Abstract
Background
Mesenchymal stromal cells (MSCs) and endothelial progenitor cells (EPCs) are used in cell-based regenerative therapy. HMG CoA reductase inhibitors (statins) appear promising in blocking apoptosis, prolonging progenitor cell survival and improving their capacity to repair organ function.
Methods
We performed a systematic review of preclinical and clinical studies to clarify whether statins can improve cell-based repair of organ injury. MEDLINE, EMBASE, and PUBMED databases were searched (1947 to June 25, 2013). Controlled clinical and pre-clinical studies were included that evaluated statin therapy used alone or in combination with MSCs or EPCs in patients or animals with organ injury.
Results
After screening 771 citations, 100 records underwent full eligibility screening of which 38 studies met eligibility and were included in the review: Studies were grouped into pre-clinical studies that involved statin treatment in combination with cell therapy (18 studies), preclinical studies of statin therapy alone (13 studies) and clinical studies of statin therapy (7 studies). Studies addressed cardiac injury (14 studies), vascular disorders (15 studies), neurologic conditions (8 studies) and bone fractures (1 study). Pre-clinical studies of statins in combination with MSC infusion (15 studies) or EPC therapy (3 studies) were described and despite marked heterogeneity in reporting outcomes of cellular analysis and organ function, all of these cell-based pre-clinical studies reported improved organ recovery with the addition of statin therapy. Moreover, 13 pre-clinical studies involved the administration of a statin drug alone to animals. An increase in EPC number and/or function (no studies of MSCs) was reported in 11 of these studies (85 %) and improved organ function in 12 studies (92 %). We also identified 7 clinical studies and none involved the administration of cells but described an increased number and/or function of EPCs (no studies of MSCs) and improved organ function with statin therapy (1.2-fold to 35-fold improvement over controls) in all 7 studies.
Conclusion
Our systematic review provides a foundation of encouraging results that support further study of statins in regenerative therapy to augment the number and/or function of MSCs used in cell-based repair and to augment the number and function of EPCs in vivo to repair damaged tissues. Larger studies are needed to ensure safety and confirm clinical benefits.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
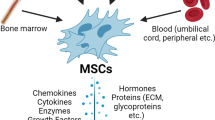
Regenerative cell-based therapy is an emerging field with increasing global activity and investment [1]. Two principal classes of progenitor cells used in cell-based regenerative therapy are mesenchymal stromal cells (MSCs) and vascular endothelial-like progenitor cells (EPCs). MSCs are adult stromal cells that can be isolated and expanded from bone marrow or adipose tissue and have the ability to differentiate into adipocytes, osteoblasts, and chondroblasts in vitro [2]. They sense hypoxia in damaged tissues and migrate to sites of injury, recruit other cells to initiate the repair process, reduce inflammation and mitigate maladaptive scarring and fibrosis [3]. On the other hand, EPCs include several cell types of blood-derived or vessel-derived cells with vascular repair function that are recruited to injured tissues and produce factors that facilitate vascular repair [4]. They may be expanded from peripheral blood or umbilical cord blood and have been studied in several models of vascular injury. Particular subtypes of EPCs, termed endothelial colony-forming cells (ECFCs), can integrate into sites of injury to augment neovascularization and improve tissue recovery [5]. Both MSCs and EPCs secrete paracrine factors and microvesicles that contain cytokines, chemokines and growth factors that can coordinate the overall repair response [6].
Statins are widely used clinically as cholesterol-lowering agents to prevent cardiovascular disease and have been used for many years with a favourable safety profile. More recently, it has been shown that statins can activate alternative signalling pathways to block apoptosis. In MSCs, lovastatin can activate the PI3K/Akt pathway and protect MSCs against hypoxia-induced apoptosis [7]. In a similar manner, simvastatin prevents the down-regulation of canonical Wnt signalling that reduces beta-catenin expression in renal mesangial cells in response to high glucose [8]. Statins have also demonstrated benefit in recent clinical studies, including the study of patients with kidney injury [9] and cancer patients [10] while statins were not effective in reducing exacerbations of COPD in a recent prospective trial [11], although the role of MSCs and EPCs were not addressed in these studies. While many promising studies have been reported, the extent to which statins can mobilize cells involved with tissue repair remains unknown and the role of statins in facilitating recovery of organ function in the context of cell-based therapy remains incompletely understood.
In this systemic review, we sought to summarize the results of preclinical and clinical studies that addressed the use of statins to augment MSC and EPC function in the context of cell-based therapy to repair organ function. Specifically, our aim was to identify whether statins improved organ recovery following tissue injury through the improved functioning of cells used in regenerative therapy. Moreover, we sought to characterize study quality and identify potential threats to bias to provide a platform for developing future clinical studies addressing use of statins in cell-based tissue repair strategies.
Methods
Search Strategy, Study Selection and Data Extraction
A systematic literature search was performed in accordance with recommendations by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [12]. A search strategy was developed by an information specialist to identify studies in MEDLINE, EMBASE, and PUBMED databases using the following search terms: (mesenchymal stromal cell or endothelial progenitor cell) AND (HMG co-A reductase or statin) AND (animals, animal experimentation, animal models of disease OR clinical study). Databases were searched from 1947 to June 25, 2013. The electronic search strategy is presented in appended supplemental material. In addition, reference lists of relevant studies were searched manually to identify any studies that may have been missed in the database search. Titles and abstracts of studies identified in the systematic search were screened for relevance independently by two investigators (AP and SP). After initial screen, relevant articles were retrieved for complete assessment of eligibility criteria (see below). Studies were classified based on clinical or preclinical nature of the study (ie. animal model), the type of injury or affected organ, and whether MSCs or EPCs were exposed to statins ex vivo as part of cellular therapy or in vivo as part of systemic combination treatment. Data was extracted independently by two individuals using standardized electronic forms. Discrepancies or disagreements were resolved by a third investigator.
