10.3389/fimmu.2018.01717.
Junghans, R. P., Ma, Q., Rathore, R., Gomes, E. M., Bais, A. J., Lo, A. S., et al. (2016). Phase I trial of anti-PSMA designer CAR-T cells in prostate Cancer: Possible role for interacting interleukin 2-T cell pharmacodynamics as a determinant of clinical response. The Prostate., 76(14), 1257–1270.
Romero, D. (2018). Haematological cancer: Favourable outcomes with CAR T cells. Nature Reviews. Clinical Oncology, 15(2), 65.
Scarfò, I., & Maus, M. V. (2017). Current approaches to increase CAR T cell potency in solid tumors: Targeting the tumor microenvironment. Journal for Immunotherapy of Cancer., 5(1), 28.
Trédan, O., Galmarini, C. M., Patel, K., & Tannock, I. F. (2007). Drug resistance and the solid tumor microenvironment. Journal of the National Cancer Institute, 99(19), 1441–1454.
Frigault, M. J., Lee, J., Basil, M. C., Carpenito, C., Motohashi, S., Scholler, J., Kawalekar, O. U., Guedan, S., McGettigan, S. E., Posey, A. D., Ang, S., Cooper, L. J. N., Platt, J. M., Johnson, F. B., Paulos, C. M., Zhao, Y., Kalos, M., Milone, M. C., & June, C. H. (2015). Identification of chimeric antigen receptors that mediate constitutive or inducible proliferation of T cells. Cancer Immunology Research, 3, 356–367. https://doi.org/10.1158/2326-6066.CIR-14-0186.
Di, S., & Li, Z. (2016). Treatment of solid tumors with chimeric antigen receptor-engineered T cells: Current status and future prospects. Science China. Life Sciences, 59(4), 360–369.
Mirzaei, H. R., Rodriguez, A., Shepphird, J., Brown, C. E., & Badie, B. (2017). Chimeric antigen receptors T cell therapy in solid tumor: Challenges and clinical applications. Frontiers in Immunology, 8, 1850.
Lo, A., Wang, L.-C. S., Scholler, J., Monslow, J., Avery, D., Newick, K., O'Brien, S., Evans, R. A., Bajor, D. J., Clendenin, C., Durham, A. C., Buza, E. L., Vonderheide, R. H., June, C. H., Albelda, S. M., & Pure, E. (2015). Tumor-promoting desmoplasia is disrupted by depleting FAP-expressing stromal cells. Cancer Research, 75(14), 2800–2810.
Wang, L.-C. S., Lo, A., Scholler, J., Sun, J., Majumdar, R. S., Kapoor, V., Antzis, M., Cotner, C. E., Johnson, L. A., Durham, A. C., Solomides, C. C., June, C. H., Pure, E., & Albelda, S. M. (2014). Targeting fibroblast activation protein in tumor stroma with chimeric antigen receptor T cells can inhibit tumor growth and augment host immunity without severe toxicity. Cancer Immunology Research, 2(2), 154–166.
Caruana, I., Savoldo, B., Hoyos, V., Weber, G., Liu, H., Kim, E. S., Ittmann, M. M., Marchetti, D., & Dotti, G. (2015). Heparanase promotes tumor infiltration and antitumor activity of CAR-redirected T lymphocytes. Nature Medicine, 21(5), 524–529.
Nishio, N., & Dotti, G. (2015). Oncolytic virus expressing RANTES and IL-15 enhances function of CAR-modified T cells in solid tumors. Oncoimmunology., 4(2), e988098.
Koneru, M., O’Cearbhaill, R., Pendharkar, S., Spriggs, D. R., & Brentjens, R. J. (2015). A phase I clinical trial of adoptive T cell therapy using IL-12 secreting MUC-16 ecto directed chimeric antigen receptors for recurrent ovarian cancer. Journal of Translational Medicine, 13(1), 102.
Zhang, L., Yu, Z., Muranski, P., Palmer, D., Restifo, N., Rosenberg, S., et al. (2013). Inhibition of TGF-β signaling in genetically engineered tumor antigen-reactive T cells significantly enhances tumor treatment efficacy. Gene Therapy, 20(5), 575–580.
Mohammed, S., Sukumaran, S., Bajgain, P., Watanabe, N., Heslop, H. E., Rooney, C. M., Brenner, M. K., Fisher, W. E., Leen, A. M., & Vera, J. F. (2017). Improving chimeric antigen receptor-modified T cell function by reversing the immunosuppressive tumor microenvironment of pancreatic cancer. Molecular Therapy, 25(1), 249–258.
Adachi, K., Kano, Y., Nagai, T., Okuyama, N., Sakoda, Y., & Tamada, K. (2018). IL-7 and CCL19 expression in CAR-T cells improves immune cell infiltration and CAR-T cell survival in the tumor. Nature Biotechnology, 36(4), 346–351.
Arab, S., Kheshtchin, N., Ajami, M., Ashurpoor, M., Safvati, A., Namdar, A., Mirzaei, R., Mousavi Niri, N., Jadidi-Niaragh, F., Ghahremani, M. H., & Hadjati, J. (2017). Increased efficacy of a dendritic cell–based therapeutic cancer vaccine with adenosine receptor antagonist and CD73 inhibitor. Tumor Biology, 39(3), 1010428317695021.
Beavis, P. A., Milenkovski, N., Henderson, M. A., John, L. B., Allard, B., Loi, S., Kershaw, M. H., Stagg, J., & Darcy, P. K. (2015). Adenosine receptor 2A blockade increases the efficacy of anti–PD-1 through enhanced antitumor T-cell responses. Cancer Immunology Research, 3(5), 506–517.
Ligtenberg, M. A., Mougiakakos, D., Mukhopadhyay, M., Witt, K., Lladser, A., Chmielewski, M., Riet, T., Abken, H., & Kiessling, R. (2016). Coexpressed catalase protects chimeric antigen receptor–redirected T cells as well as bystander cells from oxidative stress–induced loss of antitumor activity. The Journal of Immunology., 196(2), 759–766.