Eligibility Criteria for Systematic Search
We included all pre-clinical controlled studies describing in vivo experiments involving the use of statin therapy or the administration of cells treated with a statin ex vivo and tested in animal models of organ injury, tumor growth or modulation of immune responses. Controlled clinical studies were included if patients received statin therapy or cells that were treated with a statin ex vivo and the function of specific progenitor cells were correlated with organ recovery following injury. Review articles, editorials, abstracts and studies describing only in vitro data were excluded. Articles that did not report measures of progenitor cell number or function or that did not include specific measures of organ function were excluded. Articles written in languages other than English or French were excluded.
Summary Measures and Synthesis of Results
In the absence of sufficient or appropriate data for pooling, results of individual studies were presented descriptively. Measures of study quality were extracted. For preclinical studies, we extracted key parameters of study design that would reduce the bias of investigators associated with preclinical studies, including whether a clear description was provided in the “Methods” section regarding the number of treated animals, whether randomization of the animals was performed, whether details regarding how many animals contributed to data were reported in the study, and whether blinding of investigators and/or lab personnel was described. These key parameters were recently identified as threats to validity in a systematic review of guidelines for preclinical studies [13]. For clinical studies, we extracted data related to study design that would reduce the risk of bias, including method of randomization and blinding (if used), and whether allocation of study subjects was concealed. We also extracted information regarding the specific statin used in the study, the specifics of the organ damage under study including the animal model used, and the details and timing of specific endpoints reported.
Results
Our systematic search yielded 771 citations. Following an initial screen for relevance, a total of 100 citations were identified and underwent detailed eligibility screening. In total, 38 studies met eligibility and were included in the review. Sixty two studies were excluded for the following reasons: abstract only with insufficient information available (29 reports); foreign language articles not in English or French which precluded reproducible data extraction (12 reports); duplicates (5 reports); editorials (1 reports); no control for statin treatment (6 reports); no measures of organ function reported (6 reports); in vitro data only (2 reports); and no data regarding the enumeration or function of MSCs or EPCs (1 report). Of the 38 studies that met the eligibility criteria and underwent data extraction, 31 were pre-clinical studies involving animal models and 7 were clinical studies involving human subjects (see Table 1). The study selection process is summarized in Fig. 1.
Studies were grouped into pre-clinical studies that involved statin treatment in combination with cell therapy (18 studies), preclinical studies of statin therapy alone (13 studies) and clinical studies of statin therapy (7 studies). Studies addressed cardiac injury (14 studies), vascular disorders (15 studies), neurologic conditions (8 studies) and bone fractures (1 study). Studies described the use of 6 different statins (atorvastatin used in 23 studies), given at various dosages (10–40 mg daily of atorvastatin in clinical studies; 10–30 mg/kg of atorvastatin in animal studies) and for differing durations (single injection to 6 months), precluding an analysis of dosage. All 18 of the preclinical studies using statins in combination with cell-based therapy and 11 of 13 studies using statins without cell therapy reported improved EPC or MSC number and/or function. Notably, pre-clinical studies addressing the administration of statins directly to animals measured the effects on EPCs only, and not MSCs, while 15 of 18 pre-clinical studies of statins in combination with cell-based therapy investigated the effects on MSCs. Despite marked variation in defining cell types, the specifics of inducing organ damage and timing and nature of specific endpoints of organ function, all but one of the preclinical studies reported improvement in organ function or organ perfusion with statin treatment (see below for more complete analysis and description). A total of 7 clinical studies of statin therapy were identified and none involved the administration of MSCs or EPC-like cells (see Table 1). All clinical studies involved the administration of statins or placebo to patients and measured the change in number and/or function of EPCs (no studies of MSCs) that were characterized from peripheral blood samples and correlated with recovery of organ-specific measurement outcomes (see Table 4). Three main organ systems were addressed in the clinical studies, including cardiac (5 studies, [45–49]), neurologic (1 study, [50]) and vascular systems (1 study, [51]). All 7 clinical studies reported improved EPC number and/or function and improved organ recovery with the use of statin therapy. Specifics of the studies and outcomes are described in more detail below and presented in Tables 2, 3 and 4.
Pre-clinical Studies of Cell Transplantation and Statin Therapy
A total of 18 pre-clinical studies combined statins with cell-based therapy using MSCs (15 studies) or EPCs (3 studies) to repair organ damage following acute myocardial infarction (7 studies, [14–20]), hindlimb ischemia (4 studies, [21–24]), neurologic damage (5 studies, [25–29]), orthopedic injury (1 study, [30]) or arterial injury (1 study, [31]) (see Tables 1 and 2). Amongst the seven studies that investigated MI [14–20], three used the swine as the animal model, three used rats, and one used mice. Studies administered MSCs as cell therapy and compared outcomes with controls that included MSCs only (6 studies), or saline (1 study). Four studies used atorvastatin as the statin of choice, two used rosuvastatin and one used simvastatin. All 7 studies reported improvement in cellular outcomes, including improved survival of transplanted cells (5 studies) ranging from 1.7-fold to 4.4-fold greater than controls and three studies reported decreased cell apoptosis (1.4-fold to 4.4-fold reduction compared with controls), and one study reported an increase in the proliferation of transplanted cells (see Table 2). All 7 studies of statins in combination with MSCs in animals with MI reported an improvement in cardiac function, including improved LVEF (1.4-fold to 8.7 fold greater improvement in LVEF or a 6.2–8.9 % absolute difference in LVEF compared with controls), reduced fibrosis (5 studies), reduced inflammation (5 studies), and reduced infarct size (4 studies) among other parameters of cardiac function (see Table 2).
Four studies addressed hindlimb ischemia [21–24] and the combined effect of statin therapy and MSC infusion (2 studies) or EPC therapy (2 studies). All four of these studies used mice. All of the studies reported improved outcomes, including greater incorporation of transplanted cells into sites of injury (1.6-fold to 2.2-fold greater than controls with cells only and 2.9-fold greater compared to saline), and decreased apoptosis in ischemic muscle in 2 studies (1.6-fold and 2.9-fold reduced compared with cells only). All four studies reported an improvement in capillary density at the site of injury (1.5-fold compared with cells only or with saline) and two studies also reported improved perfusion in the affected limb (1.1-fold greater than cells only and 2.2-fold greater than saline controls) (see Table 2).
Two studies investigated the effect of combined statin and cellular therapy in stroke [25, 26]. Both used rats and administered MSCs and simvastatin in comparison to control animals receiving MSCs alone. One study reported greater engraftment of transplanted cells (1.5-fold greater than MSCs only), while the other study did not report on cellular outcomes (see Table 2). Both studies, however, reported improved organ function with cell therapy combined with statin treatment, reporting a 2.5-fold improvement in somatosensory and 2.0-fold improvement in motor deficits compared with cells only. One study also reported a 1.6-fold improvement in modified Neurologic Severity Scores (mNSS), a 1.6-fold increase in vessel density and a 1.3-fold improvement in arterial density compared to MSCs only (see Table 2).
Two studies of traumatic brain injury in rats combined MSCs with simvastatin or atorvastatin in comparison to cell therapy alone [27, 28]. One study reported a 2.8-fold increase in the number of transplanted cells while the other study found no difference in transplanted cell number compared with controls (see Table 2). Both studies, however, reported a 4-fold improvement in mNSS scores. One study also found an improvement spatial learning and angiogenesis with combined therapy compared to controls.
MSC transplantation combined with simvastatin was investigated in a rat model of spinal cord injury [29] compared with cells alone and found that combined therapy increased survival of transplanted cells (8.2-fold greater) and differentiation of transplanted cells (3.5-fold greater) as well as improved spinal cord reparation with reduced motor deficits (1.4-fold) and lesion volume (2.1-fold).
One study looked at the effect of combined therapy on bone fractures in a rat model [30], transplanting MSCs and using simvastatin. When compared against MSC administration alone, combined therapy was associated with an increased number of transplanted cells and improved bone union (1.9-fold). Finally, one paper studied artery injury in a rat model [31], administering EPCs and simvastatin compared with cells only or saline and reported an improvement in mobilization and adhesion of transplanted cells in sites of injury (2.5-fold greater) and reported improved re-endothelialization (1.3-fold greater) (see Table 2).
Pre-clinical Studies with Statin Therapy Alone
Amongst 13 pre-clinical studies that used statin therapy alone without cell-based therapy in animal models of organ damage, 6 studies explored effects on the peripheral vascular system (studies on vascular effects in diabetes are described separately below), including arteriosclerosis [32], atherosclerosis [33], acute kidney injury [34], hindlimb ischemia [35], hypertension [36], and vascular grafts [37]. A variety of animal models were used, including mouse (3 studies), rat (1 study), swine (1 study), and dog (1 study). Four studies used atorvastatin for statin therapy and the remaining two studies used simvastatin. Four studies enumerated EPC-like cells which were defined as c-kit + cells, Sca1/flk-1+ cells, CD34+ cells or CD34+/KDR+ cells and increased 29–90 % compared to untreated controls after 3 days to 24 weeks of treatment (see Table 3). One study reported no change in CD34+/KDR+ cells after 12 weeks of statin treatment [36] and one study reported an increase in EPC colony-forming units after 2 weeks of statin therapy compared with controls [35] (see Table 3). Increased proliferation of EPCs (1 study), increased adhesion of EPCs (1 study), reduced apoptosis (1 study) and increased migration of EPCs (1 study) were also reported although no change in migration was reported in 1 study. Notably, all six of the studies on vascular injury reported improvement in at least one measurement of organ function following treatment with statin therapy in comparison to controls, including reduced vessel or graft occlusion, improved endothelialisation, better blood flow and greater blood vessel density ranging from 1.4-fold to 4.3-fold improvement of various functional parameters (see Table 3). Given the significant variation in disease models, duration of treatment and measurement of outcomes, pooling of data was not performed.
Three pre-clinical studies specifically investigated vascular defects in diabetes [38–40]. Two studies used a swine model and one study involved mice. All of the studies reported an increase in EPC number with statin therapy (CD34 + KDR+ cells or CD45-negative side population cells) between 2 and 2.3-fold compared with controls after 2 weeks–3 months of treatment. In 2 of 3 studies, improvement was reported in at least one measure of vascular function, including improved blood flow (1 study), improved FMD (1 study), improved angiogenesis and arteriogenesis (1 study), as well as a reduction in necrotic toes (1 study) (see Table 3).
Two pre-clinical studies explored the effect of statin therapy on repair of coronary artery disease [41] and myocardial infarction (MI) [42] using a swine and mouse model, respectively. The study of CAD used simvastatin and/or pravastatin whereas the MI study used atorvastatin. The study of CAD reported an increase in EPC colony-forming units while the MI study reported increased circulating EPC numbers. Both studies reported an improvement in organ function with a 46 % increase in capillary density after 30 days of statin treatment in pigs with CAD compared with controls and a 1.5-fold improvement in LVEF compared with controls following 4 weeks of statin therapy in mice with acute MI (see Table 3).