Ninomiya, S., Narala, N., Huye, L., Yagyu, S., Savoldo, B., Dotti, G., Heslop, H. E., Brenner, M. K., Rooney, C. M., & Ramos, C. A. (2015). Tumor indoleamine 2, 3-dioxygenase (IDO) inhibits CD19-CAR T cells and is downregulated by lymphodepleting drugs. Blood., 125(25), 3905–3916.
Newick, K., O'Brien, S., Sun, J., Kapoor, V., Maceyko, S., Lo, A., Pure, E., Moon, E., & Albelda, S. M. (2016). Augmentation of CAR T-cell trafficking and antitumor efficacy by blocking protein kinase a localization. Cancer Immunology Research, 4(6), 541–551.
Scheffel, M. J., Scurti, G., Simms, P., Garrett-Mayer, E., Mehrotra, S., Nishimura, M. I., & Voelkel-Johnson, C. (2016). Efficacy of adoptive T-cell therapy is improved by treatment with the antioxidant N-acetyl cysteine, which limits activation-induced T-cell death. Cancer Research, 76(20), 6006–6016.
Peggs, K. S., Quezada, S. A., Chambers, C. A., Korman, A. J., & Allison, J. P. (2009). Blockade of CTLA-4 on both effector and regulatory T cell compartments contributes to the antitumor activity of anti–CTLA-4 antibodies. The Journal of Experimental Medicine, 206(8), 1717–1725.
Ren, J., Zhang, X., Liu, X., Fang, C., Jiang, S., June, C. H., et al. (2017). A versatile system for rapid multiplex genome-edited CAR T cell generation. Oncotarget., 8(10), 17002.
John, L. B., Devaud, C., Duong, C. P., Yong, C. S., Beavis, P. A., Haynes, N. M., et al. (2013). Anti-PD-1 antibody therapy potently enhances the eradication of established tumors by gene-modified T cells. Clinical Cancer Research, 19(20), 5636–5646.
Rupp, L. J., Schumann, K., Roybal, K. T., Gate, R. E., Chun, J. Y., Lim, W. A., et al. (2017). CRISPR/Cas9-mediated PD-1 disruption enhances anti-tumor efficacy of human chimeric antigen receptor T cells. Scientific Reports, 7(1), 737.
Liu, X., Ranganathan, R., Jiang, S., Fang, C., Sun, J., Kim, S., Newick, K., Lo, A., June, C. H., Zhao, Y., & Moon, E. K. (2016). A chimeric switch-receptor targeting PD1 augments the efficacy of second-generation CAR T cells in advanced solid tumors. Cancer Research, 76(6), 1578–1590.
Woo, S.-R., Turnis, M. E., Goldberg, M. V., Bankoti, J., Selby, M., Nirschl, C. J., Bettini, M. L., Gravano, D. M., Vogel, P., Liu, C. L., Tangsombatvisit, S., Grosso, J. F., Netto, G., Smeltzer, M. P., Chaux, A., Utz, P. J., Workman, C. J., Pardoll, D. M., Korman, A. J., Drake, C. G., & Vignali, D. A. A. (2012). Immune inhibitory molecules LAG-3 and PD-1 synergistically regulate T-cell function to promote tumoral immune escape. Cancer Research, 72(4), 917–927.
Yoon, D. H., Osborn, M. J., Tolar, J., & Kim, C. J. (2018). Incorporation of immune checkpoint blockade into chimeric antigen receptor T cells (CAR-Ts): Combination or built-in CAR-T. International Journal of Molecular Sciences, 19(2), 340.
Fourcade, J., Sun, Z., Pagliano, O., Guillaume, P., Luescher, I. F., Sander, C., et al. 2012).CD8+ T cells specific for tumor antigens can be rendered dysfunctional by the tumor microenvironment through upregulation of the inhibitory receptors BTLA and PD-1. Cancer Research. 2011:canres. 2637.011.
Beavis, P. A., Henderson, M. A., Giuffrida, L., Mills, J. K., Sek, K., Cross, R. S., Davenport, A. J., John, L. B., Mardiana, S., Slaney, C. Y., Johnstone, R. W., Trapani, J. A., Stagg, J., Loi, S., Kats, L., Gyorki, D., Kershaw, M. H., & Darcy, P. K. (2017). Targeting the adenosine 2A receptor enhances chimeric antigen receptor T cell efficacy. The Journal of Clinical Investigation., 127(3), 929–941.
Johnston, R. J., Comps-Agrar, L., Hackney, J., Yu, X., Huseni, M., Yang, Y., Park, S., Javinal, V., Chiu, H., Irving, B., Eaton, D. L., & Grogan, J. L. (2014). The immunoreceptor TIGIT regulates antitumor and antiviral CD8+ T cell effector function. Cancer Cell, 26(6), 923–937.
Kershaw, M. H., Wang, G., Westwood, J. A., Pachynski, R. K., Tiffany, H. L., Marincola, F. M., Wang, E., Young, H. A., Murphy, P. M., & Hwu, P. (2002). Redirecting migration of T cells to chemokine secreted from tumors by genetic modification with CXCR2. Human Gene Therapy, 13(16), 1971–1980.
Long, A. H., Highfill, S. L., Cui, Y., Smith, J. P., Walker, A. J., Ramakrishna, S., el-Etriby, R., Galli, S., Tsokos, M. G., Orentas, R. J., & Mackall, C. L. (2016). Reduction of MDSCs with all-trans retinoic acid improves CAR therapy efficacy for sarcomas. Cancer Immunology Research, 4(10), 869–880.
Zhou, Q., Munger, M. E., Highfill, S. L., Tolar, J., Weigel, B. J., Riddle, M., Sharpe, A. H., Vallera, D. A., Azuma, M., Levine, B. L., June, C. H., Murphy, W. J., Munn, D. H., & Blazar, B. R. (2010). Program death-1 signaling and regulatory T cells collaborate to resist the function of adoptively transferred cytotoxic T lymphocytes in advanced acute myeloid leukemia. Blood., 116(14), 2484–2493.