We identified two final pre-clinical studies that addressed the effects of statin therapy on neurologic injury, including traumatic brain injury [43] and diabetic retinopathy [44] using atorvastatin and simvastatin, respectively. Both studies used the rat model and correlated in vivo effects on CD31+ EPCs with organ repair. Following traumatic brain injury, EPC levels increased 2.2-fold in the ipsilateral cortex with statin therapy and greater incorporation of CD31+ EPCs was observed in retinal tissue of diabetic mice following statin therapy (1.5-fold greater compared to controls) (see Table 3). Mice with traumatic brain injury and treated with statins has a 1.3-fold greater improvement in mNSS scores compared to controls and long-term spatial learning was improved. Mice with diabetic retinopathy and treated with statins also had improved functional outcomes, including a 1.5-fold reduction in retinal edema compared to controls (see Table 3).
Clinical Studies with Statin Therapy Alone
All 7 clinical studies addressed the effects of statin therapy on EPCs which was similar to preclinical studies using statin therapy alone. Clinical studies of congestive heart failure (3 studies) and stroke (1 study), however, had not been reported previously in the pre-clinical setting and involved 90 patients (52 % of patients in published clinical trials) (see Table 4).
Three clinical studies explored the effect of statin therapy in patients with chronic heart failure (CHF) [45–47]. Two studies used rosuvastatin and one used atorvatastin. All three measured changes in EPCs although the studies utilized different cell markers and tests to define the EPC populations of interest. Cells with surface marker expression of CD34, CD34 and KDR co-expression with or without CD133, or acetylated LDL-positive cells were enumerated by flow cytometry and endothelial colony-forming cells were quantified in a culture-based assay in a third study (see Table 4). All three studies reported a significant increase in circulating levels of EPCs compared with controls (see Table 4). Migration and adhesion function were also measured in two of these studies with marked improvement in statin-treated patients (48–91 % improvement over baseline after 3–6 months of therapy). All of the studies also exhibited improved cardiac function, including improvement of flow-mediated dilatation (FMD) of 1.2-fold to 4-fold greater than controls receiving placebo (2 studies), improved LVEF from 30 ± 1 % to 38 ± 2 % compared with a 3 % improvement in the placebo group, a 9-fold improvement (p < 0.001) and a reduction of 14 % in pulmonary artery pressure compared with 5 % reduction with placebo (p < 0.01) in 1 study (see Table 4). Given the heterogeneity in terms of the tests used to quantify EPCs and measure changes in cell function, the variable duration of therapy and the different clinical end points reported, pooling of data was not performed.
Two additional clinical studies looked at the effect of statin therapy on coronary artery disease (CAD) [48, 49]. One study used atorvastatin and the other used rosuvastatin. One study reported an increase in circulating levels of EPCs after 5 days of statin therapy and the other reported greater numbers of colony-forming units after 6 months of treatment (see Table 4). Both studies reported clinical improvement in treated patients, with a 1.3-fold improvement in FMD in one study and reduced mediastinal drainage, fewer wound infections, reduced incidence of atrial fibrillation and other complications after following cardiac surgery.
One clinical study of patients with stroke investigated the use of atorvastatin or simvastatin and found a 4-fold increase (p = 0.002) in ECFCs after 7 days of treatment in statin-treated patients compared with placebo [50]. Moreover, treated patients had reduced infarct size on imaging (1.8-fold reduced compared with placebo group). A significant difference between atorvastatin and simvastatin as therapy was not reported (see Table 4).
A final clinical study that was identified studied the effect of statin therapy on smoking-related endothelial damage and found no change in EPC number after the administration of pitatastatin, however, FMD was increase by 49 ± 18 % with statin treatment vs. 1.4 ± 9.1 % in placebo (35-fold greater improvement, p = 0.022) [51] (see Table 4).
Threats to Bias
Twenty-two (58 %) of the 38 studies that underwent full review provided information in the “Methods” section regarding patient or animal randomization into treatment or control groups: 9 pre-clinical studies with combined statin and cell therapy [14–20, 26, 29], 7 pre-clinical studies with statin therapy alone [34, 37–40, 42, 43], and 6 clinical studies with statin therapy alone [45–49, 51]. Details of the randomization method, however, were lacking in most studies.
A total of 18 of the 22 randomized studies (82 %) provided information in the “Methods” section regarding blinding. Three clinical studies were double-blinded [45, 46, 48] while the remainder were single-blinded. Single blinding in pre-clinical studies meant that lab personnel performing lab testing on organ function or cellular testing were blinded to the treatment allocation. While all studies provided information in the results on the number of treated individuals, few studies provided a sample size calculation and no studies provided explicit information regarding animals that may have been treated but not accounted for in the results.
Discussion
In this systematic review, we have synthesized the pre-clinical and clinical experience describing the use of statin drugs in published studies to augment the function of MSCs and EPCs for regenerative cell-based therapy. The use of statins in combination with EPCs or MSCs in the context of cellular therapy appears promising in preclinical studies but has not been reported in human studies. A significant proportion of pre-clinical and clinical studies were randomized and were blinded, however, specific methodological details were not universally reported. Moreover, few preclinical studies provided sufficient detail to ensure that all treated animals were accounted for in the results and baseline testing of animal organ function or cellular function of MSCs or EPCs was rarely reported. A range of specific statins were used in the studies with few direct comparisons and no apparent advantage for any particular member of this drug class. Most clinical studies were randomized and reported on the effects of statin therapy on EPCs in the context of cardiovascular or other vascular injury. Remarkably, all preclinical and clinical studies reported benefit with statin therapy and improved MSC or EPC function and/or number. It was interesting to note that pre-clinical and clinical studies of statin therapy administered directly to subjects investigated the effects on EPCs and measures of vascular repair while studies of statins in combination with cell-based regenerative therapy studied MSCs. Studying the effects of statins on MSCs in clinical studies may be more challenging due to difficulties growing MSCs from peripheral blood samples. While the results were universally encouraging, important validation work remains and the possibility of important publication bias should temper enthusiasm. The use of statins to enhance cell-based vascular repair appears promising and warrants further study.