Markley, J. C., & Sadelain, M. (2010). IL-7 and IL-21 are superior to IL-2 and IL-15 in promoting human T cell–mediated rejection of systemic lymphoma in immunodeficient mice. Blood., 115(17), 3508–3519.
Yao, X., Ahmadzadeh, M., Lu, Y.-C., Liewehr, D. J., Dudley, M. E., Liu, F., Schrump, D. S., Steinberg, S. M., Rosenberg, S. A., & Robbins, P. F. (2012). Levels of peripheral CD4+ FoxP3+ regulatory T cells are negatively associated with clinical response to adoptive immunotherapy of human cancer. Blood., 119(24), 5688–5696.
Spear, P., Barber, A., Rynda-Apple, A., & Sentman, C. L. (2012). Chimeric antigen receptor T cells shape myeloid cell function within the tumor microenvironment through IFN-gamma and GM-CSF. Journal of Immunology (Baltimore, Md. : 1950), 188(12), 6389–6398.
Chmielewski, M., & Abken, H. (2017). CAR T cells releasing IL-18 convert to T-bet high FoxO1 low effectors that exhibit augmented activity against advanced solid tumors. Cell Reports, 21(11), 3205–3219.
Marofi, F., Vahedi, G., Biglari, A., Esmaeilzadeh, A., & Athari, S. S. (2017). Mesenchymal stromal/stem cells: A new era in the cell-based targeted gene therapy of cancer. Frontiers in Immunology, 8, 1770.
Bhowmick, N. A., Neilson, E. G., & Moses, H. L. (2004). Stromal fibroblasts in cancer initiation and progression. Nature., 432(7015), 332–337.
Kakarla, S., Chow, K. K., Mata, M., Shaffer, D. R., Song, X.-T., Wu, M.-F., et al. (2013). Antitumor effects of chimeric receptor engineered human T cells directed to tumor stroma. Molecular Therapy, 21(8), 1611–1620.
Vlodavsky, I., Elkin, M., & Ilan, N. (2011). Impact of heparanase and the tumor microenvironment on cancer metastasis and angiogenesis: Basic aspects and clinical applications. Rambam Maimonides Medical Journal., 2(1). https://doi.org/10.5041/RMMJ.10019.
Arvatz, G., Weissmann, M., Ilan, N., & Vlodavsky, I. (2016). Heparanase and cancer progression: New directions, new promises. Human Vaccines & Immunotherapeutics, 12(9), 2253–2256.
Bollard, C. M., Rössig, C., Calonge, M. J., Huls, M. H., Wagner, H.-J., Massague, J., Brenner, M. K., Heslop, H. E., & Rooney, C. M. (2002). Adapting a transforming growth factor β–related tumor protection strategy to enhance antitumor immunity. Blood., 99(9), 3179–3187.
Piri, Z., Esmaeilzadeh, A., & Hajikhanmirzaei, M. (2012). Interleukin-25 as a candidate gene in immunogene therapy of pancreatic cancer. Journal of Medical Hypotheses and Ideas., 6(2), 75–79.
Mirzaei, M. H., & Esmaeilzadeh, A. (2014). Overexpression of MDA-7/IL-24 as an anticancer cytokine in gene therapy of thyroid carcinoma. Journal of Medical Hypotheses and Ideas., 8(1), 7–13.
Esmaeilzadeh, A., Ebtekar, M., Biglari, A., & Saraf, S. (2014). Anti-proliferative effect of rmIL-27 protein on 4T1 mouse breast cancer cells as a candidate for cancer immunotherapy. ZUMS Journal., 22(91), 52–60.
Zhang, C., Liu, J., Zhong, J. F., & Zhang, X. (2017). Engineering CAR-T cells. Biomarker Research, 5(1), 22.
Hinrichs, C. S., Spolski, R., Paulos, C. M., Gattinoni, L., Kerstann, K. W., Palmer, D. C., Klebanoff, C. A., Rosenberg, S. A., Leonard, W. J., & Restifo, N. P. (2008). IL-2 and IL-21 confer opposing differentiation programs to CD8+ T cells for adoptive immunotherapy. Blood., 111(11), 5326–5333.
Zhang, E., Gu, J., & Xu, H. (2018). Prospects for chimeric antigen receptor-modified T cell therapy for solid tumors. Molecular Cancer, 17(1), 7.
Zhang, Y., & Ertl, H. C. (2016). Starved and asphyxiated: How can CD8+ T cells within a tumor microenvironment prevent tumor progression. Frontiers in Immunology, 7, 32. https://doi.org/10.3389/fimmu.2016.00032.
Maybin, J. A., Murray, A. A., Saunders, P. T., Hirani, N., Carmeliet, P., & Critchley, H. O. (2018). Hypoxia and hypoxia inducible factor-1α are required for normal endometrial repair during menstruation. Nature Communications, 9(1), 295.
Juillerat, A., Marechal, A., Filhol, J. M., Valogne, Y., Valton, J., Duclert, A., Duchateau, P., & Poirot, L. (2017). An oxygen sensitive self-decision making engineered CAR T-cell. Scientific Reports, 7, 39833.
Jadidi-Niaragh, F., Atyabi, F., Rastegari, A., Kheshtchin, N., Arab, S., Hassannia, H., Ajami, M., Mirsanei, Z., Habibi, S., Masoumi, F., Noorbakhsh, F., Shokri, F., & Hadjati, J. (2017). CD73 specific siRNA loaded chitosan lactate nanoparticles potentiate the antitumor effect of a dendritic cell vaccine in 4T1 breast cancer bearing mice. Journal of Controlled Release, 246, 46–59.
Junghans, R. P. (2017). The challenges of solid tumor for designer CAR-T therapies: A 25-years perspective. Nature Publishing Group. https://doi.org/10.1038/cgt.2016.82.