Strategies to enhance MSC and EPC function are needed to improve autologous-based treatment platforms due to known impairment in the function and/or mobilization of MSCs and EPCs in certain groups of patients. In particular, studies in patients with diabetes [52–54] and studies addressing the effects of aging [55] and smoking [56] have revealed reduced regenerative capacity and/or reduced numbers of MSCs and EPCs. Whether statins could be used in these patient groups to improve regenerative capacity will require further study. Increasing attention on the use of statins to improve organ function has raised interest in this area but studies do not focus on statin-induced MSC or EPC-based repair. The studies described in our systematic search reported benefit in studies of heart failure, coronary artery disease and stroke but the extent to which these cells were dysfunctional prior to administering statins is unknown. Baseline testing of cell function prior to the intervention and formal testing of organ function before treatment would increase the meaningfulness of observations. Moreover, autologous cell-based regenerative therapy typically involves the ex vivo expansion of MSCs, EPCs or other cells prior to re-infusion and the use of statins ex vivo to augment the function of autologous or allogeneic cells has not been addressed in published studies. Augmenting the number and function of MSCs and EPCs in third party collections remains highly relevant. The increasing practice of umbilical cord blood banking and placental tissue banking provides increasing options to grow specialised cellular products for regenerative therapy or immune modulation from banked cord blood [57]. The breadth of disorders treated with cord blood-derived cells continues to increase and was recently reviewed [58]. Strategies that build upon the efforts to bank umbilical cord blood would increase the impact of these investments. Other strategies to augment MSC and EPC number and function have also been described, including epigenetic modifications [59], enhanced homing strategies [60], and others.
Statin drugs were first tested in large cohorts of patients with hypercholesterolemia and then more broadly in patients with coronary artery disease [61, 62]. More recently, statins have been tested in newer indications, such as chronic kidney disease [9] and to prevent immune complications after blood stem cell transplantation [63]. High dose statin therapy has also been tested and appears to be well tolerated, even in older patients [64] . Statins have a favorable safety profile but can induce autoantibody formation in some patients which may contribute to myositis or rhabdomyolysis [65]. Ex vivo priming of cells during culture would limit systemic exposure of patients to significant levels although autoantibody production would still be a consideration and needs to be addressed in safety studies. Although the safety profile of statins is well established and appears favorable, reporting safety and tolerance in future preclinical trials and early phase clinical trials will remain essential.
Statins induce EPC mobilization in mice through the phosphatol inositol / Akt pathway [66]. Simvastatin rapidly activates Akt protein kinase and enhances the proliferation, migration and survival of EPCs in mice [67]. Lovastatin has been shown to induce similar changes in rat marrow-derived MSCs via the PI3K/Akt pathway and through ERK1/2 survival pathways [7]. Rosuvastatin was also shown to prolong MSC survival through PI3K/Akt signalling and increase therapeutic efficacy of adipose-derived MSCs in an animal model of myocardial infarction [20]. Additional drugs that activate the PI3K/Akt pathway may be worth considering as strategies to augment MSC or EPC-based cellular therapy. It is also possible that statins have more pleiotropic effects in progenitor cells and other mechanisms of action may be relevant.
We acknowledge that systematic reviews of preclinical studies may present a bias towards an overestimation of favourable outcomes since results of negative preclinical studies are less likely to be published. This may be particularly true in our study as all published preclinical studies reported benefit with statin therapy. Moreover, the quality of preclinical studies is typically reduced in comparison to human clinical trials and several threats to validity have been recently reported [13] and have been considered. Threats to the validity of preclinical studies can complicate or delay the translation of preclinical studies into the clinical realm. For example, preclinical studies are less likely to involve robust randomization methods or blinding and this was observed in some of the studies included in our systematic review. Moreover, the relative homogeneity of animals used in preclinical studies is in stark contrast to the heterogeneity that characterizes the realities of clinical studies. This may explain the observation that studies in our review did not provide baseline characteristics of animals with regard to organ function and this appears to be the reality of preclinical trials at this juncture. Pre-clinical studies also may not provide precise details regarding the exact allocation of animals to each treatment group or account for all treated animals in their results, which can bias the interpretation of results. In addition, clinical trials of statins in combination with MSCs or EPCs will be essential for validating the observations reported to date in preclinical studies. Since our systematic review did not identify any clinical studies of cell-based therapy in combination with statin treatment, it would be interesting to perform correlative analysis of concomitant drug usage in cohort studies of cell-based regenerative therapy to gain additional insight on the role of statins to augment the regenerative function of progenitor cells in the clinical setting.
In summary, our systematic review provides a foundation of encouraging results that support further study of statins in regenerative therapy to augment the number and/or function of MSCs and EPCs. Our systematic search highlights potential publication bias, however, and enthusiasm should be tempered when considering these positive results. More work is needed to accelerate progress in the area of statin treatment in combination with MSCs or EPCs in cell-based regenerative medicine.
References
Martin, I., Baldomero, H., Tyndall, A., Niederwiesser, D., & Gratwohl, A. (2010). A survey on cellular and engineered tissue therapies in Europe in 2008. Tissue Engineering. Part A, 16, 2419–2427.
Dominici, M., Le, B. K., Mueller, I., et al. (2006). Minimal criteria for defining multipotent mesenchymal stromalcells. The International Society for cellular therapy position statement. Cytotherapy, 8, 315–317.
Hofmann, N. A., Ortner, A., Jacamo, R. O., et al. (2012). Oxygen sensing mesenchymal progenitors promote neo-vasculogenesis in a humanized mouse model in vivo. PLoS ONE, 7, e44468.
Critser, P. J., Voytik-Harbin, S. L., & Yoder, M. C. (2011). Isolating and defining cells to engineer human blood vessels. Cell Proliferation, 33(1), 15–21.
Palii, C., Vulesevic, B., Fraineau, S., Pranckeviciene, E., Griffith, A. J., Chu, A., Faralli, H., Li, Y., McNeill, B., Sun, J., Perkins, T. J., Dilworth, F. J., Perez-Iratxeta, C., Suuronen, E. J., Allan, D. S., & Brand, M. (2014). Trichostatin A enhances the vascular repair function of injected human endothelial progenitors by increasing the expression of TAL1-dependent genes. Cell Stem Cell, 14, 644–657.
Akyurekli, C., Le, Y., Richardson, R., Fergusson, D., Tay, J., & Allan, D.S. (2014). A systematic review of preclinical studies on the therapeutic potential of mesenchymal stromal cell-derived microvesicles. Stem Cell Reviews and Reports.
Xu, R., Chen, J., Cong, X., Hu, S., & Chen, X. (2008). Lovastatin protects mesenchymal stem cells against hypoxia- and serum deprivation-induced apoptosis by activation of PI3K/Akt and ERK1/2. Journal of Cellular Biochemistry, 103, 256–269.
Lin, C. L., Cheng, H., Tung, C. W., et al. (2008). Simvastatin reverses high glucose-induced apoptosis of mesangial cells via modulation of Wnt Signaling pathway. American Journal of Nephrology, 28, 290–297.
Yan, Y. L., Qiu, B., Wang, J., et al. (2015). High-intensity statin therapy in patients with chronic kidney disease: a systematic review and meta-analysis. BMJ Open, 5, e006886.
Jeon, C. Y., Pandol, S. J., Wu, B., et al. (2015). The association of statin use after cancer diagnosis with survival in pancreatic cancer patients: a SEER-medicare analysis. PLoS ONE, 10, e0121783.
Criner, G. J., Connett, J. E., Aaron, R. K., et al. (2014). Simvastatin for the prevention of exacerbations in moderate-to-severe COPD. The New England Journal of Medicine, 370, 2201–2210.
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., & PRISMA Group. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Medicine, 6, e1000097.
Henderson, V. C., Kimmelman, J., Fergusson, D., Grimshaw, J. M., & Hackam, D. G. (2013). Threats to validity in the design and conduct of preclinical efficacy studies: a systematic review of guidelines for in vivo animal experiments. PLoS Medicine, 10, e1001489.
Song, L., Yang, Y. J., Dong, Q. T., et al. (2013). Atorvastatin enhance efficacy of mesenchymal stem cells treatment for swine myocardial infarction via activation of nitric oxide synthase. PLoS ONE, 8(5), e65702.
Yang, Y. J., Qian, H. Y., Huang, J., et al. (2008). Atorvastatin treatment improves survival and effects of implanted mesenchymal stem cells in post-infarct swine hearts. European Heart Journal, 29(12), 1578–1590.
Yang, Y. J., Qian, H. Y., Huang, J., et al. (2009). Combined therapy with simvastatin and bone marrow-derived mesenchymal stem cells increases benefits in infarcted swine hearts. Arteriosclerosis, Thrombosis, and Vascular Biology, 29(12), 2076–2082.
Cai, A., Zheng, D., Dong, Y., et al. (2011). Efficacy of Atorvastatin combined with adipose-derived mesenchymal stem cell transplantation on cardiac function in rats with acute myocardial infarction. Acta Biochimica et Biophysica Sinica (Shanghai), 43(11), 857–866.
Wang, A., Shen, F., Liang, Y., & Wang, J. (2011). Marrow-derived MSCs and atorvastatin improve cardiac function in rat model of AMI. International Journal of Cardiology, 150(1), 28–32.
Xu, H., Yang, Y. J., Qian, H. Y., et al. (2011). Rosuvastatin treatment activates JAK-STAT pathway and increases efficacy of allogeneic mesenchymal stem cell transplantation in infarcted hearts. Circulation Journal, 75(6), 1476–1485.
Zhang, Z., Li, S., Cui, M., et al. (2013). Rosuvastatin enhances the therapeutic efficacy of adipose-derived mesenchymal stem cells for myocardial infarction via PI3K/Akt and MEK/ERK pathways. Basic Research in Cardiology, 108(2), 333.
Li, Y., Zhang, D., Zhang, Y., He, G., & Zhang, F. (2010). Augmentation of neovascularization in murine hindlimb ischemia by combined therapy with simvastatin and bone marrow-derived mesenchymal stem cells transplantation. Journal of Biomedical Science, 17, 75.
Zhang, Y., Zhang, R., Li, Y., et al. (2012). Simvastatin augments the efficacy of therapeutic angiogenesis induced by bone marrow-derived mesenchymal stem cells in a murine model of hindlimb ischemia. Molecular Biology Reports, 39(1), 285–293.
Hu, Z., Zhang, F., Yang, Z., et al. (2008). Combination of simvastatin administration and EPC transplantation enhances angiogenesis and protects against apoptosis for hindlimb ischemia. Journal of Biomedical Science, 15(4), 509–517.
Zhou, J., Cheng, M., Liao, Y. H., et al. (2013). Rosuvastatin enhances angiogenesis via eNOS-dependent mobilization of endothelial progenitor cells. PLoS ONE, 8(5), e63126.
Cui, X., Chopp, M., Zacharek, A., et al. (2009). Chemokine, vascular and therapeutic effects of combination Simvastatin and BMSC treatment of stroke. Neurobiology of Disease, 36(1), 35–41.