Solinas, G., Schiarea, S., Liguori, M., Fabbri, M., Pesce, S., Zammataro, L., Pasqualini, F., Nebuloni, M., Chiabrando, C., Mantovani, A., & Allavena, P. (2010). Tumor-conditioned macrophages secrete migration-stimulating factor: A new marker for M2-polarization, influencing tumor cell motility. The Journal of Immunology., 185(1), 642–652.
Condeelis, J., & Pollard, J. W. (2006). Macrophages: Obligate partners for tumor cell migration, invasion, and metastasis. Cell., 124(2), 263–266.
Sharma, P., & Allison, J. P. (2015). Immune checkpoint targeting in cancer therapy: Toward combination strategies with curative potential. Cell., 161(2), 205–214.
Jin, C., Yu, D., & Essand, M. (2016). Prospects to improve chimeric antigen receptor T-cell therapy for solid tumors. Future Medicine, 8, 1355–1361. https://doi.org/10.2217/imt-2016-0125.
Kumar, V., Patel, S., Tcyganov, E., & Gabrilovich, D. I. (2016). The nature of myeloid-derived suppressor cells in the tumor microenvironment. Trends in Immunology, 37(3), 208–220.
Chinen, T., Kannan, A. K., Levine, A. G., Fan, X., Klein, U., Zheng, Y., Gasteiger, G., Feng, Y., Fontenot, J. D., & Rudensky, A. Y. (2016). An essential role for the IL-2 receptor in T reg cell function. Nature Immunology, 17(11), 1322–1333.
Janco, J. M. T., Lamichhane, P., Karyampudi, L., & Knutson, K. L. (2015). Tumor-infiltrating dendritic cells in cancer pathogenesis. The Journal of Immunology., 194(7), 2985–2991.
Hurt, B., Schulick, R., Edil, B., El Kasmi, K. C., & Barnett, C. (2017). Cancer-promoting mechanisms of tumor-associated neutrophils. The American Journal of Surgery., 214(5), 938–944.
van den Broek, T., Borghans, J. A., & van Wijk, F. (2018). The full spectrum of human naive T cells. Nature Reviews. Immunology, 18, 1–373. https://doi.org/10.1038/s41577-018-0001-y.
Topalian, S. L., Drake, C. G., & Pardoll, D. M. (2015). Immune checkpoint blockade: A common denominator approach to cancer therapy. Cancer Cell, 27(4), 450–461.
Postow, M. A., Callahan, M. K., & Wolchok, J. D. (2015). Immune checkpoint blockade in cancer therapy. Journal of Clinical Oncology, 33(17), 1974–1982.
Rotte, A., Jin, J., & Lemaire, V. (2017). Mechanistic overview of immune checkpoints to support the rational design of their combinations in cancer immunotherapy. Annals of Oncology, 29(1), 71–83.
Linsley, P. S., Greene, J. L., Brady, W., Bajorath, J., Ledbetter, J. A., & Peach, R. (1994). Human B7-1 (CD80) and B7-2 (CD86) bind with similar avidities but distinct kinetics to CD28 and CTLA-4 receptors. Immunity., 1(9), 793–801.
Parry, R. V., Chemnitz, J. M., Frauwirth, K. A., Lanfranco, A. R., Braunstein, I., Kobayashi, S. V., Linsley, P. S., Thompson, C. B., & Riley, J. L. (2005). CTLA-4 and PD-1 receptors inhibit T-cell activation by distinct mechanisms. Molecular and Cellular Biology, 25(21), 9543–9553.
Wing, K., Onishi, Y., Prieto-Martin, P., Yamaguchi, T., Miyara, M., Fehervari, Z., Nomura, T., & Sakaguchi, S. (2008). CTLA-4 control over Foxp3+ regulatory T cell function. Science., 322(5899), 271–275.
Ishida, Y., Agata, Y., Shibahara, K., & Honjo, T. (1992). Induced expression of PD-1, a novel member of the immunoglobulin gene superfamily, upon programmed cell death. The EMBO Journal., 11(11), 3887–3895.
Francisco, L. M., Salinas, V. H., Brown, K. E., Vanguri, V. K., Freeman, G. J., Kuchroo, V. K., & Sharpe, A. H. (2009). PD-L1 regulates the development, maintenance, and function of induced regulatory T cells. The Journal of Experimental Medicine, 206(13), 3015–3029.
Fife, B. T., Pauken, K. E., Eagar, T. N., Obu, T., Wu, J., Tang, Q., Azuma, M., Krummel, M. F., & Bluestone, J. A. (2009). Interactions between PD-1 and PD-L1 promote tolerance by blocking the TCR–induced stop signal. Nature Immunology, 10(11), 1185–1192.
Wang, X., Teng, F., Kong, L., & Yu, J. (2016). PD-L1 expression in human cancers and its association with clinical outcomes. OncoTargets and Therapy., 9, 5023.
Chen, N., Morello, A., Tano, Z., & Adusumilli, P. S. (2017). CAR T-cell intrinsic PD-1 checkpoint blockade: A two-in-one approach for solid tumor immunotherapy. Oncoimmunology., 6(2), e1273302.
Triebel, F., Jitsukawa, S., Baixeras, E., Roman-Roman, S., Genevee, C., Viegas-Pequignot, E., & Hercend, T. (1990). LAG-3, a novel lymphocyte activation gene closely related to CD4. The Journal of Experimental Medicine, 171(5), 1393–1405.
Huard, B., Prigent, P., Tournier, M., Bruniquel, D., & Triebel, F. (1995). CD4/major histocompatibility complex class II interaction analyzed with CD4-and lymphocyte activation gene-3 (LAG-3)-Ig fusion proteins. European Journal of Immunology, 25(9), 2718–2721.
Xu, F., Liu, J., Liu, D., Liu, B., Wang, M., Hu, Z., du, X., Tang, L., & He, F. (2014). LSECtin expressed on melanoma cells promotes tumor progression by inhibiting antitumor T-cell responses. Cancer Research, 74(13), 3418–3428.
Blackburn, S. D., Shin, H., Haining, W. N., Zou, T., Workman, C. J., Polley, A., Betts, M. R., Freeman, G. J., Vignali, D. A. A., & Wherry, E. J. (2009). Coregulation of CD8+ T cell exhaustion by multiple inhibitory receptors during chronic viral infection. Nature Immunology, 10(1), 29–37.
Zhang, Y., Zhang, X., Cheng, C., Mu, W., Liu, X., Li, N., Wei, X., Liu, X., Xia, C., & Wang, H. (2017). CRISPR-Cas9 mediated LAG-3 disruption in CAR-T cells. Frontiers of Medicine., 11(4), 554–562.
Prigent, P., El mir, S., Dreano, M., & Triebel, F. (1999). Lymphocyte activation gene-3 induces tumor regression and antitumor immune responses. European Journal of Immunology, 29(12), 3867–3876.
Monney, L., Sabatos, C. A., Gaglia, J. L., Ryu, A., Waldner, H., Chernova, T., Manning, S., Greenfield, E. A., Coyle, A. J., Sobel, R. A., Freeman, G. J., & Kuchroo, V. K. (2002). Th1-specific cell surface protein Tim-3 regulates macrophage activation and severity of an autoimmune disease. Nature., 415(6871), 536–541.
Dardalhon, V., Anderson, A. C., Karman, J., Apetoh, L., Chandwaskar, R., Lee, D. H., Cornejo, M., Nishi, N., Yamauchi, A., Quintana, F. J., Sobel, R. A., Hirashima, M., & Kuchroo, V. K. (2010). Tim-3/galectin-9 pathway: Regulation of Th1 immunity through promotion of CD11b+ Ly-6G+ myeloid cells. The Journal of Immunology., 185(3), 1383–1392.
Baitsch, L., Legat, A., Barba, L., Marraco, S. A. F., Rivals, J.-P., Baumgaertner, P., et al. (2012). Extended co-expression of inhibitory receptors by human CD8 T-cells depending on differentiation, antigen-specificity and anatomical localization. PLoS One, 7(2), e30852.
Pasero, C., Speiser, D. E., Derre, L., & Olive, D. (2012). The HVEM network: New directions in targeting novel costimulatory/co-inhibitory molecules for cancer therapy. Current Opinion in Pharmacology, 12(4), 478–485.
Derré, L., Rivals, J.-P., Jandus, C., Pastor, S., Rimoldi, D., Romero, P., Michielin, O., Olive, D., & Speiser, D. E. (2010). BTLA mediates inhibition of human tumor-specific CD8+ T cells that can be partially reversed by vaccination. The Journal of Clinical Investigation., 120(1), 157–167.
Stanietsky, N., Simic, H., Arapovic, J., Toporik, A., Levy, O., Novik, A., Levine, Z., Beiman, M., Dassa, L., Achdout, H., Stern-Ginossar, N., Tsukerman, P., Jonjic, S., & Mandelboim, O. (2009). The interaction of TIGIT with PVR and PVRL2 inhibits human NK cell cytotoxicity. Proceedings of the National Academy of Sciences, 106(42), 17858–17863.
Yu, X., Harden, K., Gonzalez, L. C., Francesco, M., Chiang, E., Irving, B., et al. (2009). The surface protein TIGIT suppresses T cell activation by promoting the generation of mature immunoregulatory dendritic cells. Nature Immunology, 10(1), 48–57.
Joller, N., Lozano, E., Burkett, P. R., Patel, B., Xiao, S., Zhu, C., Xia, J., Tan, T. G., Sefik, E., Yajnik, V., Sharpe, A. H., Quintana, F. J., Mathis, D., Benoist, C., Hafler, D. A., & Kuchroo, V. K. (2014). Treg cells expressing the coinhibitory molecule TIGIT selectively inhibit proinflammatory Th1 and Th17 cell responses. Immunity., 40(4), 569–581.
Levine, D. A., & Network, C. G. A. R. (2013). Integrated genomic characterization of endometrial carcinoma. Nature., 497(7447), 67–73.
Network, C. G. A. R. (2012). Comprehensive genomic characterization of squamous cell lung cancers. Nature., 489(7417), 519.
Network, C. G. A. (2012). Comprehensive molecular characterization of human colon and rectal cancer. Nature., 487(7407), 330–337.
Network, C. G. A. (2012). Comprehensive molecular portraits of human breast tumours. Nature., 490(7418), 61–70.
Network, C. G. A. R. (2013). Comprehensive molecular characterization of clear cell renal cell carcinoma. Nature., 499(7456), 43.
Casado, J. G., Pawelec, G., Morgado, S., Sanchez-Correa, B., Delgado, E., Gayoso, I., Duran, E., Solana, R., & Tarazona, R. (2009). Expression of adhesion molecules and ligands for activating and costimulatory receptors involved in cell-mediated cytotoxicity in a large panel of human melanoma cell lines. Cancer Immunology, Immunotherapy, 58(9), 1517–1526.
Ohta, A., Gorelik, E., Prasad, S. J., Ronchese, F., Lukashev, D., Wong, M. K., et al. (2006). A2A adenosine receptor protects tumors from antitumor T cells. Proceedings of the National Academy of Sciences, 103(35), 13132–13137.
Ohta, A. (2016). A metabolic immune checkpoint: Adenosine in tumor microenvironment. Frontiers in Immunology, 7, 109.
Kmiecik, J., Poli, A., Brons, N. H., Waha, A., Eide, G. E., Enger, P. Ø., et al. (2013). Elevated CD3+ and CD8+ tumor-infiltrating immune cells correlate with prolonged survival in glioblastoma patients despite integrated immunosuppressive mechanisms in the tumor microenvironment and at the systemic level. Journal of Neuroimmunology, 264(1), 71–83.
Peng, W., Ye, Y., Rabinovich, B. A., Liu, C., Lou, Y., Zhang, M., et al. (2010). Transduction of tumor-specific T cells with CXCR2 chemokine receptor improves migration to tumor and antitumor immune responses. Clinical Cancer Research 1078–0432. CCR-10-712.