Pirzad, J. G., Seidi, S., Sadr, S. S., et al. (2012). Therapeutic effects of a combinatorial treatment of simvastatin and bone marrow stromal cells on experimental embolic stroke. Basic and Clinical Pharmacology and Toxicology, 110(6), 487–493.
Mahmood, A., Lu, D., Qu, C., Goussev, A., & Chopp, M. (2007). Treatment of traumatic brain injury with a combination therapy of marrow stromal cells and atorvastatin in rats. Neurosurgery, 60(3), 546–553.
Mahmood, A., Goussev, A., Lu, D., et al. (2008). Long-lasting benefits after treatment of traumatic brain injury (TBI) in rats with combination therapy of marrow stromal cells (MSCs) and simvastatin. Journal of Neurotrauma, 25(12), 1441–1447.
Han, X., Yang, N., Cui, Y., et al. (2012). Simvastatin mobilizes bone marrow stromal cells migrating to injured areas and promotes functional recovery after spinal cord injury in the rat. Neuroscience Letters, 521(2), 136–141.
Qi, Y., Zhao, T., Yan, W., et al. (2013). Mesenchymal stem cell sheet transplantation combined with locally released simvastatin enhances bone formation in a rat tibia osteotomy model. Cytotherapy, 15(1), 44–56.
Walter, D. H., Rittig, K., Bahlmann, F. H., et al. (2002). Statin therapy accelerates reendothelialization: a novel effect involving mobilization and incorporation of bone marrow-derived endothelial progenitor cells. Circulation, 105(25), 3017–3024.
Roux, N., Brakenhielm, E., Freguin-Bouillant, C., et al. (2012). Progenitor cell mobilizing treatments prevent experimental transplant arteriosclerosis. Journal of Surgical Research, 176(2), 657–665.
Steinmetz, M., Pelster, B., Lucanus, E., et al. (2013). Atorvastatin-induced increase in progenitor cell levels is rather caused by enhanced receptor activator of NF-kappaB ligand (RANKL) cell proliferation than by bone marrow mobilization. Journal of Molecular and Cellular Cardiology, 57, 32–42.
Wu, V. C., Young, G. H., Huang, P. H., et al. (2013). In acute kidney injury, indoxyl sulfate impairs human endothelial progenitor cells: modulation by statin. Angiogenesis, 16(3), 609–624.
Matsumura, M., Fukuda, N., Kobayashi, N., et al. (2009). Effects of atorvastatin on angiogenesis in hindlimb ischemia and endothelial progenitor cell formation in rats. Journal of Atherosclerosis and Thrombosis, 16(4), 319–326.
Lavi, R., Zhu, X. Y., Chade, A. R., et al. (2010). Simvastatin decreases endothelial progenitor cell apoptosis in the kidney of hypertensive hypercholesterolemic pigs. Arteriosclerosis, Thrombosis, and Vascular Biology, 30(5), 976–983.
Jie, L., Lu, W. M., Li, X. X., et al. (2010). Intensive statin therapy: a favorable adjunct to the improvement of small-diameter vascular grafts. Angiology, 61(5), 427–436.
Mohler, E. R., Shi, Y., Moore, J., et al. (2009). Diabetes reduces bone marrow and circulating porcine endothelial progenitor cells, an effect ameliorated by atorvastatin and independent of cholesterol. Cytometry. Part A, 75(1), 75–82.
Roan, J. N., Fang, S. Y., Chang, S. W., et al. (2012). Rosuvastatin improves vascular function of arteriovenous fistula in a diabetic rat model. Journal of Vascular Surgery, 56(5), 1381.e1–1389.e1.
Emanueli, C., Monopoli, A., Kraenkel, N., et al. (2007). Nitropravastatin stimulates reparative neovascularisation and improves recovery from limb Ischaemia in type-1 diabetic mice. British Journal of Pharmacology, 150(7), 873–882.
Wang, W., Lang, J. K., Suzuki, G., Canty, J. M., Jr., & Cimato, T. (2011). Statins enhance clonal growth of late outgrowth endothelial progenitors and increase myocardial capillary density in the chronically ischemic heart. PLoS ONE, 6(9), e24868.
Landmesser, U., Engberding, N., Bahlmann, F. H., et al. (2004). Statin-induced improvement of endothelial progenitor cell mobilization, myocardial neovascularization, left ventricular function, and survival after experimental myocardial infarction requires endothelial nitric oxide synthase. Circulation, 110(14), 1933–1939.
Wang, B., Sun, L., Tian, Y., et al. (2012). Effects of atorvastatin in the regulation of circulating EPCs and angiogenesis in traumatic brain injury in rats. Journal of Neurological Sciences, 319(1-2), 117–123.
Zhang, W., & Yan, H. (2012). Simvastatin increases circulating endothelial progenitor cells and reduces the formation and progression of diabetic retinopathy in rats. Experimental Eye Research, 105, 1–8.
Erbs, S., Beck, E. B., Linke, A., et al. (2011). High-dose rosuvastatin in chronic heart failure promotes vasculogenesis, corrects endothelial function, and improves cardiac remodeling--results from a randomized, double-blind, and placebo-controlled study. International Journal of Cardiology, 146(1), 56–63.
Tousoulis, D., Andreou, I., Tsiatas, M., et al. (2011). Effects of rosuvastatin and allopurinol on circulating endothelial progenitor cells in patients with congestive heart failure: the impact of inflammatory process and oxidative stress. Atherosclerosis, 214(1), 151–157.
Liu, H. F., Qi, X. W., Ma, L. L., Yao, D. K., & Wang, L. (2013). Atorvastatin improves endothelial progenitor cell function and reduces pulmonary hypertension in patients with chronic pulmonary heart disease. Experimental and Clinical Cardiology, 18(1), e40–e43.