Spear, P., Barber, A., & Sentman, C. L. (2013). Collaboration of chimeric antigen receptor (CAR)-expressing T cells and host T cells for optimal elimination of established ovarian tumors. Oncoimmunology., 2(4), e23564.
Chinnasamy, D., Yu, Z., Theoret, M. R., Zhao, Y., Shrimali, R. K., Morgan, R. A., Feldman, S. A., Restifo, N. P., & Rosenberg, S. A. (2010). Gene therapy using genetically modified lymphocytes targeting VEGFR-2 inhibits the growth of vascularized syngenic tumors in mice. The Journal of Clinical Investigation., 120(11), 3953–3968.
Adusumilli, P. S., Cherkassky, L., Villena-Vargas, J., Colovos, C., Servais, E., Plotkin, J., Jones, D. R., & Sadelain, M. (2014). Regional delivery of mesothelin-targeted CAR T cell therapy generates potent and long-lasting CD4-dependent tumor immunity. Science Translational Medicine, 6(261), 261ra151–261ra151.
Watford, W. T., Moriguchi, M., Morinobu, A., & O’Shea, J. J. (2003). The biology of IL-12: Coordinating innate and adaptive immune responses. Cytokine & Growth Factor Reviews, 14(5), 361–368.
Kreso, A., & Dick, J. E. (2014). Evolution of the cancer stem cell model. Cell Stem Cell, 14(3), 275–291.
Petrov, J. C., Wada, M., Pinz, K. G., Yan, L. E., Chen, K. H., Shuai, X., Liu, H., Chen, X., Leung, L. H., Salman, H., Hagag, N., Liu, F., Jiang, X., & Ma, Y. (2018). Compound CAR T-cells as a double-pronged approach for treating acute myeloid leukemia. Leukemia., 32, 1–1326. https://doi.org/10.1038/s41375-018-0075-3.
Kershaw, M. H., Westwood, J. A., Parker, L. L., Wang, G., Eshhar, Z., Mavroukakis, S. A., White, D. E., Wunderlich, J. R., Canevari, S., Rogers-Freezer, L., Chen, C. C., Yang, J. C., Rosenberg, S. A., & Hwu, P. (2006). A phase I study on adoptive immunotherapy using gene-modified T cells for ovarian cancer. Clinical Cancer Research, 12(20), 6106–6115.
Park, J. R., DiGiusto, D. L., Slovak, M., Wright, C., Naranjo, A., Wagner, J., et al. (2007). Adoptive transfer of chimeric antigen receptor re-directed cytolytic T lymphocyte clones in patients with neuroblastoma. Molecular Therapy, 15(4), 825–833.
Morgan, R. A., Yang, J. C., Kitano, M., Dudley, M. E., Laurencot, C. M., & Rosenberg, S. A. (2010). Case report of a serious adverse event following the administration of T cells transduced with a chimeric antigen receptor recognizing ERBB2. Molecular Therapy, 18(4), 843–851.
Maus, M. V., Haas, A. R., Beatty, G. L., Albelda, S. M., Levine, B. L., Liu, X., Zhao, Y., Kalos, M., & June, C. H. (2013). T cells expressing chimeric antigen receptors can cause anaphylaxis in humans. Cancer Immunology Research, 1(1), 26–31.
Ahmed, N., Brawley, V. S., Hegde, M., Robertson, C., Ghazi, A., Gerken, C., Liu, E., Dakhova, O., Ashoori, A., Corder, A., Gray, T., Wu, M. F., Liu, H., Hicks, J., Rainusso, N., Dotti, G., Mei, Z., Grilley, B., Gee, A., Rooney, C. M., Brenner, M. K., Heslop, H. E., Wels, W. S., Wang, L. L., Anderson, P., & Gottschalk, S. (2015). Human epidermal growth factor receptor 2 (HER2)–specific chimeric antigen receptor–modified T cells for the immunotherapy of HER2-positive sarcoma. Journal of Clinical Oncology, 33(15), 1688–1696.
Lamers, C. H., Klaver, Y., Gratama, J. W., Sleijfer, S., & Debets, R. (2016). Treatment of metastatic renal cell carcinoma (mRCC) with CAIX CAR-engineered T-cells–a completed study overview. Biochemical Society Transactions, 44(3), 951–959.
Hege, K. M., Bergsland, E. K., Fisher, G. A., Nemunaitis, J. J., Warren, R. S., McArthur, J. G., et al. (2017). Safety, tumor trafficking and immunogenicity of chimeric antigen receptor (CAR)-T cells specific for TAG-72 in colorectal cancer. Journal for Immunotherapy of Cancer., 5(1), 22.
Ahmed, N., Brawley, V., Hegde, M., Bielamowicz, K., Kalra, M., Landi, D., Robertson, C., Gray, T. L., Diouf, O., Wakefield, A., Ghazi, A., Gerken, C., Yi, Z., Ashoori, A., Wu, M. F., Liu, H., Rooney, C., Dotti, G., Gee, A., Su, J., Kew, Y., Baskin, D., Zhang, Y. J., New, P., Grilley, B., Stojakovic, M., Hicks, J., Powell, S. Z., Brenner, M. K., Heslop, H. E., Grossman, R., Wels, W. S., & Gottschalk, S. (2017). HER2-specific chimeric antigen receptor–modified virus-specific T cells for progressive glioblastoma: A phase 1 dose-escalation trial. JAMA Oncology, 3(8), 1094–1101.
Feng, K., Liu, Y., Guo, Y., Qiu, J., Wu, Z., Dai, H., et al. (2018). Phase I study of chimeric antigen receptor modified T cells in treating HER2-positive advanced biliary tract cancers and pancreatic cancers. Protein & Cell, 2017, 1–10. https://doi.org/10.1007/s13238-017-0440-4.
Zhang, H., Ye, Z.-l., Z-g, Y., Z-q, L., & H-j, J. (2016). New strategies for the treatment of solid tumors with CAR-T cells. International Journal of Biological Sciences, 12(6), 718–729.
Newick, K., O'Brien, S., Moon, E., & Albelda, S. M. (2017). CAR T cell therapy for solid tumors. Annual Review of Medicine, 68, 139–152.
Brown, C. E., Badie, B., Barish, M. E., Weng, L., Ostberg, J. R., Chang, W.-C., Naranjo, A., Starr, R., Wagner, J., Wright, C., Zhai, Y., Bading, J. R., Ressler, J. A., Portnow, J., D'Apuzzo, M., Forman, S. J., & Jensen, M. C. (2015). Bioactivity and safety of IL13Rα2-redirected chimeric antigen receptor CD8+ T cells in patients with recurrent glioblastoma. Clinical Cancer Research, 21(18), 4062–4072.
Charlesworth, C. T., Deshpande, P. S., Dever, D. P., Dejene, B., Gomez-Ospina, N., Mantri, S., et al. (2018). Identification of pre-existing adaptive immunity to Cas9 proteins in humans. Biorxiv., 243345.
Wu, C.-Y., Roybal, K. T., Puchner, E. M., Onuffer, J., & Lim, W. A. (2015). Remote control of therapeutic T cells through a small molecule–gated chimeric receptor. Science., 350(6258), aab4077.
Tamada, K., Geng, D., Sakoda, Y., Bansal, N., Srivastava, R., & Li, Z. (2013). Redirecting gene-modified T cells toward various Cancer types using tagged antibodies (vol 18, pg 6436, 2012). Clinical Cancer Research, 19(4), 951.
Urbanska, K., Lanitis, E., Poussin, M., Lynn, R. C., Gavin, B. P., Kelderman, S. et al. (2012). A universal strategy for adoptive immunotherapy of cancer through use of a novel T cell antigen receptor. Cancer Research. 3890.2011. https://doi.org/10.1158/0008-5472.
Liu, L., Sun, M., & Wang, Z. (2012). Adoptive T-cell therapy of B-cell malignancies: Conventional and physiological chimeric antigen receptors. Cancer Letters, 316(1), 1–5.
Kahlon, K. S., Brown, C., Cooper, L. J., Raubitschek, A., Forman, S. J., & Jensen, M. C. (2004). Specific recognition and killing of glioblastoma multiforme by interleukin 13-zetakine redirected cytolytic T cells. Cancer Research, 64(24), 9160–9166.
Shaffer, D. R., Savoldo, B., Yi, Z., Chow, K. K., Kakarla, S., Spencer, D., et al. (2011:blood-2010-04-278218). T cells redirected against CD70 for the immunotherapy of CD70-positive malignancies. Blood., 117, 4304–4314.
Niederman, T. M., Ghogawala, Z., Carter, B. S., Tompkins, H. S., Russell, M. M., & Mulligan, R. C. (2002). Antitumor activity of cytotoxic T lymphocytes engineered to target vascular endothelial growth factor receptors. Proceedings of the National Academy of Sciences, 99(10), 7009–7014.
Muniappan, A., Banapour, B., Lebkowski, J., & Talib, S. (2000). Ligand-mediated cytolysis of tumor cells: Use of heregulin-ζ chimeras to redirect cytotoxic T lymphocytes. Cancer Gene Therapy, 7(1), 128–134.
Zhang, T., Barber, A., & Sentman, C. L. (2006). Generation of antitumor responses by genetic modification of primary human T cells with a chimeric NKG2D receptor. Cancer Research, 66(11), 5927–5933.
Zhang, T., Wu, M.-R., & Sentman, C. L. (2012). An NKp30-based chimeric antigen receptor promotes T cell effector functions and antitumor efficacy in vivo. The Journal of Immunology., 1103495.
Cho, J. H., Collins, J. J., & Wong, W. W. (2018). Universal chimeric antigen receptors for multiplexed and logical control of T cell responses. Cell., 173, 1426–1438.e11. https://doi.org/10.1016/j.cell.2018.03.038.
Zhao, J., Lin, Q., Song, Y., & Liu, D. (2018). Universal CARs, universal T cells, and universal CAR T cells. Journal of Hematology & Oncology, 11(1), 132.
Grada, Z., Hegde, M., Byrd, T., Shaffer, D. R., Ghazi, A., Brawley, V. S., Corder, A., Schönfeld, K., Koch, J., Dotti, G., Heslop, H. E., Gottschalk, S., Wels, W. S., Baker, M. L., & Ahmed, N. (2013). TanCAR: A novel bispecific chimeric antigen receptor for cancer immunotherapy. Molecular Therapy--Nucleic Acids, 2, e105. https://doi.org/10.1038/mtna.2013.32.
Hegde, M., Grada, Z., Pignata, A., Wakefield, A., Fousek, K., Bielamowicz, K., Chow, K., Brawley, V., Byrd, T., Gottschalk, S., Mukherjee, M., Wels, W. S., Baker, M., Dotti, G., Orange, J., & Ahmed, N. (2015). A bispecific chimeric antigen receptor molecule enhances T cell activation through dual immunological synapse formation and offsets antigen escape in glioblastoma. Journal for Immunotherapy of Cancer., 3(S2), O3.
Lanitis, E., Poussin, M., Klattenhoff, A. W., Song, D., Sandaltzopoulos, R., June, C. H., & Powell, D. J. (2013). Chimeric antigen receptor T cells with dissociated signaling domains exhibit focused antitumor activity with reduced potential for toxicity in vivo. Cancer Immunology Research, 1, 43–53. https://doi.org/10.1158/2326-6066.CIR-13-0008.
Wilkie, S., van Schalkwyk, M. C., Hobbs, S., Davies, D. M., van der Stegen, S. J., Pereira, A. C. P., et al. (2012). Dual targeting of ErbB2 and MUC1 in breast cancer using chimeric antigen receptors engineered to provide complementary signaling. Journal of Clinical Immunology, 32(5), 1059–1070.