Baran, Ç., Durdu, S., Dalva, K., et al. (2012). Effects of preoperative short term use of atorvastatin on endothelial progenitor cells after coronary surgery: a randomized, controlled trial. Stem Cell Reviews, 8(3), 963–971.
Yun, K. H., Shin, I. S., Park, E. M., et al. (2008). Effect of additional statin therapy on endothelial function and prognosis in patients with vasospastic angina. Korean Circulation Journal, 38(12), 638–643.
Sobrino, T., Blanco, M., Pérez-Mato, M., Rodríguez-Yáñez, M., & Castillo, J. (2012). Increased levels of circulating endothelial progenitor cells in patients with ischaemic stroke treated with statins during acute phase. European Journal of Neurology, 19(12), 1539–1546.
Yoshida, O., Kondo, T., Kureishi-Bando, Y., et al. (2010). Pitavastatin, an HMG-CoA reductase inhibitor, ameliorates endothelial function in chronic smokers. Circulation Journal, 74(1), 195–202.
Antonio, N., Soares, A., Fernandes, R., et al. (2014). Endothelial progenitor cells in diabetic patients with myocardial infarction – can statins improve their function? European Journal of Pharmacology, 741, 25–36.
Yuan, Q., Hu, C. P., Gong, Z. C., et al. (2015). Accelerated onset of senescence of endothelial progenitor cells in patients with type 2 diabetes mellitus: role of dimethylarginine dimethylaminohydrolase 2 and asymmetric dimethylarginine. Biochemical and Biophysical Research Communications, 458, 869–876.
Kim, J., Piao, Y., Pak, Y. K., et al. (2015). Umbilical cord mesenchymal stromal cells affected by gestational diabetes mellitus display premature aging and mitochondrial dysfunction. Stem Cells and Development, 24, 575–586.
Yu, K. R., & Kang, K. S. (2013). Aging-related genes in mesenchymal stem cells: a mini-review. Gerontology, 59, 557–563.
Zeng, H. L., Qin, Y. L., Chen, H. Z., et al. (2014). Effects of nicotine on proliferation and survival in human umbilical cord mesenchymal stem cells. Journal of Biochemical and Molecular Toxicology, 28, 181–189.
Klowak, J., Chung, J., & Allan, D.S. (2012). Cord blood banking for regenerative therapy. In D.S. Allan and D. Strunk (Eds.), Regenerative therapy using blood-derived stem cells. Science.
Fraineau, S., Palii, C.G., Allan, D.S., & Brand, M. (2014). Epigenetic regulation of endothelial stem/progenitor cell-mediated vascular repair. FEBS Journal.
Iafolla, M. A. J., Tay, J., & Allan, D. S. (2014). Transplantation of umbilical cord blood-derived cells for novel indications in regenerative or immunomodulatory therapy: a scoping review of clinical studies. Biology of Blood and Marrow Transplantation, 20, 20–25.
Eseonu, O. I., & De Bari, C. (2015). Homing of mesenchymal stem cells: mechanistic or stochastic? Implications for targeted delivery in arthritis. Rheumatology (Oxford), 54, 210–218.
(1994). Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet, 344,1383–1389.
Shepherd, J., Cobbe, S. M., Ford, I., et al. (1995). Prevention of coronary heart disease with pravastatin in men with hypercholersterolemia: west of Scotland Coronary Prevention Study Group. The New England Journal of Medicine, 333, 1301–1307.
Hamadini, M., Gibson, L. F., Remick, S. C., et al. (2013). Sibling donor and recipient immune modulation with atorvastatin for the prophylaxis of acute graft-versus-host-disease. Journal of Clinical Oncology, 31, 4416–4423.
Manocha, D., Bansal, N., Gumaste, P., & Brangman, S. (2013). Safety profile of high-dose statin therapy in geriatric patients with stroke. Southern Medical Journal, 106, 658–664.
Mohassel, P., & Mammen, A. L. (2013). Statin-associated autoimmune myopathy and anti-HMGCR autoantibodies. Muscle and Nerve, 48, 477–483.
Dimmeler, S., Aicher, A., Vasa, M., et al. (2001). HMG-CoA reductase inhibitors (statins) increase endothelial progenitor cells via the PI 3-kinase/Akt pathway. Journal of Clinical Investigation, 108, 391–397.
Llevadot, J., Murasawa, S., Kureishi, Y., et al. (2001). HMG-coAreductase inhibitor mobilizes bone marrow-derived endothelial progenitor cells. Journal of Clinical Investigation, 108, 399–405.
Acknowledgments
We wish to acknowledge the expertise and assistance of Risa Shorr from the library at The Ottawa Hospital for help with design and execution of the systematic search. Funding support for the project was provided by the Department of Medicine, University of Ottawa. We gratefully acknowledge support from Canadian Institutes of Health Research for a summer student award (SP) and a New Investigator Award (DSA) and support for a summer student research stipend from the Mach-Gaesslen Foundation of Canada (JBR). An endowed Chair in Clinical Epidemiology (DF) from the University of Ottawa (U of O) and Ottawa Hospital Research Institute is gratefully acknowledged. DSA is supported in part by the Department of Medicine at U of O. None of the authors have any conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
The authors declare no potential conflicts of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 74.9 kb)
Rights and permissions
About this article
Cite this article
Park, A., Barrera-Ramirez, J., Ranasinghe, I. et al. Use of Statins to Augment Progenitor Cell Function in Preclinical and Clinical Studies of Regenerative Therapy: a Systematic Review. Stem Cell Rev and Rep 12, 327–339 (2016). https://doi.org/10.1007/s12015-016-9647-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12015-016-9647-7