Trapani, J. A., Sutton, V. R., Thia, K. Y., Li, Y. Q., Froelich, C. J., Jans, D. A., et al. (2003). A clathrin/dynamin-and mannose-6-phosphate receptor–independent pathway for granzyme B–induced cell death. The Journal of Cell Biology., 160(2), 223–233.
Senovilla, L., Vitale, I., Martins, I., Tailler, M., Pailleret, C., Michaud, M., Galluzzi, L., Adjemian, S., Kepp, O., Niso-Santano, M., Shen, S., Marino, G., Criollo, A., Boileve, A., Job, B., Ladoire, S., Ghiringhelli, F., Sistigu, A., Yamazaki, T., Rello-Varona, S., Locher, C., Poirier-Colame, V., Talbot, M., Valent, A., Berardinelli, F., Antoccia, A., Ciccosanti, F., Fimia, G. M., Piacentini, M., Fueyo, A., Messina, N. L., Li, M., Chan, C. J., Sigl, V., Pourcher, G., Ruckenstuhl, C., Carmona-Gutierrez, D., Lazar, V., Penninger, J. M., Madeo, F., Lopez-Otin, C., Smyth, M. J., Zitvogel, L., Castedo, M., & Kroemer, G. (2012). An immunosurveillance mechanism controls cancer cell ploidy. Science., 337(6102), 1678–1684.
Martins, I., Tesniere, A., Kepp, O., Michaud, M., Schlemmer, F., Senovilla, L., Séror, C., Métivier, D., Perfettini, J. L., Zitvogel, L., & Kroemer, G. (2009). Chemotherapy induces ATP release from tumor cells. Cell Cycle, 8(22), 3723–3728.
Heylmann, D., Bauer, M., Becker, H., Van Gool, S., Bacher, N., Steinbrink, K., et al. (2013). Human CD4+ CD25+ regulatory T cells are sensitive to low dose cyclophosphamide: Implications for the immune response. PLoS One, 8(12), e83384.
Matsumura, S., Wang, B., Kawashima, N., Braunstein, S., Badura, M., Cameron TO, et al. (2008). Radiation-induced CXCL16 release by breast cancer cells attracts effector T cells. The Journal of Immunology., 181(5), 3099–3107.
Ganss, R., Ryschich, E., Klar, E., Arnold, B., & Hämmerling, G. J. (2002). Combination of T-cell therapy and trigger of inflammation induces remodeling of the vasculature and tumor eradication. Cancer Research, 62(5), 1462–1470.
Apetoh, L., Ghiringhelli, F., Tesniere, A., Obeid, M., Ortiz, C., Criollo, A., Mignot, G., Maiuri, M. C., Ullrich, E., Saulnier, P., Yang, H., Amigorena, S., Ryffel, B., Barrat, F. J., Saftig, P., Levi, F., Lidereau, R., Nogues, C., Mira, J. P., Chompret, A., Joulin, V., Clavel-Chapelon, F., Bourhis, J., André, F., Delaloge, S., Tursz, T., Kroemer, G., & Zitvogel, L. (2007). Toll-like receptor 4–dependent contribution of the immune system to anticancer chemotherapy and radiotherapy. Nature Medicine, 13(9), 1050–1059.
Aranda, F., Buqué, A., Bloy, N., Castoldi, F., Eggermont, A., Cremer, I., Fridman, W. H., Fucikova, J., Galon, J., Spisek, R., Tartour, E., Zitvogel, L., Kroemer, G., & Galluzzi, L. (2015). Trial watch: Adoptive cell transfer for oncological indications. Oncoimmunology., 4(11), e1046673.
Vanneman, M., & Dranoff, G. (2012). Combining immunotherapy and targeted therapies in cancer treatment. Nature Reviews. Cancer, 12(4), 237–251.
Ozao-Choy, J., Ma, G., Kao, J., Wang, G. X., Meseck, M., Sung, M., Schwartz, M., Divino, C. M., Pan, P. Y., & Chen, S. H. (2009). The novel role of tyrosine kinase inhibitor in the reversal of immune suppression and modulation of tumor microenvironment for immune-based cancer therapies. Cancer Research, 69, 2514–2522. https://doi.org/10.1158/0008-5472.CAN-08-4709.
Nishio, N., Diaconu, I., Liu, H., Cerullo, V., Caruana, I., Hoyos, V., Bouchier-Hayes, L., Savoldo, B., & Dotti, G. (2014). Armed oncolytic virus enhances immune functions of chimeric antigen receptor–modified T cells in solid tumors. Cancer Research, 74, 5195–5205.
Di Stasi, A., De Angelis, B., Rooney, C. M., Zhang, L., Mahendravada, A., Foster, A. E., et al. (2009). T lymphocytes coexpressing CCR4 and a chimeric antigen receptor targeting CD30 have improved homing and antitumor activity in a Hodgkin tumor model. Blood., 113(25), 6392–6402.
Brown, C. E., Alizadeh, D., Starr, R., Weng, L., Wagner, J. R., Naranjo, A., Ostberg, J. R., Blanchard, M. S., Kilpatrick, J., Simpson, J., Kurien, A., Priceman, S. J., Wang, X., Harshbarger, T. L., D’Apuzzo, M., Ressler, J. A., Jensen, M. C., Barish, M. E., Chen, M., Portnow, J., Forman, S. J., & Badie, B. (2016). Regression of glioblastoma after chimeric antigen receptor T-cell therapy. The New England Journal of Medicine, 375(26), 2561–2569.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
ST and RE contributed to data gathering, writing the primary draft of the manuscript, and designing figures and Tables. AE contributed to the hypothesis, corresponding, scientific and structural editing, and verifying the manuscript before submission.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tahmasebi, S., Elahi, R. & Esmaeilzadeh, A. Solid Tumors Challenges and New Insights of CAR T Cell Engineering. Stem Cell Rev and Rep 15, 619–636 (2019). https://doi.org/10.1007/s12015-019-09901-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12015-019-09901-7